Multi-Modal Data Analysis for Pneumonia Status Prediction Using Deep Learning (MDA-PSP)
Abstract
1. Introduction
1.1. MDA-PSP Objectives
- Scrutinizing the digital data for the pneumonia prediction using artificial intelligence: Artificial intelligence is considered to be an important factor for the pneumonia prediction in patients. Therefore, the MDA-PSP uses combined vital signs and CXR of patients to predict pneumonia status using a trained model and classifying them using deep learning.
- Leverage medical doctor’s experience for the pneumonia status: MDA-PSP provides an effective solution for pneumonia prediction based on different parameters of 19 vital signs and five different sections in CXR multi-modal data analysis with their combinations. Thus, combining the patient’s physiological data and chest X-ray image’s within first 3 days and the training model to achieve better accuracy by the predictive model interpretability benefits the physicians analysis.
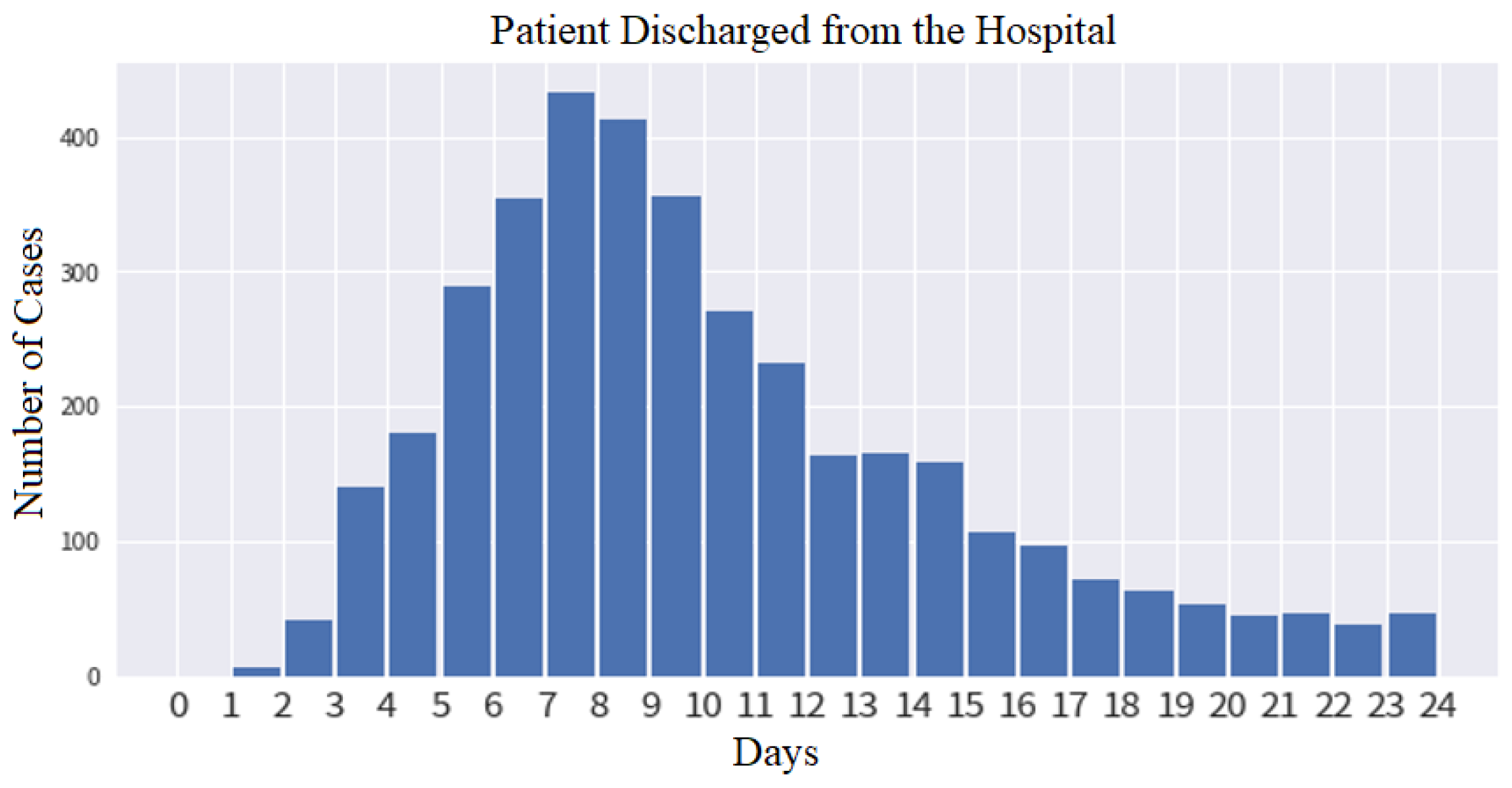
- Mean time analysis of the patient’s pneumonia recovery within the next 7 days: The analysis is evaluated by a trained model consisting of SHAP and dense layers with class weights having the input readings from the initial to 2nd/3rd day of vital signs and CXR that can effectively predict the recovery status of the patient on the 7th day.
1.2. Literature Survey
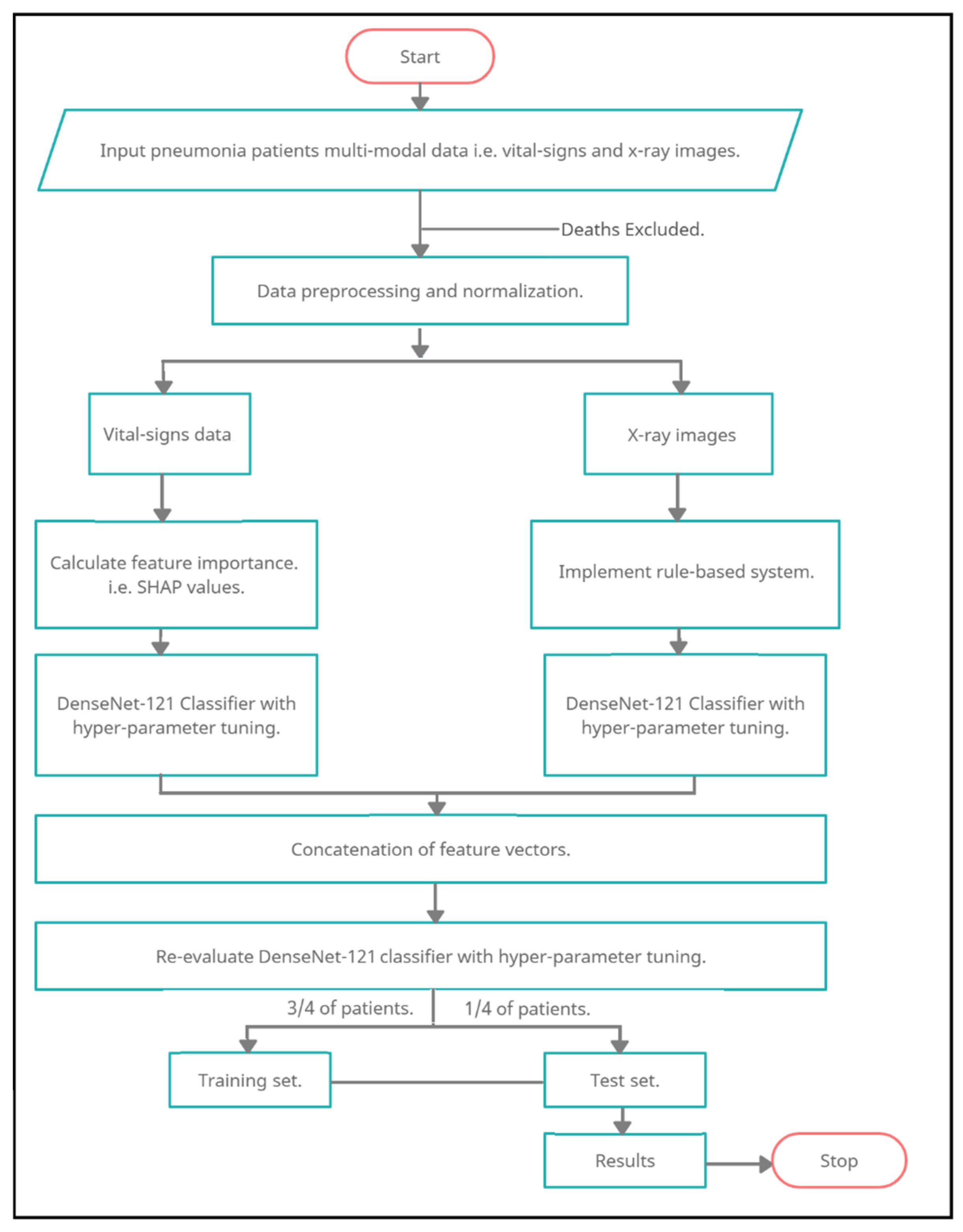
2. Materials and Methods
2.1. Hospitalization Conditions and Criteria
2.1.1. Pre-Requisite and Hospitalization Criteria of the Patients
2.1.2. The Decision for Discharge within 7 Days
2.1.3. Input Data for Multi-Modal Analysis
2.2. Data Preprocessing
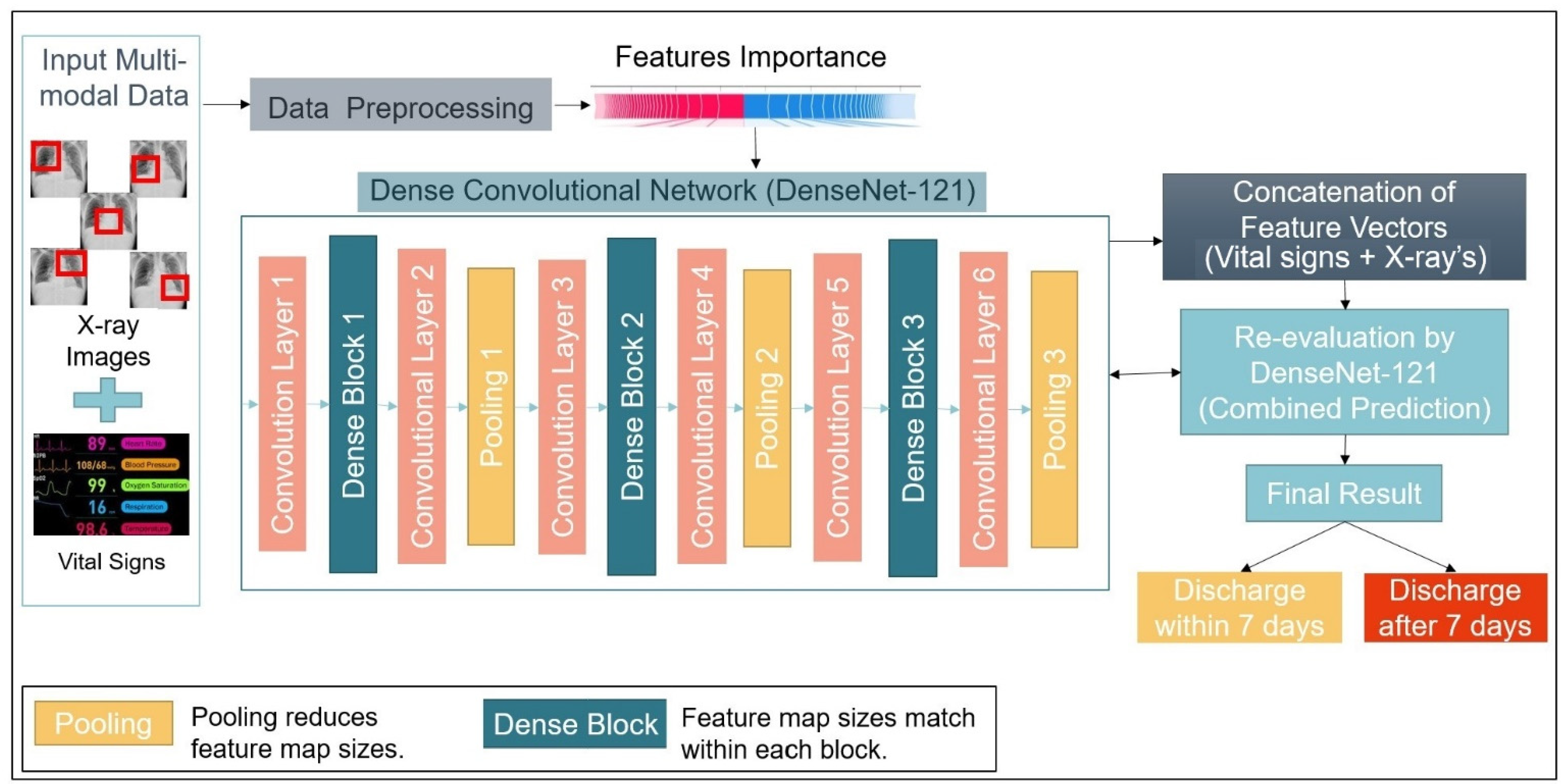
2.3. Functional Model
2.4. Algorithms
| Algorithm 1: Pneumonia Status Prediction by Data Preprocessing and Feature Vectorization using Multi-Modal Data Analysis |
|
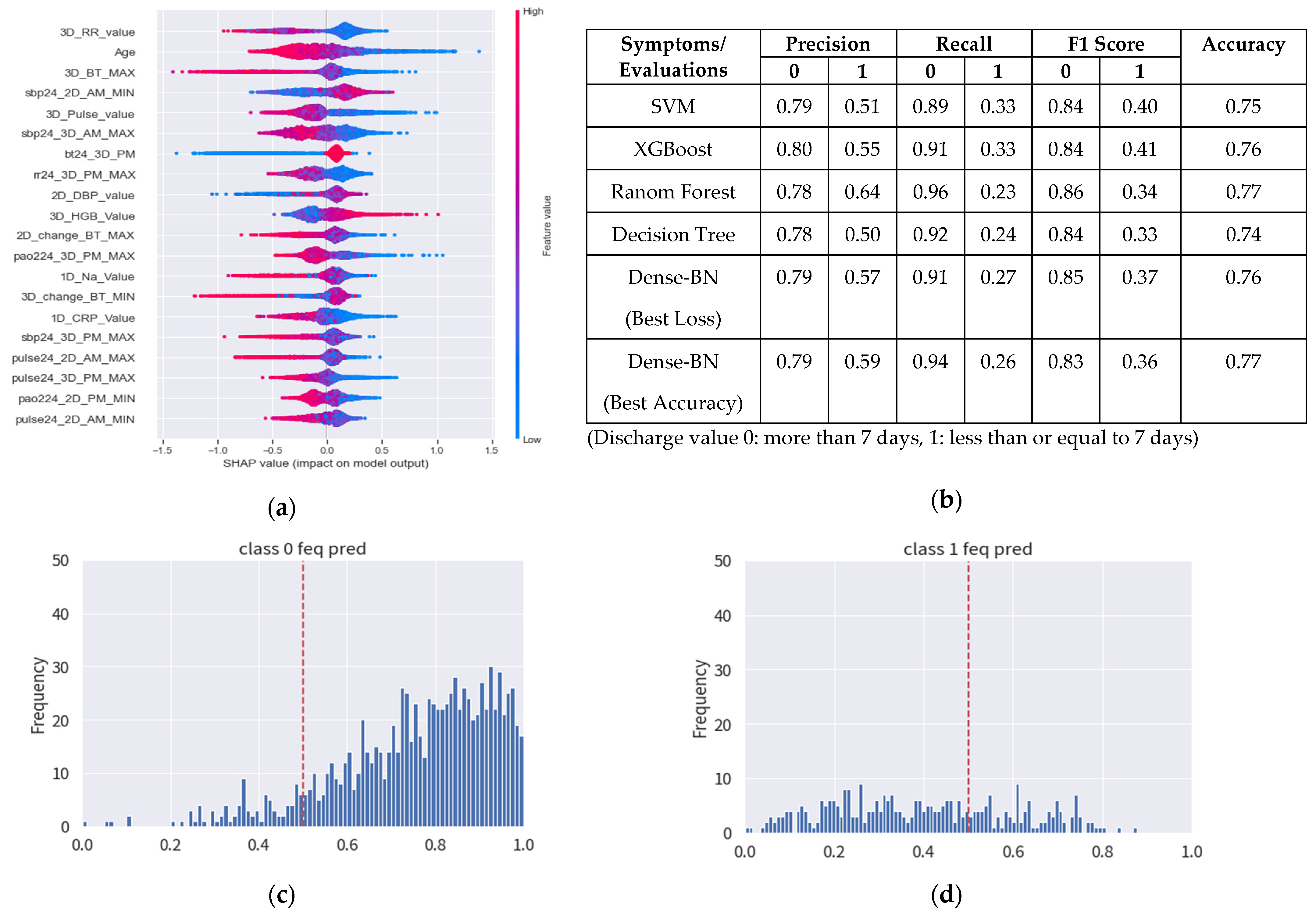
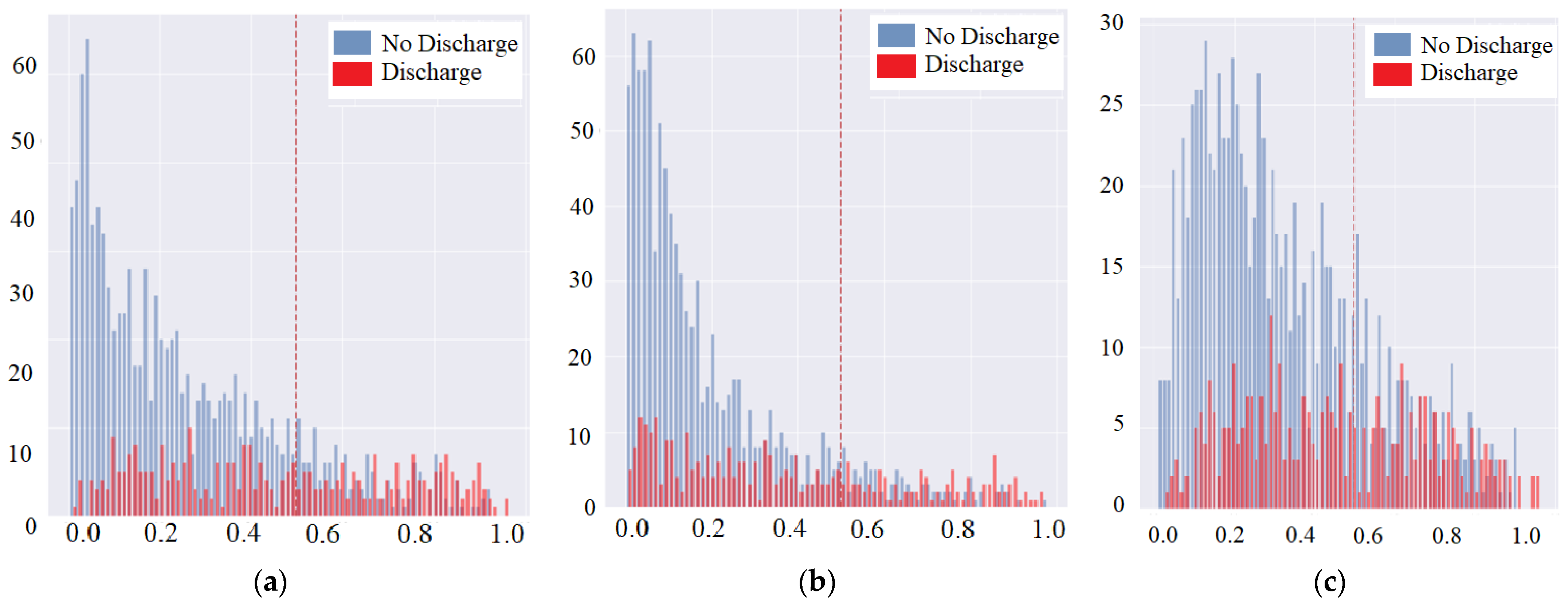
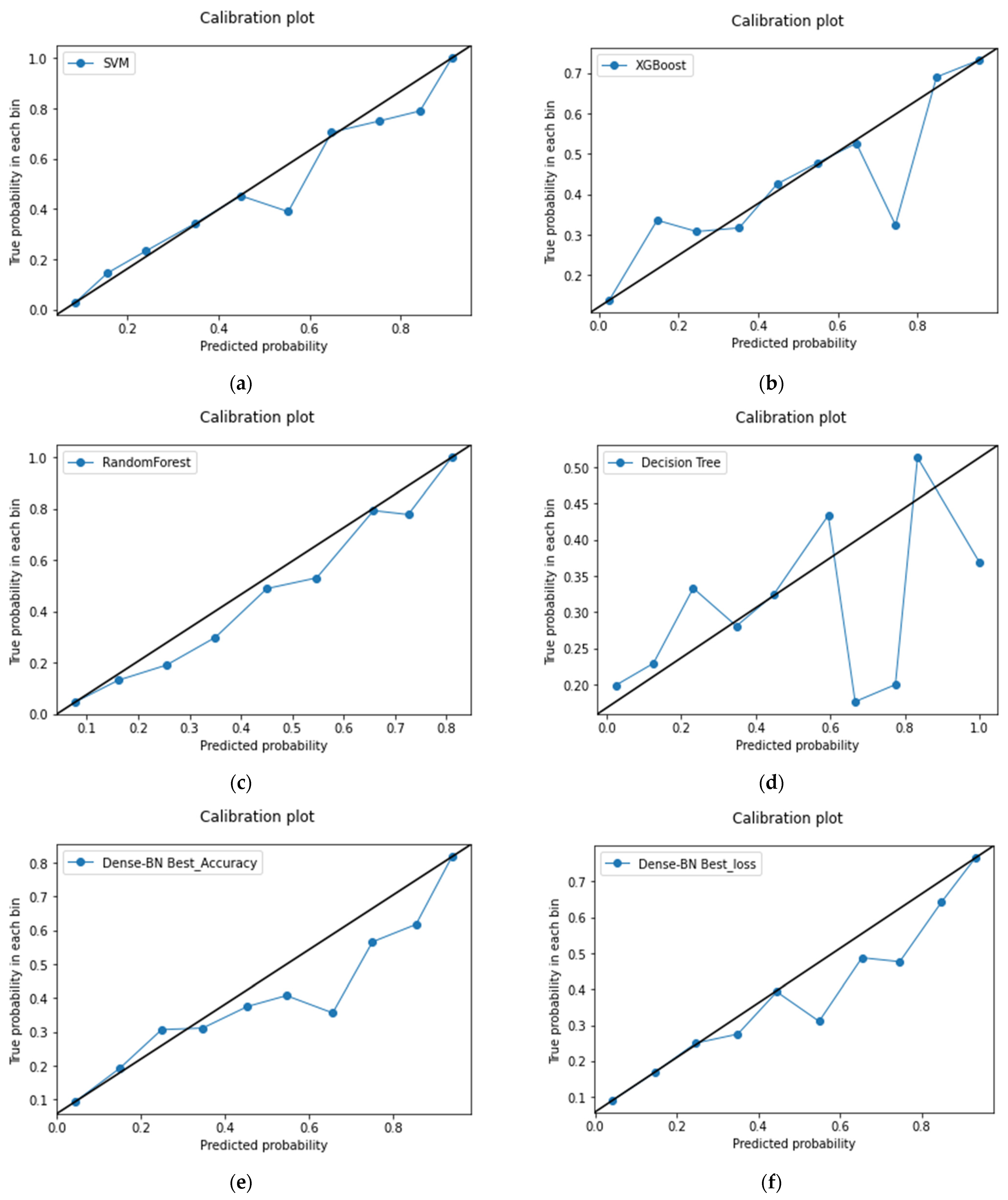
3. Results
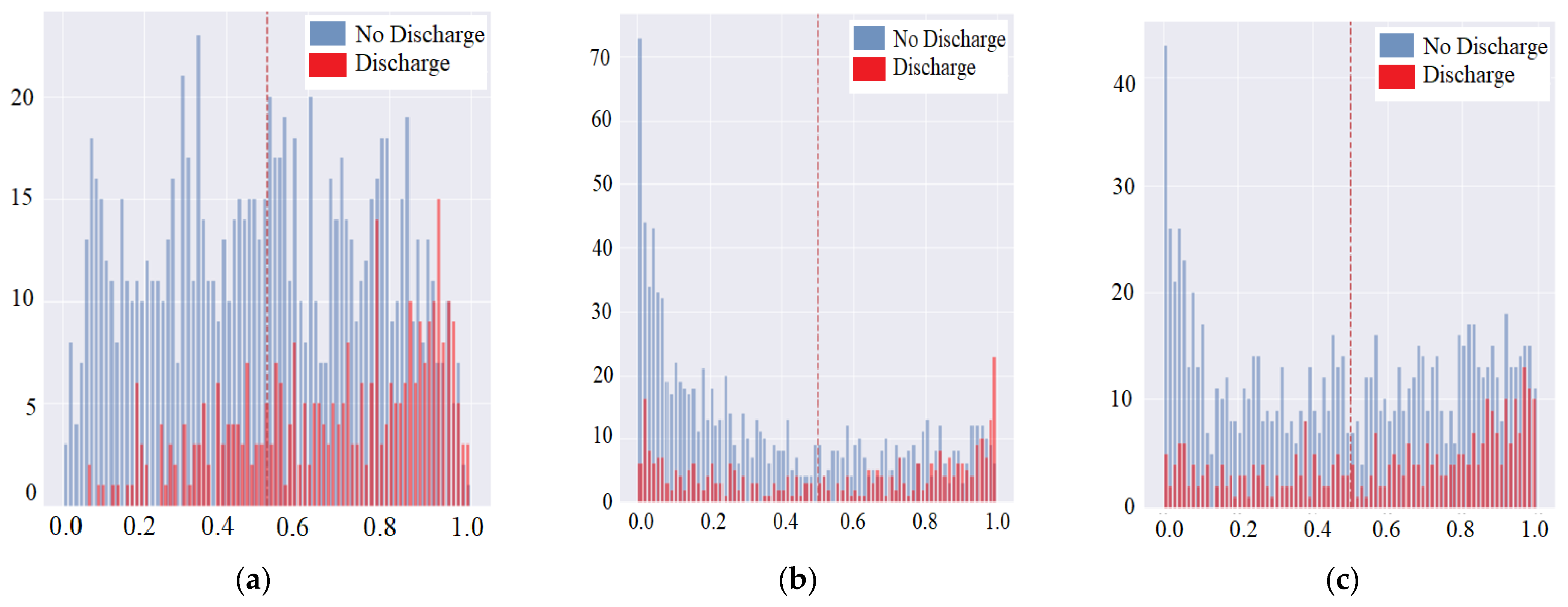
3.1. Data Preprocessing
3.1.1. Vital Signs for Data Observations, Feature Scoring and Evaluation
3.1.2. CXR Imaging Sections for Symptom Categorization
3.1.3. Symptom Feature Extraction and CXR Combination with Vital Signs
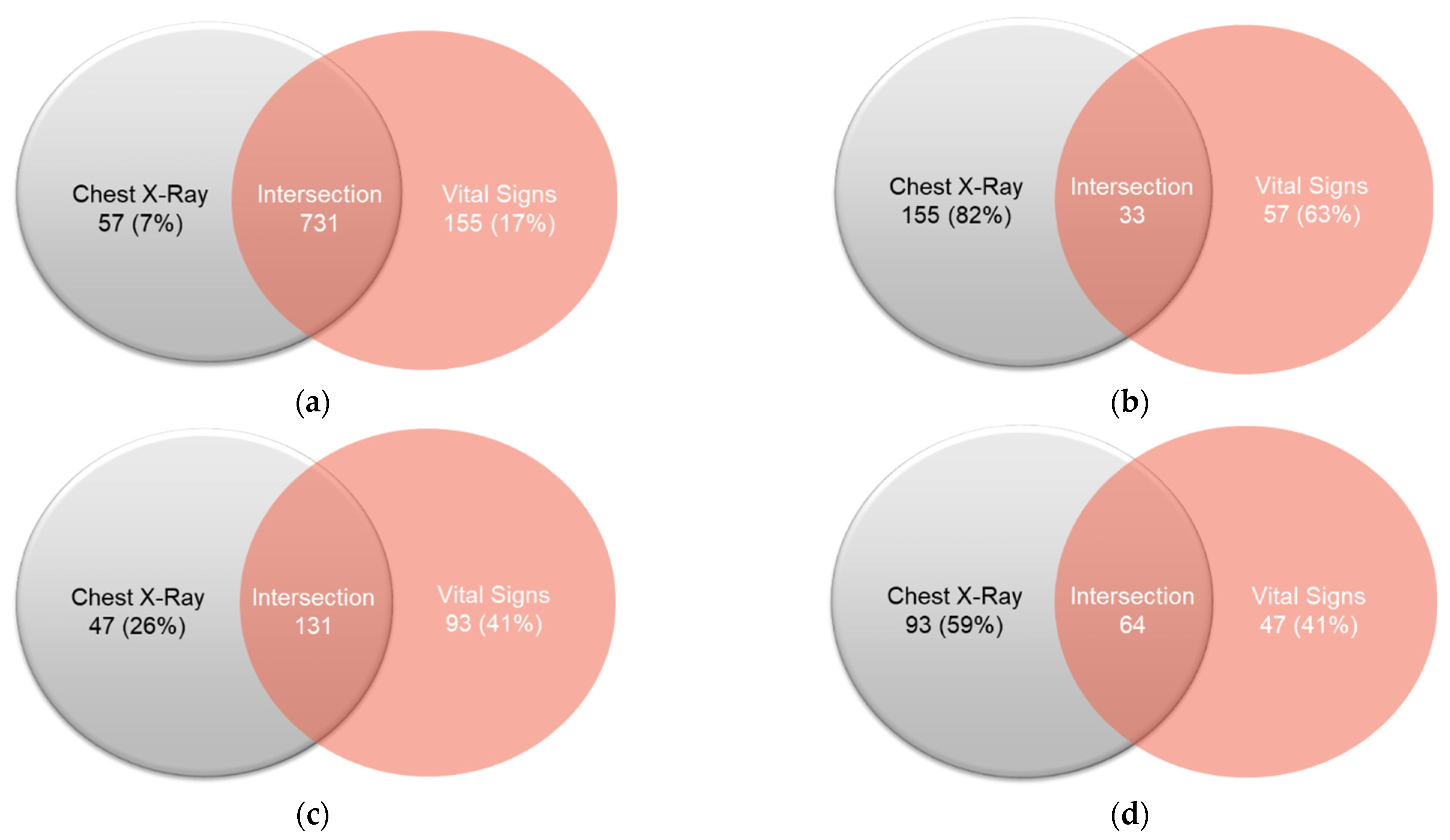
4. Discussion
4.1. The following Factors Are Completely Variable and the Occurrence of It Depends on Health, Mental, Financial Status, etc.
- Insurance: In Taiwan, the government provides national health insurance (NHI) cards to the citizens. The NHI card requires a once a year payment of nominal amount, which then provides health insurance for any major natural or accidental treatment within any Taiwanese major hospital. Even though it provides insurance for any case, the time period for the patient to be admitted should be no more than 7 days for the refund. So, this forms the need for one of our motivations to design an XAI model for prediction of the patient’s discharge on the 7th day. Due to insurance benefit conditions, both the doctor and patient prefer to have discharge within 7 days of the hospital admittance.
- Suitable Discharge Time: The suitable discharge time for the patient is considered to be less than or equal to 7 days in the treatment. Nevertheless, less time is always favorable as it can save hospital resources as well as of the doctors, patients, family, hospital staff, etc. Whereas in the case of unfavorable cases, the patient is required to stay for a longer time duration that may lead to losing the insurance claim for the refund. The suitable discharge time can also refer to the minimum treatment time required based on the patient’s health severity and may be the trainee doctor’s decision. The pneumonia is known to happen in any age range from one day born infant to any adult patient, so the decision also considers the medicine treatment effects. In the case of diet based on certain regional, lifestyle factors, the discharge time may vary, too.
- Doctor’s Recommendation: In rare cases, the doctors usually recommend the patient to take a delayed discharge. Complexity of the case may depend on age, lifestyle for the slower recovery, or adapting to the normal health status. In addition, there are foreign patients who need to be treated exclusively and by experienced doctors, as the treatment approach and the recovery may vary depending on different continents. In some cases, the treatment by some medicine may react in the medical report. Therefore, the doctor needs more time to change the treatment and to have patience for the recovery process.
- Patient’s Mental Status: The discharge time also depends on the patient’s willingness or feeling energetic to confirm complete recovery. The doctors usually check for vital signs and medical reports for the discharge approval. In rare cases, if the patient is not mentally ready to discharge and possess good financial background, then the doctor may allow to continue stay depending upon beds availability. In some cases, if a patient is addicted to some habits, then he prefers to stay until complete recovery. It can also depend on how much the patient needs medical facilities to be received in a special exclusive room for the admittance. As soon as the patient is recovered, the doctor recommends discharge and continues to monitor vital signs remotely by using sensor watch, video camera-based consulting sessions, etc. The patient then later on can stay connected with the specialist doctor to report the symptoms, if any, as the follow-up.
- Re-admission Issue: In some exceptional circumstances [48,49], the patient has to go through the re-admission in the hospital. In the case of mid-size hospitals, there may be an undetected issue or the specialist doctor and medical condition predicting machines are not available in the emergency situation. Moreover, if the patient is in the transfer period because of his work, business, family shifting, or other factors, then the patient has to request for transfer options with the hospital by co-operation process. In some insurance cases, the patient can only get refund advantage of the hospital charges with referring to some specific hospital. Possibly, there can be some recommendations by the family or doctor to shift to a specialty hospital for fast recovery and experienced approach towards serious health conditions.
- Family Care/Support: In the case of some single people residing remotely [50] from the hometown region, the doctor may advise the patient to stay a couple of days more for the complete health recovery convenience. Even if there are some foreign patients working in the company, they may need special treatment and consulting for the health recovery. When the family and financial support is good, then the services can be shifted to the patient’s home by a visiting doctor. Whereas in the case of serious health conditions, the doctor may advise the patient to shift to a exclusive room, reserved for the special treatment facility.
- Multiple Disease Disorder (Comorbidity) of a Patient: In special cases, a patient is admitted in the hospital with a chronic disease [51]. Later on, a past or new disease is diagnosed, which is required to be treated carefully. In such cases, extra time is required for the complete health recovery of the patient. There are some cases when an addicted patient needs psychological counseling for controlling habits and adopting a healthy lifestyle. A complex case can be stated as when there is a dependency between the diseases, which may require specialist treatment. Even though it is a rare case to extend discharge time for the secondary disease, it needs to be cured. When a patient may have to stay for the secondary disease for more time than expected initially, the hospital must provide necessary support for such extension. Ultimately, it is recommended by the doctor to cure completely rather than schedule follow-up for the diagnosis and treatments. Pneumonia is the third of the top ten causes of death in Taiwan as well as in the world. The longer the hospital stay, the more likely it is to cause complications, hypoxemia, anemia, hypoalbuminemia, etc.
- Deploying AI System in the Hospital: Considering most of the application domain, AI models help to predict a patient’s conditions but not to diagnose the patient’s outcomes. Doctors are responsible for diagnosis and taking actions with treatments, and AI helps to provide decision choice and recommendations. AI models provide high-quality recommendations for junior doctors. Hands-on experiences are one of the major parts of doctor training. Young doctors will have a high-quality baseline of patient diagnosis with the help of AI models. Moreover, it improves the patient-care quality, even saving patient’s lives. In most hospitals, doctors are a critical resource and almost overrun. It is not possible to take care of all patients at any time. Automatic patient’s data collection for AI models will strongly help the patients care for 24 h/day. If the sensitivity and specificity of AI model predictions are good enough, it will greatly relieve the loading of doctors, and provide persistent health-care service during patient’s stay period in the hospital.
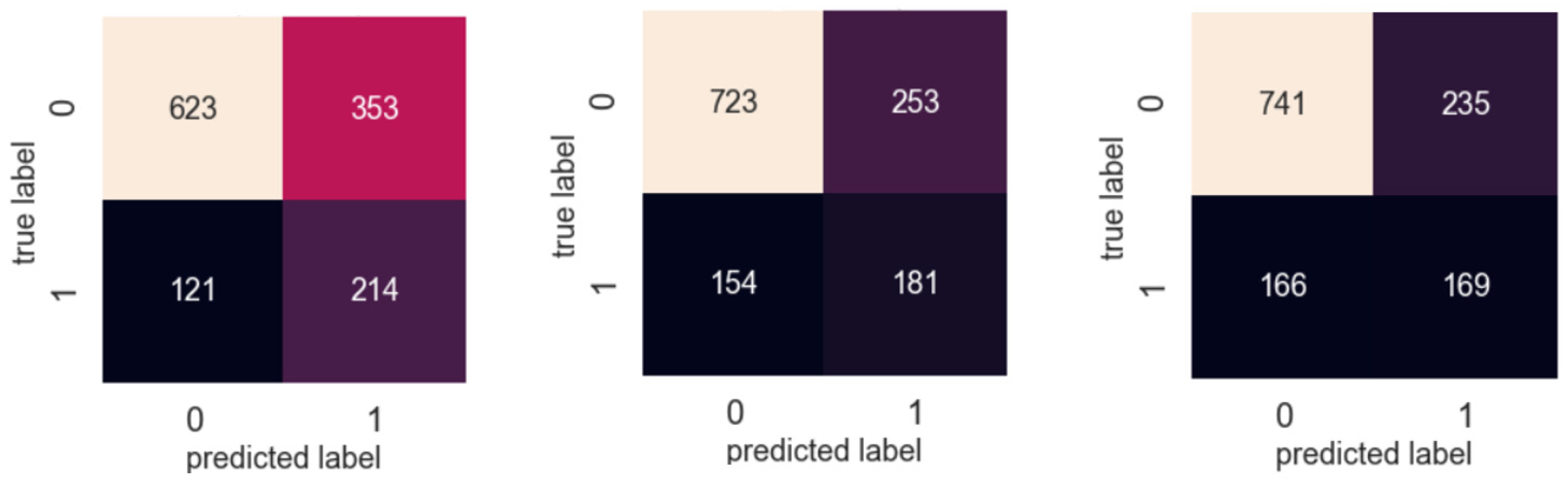
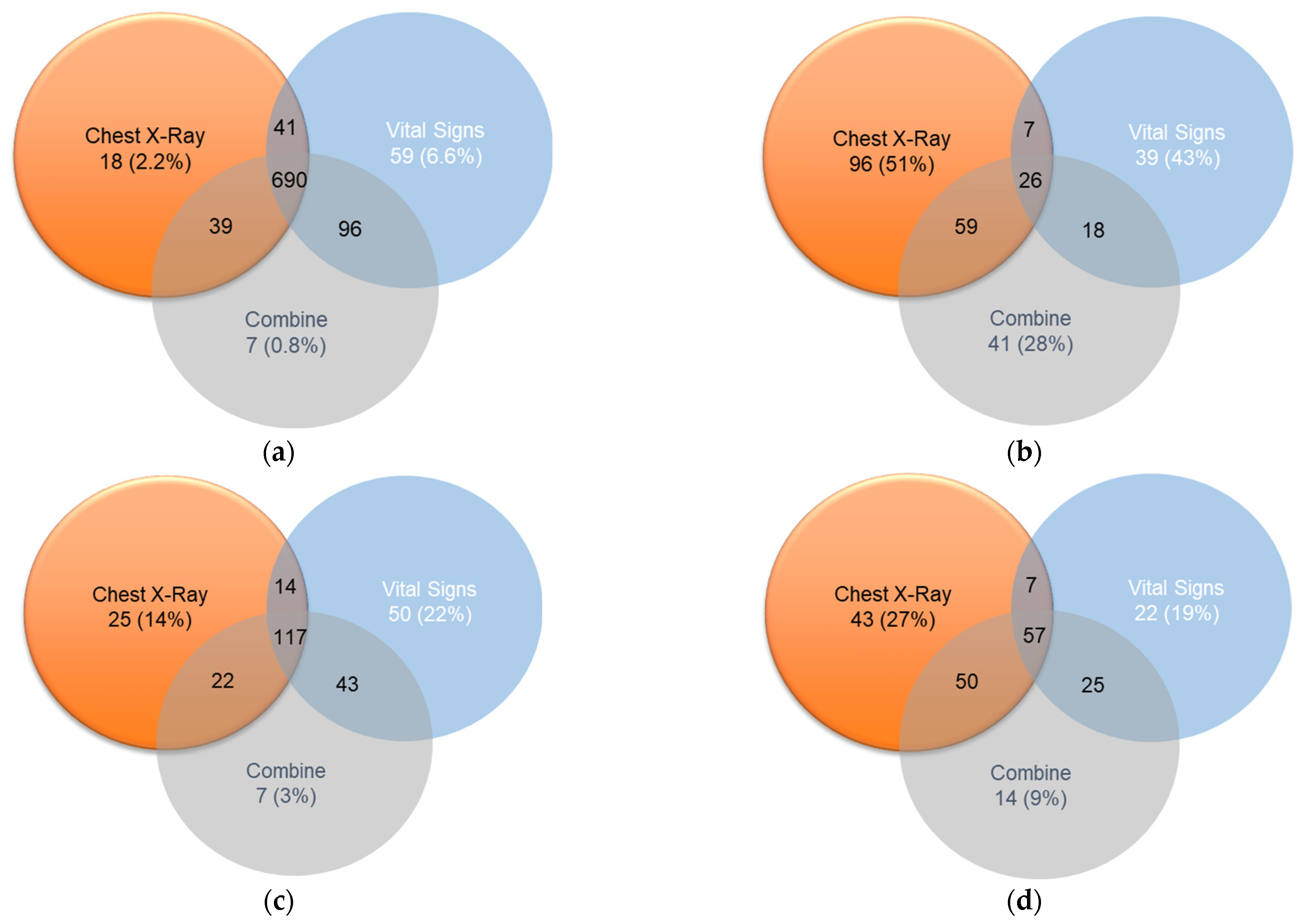
4.2. Venn Diagram Presentation for the Detail Analysis of the Prediction Results
- Cannot be discharged within seven days, the prediction is correct (true positive).
- Unable to be discharged within seven days, the prediction was wrong (false positive).
- Able to be discharged within seven days, the prediction was wrong (false negative).
- Able to be discharged within seven days, the prediction is correct (true negative).
4.3. Limitations of the Prediction System
- The medical doctors need to be trained for interpreting classification results and identifying false positive cases.
- The classification model must adapt after appending new data for training and evaluation.
- The hidden layers in the dense do not provide complete information for the doctor’s detail analysis. In the future, the system can be made more transparent at every step using explainable AI (XAI).
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
Appendix A
| Machine Learning Algorithm/Evaluations | Sensitivity | Specificity | Accuracy | F1-Score |
|---|---|---|---|---|
| Logistic Regression | 0.65 | 0.72 | 0.70 | 0.54 |
| SVM | 0.70 | 0.68 | 0.69 | 0.54 |
| Gaussian NB | 0.54 | 0.75 | 0.70 | 0.48 |
| XGBoost | 0.40 | 0.90 | 0.76 | 0.47 |
| Machine Learning Algorithm/Evaluations | Dataset | Sensitivity | Specificity | Accuracy | F1-Score |
|---|---|---|---|---|---|
| Random Forest | Vital Sign | 0.88 | 0.40 | 0.69 | 0.69 |
| XGBoost | Vital Sign | 0.91 | 0.33 | 0.76 | 0.74 |
| Feature Extraction and DNN | CXR | 0.81 | 0.47 | 0.72 | 0.72 |
| Feature Extraction and DNN | CXR and Vital Sign | 0.85 | 0.44 | 0.75 | 0.74 |
| Features/Evaluation | Precision | Recall | F1-Score | Accuracy |
|---|---|---|---|---|
| Infiltrates-Top Left | 0.58 | 0.59 | 0.57 | 0.59 |
| Infiltrates-Bottom Left | 0.63 | 0.58 | 0.57 | 0.58 |
| Infiltrates-Top Right | 0.66 | 0.67 | 0.66 | 0.67 |
| Infiltrates-Bottom Right | 0.66 | 0.67 | 0.66 | 0.67 |
| Cardiomegaly | 0.71 | 0.72 | 0.71 | 0.72 |
| Effusion Left | 0.81 | 0.81 | 0.80 | 0.81 |
| Effusion Right | 0.78 | 0.72 | 0.74 | 0.72 |
| Features/Evaluation | Precision | Recall | F1 Score | Accuracy | |||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 0 | 1 | 0 | 1 | ||
| Infiltrates-Top Left | 0.91 | 0.63 | 0.84 | 0.75 | 0.87 | 0.68 | 0.82 |
| Infiltrates-Bottom Left | 0.88 | 0.77 | 0.51 | 0.96 | 0.64 | 0.86 | 0.79 |
| Infiltrates-Top Right | 0.91 | 0.51 | 0.88 | 0.58 | 0.89 | 0.55 | 0.82 |
| Infiltrates-Bottom Right | 0.77 | 0.79 | 0.85 | 0.69 | 0.81 | 0.74 | 0.78 |
| Cardiomegaly | 0.96 | 0.71 | 0.94 | 0.81 | 0.95 | 0.76 | 0.92 |
| Effusion Left | 0.94 | 0.73 | 0.98 | 0.42 | 0.96 | 0.53 | 0.93 |
| Effusion Right | 0.95 | 0.43 | 0.98 | 0.23 | 0.96 | 0.30 | 0.93 |






Appendix B
Appendix B.1. Introduction (Extension)
Appendix B.2. Literature Survey (Extension)
- MDA-PSP uses both machine and deep learning-based algorithm to decide which approach evaluates to be effective for pneumonia prediction of the patient.
- The use of multi-modal data analysis is considered to be efficient, which was less evaluated previously.
- Mean-time analysis helps to provide recovery status within the 7th day treatment of the patient.
- The properly defined pseudo-code of the algorithms and experiments will be helpful for detailed understanding and future research, and to simulate physician diagnosis and treatment, combine images and data for machine learning, and build predictive models.
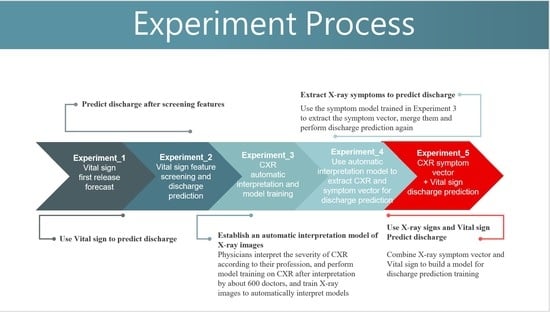
Appendix B.3. Experiments (Extension)
References
- Department of Statistics, Ministry of Health and Welfare, Taiwan’s Leading Causes of Death in 2019. 2019. Available online: https://www.mohw.gov.tw/cp-4964-55572-2.html (accessed on 11 June 2021).
- Chen, C.Z.; Fan, P.S.; Lin, C.C.; Lee, C.H.; Hsiue, T.R. Repeated pneumonia severity index measurement after admission increases its predictive value for mortality in severe community-acquired pneumonia. J. Formos. Med. Assoc. 2009, 108, 219–223. [Google Scholar] [CrossRef][Green Version]
- Chen, J.H.; Chang, S.S.; Liu, J.J.; Chan, R.C.; Wu, J.Y.; Wang, W.C.; Lee, S.H.; Lee, C.C. Comparison of clinical characteristics and performance of pneumonia severity score and CURB-65 among younger adults, elderly and very old subjects. Thorax 2010, 65, 971–977. [Google Scholar] [CrossRef]
- Lee, Y.T.; Chen, S.C.; Chan, K.C.; Wu, T.C.; Tsao, S.M.; Chan, C.H. Impact of infectious etiology on the outcome of Taiwanese patients hospitalized with community acquired pneumonia. J. Infect. Dev. Ctries. 2013, 7, 116–124. [Google Scholar] [CrossRef][Green Version]
- Song, J.H.; Oh, W.S.; Kang, C.I.; Chung, D.R.; Peck, K.R.; Ko, K.S.; Yeom, J.S.; Kim, C.K.; Kim, S.W.; Chang, H.H.; et al. Epidemiology and clinical outcomes of community-acquired pneumonia in adult patients in Asian countries: A prospective study by the Asian network for surveillance of resistant pathogens. Int. J. Antimicrob Agents 2008, 31, 107–114. [Google Scholar] [CrossRef]
- Chou, C.C.; Shen, C.F.; Chen, S.J.; Chen, H.M.; Wang, Y.C.; Chang, W.S.; Chang, Y.T.; Chen, W.Y.; Huang, C.Y.; Kuo, C.C.; et al. Recommendations and guidelines for the treatment of pneumonia in Taiwan. J. Microbiol. Immunol. Infect. 2019, 52, 172–199. [Google Scholar] [CrossRef]
- Wu, C.L.; Ku, S.C.; Yang, K.Y.; Fang, W.F.; Tu, C.Y.; Chen, C.W.; Hsu, K.H.; Fan, W.C.; Lin, M.C.; Chen, W.; et al. Antimicrobial drug-resistant microbes associated with hospitalized community-acquired and healthcare-associated pneumonia: A multi-center study in Taiwan. J. Med. Assoc. 2013, 112, 31–40. [Google Scholar] [CrossRef]
- Ngeow, Y.F.; Suwanjutha, S.; Chantarojanasriri, T.; Wang, F.; Saniel, M.; Alejandria, M.; Hsueh, P.R.; Ping-Ing, L.; Park, S.C.; Sohn, J.W.; et al. An Asian study on the prevalence of atypical respiratory pathogens in community-acquired pneumonia. Int. J. Infect. Dis. 2005, 9, 144–153. [Google Scholar] [CrossRef]
- Mandell, L.A.; Wunderink, R.G.; Anzueto, A.; Bartlett, J.G.; Campbell, G.D.; Dean, N.C.; Dowell, S.F.; File, T.M., Jr.; Musher, D.M.; Niederman, M.S.; et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. 2007, 44 (Suppl. S2), S27–S72. [Google Scholar] [CrossRef]
- Niederman, M.S.; Mandell, L.A.; Anzueto, A.; Bass, J.B.; Broughton, W.A.; Campbell, G.D.; Dean, N.; File, T.; Fine, M.J.; Gross, P.A.; et al. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am. J. Respir. Crit. Care Med. 2001, 163, 1730–1754. [Google Scholar] [CrossRef]
- Blasi, F.; Ostermann, H.; Racketa, J.; Medina, J.; McBride, K.; Garau, J.; REACH Study Group. Early versus later response to treatment in patients with community-acquired pneumonia: Analysis of the REACH study. Respir. Res. 2014, 15, 6. [Google Scholar] [CrossRef]
- Choudhury, G.; Mandal, P.; Singanayagam, A.; Akram, A.R.; Chalmers, J.D.; Hill, A.T. Seven-day antibiotic courses have similar efficacy to prolonged courses in severe community-acquired pneumonia—A propensity-adjusted analysis. Clin. Microbiol. Infect. 2011, 17, 1852–1858. [Google Scholar] [CrossRef]
- El Moussaoui, R.; De Borgie, C.A.; Van Den Broek, P.; Hustinx, W.N.; Bresser, P.; Van Den Berk, G.E.; Poley, J.W.; Van Den Berg, B.; Krouwels, F.H.; Bonten, M.J.; et al. Effectiveness of discontinuing antibiotic treatment after three days versus eight days in mild to moderate-severe community acquired pneumonia: Randomised, double blind study. BMJ 2006, 332, 1355. [Google Scholar] [CrossRef]
- Prina, E.; Ranzani, O.T.; Torres, A. Community-acquired pneumonia. Lancet 2015, 386, 1097–1108. [Google Scholar] [CrossRef]
- Aliberti, S.; Peyrani, P.; Filardo, G.; Mirsaeidi, M.; Amir, A.; Blasi, F.; Ramirez, J.A. Association between time to clinical stability and outcomes after discharge in hospitalized patients with community-acquired pneumonia. Chest 2011, 140, 482–488. [Google Scholar] [CrossRef]
- Garin, N.; Felix, G.; Chuard, C.; Genné, D.; Carballo, S.; Hugli, O.; Lamy, O.; Marti, C.; Nendaz, M.; Rutschmann, O.; et al. Predictors and Implications of Early Clinical Stability in Patients Hospitalized for Moderately Severe Community-Acquired Pneumonia. PLoS ONE 2016, 11, e0157350. [Google Scholar] [CrossRef]
- Hoogewerf, M.; Oosterheert, J.J.; Hak, E.; Hoepelman, I.M.; Bonten, M.J. Prognostic factors for early clinical failure in patients with severe community-acquired pneumonia. Clin. Microbiol. Infect. 2006, 12, 1097–1104. [Google Scholar] [CrossRef]
- Menéndez, R.; Torres, A.; Zalacaín, R.; Aspa, J.; Martín Villasclaras, J.J.; Borderías, L.; Benítez Moya, J.M.; Ruiz-Manzano, J.; Rodríguez de Castro, F.; Blanquer, J.; et al. Risk factors of treatment failure in community acquired pneumonia: Implications for disease outcome. Thorax 2004, 59, 960–965. [Google Scholar] [CrossRef]
- Rosón, B.; Carratalà, J.; Fernández-Sabé, N.; Tubau, F.; Manresa, F.; Gudiol, F. Causes and factors associated with early failure in hospitalized patients with community-acquired pneumonia. Arch. Intern. Med. 2004, 164, 502–508. [Google Scholar] [CrossRef]
- Alhasan, M.; Hasaneen, M. Digital imaging, technologies and artificial intelligence applications during COVID-19 pandemic. Comput. Med. Imaging Graph. 2021, 91, 101933. [Google Scholar] [CrossRef]
- Qin, C.; Yao, D.; Shi, Y.; Song, Z. Computer-aided detection in chest radiography based on artificial intelligence: A survey. Biomed. Eng. Online 2018, 17, 113. [Google Scholar] [CrossRef]
- Zeiberg, D.; Prahlad, T.; Nallamothu, B.K.; Iwashyna, T.J.; Wiens, J.; Sjoding, M.W. Machine learning for patient risk stratification for acute respiratory distress syndrome. PLoS ONE 2019, 14, e0214465. [Google Scholar] [CrossRef]
- Chouhan, V.; Singh, S.K.; Khamparia, A.; Gupta, D.; Tiwari, P.; Moreira, C.; Damaševičius, R.; de Albuquerque, V.H.C. A Novel Transfer Learning Based Approach for Pneumonia Detection in Chest X-ray Images. Appl. Sci. 2020, 10, 559. [Google Scholar] [CrossRef]
- Yamagata, A.; Ito, A.; Nakanishi, Y.; Ishida, T. Prognostic factors in nursing and healthcare-associated pneumonia. J. Infect. Chemother. 2020, 26, 563–569. [Google Scholar] [CrossRef]
- Zhang, J.; Xie, Y.; Pang, G.; Liao, Z.; Verjans, J.; Li, W.; Sun, Z.; He, J.; Li, Y.; Shen, C.; et al. Viral Pneumonia Screening on Chest X-Rays Using Confidence-Aware Anomaly Detection. IEEE Trans. Med. Imaging 2021, 40, 879–890. [Google Scholar] [CrossRef]
- Reamaroon, N.; Sjoding, M.W.; Lin, K.; Iwashyna, T.J.; Najarian, K. Accounting for Label Uncertainty in Machine Learning for Detection of Acute Respiratory Distress Syndrome. IEEE J. Biomed. Health Inform. 2019, 23, 407–415. [Google Scholar] [CrossRef]
- Ding, X.F.; Li, J.B.; Liang, H.Y.; Wang, Z.Y.; Jiao, T.T.; Liu, Z.; Yi, L.; Bian, W.S.; Wang, S.P.; Zhu, X.; et al. Predictive model for acute respiratory distress syndrome events in ICU patients in China using machine learning algorithms: A secondary analysis of a cohort study. J. Transl. Med. 2019, 17, 326. [Google Scholar] [CrossRef]
- Rehm, G.B.; Woo, S.H.; Chen, X.L.; Kuhn, B.T.; Cortes-Puch, I.; Anderson, N.R.; Adams, J.Y.; Chuah, C.N. Leveraging IoTs and Machine Learning for Patient Diagnosis and Ventilation Management in the Intensive Care Unit. IEEE Pervasive Comput. 2020, 19, 68–78. [Google Scholar] [CrossRef]
- Sinha, P.; Churpek, M.M.; Calfee, C.S. Machine Learning Classifier Models Can Identify Acute Respiratory Distress Syndrome Phenotypes Using Readily Available Clinical Data. Am. J. Respir. Crit. Care Med. 2020, 202, 996–1004. [Google Scholar] [CrossRef]
- Le, S.; Pellegrini, E.; Green-Saxena, A.; Summers, C.; Hoffman, J.; Calvert, J.; Das, R. Supervised machine learning for the early prediction of acute respiratory distress syndrome (ARDS). J. Crit. Care 2020, 60, 96–102. [Google Scholar] [CrossRef]
- Tsai, P.F.; Chen, P.C.; Chen, Y.Y.; Song, H.Y.; Lin, H.M.; Lin, F.M.; Huang, Q.P. Length of Hospital Stay Prediction at the Admission Stage for Cardiology Patients Using Artificial Neural Network. J. Healthc. Eng. 2016, 2016, 7035463. [Google Scholar] [CrossRef]
- Jamei, M.; Nisnevich, A.; Wetchler, E.; Sudat, S.; Liu, E. Predicting all-cause risk of 30-day hospital readmission using artificial neural networks. PLoS ONE 2017, 12, e0181173. [Google Scholar] [CrossRef]
- Ghazal, S.; Sauthier, M.; Brossier, D.; Bouachir, W.; Jouvet, P.A.; Noumeir, R. Using machine learning models to predict oxygen saturation following ventilator support adjustment in critically ill children: A single center pilot study. PLoS ONE 2019, 14, e0198921. [Google Scholar] [CrossRef]
- Yang, P.; Wu, T.; Yu, M.; Chen, F.; Wang, C.; Yuan, J.; Xu, J.; Zhang, G. A new method for identifying the acute respiratory distress syndrome disease based on noninvasive physiological parameters. PLoS ONE 2020, 15, e0226962. [Google Scholar] [CrossRef]
- Zhang, Z. Prediction model for patients with acute respiratory distress syndrome: Use of a genetic algorithm to develop a neural network model. PeerJ 2019, 7, e7719. [Google Scholar] [CrossRef]
- Afshar, M.; Joyce, C.; Oakey, A.; Formanek, P.; Yang, P.; Churpek, M.M.; Cooper, R.S.; Zelisko, S.; Price, R.; Dligach, D. A Computable Phenotype for Acute Respiratory Distress Syndrome Using Natural Language Processing and Machine Learning. AMIA Annu. Symp. Proc. 2018, 2018, 157–165. [Google Scholar]
- Rajpurkar, P.; Irvin, J.; Ball, R.L.; Zhu, K.; Yang, B.; Mehta, H.; Duan, T.; Ding, D.; Bagul, A.; Langlotz, C.P.; et al. Deep learning for chest radiograph diagnosis: A retrospective comparison of the CheXNeXt algorithm to practicing radiologists. PLoS Med. 2018, 15, e1002686. [Google Scholar] [CrossRef]
- Nguyen, H.X.; Dang, T.T. Ribs Suppression in Chest X-Ray Images by Using ICA Method. In 5th International Conference on Biomedical Engineering in Vietnam; IFMBE Proceedings; Toi, V., Lien Phuong, T., Eds.; Springer: Cham, Switzerland, 2015; Volume 46. [Google Scholar] [CrossRef]
- Gusarev, M.; Kuleev, R.; Khan, A.; Rivera, A.R.; Khattak, A.M. Deep learning models for bone suppression in chest radiographs. In Proceedings of the 2017 IEEE Conference on Computational Intelligence in Bioinformatics and Computational Biology (CIBCB), Manchester, UK, 23–25 August 2017; pp. 1–7. [Google Scholar] [CrossRef]
- Matsubara, N.; Teramoto, A.; Saito, K.; Fujita, H. Bone suppression for chest X-ray image using a convolutional neural filter. Phys. Eng. Sci. Med. 2020, 43, 97–108. [Google Scholar] [CrossRef]
- Xu, X.; Jiang, X.; Ma, C.; Du, P.; Li, X.; Lv, S.; Yu, L.; Ni, Q.; Chen, Y.; Su, J.; et al. A Deep Learning System to Screen Novel Coronavirus Disease 2019 Pneumonia. Engineering 2020, 6, 1122–1129. [Google Scholar] [CrossRef]
- Pan, F.; Ye, T.; Sun, P.; Gui, S.; Liang, B.; Li, L.; Zheng, D.; Wang, J.; Hesketh, R.L.; Yang, L.; et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef]
- Chen, J.; Wu, L.; Zhang, J.; Zhang, L.; Gong, D.; Zhao, Y.; Chen, Q.; Huang, S.; Yang, M.; Yang, X.; et al. Deep learning-based model for detecting 2019 novel coronavirus pneumonia on high-resolution computed tomography. Sci. Rep. 2020, 10, 19196. [Google Scholar] [CrossRef]
- Shi, F.; Xia, L.; Shan, F.; Song, B.; Wu, D.; Wei, Y.; Yuan, H.; Jiang, H.; He, Y.; Gao, Y.; et al. Large-scale screening of COVID-19 from community acquired pneumonia using infection size-aware classification. Phys. Med. Biol. 2021, 66, 065031. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Erion, G.G.; Lee, S.I. Consistent individualized feature attribution for tree ensembles. arXiv 2018, arXiv:1802.03888. [Google Scholar]
- Huang, G.; Liu, Z.; Van Der Maaten, L.; Weinberger, K.Q. Densely connected convolutional networks. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Honolulu, HI, USA, 21–26 July 2017; pp. 4700–4708. [Google Scholar]
- Zhu, Y.; Newsam, S. Densenet for dense flow. In Proceedings of the 2017 IEEE International Conference on Image Processing (ICIP), Beijing, China, 17–20 September 2017; pp. 790–794. [Google Scholar] [CrossRef]
- Abd-Alrazaq, A.; Schneider, J.; Mifsud, B.; Alam, T.; Househ, M.; Hamdi, M.; Shah, Z. A Comprehensive Overview of the COVID-19 Literature: Machine Learning—Based Bibliometric Analysis. J. Med. Internet. Res. 2021, 23, e23703. [Google Scholar] [CrossRef]
- Yu, C.S.; Chang, S.S.; Chang, T.H.; Wu, J.L.; Lin, Y.J.; Chien, H.F.; Chen, R.J. A COVID-19 Pandemic Artificial Intelligence–Based System With Deep Learning Forecasting and Automatic Statistical Data Acquisition: Development and Implementation Study. J. Med. Internet Res. 2021, 23, e27806. [Google Scholar] [CrossRef]
- Suzuki, R.; Suzuki, T.; Tsuji, S.; Fujiwara, K.; Yamashina, H.; Endoh, A.; Ogasawara, K. A Bayesian Network–Based Browsing Model for Patients Seeking Radiology-Related Information on Hospital Websites: Development and Usability Study. J. Med. Internet Res. 2021, 23, e14794. [Google Scholar] [CrossRef]
- Bezemer, T.; de Groot, M.C.H.; Blasse, E.; ten Berg, M.J.; Kappen, T.H.; Bredenoord, A.L.; van Solinge, W.W.; Hoefer, I.E.; Haitjema, S. A Human(e) Factor in Clinical Decision Support Systems. J. Med. Internet Res. 2019, 21, e11732. [Google Scholar] [CrossRef]


| References | Study Aims | Source/ Input Data | Preprocessing/ Statistical Analysis | Machine Learning/Deep Learning Algorithms | Evaluation |
|---|---|---|---|---|---|
| D. Zeiberg et al. 2019 [22] | A machine learning approach to risk stratifying patients for ARDS. | Electronic Health Record (EHR) | 5-fold cross validation and categorical data transforms. | Extreme gradient boosted (XGBoost) decision tree model. | AUROC |
| V. Chouhan et al. 2020 [23] | Pneumonia prediction using ensemble model. | CXR dataset, pre-trained on ImageNet. | Augmentation techniques: Random Horizontal Flip, Random Resized Crop, and Varying Intensity. | AlexNet, DenseNet121, ResNet18, InceptionV3, and GoogLeNet. | Area under the receiver operating characteristic curve (AUROC) |
| A. Yamagata et al. 2020 [24] | To investigate the prognostic factors related to 30-day mortality in patients. | Nursing and healthcare-associated pneumonia | Student’s t-test and chi-squared test | Univariate analysis and multivariate analysis using stepwise logistic regression. | p value |
| J. Zhang et al. 2020 [25] | A confidence aware anomaly detection (CAAD) model, with a shared feature extractor, an anomaly detection module, and a confidence prediction module for viral pneumonia. | CXR Dataset | Weights in ImageNet | CAAD model/Dense-Net and One-Class SVM (OC-SVM). | AUC, accuracy, sensitivity, and specificity. |
| MDA-PSP | Pneumonia status prediction for patient discharge within 7 days or not. | Vital Signs and CXR | Standard Scalar, SHAP, imputation, adaptive imputation, and SMOTE. | Dense-BN with class weights, dense layers, XGBoost, RF, SVM, and decision tree. | Precision, recall, F1 score, and accuracy. |
| Serial No. | Vital Sign | Range (Total = 3972) | Mean (within 7 Days–after 7 Days) | Median (within 7 Days–after 7 Days) | Mode (within 7 Days–after 7 Days) | |||
|---|---|---|---|---|---|---|---|---|
| 1 | Age | 18–106 | 65.09 | 72.88 | 66 | 76 | 62 | 88 |
| 2 | Gender (M:1) | 64% | 62% | 65% | 1 | 1 | 1 | 1 |
| 3 | Glutamic-Oxalacetic Transaminase (GOT U/L) | 6–1251 | 28.17 | 29.95 | 23 | 23 | 23 | 23 |
| 4 | Glutamic-Pyruvic Transaminase (GPT U/L) | 0–1488 | 29.77 | 30.36 | 22.5 | 22.5 | 30 | 30 |
| 5 | White Blood Cell (WBC/μL) | 80–70,630 | 10,425.45 | 11,536.66 | 9620 | 10,500 | 7250 | 7250 |
| 6 | Hemoglobin (HGB g/dL) | 4.6–20.9 | 12.23 | 11.48 | 12.5 | 11.4 | 14 | 11 |
| 7 | Platelets (PLT × 1000/μL) | 3–1066 | 228.36 | 237.42 | 217 | 220 | 275 | 275 |
| 8 | Sodium (Na meq/L) | 100–163 | 135.58 | 135 | 136 | 136 | 136 | 136 |
| 9 | Potassium (K meq/L) | 1.7–6.5 | 3.88 | 3.93 | 3.8 | 3.9 | 3.7 | 4 |
| 10 | Blood Urea Nitrogen (BUN mg/dL) | 3–167 | 21 | 25.43 | 16 | 19 | 15 | 15 |
| 11 | Creatinine (Cr mg/dL) | 0.05–19.03 | 1.39 | 1.47 | 0.98 | 1.05 | 1.05 | 1.05 |
| 12 | C-Reactive Protein (CRP mg/dL) | 0.004–52.16 | 7.85 | 9.41 | 5.78 | 7.28 | 0.15 | 0.15 |
| 13 | Glucose (Glu mg/dL) | 13–1048 | 131.62 | 147.24 | 114 | 123 | 95 | 95 |
| 14 | Respiratory Rate (RR /min) | |||||||
| Day 1 | 17–100 | 20.45 | 21.75 | 20 | 20 | 20 | 20 | |
| Day 2 | 14–120 | 20.24 | 21.65 | 20 | 20 | 20 | 20 | |
| Day 3 | 12–116 | 19.87 | 21.53 | 20 | 20 | 20 | 20 | |
| 15 | Systolic Blood Pressure (SBP mmHg) | |||||||
| Day 1 | 74–220 | 126.37 | 127.31 | 124 | 125 | 110 | 109 | |
| Day 2 | 73–222 | 127.79 | 128.65 | 125 | 127 | 117 | 118 | |
| Day 3 | 75–229 | 127.90 | 129.83 | 127 | 128 | 121 | 122 | |
| 16 | Diastolic Blood Pressure (DBP mmHg) | |||||||
| Day 1 | 6–108 | 62.97 | 61.03 | 62 | 60 | 56 | 60 | |
| Day 2 | 13–115 | 64.40 | 61.90 | 63 | 61 | 65 | 59 | |
| Day 3 | 0–105 | 65.32 | 63.03 | 64 | 62 | 63 | 60 | |
| 17 | Pulse (/min) | |||||||
| Day 1 | 56–901 | 102.36 | 105.93 | 100 | 104 | 100 | 100 | |
| Day 2 | 56–192 | 93.96 | 100.49 | 93 | 99 | 92 | 100 | |
| Day 3 | 53–779 | 90.20 | 97.98 | 89 | 97 | 84 | 100 | |
| 18 | BT_MIN (min °C) | |||||||
| Day 1 | 30–38.8 | 36.43 | 36.39 | 36.4 | 36.4 | 36 | 36 | |
| Day 2 | 33.1–38.4 | 36.22 | 36.26 | 36.2 | 36.2 | 36 | 36 | |
| Day 3 | 33.9–37.8 | 36.11 | 36.19 | 36.1 | 36.2 | 36 | 36 | |
| 19 | BT_MAX (max °C) | |||||||
| Day 1 | 35.4–41.4 | 38.04 | 37.95 | 38 | 37.9 | 38.1 | 37.5 | |
| Day 2 | 34.4–40.4 | 37.38 | 37.54 | 37.3 | 37.4 | 37.2 | 37.4 | |
| Day 3 | 35.2–40.3 | 36.97 | 37.27 | 36.9 | 37.2 | 36.8 | 37.2 | |
| Serial No. | Comorbidity | Mean (within 7 Days–after 7 Days) | Median (within 7 Days–after 7 Days) | Mode (within 7 Days–after 7 Days) | |||
|---|---|---|---|---|---|---|---|
| 1 | Cancer | 38.22% | 41% | 0 | 0 | 0 | 0 |
| 2 | Cardiovascular Disorder | 51.57% | 65.27% | 1 | 1 | 1 | 1 |
| 3 | Neurological Disorder (Non-Stroke) | 29.93% | 40.78% | 0 | 0 | 0 | 0 |
| 4 | Neurological Disorder (Stroke) | 16.59% | 24.36% | 0 | 0 | 0 | 0 |
| 5 | Respiratory Disorder | 59.87% | 71.95% | 1 | 1 | 1 | 1 |
| 6 | Diabetes | 22.59% | 29.29% | 0 | 0 | 0 | 0 |
| 7 | Gastroenterology | 43.85% | 54.34% | 0 | 1 | 0 | 1 |
| 8 | Renal Disorder | 33.75% | 43% | 0 | 0 | 0 | 0 |
| Clinical Feature Screening | Category | Parameters |
|---|---|---|
| Once in a Day (24 h). | 3 days’ lab data and its differences. | PaO2, pH, HGB, HCT, WBC, CRP, PCT. Cr, BUN, PLT, Ca, GLU, ALB, K, NA, GPT, GOT. and AGE. |
| Comorbidity with 0/1 value as categories | Sex, Cancer, Cardiovascular disorder, Neurological disorder (non-stroke), Neurological disorder (stroke), Respiratory disorder, Diabetes, Gastroenterology, and Renal disorder. | |
| Vital signs (3 days: 0/1 value) | RR, Pulse, SBP, DBP, and BT. | |
| Twice in a Day (Every 12 h). | 3 days’ score corresponding data. | RR, Pulse, SBP, PaO2, BT_MIN, and BT_MAX. |
| Category data. | RR, Pulse, SBP, PaO2, and BT as metric. |
| Vital Sign | Cut-Off (Normal) |
|---|---|
| ≥20 |
| <100/min |
| ≥95% |
| ≤24/min |
| ≤37.8 °C |
| >90 mmHg |
Oxygen Saturation | >90% |
| System | Workstation (Windows 10, 64-bit OS) |
|---|---|
| Processor | AMD Ryzen 9 3900XT @ 4.7 GHz |
| Memory | TridentZ RGB 32G, DDR4-3200 |
| Graphics Card (GPU) | Gigabyte AORUS RTX2080Ti 11G |
| Python Library | Numpy, Pandas, Matplotlib, Seaborn, OpenCV, and Keras. |
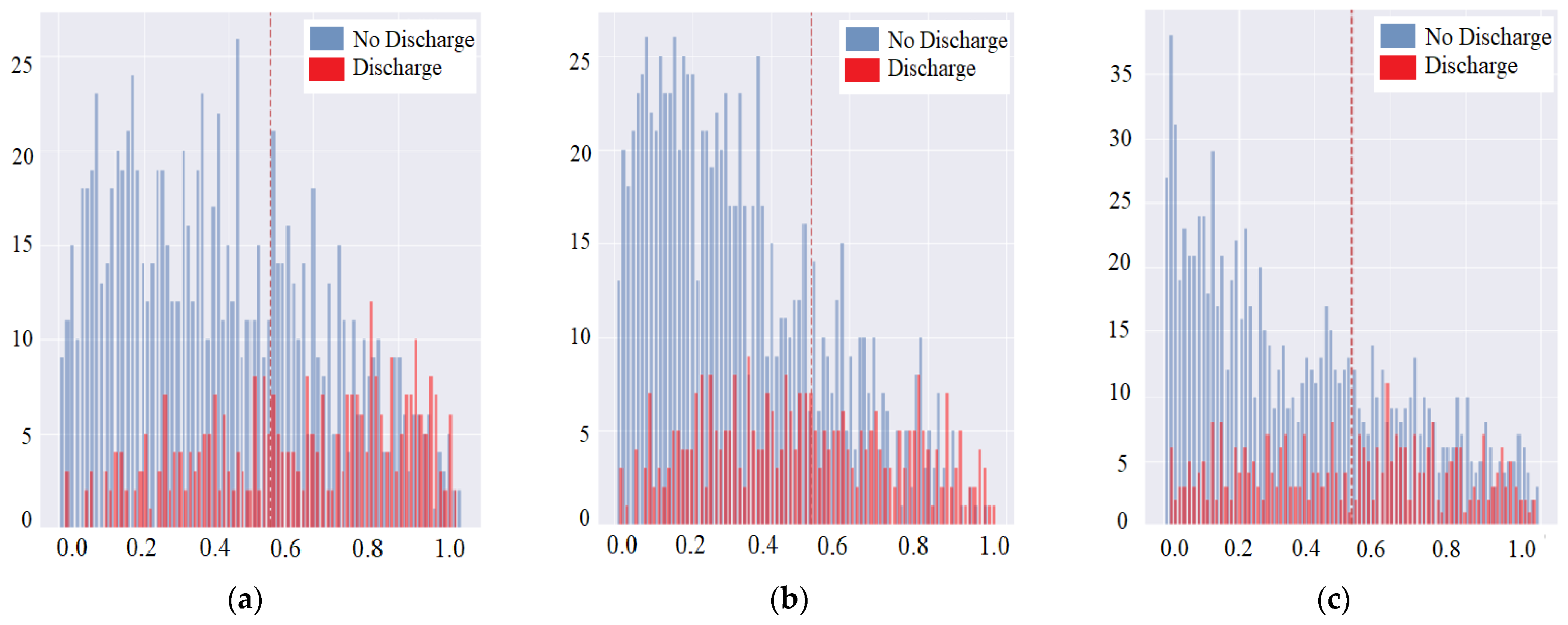
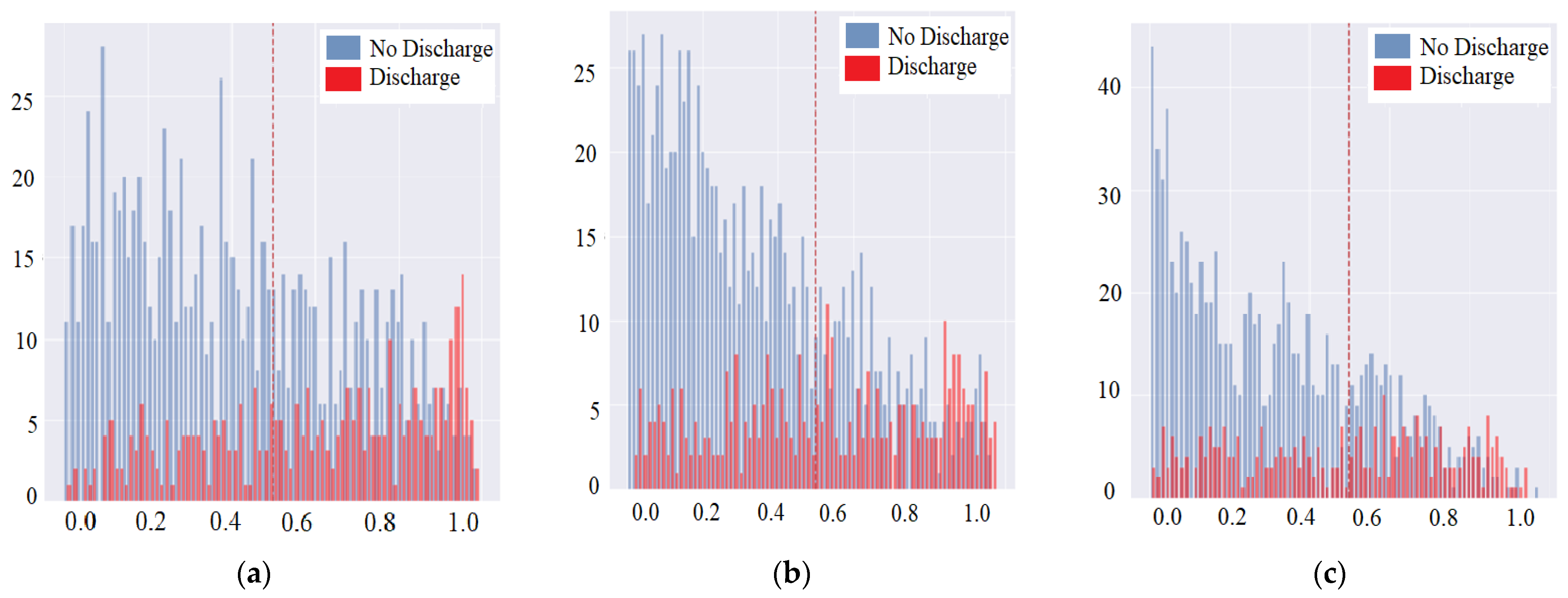
| Algorithms | Cut-off Threshold | Precision (0/1) | Sensitivity (95% CI) | Specificity (95% CI) | F1-Score (0/1) | Accuracy | PPV/NPV | AUROC (95% CI) |
|---|---|---|---|---|---|---|---|---|
| SVM | 0.3 | 0.83/0.48 | 0.51 (0.46–0.57) | 0.81 (0.78–0.83) | 0.82/0.49 | 0.73 | 0.48/0.83 | 0.64–0.68 |
| 0.5 | 0.79/0.58 | 0.27 (0.23–0.32) | 0.93 (0.91–0.95) | 0.85/0.37 | 0.76 | 0.58/0.79 | 0.58–0.63 | |
| 0.7 | 0.77/0.79 | 0.13 (0.1–0.17) | 0.99 (0.98–0.99) | 0.86/0.23 | 0.77 | 0.79/0.77 | 0.54–0.58 | |
| XGBoost | 0.3 | 0.82/0.49 | 0.45 (0.4–0.5) | 0.84 (0.81–0.86) | 0.83/0.47 | 0.74 | 0.49/0.82 | 0.62–0.67 |
| 0.5 | 0.8/0.55 | 0.33 (0.29–0.39) | 0.91 (0.89–0.92) | 0.85/0.42 | 0.76 | 0.55/0.8 | 0.6–0.64 | |
| 0.7 | 0.78/0.59 | 0.21 (0.17–0.26) | 0.95 (0.93–0.96) | 0.86/0.31 | 0.76 | 0.59/0.78 | 0.56–0.6 | |
| Random Forest | 0.3 | 0.85/0.39 | 0.66 (0.61–0.71) | 0.65 (0.62–0.68) | 0.74/0.49 | 0.65 | 0.39/0.85 | 0.63–0.68 |
| 0.5 | 0.78/0.59 | 0.21 (0.17–0.26) | 0.95 (0.94–0.96) | 0.86/0.31 | 0.76 | 0.59/0.78 | 0.56–0.6 | |
| 0.7 | 0.75/0.73 | 0.02 (0.01–0.05) | 1 (0.99–1) | 0.86/0.05 | 0.75 | 0.73/0.75 | 0.5–0.52 | |
| Decision Tree | 0.3 | 0.78/0.36 | 0.39 (0.34–0.44) | 0.77 (0.74–0.79) | 0.77/0.37 | 0.67 | 0.36/0.78 | 0.55–0.6 |
| 0.5 | 0.78/0.37 | 0.31 (0.26–0.36) | 0.82 (0.79–0.84) | 0.8/0.34 | 0.69 | 0.37/0.78 | 0.54–0.59 | |
| 0.7 | 0.78/0.39 | 0.3 (0.25–0.35) | 0.84 (0.82–0.87) | 0.81/0.34 | 0.7 | 0.39/0.78 | 0.55–0.59 | |
| Dense-BN (Accuracy) | 0.3 | 0.84/0.43 | 0.61 (0.56–0.66) | 0.72 (0.69–0.74) | 0.78/0.5 | 0.69 | 0.43/0.84 | 0.64–0.69 |
| 0.5 | 0.8/0.49 | 0.35 (0.3–0.4) | 0.88 (0.86–0.9) | 0.84/0.41 | 0.74 | 0.49/0.8 | 0.59–0.63 | |
| 0.7 | 0.77/0.64 | 0.17 (0.13–0.21) | 0.97 (0.96–0.98) | 0.86/0.27 | 0.76 | 0.64/0.77 | 0.55–0.59 | |
| Dense-BN (Loss) | 0.3 | 0.85/0.41 | 0.66 (0.61–0.71) | 0.67 (0.64–0.7) | 0.75/0.51 | 0.67 | 0.41/0.85 | 0.64–0.69 |
| 0.5 | 0.81/0.47 | 0.44 (0.39–0.49) | 0.83 (0.8–0.85) | 0.82/0.45 | 0.73 | 0.47/0.81 | 0.61–0.66 | |
| 0.7 | 0.78/0.58 | 0.23 (0.19–0.28) | 0.94 (0.93–0.96) | 0.85/0.33 | 0.76 | 0.58/0.78 | 0.57–0.61 |
| Feature Category | Label |
|---|---|
| 1. CXR | (Quality) 1: Good, 2: Medium, and 3: Bad. |
| 2. Infiltrate (Location: 1: Top Left, 2: Bottom Left, 3: Top Right, and 4: Bottom Right) | (Symptoms) 0: Normal, 1: Slight, 2: Medium, and 3: Severe. |
| 3. Cardiomegaly | (Symptoms) 0: Normal, 1: Slight, 2: Medium, and 3: Severe. |
| Symptoms/Evaluations | Precision | Recall | F1 Score | Accuracy | |||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 0 | 1 | 0 | 1 | ||
| Infiltrate–1 | 0.91 | 0.63 | 0.84 | 0.75 | 0.87 | 0.68 | 0.82 |
| Infiltrate–2 | 0.88 | 0.77 | 0.51 | 0.96 | 0.64 | 0.86 | 0.79 |
| Infiltrate–3 | 0.91 | 0.51 | 0.88 | 0.58 | 0.89 | 0.55 | 0.82 |
| Infiltrate–4 | 0.77 | 0.79 | 0.85 | 0.69 | 0.81 | 0.74 | 0.78 |
| Cardiomegaly | 0.96 | 0.71 | 0.94 | 0.81 | 0.95 | 0.76 | 0.92 |
| Symptoms/Evaluations | Precision | Recall | F1 Score | Accuracy | |||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 0 | 1 | 0 | 1 | ||
| 4 infiltrates with cardiomegaly by class weight [0.68335901, 1.86344538] | 0.81 | 0.50 | 0.85 | 0.44 | 0.83 | 0.47 | 0.75 |
| 4 infiltrates with cardiomegaly by no class weights | 0.79 | 0.60 | 0.94 | 0.28 | 0.86 | 0.38 | 0.77 |
| Confusion Matrix / Evaluations | Chest X-ray (A) | Vital Sign (B) | Combine Image/Feature Points | |||||
|---|---|---|---|---|---|---|---|---|
| A | B | A ⋂ B | ||||||
| 4 Features | 7 Features | 4 Features | 7 Features | 4 Features | 7 Features | |||
| TP | 788 | 886 | 4.754 | 5.421 | 4.384 | 4.881 | 5.32 | 6.549 |
| FP | 188 | 90 | 4.384 | 4.881 | 4.754 | 5.421 | 3.985 | 4.303 |
| FN | 178 | 224 | 4.564 | 5.202 | 5.141 | 6.328 | 3.763 | 4.226 |
| TN | 157 | 111 | 3.763 | 4.226 | 4.564 | 5.202 | 3.391 | 3.57 |
| Confusion Matrix/ Evaluations | Chest X-ray (A) | Vital Sign (B) | Combine (C) | Combine Image/Feature Points | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | A ⋂ B | B ⋂ C | A ⋂ C | A ⋂ B ⋂ C | |||||||||||
| 4 F | 7 F | 4 F | 7 F | 4 F | 7 F | 4 F | 7 F | 4 F | 7 F | 4 F | 7 F | 4 F | 7 F | ||||
| TP | 788 | 886 | 832 | 4.22 | 4.56 | 3.98 | 4.37 | 4.07 | 4.71 | 4.51 | 5.23 | 4.63 | 5.19 | 5.0 | 5.82 | 5.37 | 6.63 |
| FP | 188 | 90 | 144 | 4.63 | 5.19 | 5.0 | 5.82 | 4.51 | 5.23 | 4.07 | 4.71 | 4.22 | 4.56 | 3.98 | 4.37 | 3.96 | 4.19 |
| FN | 178 | 224 | 189 | 4.36 | 4.88 | 3.57 | 3.84 | 3.64 | 3.93 | 4.29 | 5.47 | 3.99 | 4.67 | 4.79 | 5.57 | 5.24 | 6.43 |
| TN | 157 | 111 | 146 | 3.99 | 4.67 | 4.79 | 5.57 | 4.29 | 5.46 | 3.64 | 3.93 | 4.36 | 4.88 | 3.57 | 3.84 | 3.36 | 3.53 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheu, R.-K.; Chen, L.-C.; Wu, C.-L.; Pardeshi, M.S.; Pai, K.-C.; Huang, C.-C.; Chen, C.-Y.; Chen, W.-C. Multi-Modal Data Analysis for Pneumonia Status Prediction Using Deep Learning (MDA-PSP). Diagnostics 2022, 12, 1706. https://doi.org/10.3390/diagnostics12071706
Sheu R-K, Chen L-C, Wu C-L, Pardeshi MS, Pai K-C, Huang C-C, Chen C-Y, Chen W-C. Multi-Modal Data Analysis for Pneumonia Status Prediction Using Deep Learning (MDA-PSP). Diagnostics. 2022; 12(7):1706. https://doi.org/10.3390/diagnostics12071706
Chicago/Turabian StyleSheu, Ruey-Kai, Lun-Chi Chen, Chieh-Liang Wu, Mayuresh Sunil Pardeshi, Kai-Chih Pai, Chien-Chung Huang, Chia-Yu Chen, and Wei-Cheng Chen. 2022. "Multi-Modal Data Analysis for Pneumonia Status Prediction Using Deep Learning (MDA-PSP)" Diagnostics 12, no. 7: 1706. https://doi.org/10.3390/diagnostics12071706
APA StyleSheu, R.-K., Chen, L.-C., Wu, C.-L., Pardeshi, M. S., Pai, K.-C., Huang, C.-C., Chen, C.-Y., & Chen, W.-C. (2022). Multi-Modal Data Analysis for Pneumonia Status Prediction Using Deep Learning (MDA-PSP). Diagnostics, 12(7), 1706. https://doi.org/10.3390/diagnostics12071706