Opportunities and Advances in Radiomics and Radiogenomics for Pediatric Medulloblastoma Tumors
Abstract
:1. Introduction
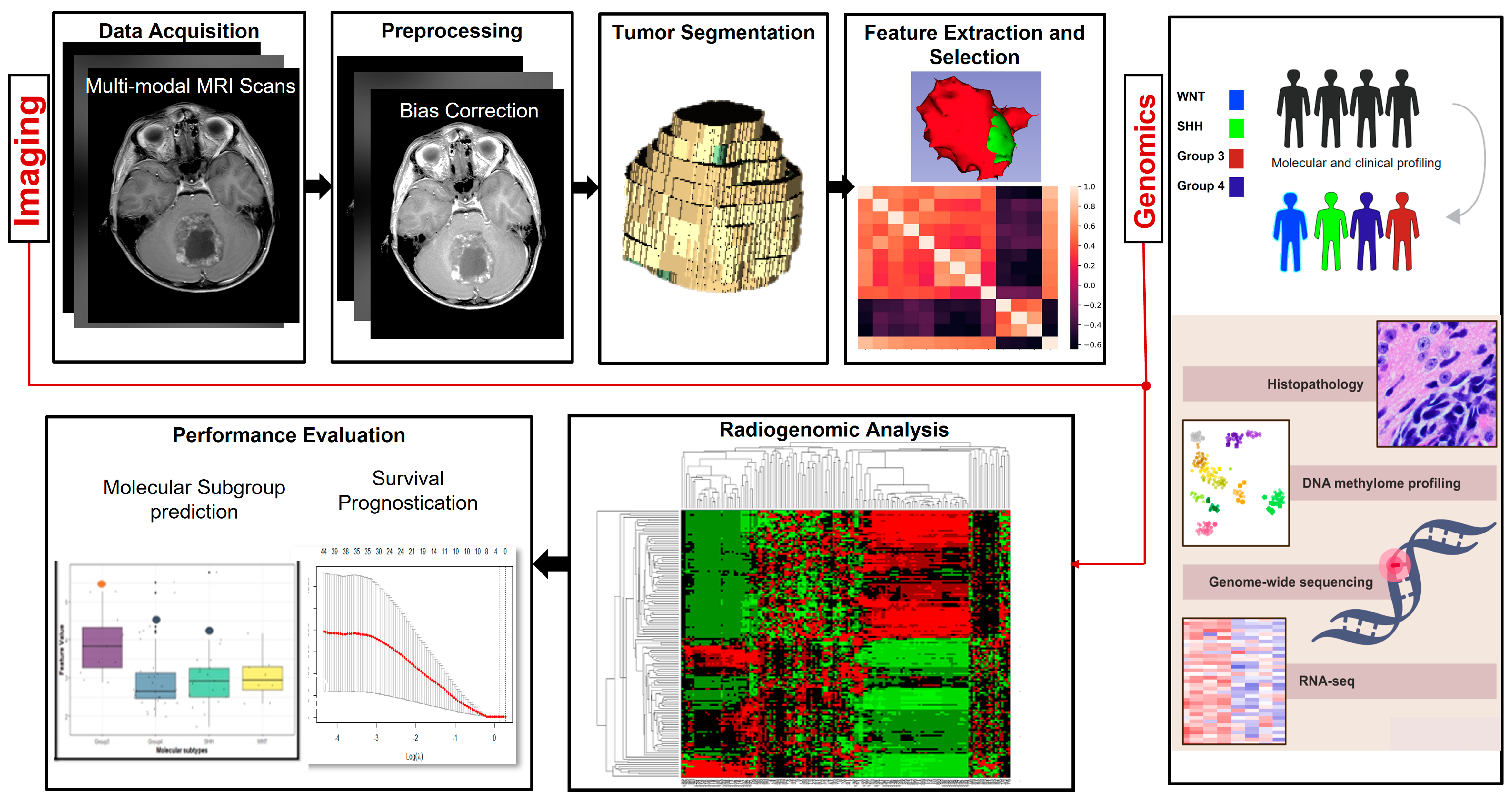
2. Overview of Radiomic and Radiogenomic Pipelines
3. Literature Review
3.1. Segmentation of Pediatric MB Tumors
3.2. Survival Prognostication in Pediatric MB Using Radiomic Approaches
3.2.1. Feature Extraction and Selection
3.2.2. Statistical Models for Survival Prognostication
3.3. Molecular Subgroup Identification in Pediatric MB Using Radiomic Approaches
3.3.1. Feature Extraction and Selection
3.3.2. Statistical Models for Molecular Subgroup Identification
4. Challenges and Future Directions
4.1. Limited Sample Size and Class Imbalances
4.2. Data-Shift and Model Generalizability across Multi-Institutional Studies
4.3. Lack of Uniformity in the Treatment Strategies across the Different MB Risk Groups
4.4. Unavailability of Molecular Subgroup Information
4.5. Linking the Extracted Radiomic Features to the Underlying Disease Pathobiology
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dressler, E.V.; Dolecek, T.A.; Liu, M.; Villano, J.L. Demographics, patterns of care, and survival in pediatric medulloblastoma. J. Neuro-Oncol. 2017, 132, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Quinlan, A.; Rizzolo, D. Understanding medulloblastoma. JAAPA 2017, 30, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, J.F.; Van Hecke, W.; Adriaansen, E.J.; Jansen, M.K.; Bouma, R.G.; Villacorta Hidalgo, J.; Fisch, P.; Broekhuizen, R.; Spliet, W.G.; Kool, M.; et al. Prognostic relevance of tumor-infiltrating lymphocytes and immune checkpoints in pediatric medulloblastoma. Oncoimmunology 2018, 7, e1398877. [Google Scholar] [CrossRef] [PubMed]
- Quaglietta, L.; Vitale, V.; Verrico, A.; Migliorati, R. Treatment of Medulloblastoma: Chemotherapy. In Posterior Fossa Tumors in Children; Springer: Cham, Switzerland, 2015; pp. 349–361. [Google Scholar]
- Dufour, C.; Beaugrand, A.; Pizer, B.; Micheli, J.; Aubelle, M.S.; Fourcade, A.; Couanet, D.; Laplanche, A.; Kalifa, C.; Grill, J. Metastatic medulloblastoma in childhood: Chang’s classification revisited. Int. J. Surg. Oncol. 2012, 2012, 245385. [Google Scholar] [CrossRef]
- Ramaswamy, V.; Remke, M.; Bouffet, E.; Bailey, S.; Clifford, S.C.; Doz, F.; Kool, M.; Dufour, C.; Vassal, G.; Milde, T.; et al. Risk stratification of childhood medulloblastoma in the molecular era: The current consensus. Acta Neuropathol. 2016, 131, 821–831. [Google Scholar] [CrossRef]
- Taylor, M.D.; Northcott, P.A.; Korshunov, A.; Remke, M.; Cho, Y.J.; Clifford, S.C.; Eberhart, C.G.; Parsons, D.W.; Rutkowski, S.; Gajjar, A.; et al. Molecular subgroups of medulloblastoma: The current consensus. Acta Neuropathol. 2012, 123, 465–472. [Google Scholar] [CrossRef]
- Kool, M.; Korshunov, A.; Remke, M.; Jones, D.T.; Schlanstein, M.; Northcott, P.A.; Cho, Y.J.; Koster, J.; Schouten-van Meeteren, A.; Van Vuurden, D.; et al. Molecular subgroups of medulloblastoma: An international meta-analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, Group 3, and Group 4 medulloblastomas. Acta Neuropathol. 2012, 123, 473–484. [Google Scholar] [CrossRef]
- Schwalbe, E.C.; Lindsey, J.C.; Nakjang, S.; Crosier, S.; Smith, A.J.; Hicks, D.; Rafiee, G.; Hill, R.M.; Iliasova, A.; Stone, T.; et al. Novel molecular subgroups for clinical classification and outcome prediction in childhood medulloblastoma: A cohort study. Lancet Oncol. 2017, 18, 958–971. [Google Scholar] [CrossRef]
- Cavalli, F.M.; Remke, M.; Rampasek, L.; Peacock, J.; Shih, D.J.; Luu, B.; Garzia, L.; Torchia, J.; Nor, C.; Morrissy, A.S.; et al. Intertumoral heterogeneity within medulloblastoma subgroups. Cancer Cell 2017, 31, 737–754. [Google Scholar] [CrossRef]
- Northcott, P.A.; Korshunov, A.; Pfister, S.M.; Taylor, M.D. The clinical implications of medulloblastoma subgroups. Nat. Rev. Neurol. 2012, 8, 340–351. [Google Scholar] [CrossRef]
- Thompson, E.M.; Ashley, D.; Landi, D. Current medulloblastoma subgroup specific clinical trials. Transl. Pediatr. 2020, 9, 157. [Google Scholar] [CrossRef] [PubMed]
- Salloum, R.; Chen, Y.; Yasui, Y.; Packer, R.; Leisenring, W.; Wells, E.; King, A.; Howell, R.; Gibson, T.M.; Krull, K.R.; et al. Late morbidity and mortality among medulloblastoma survivors diagnosed across three decades: A report from the childhood cancer survivor study. J. Clin. Oncol. 2019, 37, 731. [Google Scholar] [CrossRef] [PubMed]
- Packer, R.J.; Gurney, J.G.; Punyko, J.A.; Donaldson, S.S.; Inskip, P.D.; Stovall, M.; Yasui, Y.; Mertens, A.C.; Sklar, C.A.; Nicholson, H.S.; et al. Long-term neurologic and neurosensory sequelae in adult survivors of a childhood brain tumor: Childhood cancer survivor study. J. Clin. Oncol. 2003, 21, 3255–3261. [Google Scholar] [CrossRef] [PubMed]
- Fossati, P.; Ricardi, U.; Orecchia, R. Pediatric medulloblastoma: Toxicity of current treatment and potential role of protontherapy. Cancer Treat. Rev. 2009, 35, 79–96. [Google Scholar] [CrossRef] [PubMed]
- Larsen, E.C.; Müller, J.; Schmiegelow, K.; Rechnitzer, C.; Andersen, A.N. Reduced ovarian function in long-term survivors of radiation-and chemotherapy-treated childhood cancer. J. Clin. Endocrinol. Metab. 2003, 88, 5307–5314. [Google Scholar] [CrossRef] [PubMed]
- Michalski, J.M.; Janss, A.J.; Vezina, L.G.; Smith, K.S.; Billups, C.A.; Burger, P.C.; Embry, L.M.; Cullen, P.L.; Hardy, K.K.; Pomeroy, S.L.; et al. Children’s oncology group phase III trial of reduced-dose and reduced-volume radiotherapy with chemotherapy for newly diagnosed average-risk medulloblastoma. J. Clin. Oncol. 2021, 39, 2685–2697. [Google Scholar] [CrossRef] [PubMed]
- Zou, H.; Poore, B.; Broniscer, A.; Pollack, I.F.; Hu, B. Molecular heterogeneity and cellular diversity: Implications for precision treatment in medulloblastoma. Cancers 2020, 12, 643. [Google Scholar] [CrossRef]
- Erker, C.; Tamrazi, B.; Poussaint, T.Y.; Mueller, S.; Mata-Mbemba, D.; Franceschi, E.; Brandes, A.A.; Rao, A.; Haworth, K.B.; Wen, P.Y.; et al. Response assessment in paediatric high-grade glioma: Recommendations from the Response Assessment in Pediatric Neuro-Oncology (RAPNO) working group. Lancet Oncol. 2020, 21, e317–e329. [Google Scholar] [CrossRef]
- Rizzo, S.; Botta, F.; Raimondi, S.; Origgi, D.; Fanciullo, C.; Morganti, A.G.; Bellomi, M. Radiomics: The facts and the challenges of image analysis. Eur. Radiol. Exp. 2018, 2, 1–8. [Google Scholar] [CrossRef]
- Ismail, M.; Prasanna, P.; Bera, K.; Statsevych, V.; Hill, V.; Singh, G.; Partovi, S.; Beig, N.; McGarry, S.; Laviolette, P.; et al. Radiomic deformation and textural heterogeneity (r-depth) descriptor to characterize tumor field effect: Application to survival prediction in glioblastoma. IEEE Trans. Med. Imaging 2022, 41, 1764–1777. [Google Scholar] [CrossRef]
- Ismail, M.; Hill, V.; Statsevych, V.; Huang, R.; Prasanna, P.; Correa, R.; Singh, G.; Bera, K.; Beig, N.; Thawani, R.; et al. Shape features of the lesion habitat to differentiate brain tumor progression from pseudoprogression on routine multiparametric MRI: A multisite study. Am. J. Neuroradiol. 2018, 39, 2187–2193. [Google Scholar] [CrossRef]
- Weninger, L.; Haarburger, C.; Merhof, D. Robustness of radiomics for survival prediction of brain tumor patients depending on resection status. Front. Comput. Neurosci. 2019, 13, 73. [Google Scholar] [CrossRef]
- Kotrotsou, A.; Zinn, P.O.; Colen, R.R. Radiomics in brain tumors: An emerging technique for characterization of tumor environment. Magn. Reson. Imaging Clin. 2016, 24, 719–729. [Google Scholar] [CrossRef]
- Baid, U.; Rane, S.U.; Talbar, S.; Gupta, S.; Thakur, M.H.; Moiyadi, A.; Mahajan, A. Overall survival prediction in glioblastoma with radiomic features using machine learning. Front. Comput. Neurosci. 2020, 14, 61. [Google Scholar] [CrossRef] [PubMed]
- Kickingereder, P.; Burth, S.; Wick, A.; Götz, M.; Eidel, O.; Schlemmer, H.P.; Maier-Hein, K.H.; Wick, W.; Bendszus, M.; Radbruch, A.; et al. Radiomic profiling of glioblastoma: Identifying an imaging predictor of patient survival with improved performance over established clinical and radiologic risk models. Radiology 2016, 280, 880–889. [Google Scholar] [CrossRef] [PubMed]
- Pinker, K.; Shitano, F.; Sala, E.; Do, R.K.; Young, R.J.; Wibmer, A.G.; Hricak, H.; Sutton, E.J.; Morris, E.A. Background, current role, and potential applications of radiogenomics. J. Magn. Reson. Imaging 2018, 47, 604–620. [Google Scholar] [CrossRef]
- Grist, J.T.; Withey, S.; Bennett, C.; Rose, H.E.; MacPherson, L.; Oates, A.; Powell, S.; Novak, J.; Abernethy, L.; Pizer, B.; et al. Combining multi-site magnetic resonance imaging with machine learning predicts survival in pediatric brain tumors. Sci. Rep. 2021, 11, 18897. [Google Scholar] [CrossRef]
- Yan, J.; Zhang, S.; Li, K.K.; Wang, W.; Li, K.; Duan, W.; Yuan, B.; Wang, L.; Liu, L.; Zhan, Y.; et al. Incremental prognostic value and underlying biological pathways of radiomics patterns in medulloblastoma. eBioMedicine 2020, 61. [Google Scholar] [CrossRef]
- Liu, Z.M.; Zhang, H.; Ge, M.; Hao, X.L.; An, X.; Tian, Y.J. Radiomics signature for the prediction of progression-free survival and radiotherapeutic benefits in pediatric medulloblastoma. Child’s Nerv. Syst. 2022, 38, 1085–1094. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Li, J.; Liu, H.; Ting, G.; Yin, Q.; Li, R.; Liu, M.; Zhang, Y.; Duan, S.; Li, Y.; et al. MRI Radiomics Signature of Pediatric Medulloblastoma Improves Risk Stratification Beyond Clinical and Conventional MR Imaging Features. J. Magn. Reson. Imaging 2022, 58, 236–246. [Google Scholar] [CrossRef]
- Iyer, S.; Ismail, M.; Tamrazi, B.; Salloum, R.; de Blank, P.; Margol, A.; Correa, R.; Chen, J.; Bera, K.; Statsevych, V.; et al. Novel MRI deformation-heterogeneity radiomic features are associated with molecular subgroups and overall survival in pediatric medulloblastoma: Preliminary findings from a multi-institutional study. Front. Oncol. 2022, 12, 915143. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.C.; Wong, T.T.; Wu, K.S.; Lu, C.F.; Weng, T.W.; Liang, M.L.; Wu, C.C.; Guo, W.Y.; Chen, C.Y.; Hsieh, K.L. Magnetic resonance radiomics features and prognosticators in different molecular subtypes of pediatric Medulloblastoma. PLoS ONE 2021, 16, e0255500. [Google Scholar] [CrossRef] [PubMed]
- Iv, M.; Zhou, M.; Shpanskaya, K.; Perreault, S.; Wang, Z.; Tranvinh, E.; Lanzman, B.; Vajapeyam, S.; Vitanza, N.A.; Fisher, P.G.; et al. MR imaging–based radiomic signatures of distinct molecular subgroups of medulloblastoma. Am. J. Neuroradiol. 2019, 40, 154–161. [Google Scholar] [CrossRef]
- Saju, A.C.; Chatterjee, A.; Sahu, A.; Gupta, T.; Krishnatry, R.; Mokal, S.; Sahay, A.; Epari, S.; Prasad, M.; Chinnaswamy, G.; et al. Machine-learning approach to predict molecular subgroups of medulloblastoma using multiparametric MRI-based tumor radiomics. Br. J. Radiol. 2022, 95, 20211359. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, L.; Qin, B.; Hu, X.; Xiao, W.; Tong, Z.; Li, S.; Jing, Y.; Li, L.; Zhang, Y. Preoperative prediction of sonic hedgehog and group 4 molecular subtypes of pediatric medulloblastoma based on radiomics of multiparametric MRI combined with clinical parameters. Front. Neurosci. 2023, 17, 1157858. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Liu, L.; Wang, W.; Zhao, Y.; Li, K.K.; Li, K.; Wang, L.; Yuan, B.; Geng, H.; Zhang, S.; et al. Radiomic features from multi-parameter MRI combined with clinical parameters predict molecular subgroups in patients with medulloblastoma. Front. Oncol. 2020, 10, 558162. [Google Scholar] [CrossRef]
- Zhang, M.; Wong, S.W.; Wright, J.N.; Wagner, M.W.; Toescu, S.; Han, M.; Tam, L.T.; Zhou, Q.; Ahmadian, S.S.; Shpanskaya, K.; et al. MRI radiogenomics of pediatric medulloblastoma: A multicenter study. Radiology 2022, 304, 406–416. [Google Scholar] [CrossRef]
- Dasgupta, A.; Gupta, T.; Pungavkar, S.; Shirsat, N.; Epari, S.; Chinnaswamy, G.; Mahajan, A.; Janu, A.; Moiyadi, A.; Kannan, S.; et al. Nomograms based on preoperative multiparametric magnetic resonance imaging for prediction of molecular subgrouping in medulloblastoma: Results from a radiogenomics study of 111 patients. Neuro-Oncology 2019, 21, 115–124. [Google Scholar] [CrossRef]
- Chen, X.; Fan, Z.; Li, K.K.; Wu, G.; Yang, Z.; Gao, X.; Liu, Y.; Wu, H.; Chen, H.; Tang, Q.; et al. Molecular subgrouping of medulloblastoma based on few-shot learning of multitasking using conventional MR images: A retrospective multicenter study. Neuro-Oncol. Adv. 2020, 2, vdaa079. [Google Scholar] [CrossRef]
- Madhogarhia, R.; Fathi Kazerooni, A.; Arif, S.; Ware, J.B.; Familiar, A.M.; Vidal, L.; Bagheri, S.; Anderson, H.; Haldar, D.; Yagoda, S.; et al. Automated segmentation of pediatric brain tumors based on multi-parametric MRI and deep learning. In Medical Imaging 2022: Computer-Aided Diagnosis; Iftekharuddin, K.M., Drukker, K., Mazurowski, M.A., Lu, H., Muramatsu, C., Samala, R.K., Eds.; SPIE: Philadelphia, PA, USA, 2022; Volume 124. [Google Scholar] [CrossRef]
- Peng, J.; Kim, D.D.; Patel, J.B.; Zeng, X.; Huang, J.; Chang, K.; Xun, X.; Zhang, C.; Sollee, J.; Wu, J.; et al. Deep learning-based automatic tumor burden assessment of pediatric high-grade gliomas, medulloblastomas, and other leptomeningeal seeding tumors. Neuro-Oncology 2022, 24, 289–299. [Google Scholar] [CrossRef]
- Shaari, H.; Kevrić, J.; Jukić, S.; Bešić, L.; Jokić, D.; Ahmed, N.; Rajs, V. Deep learning-based studies on pediatric brain tumors imaging: Narrative review of techniques and challenges. Brain Sci. 2021, 11, 716. [Google Scholar] [CrossRef] [PubMed]
- Artzi, M.; Gershov, S.; Ben-Sira, L.; Roth, J.; Kozyrev, D.; Shofty, B.; Gazit, T.; Halag-Milo, T.; Constantini, S.; Ben Bashat, D. Automatic segmentation, classification, and follow-up of optic pathway gliomas using deep learning and fuzzy c-means clustering based on MRI. Med. Phys. 2020, 47, 5693–5701. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Edwards, A.; Wang, S.; Patay, Z.; Bag, A.; Scoggins, M.A. A Prior Knowledge Based Tumor and Tumoral Subregion Segmentation Tool for Pediatric Brain Tumors. arXiv 2021, arXiv:2109.14775. [Google Scholar]
- Bakas, S.; Reyes, M.; Jakab, A.; Bauer, S.; Rempfler, M.; Crimi, A.; Shinohara, R.T.; Berger, C.; Ha, S.M.; Rozycki, M.; et al. Identifying the best machine learning algorithms for brain tumor segmentation, progression assessment, and overall survival prediction in the BRATS challenge. arXiv 2018, arXiv:1811.02629. [Google Scholar]
- Liu, Z.; Tong, L.; Chen, L.; Jiang, Z.; Zhou, F.; Zhang, Q.; Zhang, X.; Jin, Y.; Zhou, H. Deep learning-based brain tumor segmentation: A survey. Complex Intell. Syst. 2023, 9, 1001–1026. [Google Scholar] [CrossRef]
- Smoll, N.R.; Drummond, K.J. The incidence of medulloblastomas and primitive neurectodermal tumours in adults and children. J. Clin. Neurosci. 2012, 19, 1541–1544. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society. Available online: https://www.cancer.org/cancer/types/brain-spinal-cord-tumors-adults/about/key-statistics.html (accessed on 27 June 2023).
- Pediatric Brain Tumor Consortium. Available online: https://www.pbtc.org (accessed on 1 July 2023).
- Ali, A.; Shamsuddin, S.M.; Ralescu, A.L. Classification with class imbalance problem. Int. J. Adv. Soft Comput. Appl. 2013, 5, 176–204. [Google Scholar]
- Madabhushi, A.; Udupa, J.K. Interplay between intensity standardization and inhomogeneity correction in MR image processing. IEEE Trans. Med. Imaging 2005, 24, 561–576. [Google Scholar] [CrossRef]
| Acronym | Term | Acronym | Term |
|---|---|---|---|
| ADC | Apparent Diffusion Coefficient | ICC | Intraclass Correlation Coefficient |
| AUC | Area Under the Curve | KPS | Karnofsky Performance Status |
| CBV | Cerebral Blood Volume | LASSO | Least Absolute Shrinkage and Selection Operator |
| CE | Contrast-Enhanced | LOOCV | Leave-One-Out Cross-Validation |
| CI | Concordance Index | MB | Medulloblastoma |
| CNN | Convolutional Neural Network | MRI | Magnetic Resonance Imaging |
| DC | Dice Coefficient | OS | Overall Survival |
| DSC | Dynamic Susceptibility Contrast | PFS | Progression-Free survival |
| DWI | Diffusion-Weighted Images | RF | Random Forest |
| Gd-T1w | Gadolinium-enhanced T1-weighted | SHH | Sonic Hedgehog |
| GLCM | Gray-level co-occurrence matrix | SVM | Support Vector Machine |
| HR | Hazard Ratio | uCBV | Uncorrected Cerebral Blood Volume |
| WNT | Wingless |
| Group | Radiomic Endpoint | Sample Size | Single or Multi-Institution | Mean Age (Years) Unless Otherwise Denoted | Features | Modality | Models & Feature Selection Methods | Performance Metrics/Statistical Analysis | Model Performance | Limitations |
|---|---|---|---|---|---|---|---|---|---|---|
| Grist et al., 2021 [28] | Survival prediction | 17 | Multi | 8.85 | ADC maps (kurtosis, mean, etc.), mean of corrected CBV, mean of uncorrected CBV, tumor volume | T2w, DWI, DSC | Cox regression; Iterative Bayesian analysis; KNN; SVM; RF | Kaplan–Meier Analysis, HR | Unsupervised clustering: HR = 5.6, confidence intervals = 1.6–20.1, p < 0.001 for high-risk patients Supervised machine learning: Bayesian features with a single-layer neural network & 10-fold cross-validation provided 98% accuracy | Small cohort size |
| Iyer et al., 2022 [32] | Survival prediction | 88 (n = 60 for training, n = 28 for testing) | Multi | 5.4 | Deformation heterogeneity features | Gd-enhanced T1w | Logistic regression, Cox models, LASSO | Kaplan–Meier Analysis, HR, CI | , CI = 0.7 between low- and high-risk patients , CI = 0.75) | Small cohort size Lack of uniformity in the treatment strategies for the risk groups |
| Liu et al., 2021 [30] | Survival prediction | 253 (113: training; 113:hold-out test set 1; 27:hold-out test set 2) | Multi | 7.4 for training set; 8.1 for hold-out test set 1; 6.8 for hold-out test set 2 | 647 features per modality (8 size and shape, 639 texture) | T1w, CE-T1w | Pearson’s correlation, Cox Regression with LASSO | Kaplan–Meier Analysis, Kruskal–Wallis test | Predictive model of PFS yielded C-indices of 0.71, 0.7, and 0.72 on training and hold-out test sets 1 and 2. The radiomics nomogram integrating radiomic features, age, metastasis performed better than the nomogram incorporating clinicopathological factors (CI = 0.723 vs. 0.665 and 0.722 vs. 0.677 on the held-out test sets 1 and 2) | Molecular information was not involved. Limited size for hold-out test set 2 |
| Yan et al., 2020 [29] | Survival prediction | 166 (83: training,83: testing) | Single | Median: 8 | 5929 features (shape, first-order intensity, higher-order texture). | T1w, CE-T1w, T2w, FLAIR, ADC maps | ICC, LASSO, Cox regression | Kaplan–Meier Analysis; Wilcoxon test/chi-square test | Radiomics-clinicomolecular signature predicted OS (CI = 0.762), PFS (CI = 0.697) better than radiomics signature (CIs = 0.649,0.593 for OS, PFS) or the clinicomolecular signature (CIs = 0.725, 0.691 for OS, PFS) | Limited sample size Lack of volumetric MRI data |
| Zheng et al., 2022 [31] | Survival prediction | 111 (77: training, 34: testing) | Single | 5.82 | 1132 features (first-order statistics, volume, shape, GLCM, gray-level run-length matrix, gray-level size zone matrix) | CE-T1w | Cox regression model, LASSO | T-test, Mann–Whitney U test, Fisher’s exact/chi-square test | Radiomic features + clinical + conventional MRI features yielded best results for predicting OS (CI = 0.82), vs. using the radiomic signature alone (CI = 0.7) on training set CIs were 0.78 and 0.75 using the integrative model and the radiomic model, on the test set | Limited sample size Data was from a single institution. Molecular information was not available |
| Group | Radiomic Endpoint | Sample Size | Single or Multi-Institution | Mean * Age (Years) * Unless Otherwise Denoted | Features | Modality | Models & Feature Selection Methods | Performance Metrics/Statistical Analysis | Model Performance | Limitations |
|---|---|---|---|---|---|---|---|---|---|---|
| Chang et al., 2021 [33] | Molecular classification | 38 (WNT: 7, SHH: 12, Group 3: 8, Group 4: 11) | Multi | 7.5 | 253 features (intensity, shape and size, texture) | T1w, T2w, FLAIR, CE- T1w, ADC | minimum redundancy maximum relevance; sequential backward elimination; SVM | Accuracy, Sensitivity, Specificity | The model based on 8 GLCM features has AUCs of 0.82, 0.72, and 0.78 for WNT, Group 3, and Group 4 | Limited sample size |
| Iyer et al., 2022 [32] | Molecular classification | 71 (n = 49 for training- WNT:4, SHH:15, Group 3:8, Group 4: 22; n = 22 for testing- WNT:3, SHH:6, Group 3:3, Group 4:10) | Multi | 5.4 | Deformation heterogeneity features | Gd-T1w | Multiclass ANOVA; multiple comparison of means | HR, CI | p-values = 0.028 for Group 3 vs. SHH and Group 4, 0.05 for Group 3 vs. Group 4 | Small cohort size Lack of uniformity in the treatment strategies for the different subgroups Mutation information for the molecular subgroups was not available |
| Chen et al., 2020 [40] | Molecular classification | 113 (n = 74 for validation- WNT:17, SHH:18, Group 3:20, Group 4:19; n = 39 for testing- WNT:7, SHH:9, Group 3:11, Group 4: 12) | Multi | 4.4 for infants, 10.5 for children | Feature pyramid network & refined feature layers of Residual neural network (ResNet101) | CE-T1w, T2w | Mask-RCNN model: feature extraction, region proposal, prediction. | Kruskal–Wallis test, AUC, sensitivity, specificity | Accuracy of 0.93 in the cross-validation cohort and 0.85 in the testing cohort. AUCs of molecular subgrouping were 0.97 and 0.92 in cross-validation and independent test cohorts | Limited sample size No information about evidence of spinal metastasis to predict dissemination |
| Dasgupta et al., 2019 [39] | Molecular classification | 111 (WNT: 17, SHH: 44, Group 3: 27, Group 4: 23) | Multi | Median = 9 | Tumor size, MR Imaging characteristics | T1w, T2w, DWI | Multimodal logistic regression, nomogram construction | Pearson chi-square test, Fisher’s exact test, Cohen’s Kappa statistics | Overall molecular subgroup accuracy = 74%; 95% SHH, 78% Group 4, 56% Group 3, 41% WNT | No reliable prediction of WNT and Group 3 A uniform MRI protocol was not used No correlation between magnetic resonance spectroscopy findings & molecular subgrouping |
| IV et al., 2019 [34] | Molecular classification | 109 (WNT: 19, SHH: 30, Group 3: 24, Group 4: 36) | Multi | 8.7 (across three sites) | 590 features (intensity-based histograms, tumor edge-sharpness, Gabor, local area integral invariant features) | T1w, T2w | Wilcoxon rank sum test, SVM classifier | AUC, ROC curves | Double 10-fold cross-validation for predicting SHH, Group 3, Group 4 using combined T1w and T2w images yielded AUCs = 0.79, 0.70, and 0.83, respectively | Heterogeneity in image data (different scanners, etc.) Limited imaging sequences |
| Saju et al., 2022 [35] | Molecular classification | 38 (WNT:7, SHH:7, Group 3:12, Group 4:12) | Single | Median = 9 | 82 features from each modality; first and second-order GLCM and shape features | CE-T1w, T2w | LASSO, SVM | AUC, ROC curves | 10-fold cross-validation yielded AUCs of 0.93, 0.9, 0.93, and 0.93 in predicting WNT, SHH, Group 3, and Group 4 | Very limited sample size |
| Wang et al., 2023 [36] | SHH and Group 4 prediction | 95 (SHH:47, Group 4:48; ratio 7:3 training: test) | Multi | 6.75 for SHH, 7.5 for Group 4 | 7045 features (intensity statistics, texture, shape and size, high-order statistics) | T1-, CE- T1-, T2-weighted, FLAIR, ADC | LASSO | T-test, Fisher’s exact test, Delong test, AUC, ROC curves | Classification model with 17 optimal features yielded AUCs of 0.96 and 0,75 in training and test cohorts | Limited sample size No external validation No inclusion of WNT, Group 3 |
| Yan et al., 2020 [37] | Molecular classification | 122 (92 for training- WNT:15, SHH:16, Group 3:40, Group 4:21; 30 for testing- WNT:6, SHH:4, Group 3:14, Group 4:6) | Single | 11.57 | 5929 features (location, shape, intensity, texture) | T1w, CE-T1w, T2w, FLAIR, ADC | ICC, RF-based wrapper algorithm, logistic regression | Kruskal–Wallis test, Wilcoxon test, ROC, AUC | Incorporating tumor location, gender, age, and hydrocephalus with radiomics generated AUCs of 0.91 and 0.86 for WNT and SHH | Advanced MR sequences not included Limited sample size Nanostring assay was utilized for molecular subgrouping, which is not a calibrated assay |
| Zhang et al., 2022 [38] | Molecular classification | 263 (WNT: 26, SHH: 83, Group 3/4: 154; 75:25 for training: test set) | Multi | 10.1 for WNT, 6.9 for SHH, 12.8 for Group 3/4 | 1800 texture features | CE-T1w, T2w | Binary classifier along with SVM, logistic regression, KNN, RF, extreme gradient boosting, neural network | Wald test, Dice Similarity Score | Combined, the sequential classifier achieved a DC score of 88% and a binary score of 95% for WNT. Group 3 vs. Group 4 classifier achieved an AUC of 98% | Limited sample size Heterogeneity of MR scans (12 sites) Features extracted from isolated tumor volumes No incorporation of tumor-brain spatial relationships |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ismail, M.; Craig, S.; Ahmed, R.; de Blank, P.; Tiwari, P. Opportunities and Advances in Radiomics and Radiogenomics for Pediatric Medulloblastoma Tumors. Diagnostics 2023, 13, 2727. https://doi.org/10.3390/diagnostics13172727
Ismail M, Craig S, Ahmed R, de Blank P, Tiwari P. Opportunities and Advances in Radiomics and Radiogenomics for Pediatric Medulloblastoma Tumors. Diagnostics. 2023; 13(17):2727. https://doi.org/10.3390/diagnostics13172727
Chicago/Turabian StyleIsmail, Marwa, Stephen Craig, Raheel Ahmed, Peter de Blank, and Pallavi Tiwari. 2023. "Opportunities and Advances in Radiomics and Radiogenomics for Pediatric Medulloblastoma Tumors" Diagnostics 13, no. 17: 2727. https://doi.org/10.3390/diagnostics13172727
APA StyleIsmail, M., Craig, S., Ahmed, R., de Blank, P., & Tiwari, P. (2023). Opportunities and Advances in Radiomics and Radiogenomics for Pediatric Medulloblastoma Tumors. Diagnostics, 13(17), 2727. https://doi.org/10.3390/diagnostics13172727






