Evaluation of the Diagnostic Performances of the SD-Bioline®HBeAg Rapid Test Used Routinely for the Management of HBV-Infected Individuals in Burkina Faso
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. SD-Bioline®HBeAg RDT
2.3. Gold Standard: VIDAS HBe/Anti-HBe (ELFA)
2.4. Quantification of HBV Viral DNA
2.5. Statistical Analysis
2.6. Ethical Approval
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- OMS. Interim Guidance for Country Validation of Viral Hepatitis Elimination; Technical Report; WHO: Geneva, Switzerland, 2021; p. 96. [Google Scholar]
- Word Health Organization. Global Progress Report on HIV, Viral Hepatitis and Sexually Transmitted Infections, 2021. 2021. Available online: https://www.who.int/publications-detail-redirect/9789240027077 (accessed on 16 February 2023).
- Chang, M.L.; Liaw, Y.F. Hepatitis B Flare in Hepatitis B e Antigen-Negative Patients: A Complicated Cascade of Innate and Adaptive Immune Responses. Int. J. Mol. Sci. 2022, 23, 1552. [Google Scholar] [CrossRef] [PubMed]
- Lemoine, M.; Thursz, M.R. Battlefield against hepatitis B infection and HCC in Africa. J. Hepatol. 2017, 66, 645–654. [Google Scholar] [CrossRef]
- Sheena, B.S.; Hiebert, L.; Han, H.; Ippolito, H.; Abbasi-Kangevari, M.; Abbasi-Kangevari, Z.; Abbastabar, H.; Abdoli, A.; Ali, H.A.; Adane, M.M.; et al. Global, regional, and national burden of hepatitis B, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 2022, 7, 796–829. [Google Scholar] [CrossRef]
- Stockdale, A.J.; Silungwe, N.M.; Shawa, I.T.; Kreuels, B.; Gordon, M.A.; Geretti, A.M. Diagnostic performance evaluation of hepatitis B e antigen rapid diagnostic tests in Malawi. BMC Infect. Dis. 2021, 21, 487. [Google Scholar] [CrossRef] [PubMed]
- Clement, F.; Dewint, P.; Leroux-Roels, G. Evaluation of a New Rapid Test for the Combined Detection of Hepatitis B Virus Surface Antigen and Hepatitis B Virus e Antigen. J. Clin. Microbiol. 2002, 40, 4603–4606. [Google Scholar] [CrossRef] [PubMed]
- Stoeckl, L.; Funk, A.; Kopitzki, A.; Brandenburg, B.; Oess, S.; Will, H.; Sirma, H.; Hildt, E. Identification of a structural motif crucial for infectivity of hepatitis B viruses. Proc. Natl. Acad. Sci. USA 2006, 103, 6730–6734. [Google Scholar] [CrossRef] [PubMed]
- Seck, A.; Ndiaye, F.; Maylin, S.; Ndiaye, B.; Simon, F.; Funk, A.; Fontanet, A.; Takahashi, K.; Akbar, S.M.F.; Mishiro, S.; et al. Poor Sensitivity of Commercial Rapid Diagnostic Tests for Hepatitis B e Antigen in Senegal, West Africa. Am. J. Trop. Med. Hyg. 2018, 99, 428–434. [Google Scholar] [CrossRef]
- Sanou, A.M.; Toyé, R.; Kagoné, T.; Nikiéma, A.; Testa, J.; Sakandé, J.; Sangaré, L.; Tarnagda, Z.; Kania, D. Analytical performance of eight rapid point-of-care tests routinely used for the detection of HBsAg in Burkina Faso: A cross-sectional study. J. Clin. Virol. 2020, 129, 104546. [Google Scholar] [CrossRef]
- Sanou, A.M.; Nikièma, A.S.; Zalla, S.; Ouattara, M.; Dakouo, N.P.S.; Kiba-Koumare, A.; Seynou, M.; Napon-Zongo, D.; Sombié, R. Residual risk of hepatitis B virus transmission through blood donations in Burkina Faso screened with rapid diagnostic tests. Heal. Sci. Rep. 2022, 5, e748. [Google Scholar] [CrossRef]
- Meda, N.; Tuaillon, E.; Kania, D.; Tiendrebeogo, A.; Pisoni, A.; Zida, S.; Bollore, K.; Medah, I.; Laureillard, D.; Moles, J.P.; et al. Hepatitis B and C virus seroprevalence, Burkina Faso: A cross-sectional study. Bull. World Health Organ. 2018, 96, 750–759. [Google Scholar] [CrossRef]
- Lingani, M.; Akita, T.; Ouoba, S.; Sanou, A.M.; Sugiyama, A.; Tarnagda, Z.; Ohisa, M.; Tinto, H.; Mishiro, S.; Tanaka, J. High prevalence of hepatitis B infections in Burkina Faso (1996–2017): A systematic review with meta-analysis of epidemiological studies. BMC Public Health 2018, 18, 1–11. [Google Scholar] [CrossRef]
- Ministère de la Santé. Normes et Protocoles de Prise en Charge des Hépatites Virales au Burkina Faso; Institut National de Santé Publique: Ouagadougou, Burkina Faso, 2019; Available online: https://insp.bf/wp-content/uploads/2023/06/Normes-et-protocoles-de-Prise-en-charge-HV-au-BF-Vf-2019.pdf (accessed on 16 February 2023).
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Ségéral, O.S.; N’Diaye, D.; Prak, S.; Nouhin, J.; Chhun, S.; Khamduang, W.; Chim, K.; Roque-Afonso, A.M.; Piola, P.; Borand, L.; et al. Usefulness of a serial algorithm of HBsAg and HBeAg rapid diagnosis tests to detect pregnant women at risk of HBV mother-to-child transmission in Cambodia, the ANRS 12328 pilot study. J. Clin. Virol. 2018, 109, 29–34. [Google Scholar] [CrossRef]
- Knipe, D.M.; Howley, P.M.; Griffin, D.E.; Lamb, R.A.; Martin, M.A.; Roizman, B.; Straus, S.E. (Eds.) Fields’ Virology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006; ISBN-13: 978-0-7817-6060-7. [Google Scholar]
- Ouneissa, R.; Bahri, O.; Alaya-Bouafif, N.B.; Chouaieb, S.; Yahia, A.B.; Sadraoui, A.; Hammami, W.; Filali, N.; Azzouz, M.M.; Ben Mami, N.; et al. Frequency and clinical significance of core promoter and precore region mutations in Tunisian patients infected chronically with hepatitis B. J. Med. Virol. 2012, 84, 1719–1726. [Google Scholar] [CrossRef]
- Kramvis, A.; Arakawa, K.; Yu, M.C.; Nogueira, R.; Stram, D.O.; Kew, M.C. Relationship of serological subtype, basic core promoter and precore mutations to genotypes/subgenotypes of hepatitis B virus. J. Med. Virol. 2008, 80, 27–46. [Google Scholar] [CrossRef]
- Besharat, S.; Poustchi, H.; Mohamadkhani, A.; Katoonizadeh, A.; Moradi, A.; Roshandel, G.; Freedman, N.D.; Malekzadeh, R. Association of Mutations in the Basal Core Promoter and Pre-core Regions of the Hepatitis B Viral Genome and Longitudinal Changes in HBV Level in HBeAg Negative Individuals: Results from a Cohort Study in Northern Iran. Hepat. Mon. 2015, 15, e23875. [Google Scholar] [CrossRef]
- Jammeh, S.; Tavner, F.; Watson, R.; Thomas, H.C.; Karayiannis, P. Effect of basal core promoter and pre-core mutations on hepatitis B virus replication. J. Gen. Virol. 2008, 89, 901–909. [Google Scholar] [CrossRef]
- Pivert, A.; Servant-Delmas, A.; Lunel-Fabiani, F.; Le Guillou-Guillemette, H.; Laperche, S.; Ducancelle, A. Correlation between the promoter basal core and precore mutations and HBsAg quantification in French blood donors infected with hepatitis B virus: HBV in French Blood Donors. J. Med. Virol. 2015, 87, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Boucheron, P.; Lu, Y.; Yoshida, K.; Zhao, T.; Funk, A.L.; Lunel-Fabiani, F.; Guingané, A.; Tuaillon, E.; van Holten, J.; Chou, R.; et al. Accuracy of HBeAg to identify pregnant women at risk of transmitting hepatitis B virus to their neonates: A systematic review and meta-analysis. Lancet Infect. Dis. 2020, 21, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Johannessen, A.; Mekasha, B.; Desalegn, H.; Aberra, H.; Stene-Johansen, K.; Berhe, N. Mother-to-Child Transmission of Hepatitis B Virus in Ethiopia. Vaccines 2021, 9, 430. [Google Scholar] [CrossRef] [PubMed]
- OMS. Guidelines for the Prevention, Care and Treatment of Persons with Chronic Hepatitis B Infection; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Lee, J.H.; Hong, S.P.; Jang, E.S.; Park, S.J.; Hwang, S.G.; Kang, S.-K.; Jeong, S.-H. Analysis of HBV genotype, drug resistant mutations, and pre-core/basal core promoter mutations in Korean patients with acute hepatitis B. J. Med. Virol. 2015, 87, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Lau, K.C.K.; Joshi, S.S.; Mahoney, D.J.; Mason, A.L.; van Marle, G.; Osiowy, C.; Coffin, C.S. Differences in HBV Replication, APOBEC3 Family Expression, and Inflammatory Cytokine Levels Between Wild-Type HBV and Pre-core (G1896A) or Basal Core Promoter (A1762T/G1764A) Mutants. Front. Microbiol. 2020, 11, 1653. [Google Scholar] [CrossRef] [PubMed]
- Bhukya, P.L.; Vignesh, K.C.; Lole, K.S. Transcriptome analysis of hepatoma cells transfected with Basal Core Promoter (BCP) and Pre-Core (PC) mutant hepatitis B virus full genome construct. J. Gen. Virol. 2021, 102, 001568. [Google Scholar] [CrossRef] [PubMed]
- Somé, E.N.; Guingané, A.N.; Zongo, I.; Sané, D.; Drabo, K.M.; Sombié, R. Chronic viral HBeAg-negative hepatitis B: Epidemiological, clinical and biochemical characteristics in an outpatient descriptive cohort in Burkina Faso. Clin. Epidemiol. Glob. Health 2021, 11, 100799. [Google Scholar] [CrossRef]
| Results | VIDAS HBe/Anti-HBe | |||
|---|---|---|---|---|
| SD-Bioline®HBeAg RDT | Positive (%) | Negative (%) | Total | |
| Positive | 12 | 4 | 16 | |
| Negative | 24 | 300 | 324 | |
| Total | 36 | 304 | 340 | |
| Performance Parameters | SD-Bioline®HBeAg RDT | |
|---|---|---|
| Estimate (%) | 95% CI | |
| Se | 33.3 | 18.5–50.9 |
| Sp | 98.6 | 96.6–99.6 |
| VPP | 75.0 | 47.6–92.7 |
| VPN | 92.5 | 89.1–95.1 |
| Kappa | 0.42 | 0.25–0.59 |
| Viral Load | SD-Bioline®HbeAg RDT | |||
|---|---|---|---|---|
| Positive | Negative | Total | ||
| VL ≥ 3.3 log10 UI/mL (VL ≥ 2000 UI/mL) | ≥3.3 log10 UI/mL | 14 | 145 | 159 |
| <3.3 log10 UI/mL | 2 | 179 | 181 | |
| Total | 16 | 324 | 340 | |
| VL ≥ 4.3 log10 UI/mL (VL ≥ 20,000 UI/mL) | ≥4.3 log10 UI/mL | 13 | 53 | 66 |
| <4.3 log10 UI/mL | 3 | 271 | 274 | |
| Total | 16 | 324 | 340 | |
| VL ≥ 5.3 log10 UI/mL (VL ≥ 200,000 UI/mL) | ≥5.3 log10 UI/mL | 11 | 28 | 39 |
| <5.3 log10 UI/mL | 5 | 296 | 301 | |
| Total | 16 | 324 | 340 | |
| VL ≥ 6.3 log10 UI/mL (VL ≥ 2,000,000 UI/mL) | ≥6.3 log10 UI/mL | 11 | 20 | 31 |
| <6.3 log10 UI/mL | 5 | 304 | 309 | |
| Total | 16 | 324 | 340 | |
| Viral Load | SD-Bioline®HBeAg RDT | |||||||
|---|---|---|---|---|---|---|---|---|
| Se | Sp | VPP * | VPN ** | |||||
| Estimate (%) | 95% CI | Estimate (%) | 95% CI | Estimate (%) | 95% CI | Estimate (%) | 95% CI | |
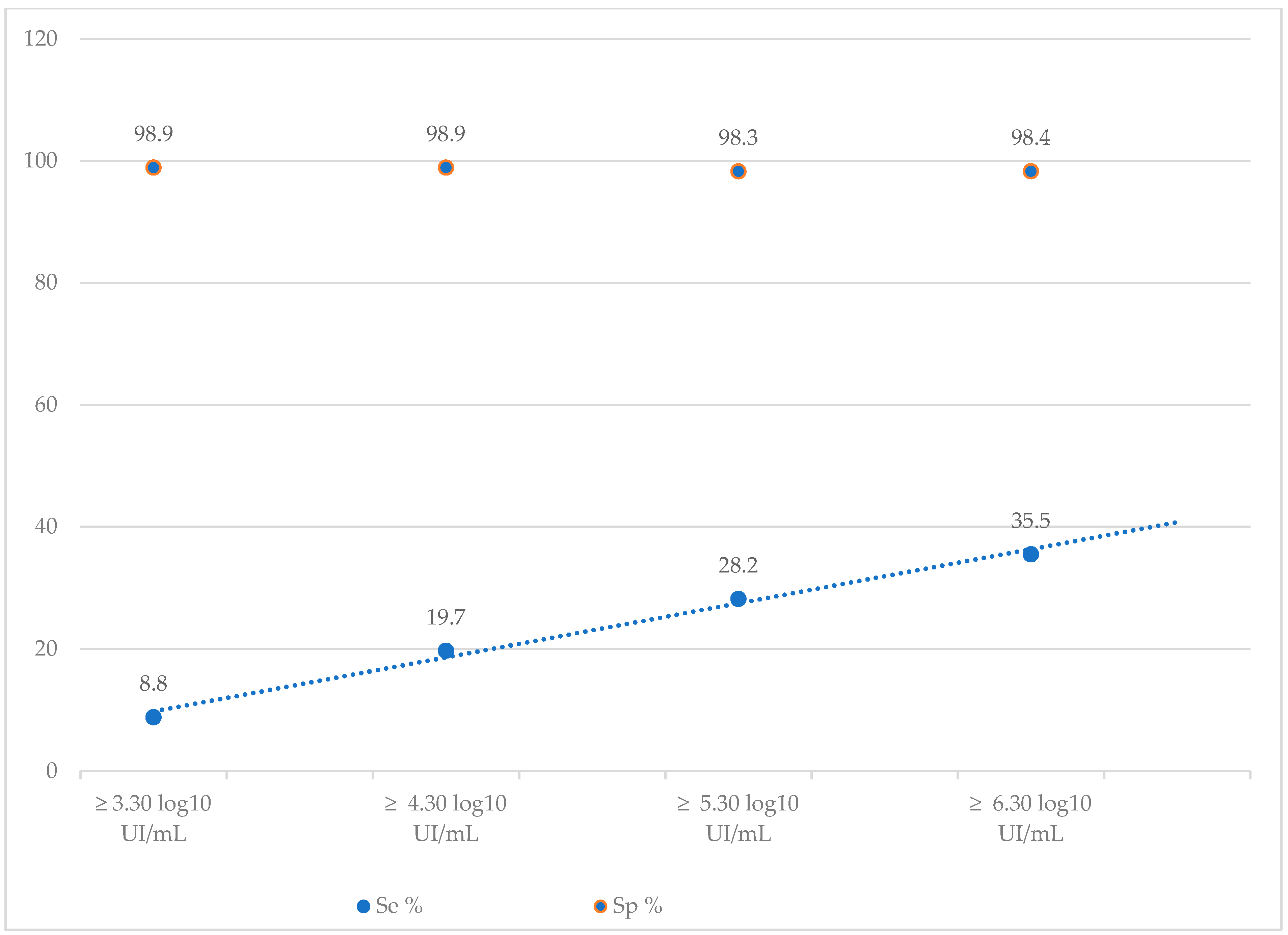
| VL ≥ 3.3 log10 UI/mL (VL ≥ 2000 UI/mL) | 8.8 | 4.9–14.3 | 98.9 | 96.1–99.9 | 87.5 | 61.6–98.4 | 55.2 | 49.6–60.7 |
| VL ≥ 4.3 log10 UI/mL (VL ≥ 20,000 UI/mL) | 19.7 | 10.9–31.3 | 98.9 | 96.7–99.7 | 81.3 | 54.3–95.9 | 83.6 | 79.1–87.7 |
| VL ≥ 5.3 log10 UI/mL (VL ≥ 200,000 UI/mL) | 28.2 | 15.0–44.9 | 98.3 | 96.2–99.4 | 68.8 | 41.3–89.0 | 91.4 | 87.7–94.2 |
| VL ≥ 6.3 log10 UI/mL (VL ≥ 2,000,000 UI/mL) | 35.5 | 19.2–54.6 | 98.4 | 96.3–99.5 | 68.8 | 41.3–89.0 | 93.8 | 90.2–95.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dera, A.; Sanou, A.M.; Ouattara, M.N.G.; Ilboudo, A.K.; Lankoande, D.B.; Ilboudo, D.; Napon-Zongo, D.; Gomgnimbou, M.K. Evaluation of the Diagnostic Performances of the SD-Bioline®HBeAg Rapid Test Used Routinely for the Management of HBV-Infected Individuals in Burkina Faso. Diagnostics 2023, 13, 3144. https://doi.org/10.3390/diagnostics13193144
Dera A, Sanou AM, Ouattara MNG, Ilboudo AK, Lankoande DB, Ilboudo D, Napon-Zongo D, Gomgnimbou MK. Evaluation of the Diagnostic Performances of the SD-Bioline®HBeAg Rapid Test Used Routinely for the Management of HBV-Infected Individuals in Burkina Faso. Diagnostics. 2023; 13(19):3144. https://doi.org/10.3390/diagnostics13193144
Chicago/Turabian StyleDera, Abdoulaye, Armel M. Sanou, Mathuola N. G. Ouattara, Abdoul K. Ilboudo, David B. Lankoande, Dieudonné Ilboudo, Delphine Napon-Zongo, and Michel K. Gomgnimbou. 2023. "Evaluation of the Diagnostic Performances of the SD-Bioline®HBeAg Rapid Test Used Routinely for the Management of HBV-Infected Individuals in Burkina Faso" Diagnostics 13, no. 19: 3144. https://doi.org/10.3390/diagnostics13193144
APA StyleDera, A., Sanou, A. M., Ouattara, M. N. G., Ilboudo, A. K., Lankoande, D. B., Ilboudo, D., Napon-Zongo, D., & Gomgnimbou, M. K. (2023). Evaluation of the Diagnostic Performances of the SD-Bioline®HBeAg Rapid Test Used Routinely for the Management of HBV-Infected Individuals in Burkina Faso. Diagnostics, 13(19), 3144. https://doi.org/10.3390/diagnostics13193144





