Paramedics Performed Sonographic Identification of the Conic Ligament—A Prospective Controlled Trial
Abstract
1. Introduction
1.1. Background
1.2. Research Problem and Aim
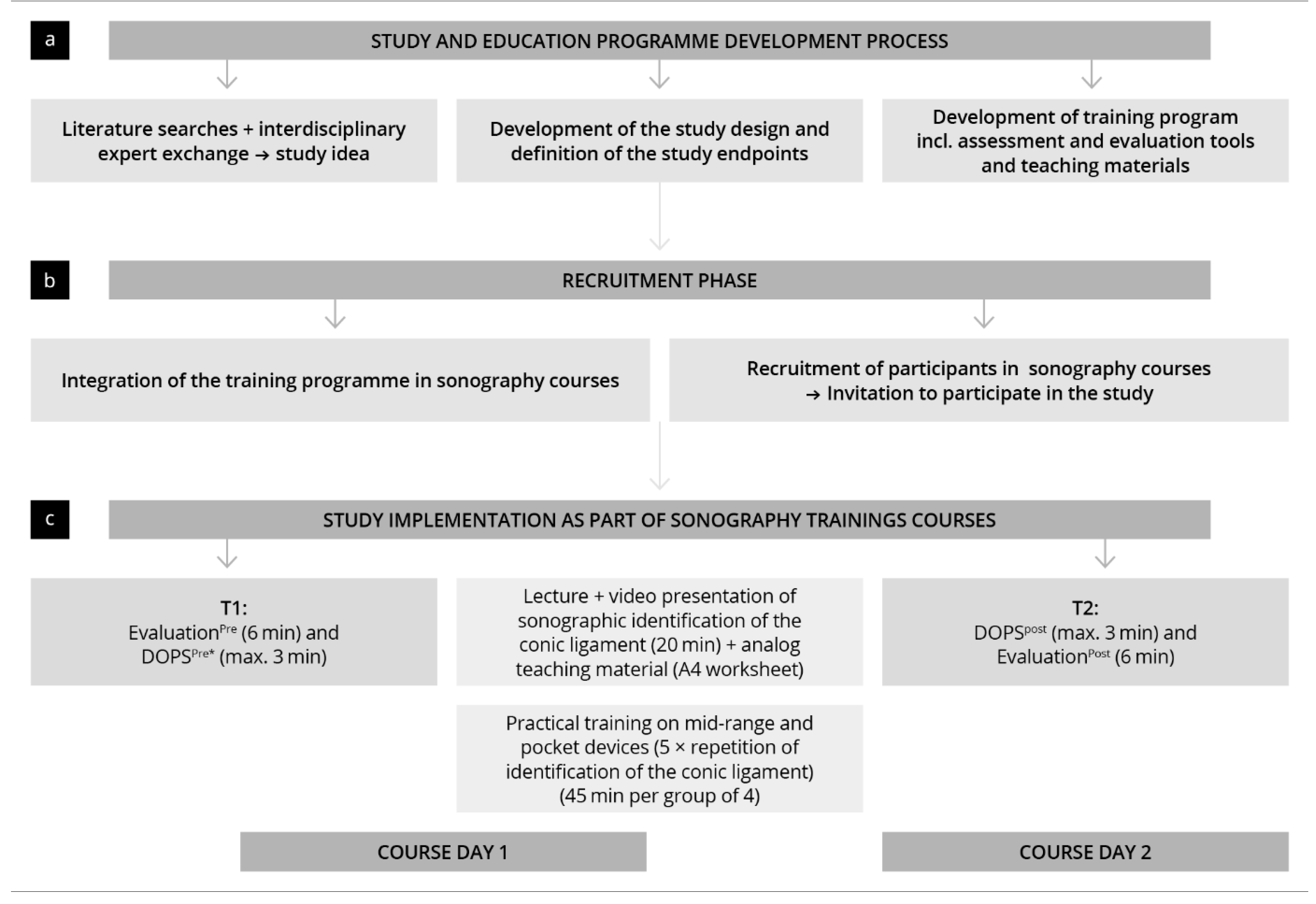
2. Material and Methodology
2.1. Study Design, Participant Recruitment, and Inclusion Criteria
2.2. Training and Study-Materials
- 10-min theoretical training (lecture);
- A worksheet and complementary 10-min video presentation of sonographic instructions;
- 45-min practical training in groups of 4.
2.3. Questionnaires and Practical Tests
2.3.1. Questionnaires
2.3.2. Practical Test
2.3.3. Statistics
3. Results
3.1. Demographics and Previous Experience
3.2. Practical Skills Development
3.3. Validation of Practical Test
3.4. Factors Influencing DOPS Results and Time to Completion
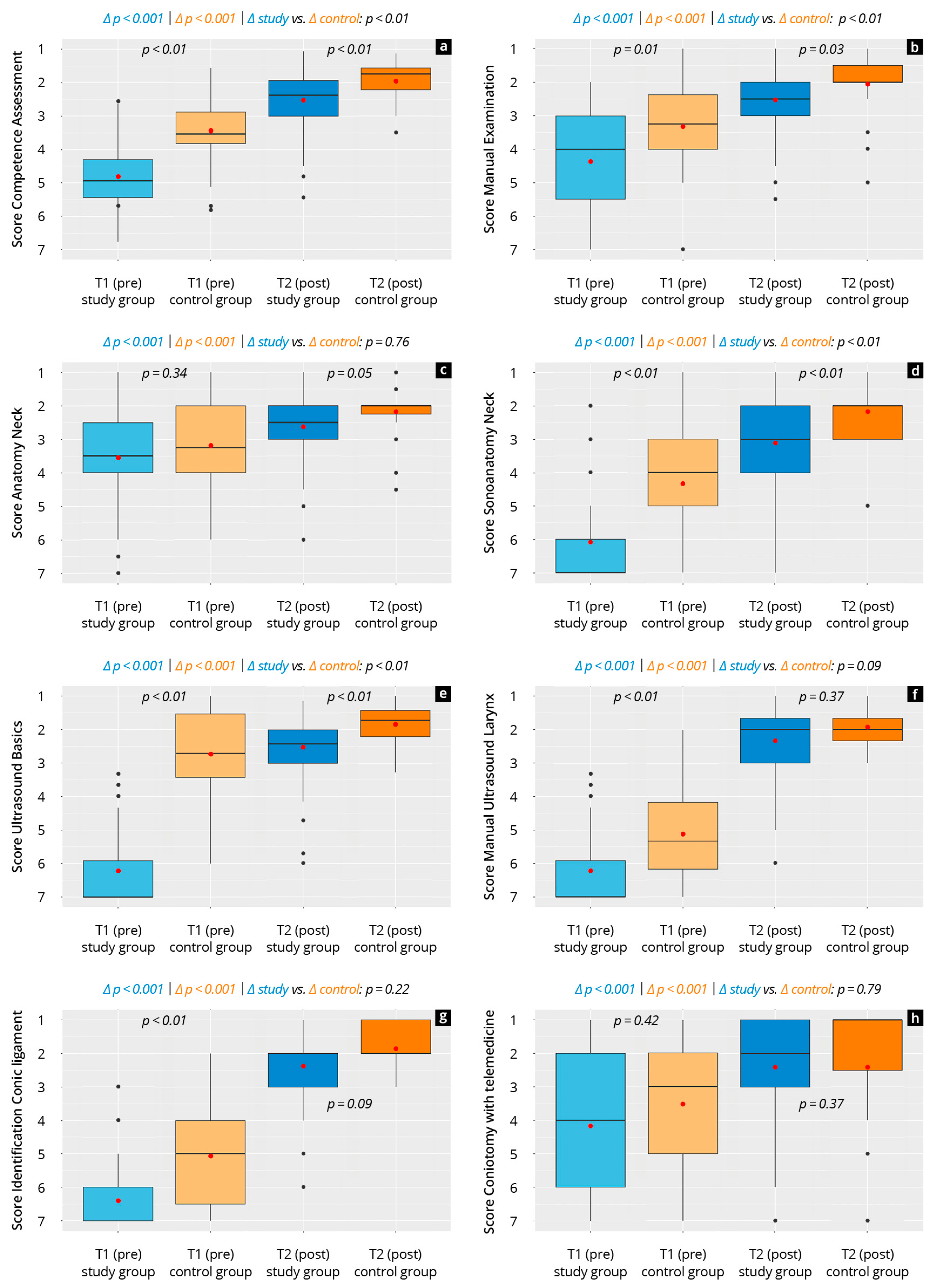
3.5. Subjective Development of Competency
3.6. Evaluation of Training and Study Materials
4. Discussion
4.1. Objective and Subjective Competencies
4.2. Training
4.3. Outlook
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, S.; Liu, M.; Ball, I.; Meunier, B.; Hilsden, R. A Systematic Review of Prehospital Combat Airway Management. J. Spec. Oper. Med. 2023, 23, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Piepho, T.; Kriege, M.; Byhahn, C.; Cavus, E.; Dörges, V.; Ilper, H.; Kehl, F.; Loop, T.; Raymondos, K.; Sujatta, S.; et al. S1 Leitlinie Atemwegsmanagement 2023. Available online: https://register.awmf.org/assets/guidelines/001-028l_S1_Atemwegsmanagement_2023-09.pdf (accessed on 10 February 2025).
- Apfelbaum, J.L.; Hagberg, C.A.; Connis, R.T.; Abdelmalak, B.B.; Agarkar, M.; Dutton, R.P.; Fiadjoe, J.E.; Greif, R.; Klock, P.A.; Mercier, D.; et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology 2022, 136, 31–81. [Google Scholar] [CrossRef]
- Kornas, R.L.; Owyang, C.G.; Sakles, J.C.; Foley, L.J.; Mosier, J.M. Evaluation and Management of the Physiologically Difficult Airway: Consensus Recommendations From Society for Airway Management. Anesth. Analg. 2021, 132, 395–405. [Google Scholar] [CrossRef]
- Law, J.A.; Duggan, L.V.; Asselin, M.; Baker, P.; Crosby, E.; Downey, A.; Hung, O.R.; Jones, P.M.; Lemay, F.; Noppens, R.; et al. Canadian Airway Focus Group updated consensus-based recommendations for management of the difficult airway: Part 1. Difficult airway management encountered in an unconscious patient. Can. J. Anaesth. 2021, 68, 1373–1404. [Google Scholar] [CrossRef] [PubMed]
- Mutzbauer, T.S.; Keul, W.; Bernhard, M.; Völkl, A.; Gries, A. Invasive techniques in emergency medicine. IV. Cricothyrotomy in emergency situations. Anaesthesist 2005, 54, 145–154. [Google Scholar] [CrossRef]
- DeVore, E.K.; Redmann, A.; Howell, R.; Khosla, S. Best practices for emergency surgical airway: A systematic review. Laryngoscope Investig. Otolaryngol. 2019, 4, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Walls, R.M. Cricothyroidotomy. Emerg. Med. Clin. N. Am. 1988, 6, 725–736. [Google Scholar] [CrossRef]
- Aziz, S.; Foster, E.; Lockey, D.J.; Christian, M.D. Emergency scalpel cricothyroidotomy use in a prehospital trauma service: A 20-year review. Emerg. Med. J. 2021, 38, 349–354. [Google Scholar] [CrossRef]
- Chang, J.E.; Kim, H.; Won, D.; Lee, J.M.; Kim, T.K.; Min, S.W.; Hwang, J.Y. Comparison of the Conventional Downward and Modified Upward Laryngeal Handshake Techniques to Identify the Cricothyroid Membrane: A Randomized, Comparative Study. Anesth. Analg. 2021, 133, 1288–1295. [Google Scholar] [CrossRef]
- Campbell, M.; Shanahan, H.; Ash, S.; Royds, J.; Husarova, V.; McCaul, C. The accuracy of locating the cricothyroid membrane by palpation—An intergender study. BMC Anesthesiol. 2014, 14, 108. [Google Scholar] [CrossRef]
- You-Ten, K.E.; Wong, D.T.; Ye, X.Y.; Arzola, C.; Zand, A.; Siddiqui, N. Practice of Ultrasound-Guided Palpation of Neck Landmarks Improves Accuracy of External Palpation of the Cricothyroid Membrane. Anesth. Analg. 2018, 127, 1377–1382. [Google Scholar] [CrossRef]
- Siddiqui, N.; Yu, E.; Boulis, S.; You-Ten, K.E. Ultrasound Is Superior to Palpation in Identifying the Cricothyroid Membrane in Subjects with Poorly Defined Neck Landmarks: A Randomized Clinical Trial. Anesthesiology 2018, 129, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.S.; Teoh, W.H.; Rudolph, S.S. Ultrasonographic identification of the cricothyroid membrane: Best evidence, techniques, and clinical impact. Br. J. Anaesth. 2016, 117 (Suppl. S1), i39–i48. [Google Scholar] [CrossRef]
- Kristensen, M.S.; Teoh, W.H. Ultrasound identification of the cricothyroid membrane: The new standard in preparing for front-of-neck airway access. Br. J. Anaesth. 2021, 126, 22–27. [Google Scholar] [CrossRef]
- Hung, K.C.; Chen, I.W.; Lin, C.M.; Sun, C.K. Comparison between ultrasound-guided and digital palpation techniques for identification of the cricothyroid membrane: A meta-analysis. Br. J. Anaesth. 2021, 126, e9–e11. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, N.; Arzola, C.; Friedman, Z.; Guerina, L.; You-Ten, K.E. Ultrasound Improves Cricothyrotomy Success in Cadavers with Poorly Defined Neck Anatomy: A Randomized Control Trial. Anesthesiology 2015, 123, 1033–1041. [Google Scholar] [CrossRef]
- Bair, A.E.; Panacek, E.A.; Wisner, D.H.; Bales, R.; Sakles, J.C. Cricothyrotomy: A 5-year experience at one institution. J. Emerg. Med. 2003, 24, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Marcolini, E.G.; Burton, J.H.; Bradshaw, J.R.; Baumann, M.R. A standing-order protocol for cricothyrotomy in prehospital emergency patients. Prehospital Emerg. Care 2004, 8, 23–28. [Google Scholar] [CrossRef]
- Weimer, A.M.; Weimer, J.M.; Jonck, C.; Müller, L.; Stäuber, M.; Chrissostomou, C.D.; Buggenhagen, H.; Klöckner, R.; Pirlich, N.; Künzel, J.; et al. Ultrasound supported identification of the ligamentum conicum in teaching head and neck sonography. Laryngorhinootologie 2024, 104, 23–33. [Google Scholar] [CrossRef]
- Kristensen, M.S.; Teoh, W.H.; Rudolph, S.S.; Tvede, M.F.; Hesselfeldt, R.; Børglum, J.; Lohse, T.; Hansen, L.N. Structured approach to ultrasound-guided identification of the cricothyroid membrane: A randomized comparison with the palpation method in the morbidly obese. Br. J. Anaesth. 2015, 114, 1003–1004. [Google Scholar] [CrossRef]
- Kristensen, M.S.; Teoh, W.H.; Rudolph, S.S.; Hesselfeldt, R.; Børglum, J.; Tvede, M.F. A randomised cross-over comparison of the transverse and longitudinal techniques for ultrasound-guided identification of the cricothyroid membrane in morbidly obese subjects. Anaesthesia 2016, 71, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, K.F.; Arzola, C.; Ye, X.Y.; Clivatti, J.; Siddiqui, N.; You-Ten, K.E. Determining the amount of training needed for competency of anesthesia trainees in ultrasonographic identification of the cricothyroid membrane. BMC Anesthesiol. 2017, 17, 74. [Google Scholar] [CrossRef] [PubMed]
- Yıldız, G.; Göksu, E.; Şenfer, A.; Kaplan, A. Comparison of ultrasonography and surface landmarks in detecting the localization for cricothyroidotomy. Am. J. Emerg. Med. 2016, 34, 254–256. [Google Scholar] [CrossRef] [PubMed]
- Barbe, N.; Martin, P.; Pascal, J.; Heras, C.; Rouffiange, P.; Molliex, S. Locating the cricothyroid membrane in learning phase: Value of ultrasonography? Ann. Fr. D’anesthesie Reanimation 2014, 33, 163–166. [Google Scholar] [CrossRef]
- Shetty, K.; Nayyar, V.; Stachowski, E.; Byth, K. Training for cricothyroidotomy. Anaesth. Intensive Care 2013, 41, 623–630. [Google Scholar] [CrossRef]
- Andresen Å, E.L.; Kramer-Johansen, J.; Kristiansen, T. Emergency cricothyroidotomy in difficult airway simulation—A national observational study of Air Ambulance crew performance. BMC Emerg. Med. 2022, 22, 64. [Google Scholar] [CrossRef]
- Backlund, B.; Utarnachitt, R.; Jauregui, J.; Watase, T. A Comprehensive Course for Teaching Emergency Cricothyrotomy. J. Educ. Teach. Emerg. Med. 2020, 5, Sg17–Sg35. [Google Scholar] [CrossRef]
- Speck, I.; Merk, A.; Burkhardt, V.; Flayyih, O.; Huber, C.; Widder, A.; Everad, F.; Offergeld, C. Virtual reality cricothyrotomy—A case-control study on gamification in emergency education. BMC Med. Educ. 2024, 24, 148. [Google Scholar] [CrossRef]
- Fairley, R.R.; Ahmed, S.; Schauer, S.G.; Wampler, D.A.; Tanaka, K.; Everitt, B.; Sparkman, M.K.; Casanova, R.; Sifuentes, J.; Winckler, C.J. A Pilot Study to Assess Urban, Fire-Based Paramedic Accuracy in Identification of Anatomical Landmarks Necessary for Cricothyrotomy and Needle Chest Decompression Using Live Patient Models. Prehospital Disaster Med. 2021, 36, 408–411. [Google Scholar] [CrossRef]
- Weimer, J.M.; Beer, D.; Schneider, C.; Yousefzada, M.; Gottwald, M.; Züllich, T.F.; Weimer, A.; Jonck, C.; Buggenhagen, H.; Kloeckner, R.; et al. Inter-System Variability of Eight Different Handheld Ultrasound (HHUS) Devices—A Prospective Comparison of B-Scan Quality and Clinical Significance in Intensive Care. Diagnostics 2024, 14, 54. [Google Scholar]
- Merkel, D.; Lueders, C.; Schneider, C.; Yousefzada, M.; Ruppert, J.; Weimer, A.; Herzog, M.; Lorenz, L.A.; Vieth, T.; Buggenhagen, H.; et al. Prospective Comparison of Nine Different Handheld Ultrasound (HHUS) Devices by Ultrasound Experts with Regard to B-Scan Quality, Device Handling and Software in Abdominal Sonography. Diagnostics 2024, 14, 1913. [Google Scholar] [CrossRef] [PubMed]
- von Foerster, N.; Radomski, M.A.; Martin-Gill, C. Prehospital Ultrasound: A Narrative Review. Prehospital Emerg. Care 2022, 28, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Sotoodehnia, M.; Rafiemanesh, H.; Mirfazaelian, H.; Safaie, A.; Baratloo, A. Ultrasonography indicators for predicting difficult intubation: A systematic review and meta-analysis. BMC Emerg. Med. 2021, 21, 76. [Google Scholar] [CrossRef]
- Kaminski, A.; Dike, N.O.; Bachista, K.; Boniface, M.; Dove, C.; Simon, L.V. Differences Between Esophageal and Tracheal Intubation Ultrasound View Proficiency: An Educational Study of Novice Prehospital Providers. Cureus 2020, 12, e8686. [Google Scholar] [CrossRef] [PubMed]
- Donovan, J.K.; Burton, S.O.; Jones, S.L.; Phillips, L.M.; Anderson, D.; Meadley, B.N. Use of Point-of-Care Ultrasound by Intensive Care Paramedics to Assess Respiratory Distress in the Out-of-Hospital Environment: A Pilot Study. Prehospital Emerg. Care 2022, 27, 800–806. [Google Scholar] [CrossRef]
- Kreiser, M.A.; Hill, B.; Karki, D.; Wood, E.; Shelton, R.; Peterson, J.; Riccio, J.; Zapata, I.; Khalil, P.A.; Gubler, D.; et al. Point-of-Care Ultrasound Use by EMS Providers in Out-of-Hospital Cardiac Arrest. Prehospital Disaster Med. 2022, 37, 39–44. [Google Scholar] [CrossRef]
- Reed, M.J.; Gibson, L.; Dewar, A.; Short, S.; Black, P.; Clegg, G.R. Introduction of paramedic led Echo in Life Support into the pre-hospital environment: The PUCA study. Resuscitation 2017, 112, 65–69. [Google Scholar] [CrossRef]
- McCallum, J.; Vu, E.; Sweet, D.; Kanji, H.D. Assessment of Paramedic Ultrasound Curricula: A Systematic Review. Air Med. J. 2015, 34, 360–368. [Google Scholar] [CrossRef]
- Donovan, J.K.; Burton, S.O.; Jones, S.L.; Meadley, B.N. Use of Point-of-Care Ultrasound by Non-Physicians to Assess Respiratory Distress in the Out-of-Hospital Environment: A Scoping Review. Prehospital Disaster Med. 2022, 37, 520–528. [Google Scholar] [CrossRef]
- Nadim, G.; Laursen, C.B.; Pietersen, P.I.; Wittrock, D.; Sørensen, M.K.; Nielsen, L.B.; Rasmussen, C.H.; Christensen, H.M.; Helmerik, S.; Jørgensen, G.; et al. Prehospital emergency medical technicians can perform ultrasonography and blood analysis in prehospital evaluation of patients with chronic obstructive pulmonary disease: A feasibility study. BMC Health Serv. Res. 2021, 21, 290. [Google Scholar] [CrossRef]
- Schoeneck, J.H.; Coughlin, R.F.; Baloescu, C.; Cone, D.C.; Liu, R.B.; Kalam, S.; Medoro, A.K.; Medoro, I.; Joseph, D.; Burns, K.; et al. Paramedic-performed Prehospital Point-of-care Ultrasound for Patients with Undifferentiated Dyspnea: A Pilot Study. West. J. Emerg. Med. 2021, 22, 750–755. [Google Scholar] [CrossRef] [PubMed]
- Pietersen, P.I.; Mikkelsen, S.; Lassen, A.T.; Helmerik, S.; Jørgensen, G.; Nadim, G.; Christensen, H.M.; Wittrock, D.; Laursen, C.B. Quality of focused thoracic ultrasound performed by emergency medical technicians and paramedics in a prehospital setting: A feasibility study. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 40. [Google Scholar] [CrossRef]
- Guy, A.; Bryson, A.; Wheeler, S.; McLean, N.; Kanji, H.D. A Blended Prehospital Ultrasound Curriculum for Critical Care Paramedics. Air Med. J. 2019, 38, 426–430. [Google Scholar] [CrossRef] [PubMed]
- Jonck, C.; Weimer, A.M.; Fundel, B.; Heinz, W.; Merkel, D.; Fiedel, H.; Ille, C.; Kloeckner, R.; Buggenhagen, H.; Piepho, T.; et al. Development and evaluation of a point-of-care ultrasound curriculum for paramedics in Germany—A prospective observational study and comparison. BMC Med. Educ. 2024, 24, 811. [Google Scholar] [CrossRef]
- von Elm, E.; Altmann, D.G.; Egger, M.; Pocock, S.C.; Gøtzsche, P.C.; Vandenbroucke, J.P.; für die, S.-I. Das Strengthening the Reporting of Observational Studies in Epidemiology (STROBE-) Statement. Der Internist 2008, 49, 688–693. [Google Scholar] [CrossRef] [PubMed]
- Höhne, E.; Recker, F.; Dietrich, C.F.; Schäfer, V.S. Assessment Methods in Medical Ultrasound Education. Front. Med. 2022, 9, 871957. [Google Scholar] [CrossRef] [PubMed]
- Weimer, J.M.; Rink, M.; Müller, L.; Dirks, K.; Ille, C.; Bozzato, A.; Sproll, C.; Weimer, A.M.; Neubert, C.; Buggenhagen, H.; et al. Development and Integration of DOPS as Formative Tests in Head and Neck Ultrasound Education: Proof of Concept Study for Exploration of Perceptions. Diagnostics 2023, 13, 661. [Google Scholar] [CrossRef]
- DEGUM. Grundkurs Notfallsonografie. Available online: https://www.degum.de/fachgebiete/arbeitskreise/notfallsonografie/kurscurriculum/grundkurs.html (accessed on 24 October 2024).
- Austin, D.R.; Chang, M.G.; Bittner, E.A. Use of Handheld Point-of-Care Ultrasound in Emergency Airway Management. Chest 2021, 159, 1155–1165. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.S. Ultrasonography in the management of the airway. Acta Anaesthesiol. Scand. 2011, 55, 1155–1173. [Google Scholar] [CrossRef]
- Kruger, J.; Dunning, D. Unskilled and unaware of it: How difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J. Pers. Soc. Psychol. 1999, 77, 1121–1134. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: The Exercise of Control; W.H. Freeman: New York, NY, USA, 1997. [Google Scholar]
- Bansbach, J.; Bentele, M.; Bollinger, M.; Bentele, S.; Langenhan, R.; Gerber, B.; Trifunovic-Koenig, M.; Bushuven, S. Self-assessment and learning motivation in emergency point-of-care ultrasound: An online pilot investigation in German physicians. BMC Emerg. Med. 2024, 24, 235. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; Kleinschmidt, S.; Mörsdorf, P.; Conrad, D.; Berwanger, U.; Armbruster, W. Vergleich der präklinischen Analgesiequalität von Notarzt und Notfallsanitäter anhand traumatologischer Patienten. Die Anaesthesiol. 2024, 73, 576–582. [Google Scholar] [CrossRef]
- Bollinger, M.; Russo, S. Notfall- und Rettungsmedizin: Grenzen der Substitution ärztlicher Leistungen durch nichtärztliches Rettungsdienstpersonal. Eine systematische Literaturrecherche zum Erfolg der präklinischen endotrachealen Intubation durch nichtärztliches Rettungsdienstpersonal und Notärzte. Notfall + Rettungsmedizin 2023, 27, 385–392. [Google Scholar] [CrossRef]
- Zasso, F.B.; You-Ten, K.E.; Ryu, M.; Losyeva, K.; Tanwani, J.; Siddiqui, N. Complications of cricothyroidotomy versus tracheostomy in emergency surgical airway management: A systematic review. BMC Anesthesiol. 2020, 20, 216. [Google Scholar] [CrossRef] [PubMed]
- Weimer, J.M.; Recker, F.; Horn, L.; Kuenzel, J.; Dirks, K.; Ille, C.; Buggenhagen, H.; Börner, N.; Weimer, A.M.; Vieth, T.; et al. Insights Into Modern Undergraduate Ultrasound Education: Prospective Comparison of Digital and Analog Teaching Resources in a Flipped Classroom Concept—The DIvAN Study. Ultrasound Int. Open 2024, 10, a23899410. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.B.; Cantisani, V.; Sidhu, P.S.; Badea, R.; Batko, T.; Carlsen, J.; Claudon, M.; Ewertsen, C.; Garre, C.; Genov, J.; et al. The Use of Handheld Ultrasound Devices—An EFSUMB Position Paper. Ultraschall Med. 2019, 40, e1. [Google Scholar] [CrossRef]
- Shi, R.; Rosario, J. Paramedic-Performed Prehospital Tele-Ultrasound: A Powerful Technology or an Impractical Endeavor? A Scoping Review. Prehospital Disaster Med. 2023, 38, 645–653. [Google Scholar] [CrossRef]
- Uschnig, C.; Recker, F.; Blaivas, M.; Dong, Y.; Dietrich, C.F. Tele-ultrasound in the Era of COVID-19: A Practical Guide. Ultrasound Med. Biol. 2022, 48, 965–974. [Google Scholar] [CrossRef]
- Weimer, J.M.; Widmer, N.; Strelow, K.-U.; Hopf, P.; Buggenhagen, H.; Dirks, K.; Künzel, J.; Börner, N.; Weimer, A.M.; Lorenz, L.A.; et al. Long-Term Effectiveness and Sustainability of Integrating Peer-Assisted Ultrasound Courses into Medical School—A Prospective Study. Tomography 2023, 9, 1315–1328. [Google Scholar] [CrossRef]
- March, J.A.; Kiemeney, M.J.; De Guzman, J.; Ferguson, J.D. Retention of cricothyrotomy skills by paramedics using a wire guided technique. Am. J. Emerg. Med. 2019, 37, 407–410. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weimer, J.; Chrissostomou, C.D.; Jonck, C.; Weimer, A.M.; Ille, C.; Müller, L.; Lorenz, L.A.; Stäuber, M.; Vieth, T.; Buggenhagen, H.; et al. Paramedics Performed Sonographic Identification of the Conic Ligament—A Prospective Controlled Trial. Diagnostics 2025, 15, 1296. https://doi.org/10.3390/diagnostics15101296
Weimer J, Chrissostomou CD, Jonck C, Weimer AM, Ille C, Müller L, Lorenz LA, Stäuber M, Vieth T, Buggenhagen H, et al. Paramedics Performed Sonographic Identification of the Conic Ligament—A Prospective Controlled Trial. Diagnostics. 2025; 15(10):1296. https://doi.org/10.3390/diagnostics15101296
Chicago/Turabian StyleWeimer, Johannes, Christopher David Chrissostomou, Christopher Jonck, Andreas Michael Weimer, Carlotta Ille, Lukas Müller, Liv Annebritt Lorenz, Marie Stäuber, Thomas Vieth, Holger Buggenhagen, and et al. 2025. "Paramedics Performed Sonographic Identification of the Conic Ligament—A Prospective Controlled Trial" Diagnostics 15, no. 10: 1296. https://doi.org/10.3390/diagnostics15101296
APA StyleWeimer, J., Chrissostomou, C. D., Jonck, C., Weimer, A. M., Ille, C., Müller, L., Lorenz, L. A., Stäuber, M., Vieth, T., Buggenhagen, H., Weinmann-Menke, J., Rink, M., & Künzel, J. (2025). Paramedics Performed Sonographic Identification of the Conic Ligament—A Prospective Controlled Trial. Diagnostics, 15(10), 1296. https://doi.org/10.3390/diagnostics15101296






