Comparison of SD Bioline Malaria Ag Pf/Pan and Acro Malaria P.f./P.v./Pan with Microscopy and Real Time PCR for the Diagnosis of Human Plasmodium Species
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. Malaria Diagnosis Using Microscopy
2.3. Malaria Diagnosis by RDTs
2.4. Malaria Diagnosis by Real Time PCR
2.5. Statistical Analysis
- Sensitivity = TP/(TP + FN), proportion of samples with the malaria species correctly identified.
- Specificity = TN/(FP + TN), proportion of samples without the malaria species correctly identified.
3. Results
3.1. Microscopy
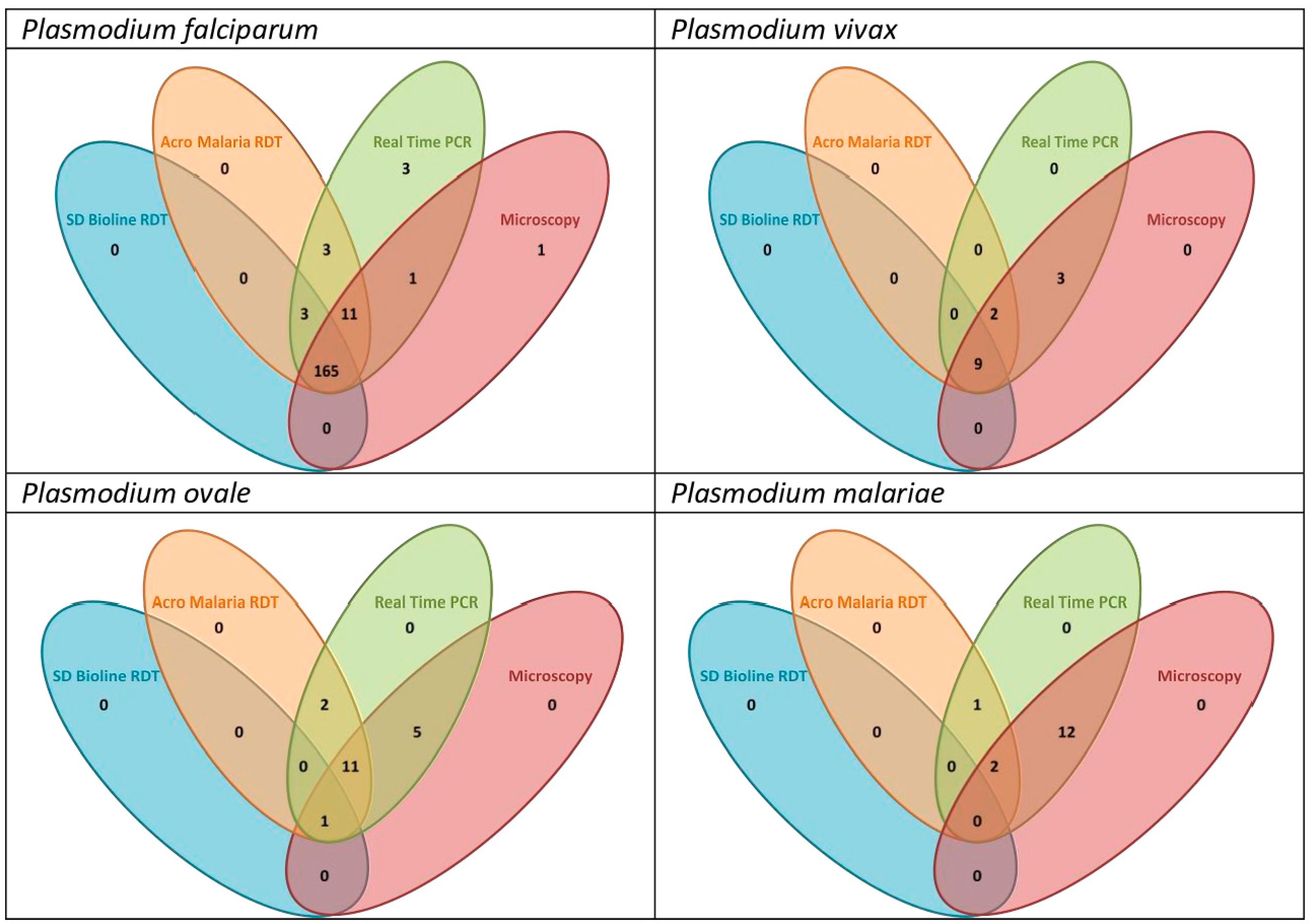
3.2. Comparison of Malaria RDTs
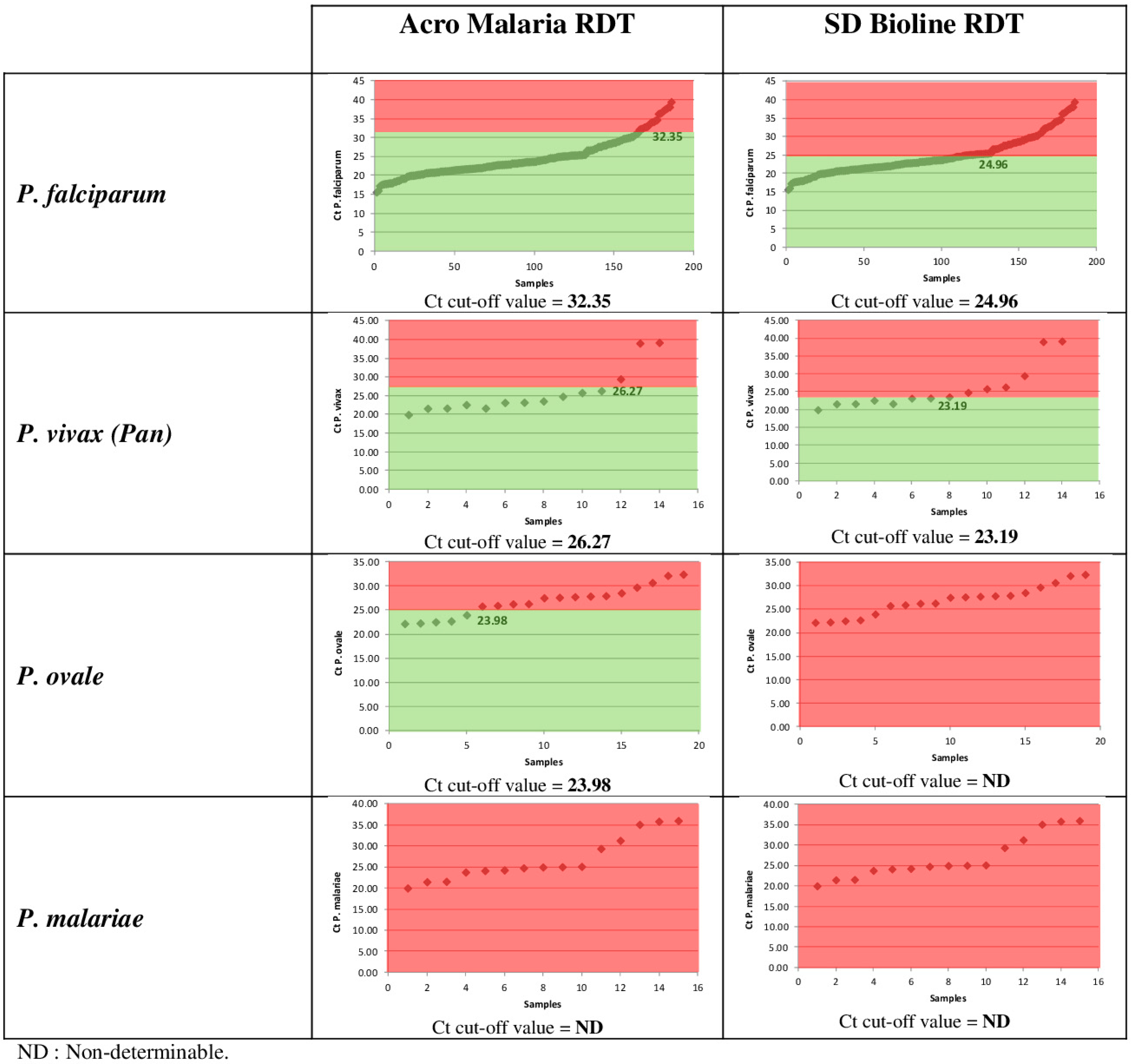
3.3. Performance of Malaria RDTs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Malaria Report 2023; World Health Organization: Geneva, Switzerland, 2023. Available online: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2023 (accessed on 15 February 2024).
- Wangdi, K.; Wetzler, E.; Cox, H.; Marchesini, P.; Villegas, L.; Canavati, S. Spatial patterns and climate drivers of malaria in three border areas of Brazil, Venezuela and Guyana, 2016–2018. Sci. Rep. 2022, 12, 10995. [Google Scholar] [CrossRef] [PubMed]
- Hawadak, J.; Dongang Nana, R.R.; Singh, V. Global trend of Plasmodium malariae and Plasmodium ovale spp. malaria infections in the last two decades (2000–2020): A systematic review and meta-analysis. Parasit. Vectors 2021, 14, 297. [Google Scholar] [CrossRef] [PubMed]
- Sendor, R.; Banek, K.; Kashamuka, M.M.; Mvuama, N.; Bala, J.A.; Nkalani, M.; Kihuma, G.; Atibu, J.; Thwai, K.L.; Svec, W.M.; et al. Epidemiology of Plasmodium malariae and Plasmodium ovale spp. in Kinshasa Province, Democratic Republic of Congo. Nat. Commun. 2023, 14, 6618. [Google Scholar] [CrossRef] [PubMed]
- Jeyaprakasam, N.K.; Liew, J.W.K.; Low, V.L.; Wan-Sulaiman, W.Y.; Vythilingam, I. Plasmodium knowlesi infecting humans in Southeast Asia: What’s next? PLoS Negl. Trop. Dis. 2020, 14, e0008900. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Malaria Annual Epidemiological Report for 2021; ECDC: Stockholm, Sweden, 2023; Available online: https://www.ecdc.europa.eu/en/publications-data/malaria-annual-epidemiological-report-2021 (accessed on 15 February 2024).
- Mosnier, E.; Roux, E.; Cropet, C.; Lazrek, Y.; Moriceau, O.; Gaillet, M.; Mathieu, L.; Nacher, M.; Demar, M.; Odonne, G.; et al. Prevalence of Plasmodium spp. in the Amazonian border context (French Guiana-Brazil): Associated factors and spatial distribution. Am. J. Trop. Med. Hyg. 2020, 102, 130–141. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Malaria Rapid Diagnostic Test Performance. In Results of WHO Product Testing of Malaria RDTs: Round 8 (2016–2018); World Health Organization, Geneva, Switzerland. 2018. Available online: https://www.who.int/publications/i/item/9789241514965 (accessed on 15 February 2024).
- World Health Organization. Response Plan to pfhrp2 Gene Deletions; World Health Organization: Geneva, Switzerland, 2019. Available online: https://www.who.int/publications/i/item/WHO-CDS-GMP-2019.02 (accessed on 15 February 2024).
- Wurtz, N.; Mint Lekweiry, K.; Bogreau, H.; Pradines, B.; Rogier, C.; Ould Mohamed Salem Boukhary, A.; Hafid, J.E.; Ould Ahmedou Salem, M.S.; Trape, J.F.; Basco, L.K.; et al. Vivax malaria in Mauritania includes infection of a Duffy-negative individual. Malar. J. 2011, 10, 336. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Newcombe, R.G. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat. Med. 1998, 17, 857–872. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Yimam, Y.; Mohebali, M.; Abbaszadeh Afshar, M.J. Comparison of diagnostic performance between conventional and ultrasensitive rapid diagnostic tests for diagnosis of malaria: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0263770. [Google Scholar] [CrossRef]
- Kavanaugh, M.J.; Azzam, S.E.; Rockabrand, D.M. Malaria rapid diagnostic tests: Literary review and recommendation for a quality assurance, quality control algorithm. Diagnostics 2021, 11, 768. [Google Scholar] [CrossRef]
- Wu, J.; Tang, J.; Wang, W.; Chen, G.; He, X.; Xu, S.; Cao, Y.; Gu, Y.; Zhu, G.; Cao, J. Poor performance of malaria rapid diagnostic tests for the detection of Plasmodium malariae among returned international travellers in China. Malar. J. 2023, 22, 163. [Google Scholar] [CrossRef] [PubMed]
- De Laval, F.; Simon, F.; Bogreau, H.; Rapp, C.; Wurtz, N.; Oliver, M.; Demaison, X.; Dia, A.; De Pina, J.J.; Merens, A.; et al. Emergence of Plasmodium ovale malaria among the French Armed Forces in the Republic of Ivory Coast: 20 years of clinical and biological experience. Clin. Infect. Dis. 2014, 58, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Manego, R.Z.; Mombo-Ngoma, G.; Witte, M.; Held, J.; Gmeiner, M.; Gebru, T.; Tazemda, B.; Mischlinger, J.; Groger, M.; Lell, A.A.; et al. Demography, maternal health and the epidemiology of malaria and other major infectious diseases in the rural department Tsamba-Magotsi, Ngounie Province, in central African Gabon. BMC Public Health 2017, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- Roucher, C.; Rogier, C.; Sokhna, C.; Tall, A.; Trape, J.F. A 20-year longitudinal study of Plasmodium ovale and Plasmodium malariae prevalence and morbidity in a West African population. PLoS ONE 2014, 9, e87169. [Google Scholar] [CrossRef] [PubMed]
- Velut, G.; Dia, A.; Briolant, S.; Javelle, E.; Pommier de Santi, V.; Berger, F.; Savini, H.; Simon, F.; Michel, R.; Pradines, B. Le paludisme: Toujours d’actualité dans les armées françaises. Med. Armées 2018, 46, 13–26. [Google Scholar]
- Thellier, M.; Simard, F.; Musset, L.; Cot, M.; Velut, G.; Kendjo, E.; Pradines, B. Evolution épidémiologique du paludisme eu niveau mondial et national, 2000–2015. Med. Mal. Infect. 2020, 50, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Ginouves, M.; Veron, V.; Musset, L.; Legrand, E.; Stefani, A.; Prevot, G.; Demar, M.; Djossou, F.; Brousse, P.; Nacher, M.; et al. Frequency and distribution of mixed Plasmodium falciparum-vivax infections in French Guiana between 2000 and 2008. Malar. J. 2015, 14, 446. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, R.; Choi, L.; Johnson, S.; Takwoingi, Y. Rapid diagnostic tests for Plasmodium vivax malaria in endemic countries. Cochrane Database Syst; Rev. 2020, 11, CD013218. [Google Scholar] [CrossRef]
- Oulton, T.; Mahamar, A.; Sanogo, K.; Diallo, M.; Youssouf, A.; Niambele, S.M.; Samaké, S.; Keita, S.; Sinaba, Y.; Sacko, A.; et al. Persistence of Plasmodium falciparum HRP-2 antigenaemia after artemisinin combination therapy is not associated with gametocytes. Malar. J. 2022, 21, 372. [Google Scholar] [CrossRef]
- Nana, R.R.D.; Ngum, N.L.; Makoge, V.; Amvongo-Adja, N.; Hawadak, J.; Singh, V. Rapid diagnostic tests for malaria diagnosis in Cameroon: Impact of histidine rich protein 2/3 deletions and lactate dehydrogenase gene polymorphism. Diagn. Microbiol. Infect. Dis. 2024, 108, 116103. [Google Scholar] [CrossRef]
- Krueger, T.; Ikegbunam, M.; Lissom, A.; Sandri, T.L.; Ntabi JD, M.; Djontu, J.C.; Kreidenweiss, A. Low prevalence of Plasmodium falciparum histidine-rich protein 2 and 3 gene deletions-A multiregional study in Central and West Africa. Pathogens 2023, 12, 455. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. False-Negative RDT Results and Implications of New Reports of P. Falciparum Histidine-Rich Protein 2/3 Gene Deletions; WHO reference no.WHO/HTM/GMP/2017.18; World Health Organization: Geneva, Switzerland, 2017.
- Nyataya, J.; Waitumbi, J.; Mobegi, V.A.; Noreddin, A.; El Zowalaty, M.E. Plasmodium falciparum Histidine-Rich Protein 2 and 3 gene deletions and their implications in malaria Control. Diseases 2020, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- Golassa, L.; Messele, A.; Amambua-Ngwa, A.; Swedberg, G. High prevalence and extended deletions in Plasmodium falciparum hrp2/3 genomic loci in Ethiopia. PLoS ONE 2020, 15, e0241807. [Google Scholar] [CrossRef]
- Wurtz, N.; Fall, B.; Bui, K.; Pascual, A.; Fall, M.; Camara, C.; Diatta, B.; Fall, K.B.; Mbaye, P.S.; Diémé, Y.; et al. Pfhrp2 and pfhrp3 polymorphisms in Plasmodium falciparum isolates from Dakar, Senegal: Impact on rapid malaria diagnostic tests. Malar. J. 2013, 12, 34. [Google Scholar] [CrossRef]
- Gendrot, M.; Fawaz, R.; Dormoi, J.; Madamet, M.; Pradines, B. Genetic diversity and deletion of Plasmodium falciparum histidine-rich protein 2 and 3: A threat to diagnosis of P. falciparum malaria. Clin. Microbiol. Infect. 2019, 25, 580–585. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not those of affiliated organizations or those of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
| Malaria Diagnosis | P. falciparum | P. vivax | P. ovale | P. malariae | Non-Identified Infections a | Negative |
|---|---|---|---|---|---|---|
| Microscopy | 166 | 11 | 12 | 8 | 14 | 18 |
| Real time PCR | 174 | 11 | 14 | 9 | 13 | 8 |
| Malaria Diagnosis | P. falciparum a | P. vivax a | P. ovale a | P. malariae a | Negative |
|---|---|---|---|---|---|
| Real-time PCR | 186 | 14 | 19 | 15 | 8 |
| ACRO MALARIA RDT | 180 | 11 | 14 | 3 | 34 |
| SD BIOLINE RDT | 167 | 9 | 1 | 0 | 65 |
| RDTs | Specific Antigen | Parasitemia Category (%) | Negative-RDT | False-Negative | False-Positive | |||
|---|---|---|---|---|---|---|---|---|
| 0.001 ≤ p < 0.01 | 0.01 ≤ p < 0.1 | 0.1 ≤ p < 1 | p ≥ 1 | |||||
| ACRO RDT | PfHRP2 (n = 186) | 20 | 42 | 70 | 48 | 6 | 4 | 3 |
| PvLDH (n = 14) | 0 | 5 | 6 | 0 | 3 | 1 | 0 | |
| panLDH (n = 229) | 4 | 28 | 71 | 47 | 79 | 13 | 0 | |
| SD RDT | PfHRP2 (n = 186) | 12 | 38 | 69 | 48 | 19 | 18 | 2 |
| panLDH (n = 229) | 2 | 12 | 45 | 46 | 124 | 26 | 0 | |
| Plasmodium Species | Sensitivity a Acro Malaria RDT | Specificity b Acro Malaria RDT | PPV c Acro Malaria RDT | NPV d Acro Malaria RDT | Sensitivity a SD Bioline RDT | Specificity b SD Bioline RDT | PPV c SD Bioline RDT | NPV d SD Bioline RDT |
|---|---|---|---|---|---|---|---|---|
| P. falciparum (n = 186) | 96.8% | 90.7% | 97.3% | 86.7% | 89.8% | 95.3% | 98.8% | 68.3% |
| P. vivax (n = 14) | 78.6% | 100.0% | 100% | 98.6% | 64.3% | ND | ND | ND |
| P. ovale (n = 19) | 73.7% | ND | ND | ND | 5.3% | ND | ND | ND |
| P. malariae (n = 15) | 20.0% | ND | ND | ND | 0% | ND | ND | ND |
| Plasmodium | 69.2% | 100.0% | 100% | 10.5% | 47.5% | 100.0% | 100% | 6.5% |
| RDTs | Species | Cycle Threshold Category | ||
|---|---|---|---|---|
| Sensitivity at Ct < 25 | Sensitivity at Ct 25–30 | Sensitivity at Ct > 30 | ||
| ACRO RDT | P. falciparum (n = 186) | 100 | 100 | 73.9 |
| P. vivax (Pv) (n = 14) | 100 | 66.7 | 0 | |
| P. vivax (Pan) (n = 14) | 88.9 | 66.7 | 50 | |
| P. ovale (n = 19) | 100 | 72.7 | 33.3 | |
| P. malariae (n = 15) | 12.5 | 0 | 50 | |
| SD RDT | P. falciparum (n = 186) | 99.1 | 85.1 | 52.2 |
| P. vivax (Pan) (n = 14) | 88.9 | 33.3 | 0 | |
| P. ovale (n = 19) | 20 | 0 | 0 | |
| P. malariae (n = 15) | 0 | 0 | 0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Madamet, M.; Fonta, I.; Mosnier, J.; Benoit, N.; Amalvict, R.; Briolant, S.; French National Reference Centre for Imported Malaria Study Group; Pradines, B. Comparison of SD Bioline Malaria Ag Pf/Pan and Acro Malaria P.f./P.v./Pan with Microscopy and Real Time PCR for the Diagnosis of Human Plasmodium Species. Diagnostics 2024, 14, 721. https://doi.org/10.3390/diagnostics14070721
Madamet M, Fonta I, Mosnier J, Benoit N, Amalvict R, Briolant S, French National Reference Centre for Imported Malaria Study Group, Pradines B. Comparison of SD Bioline Malaria Ag Pf/Pan and Acro Malaria P.f./P.v./Pan with Microscopy and Real Time PCR for the Diagnosis of Human Plasmodium Species. Diagnostics. 2024; 14(7):721. https://doi.org/10.3390/diagnostics14070721
Chicago/Turabian StyleMadamet, Marylin, Isabelle Fonta, Joel Mosnier, Nicolas Benoit, Rémy Amalvict, Sébastien Briolant, French National Reference Centre for Imported Malaria Study Group, and Bruno Pradines. 2024. "Comparison of SD Bioline Malaria Ag Pf/Pan and Acro Malaria P.f./P.v./Pan with Microscopy and Real Time PCR for the Diagnosis of Human Plasmodium Species" Diagnostics 14, no. 7: 721. https://doi.org/10.3390/diagnostics14070721
APA StyleMadamet, M., Fonta, I., Mosnier, J., Benoit, N., Amalvict, R., Briolant, S., French National Reference Centre for Imported Malaria Study Group, & Pradines, B. (2024). Comparison of SD Bioline Malaria Ag Pf/Pan and Acro Malaria P.f./P.v./Pan with Microscopy and Real Time PCR for the Diagnosis of Human Plasmodium Species. Diagnostics, 14(7), 721. https://doi.org/10.3390/diagnostics14070721






