Nonlinear and Linear Measures in the Differentiation of Postural Control in Patients after Total Hip or Knee Replacement and Healthy Controls
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Ethical Approval
2.3. Measurement Methods
2.4. Calculation Methods
2.5. Statistical Analysis
3. Results
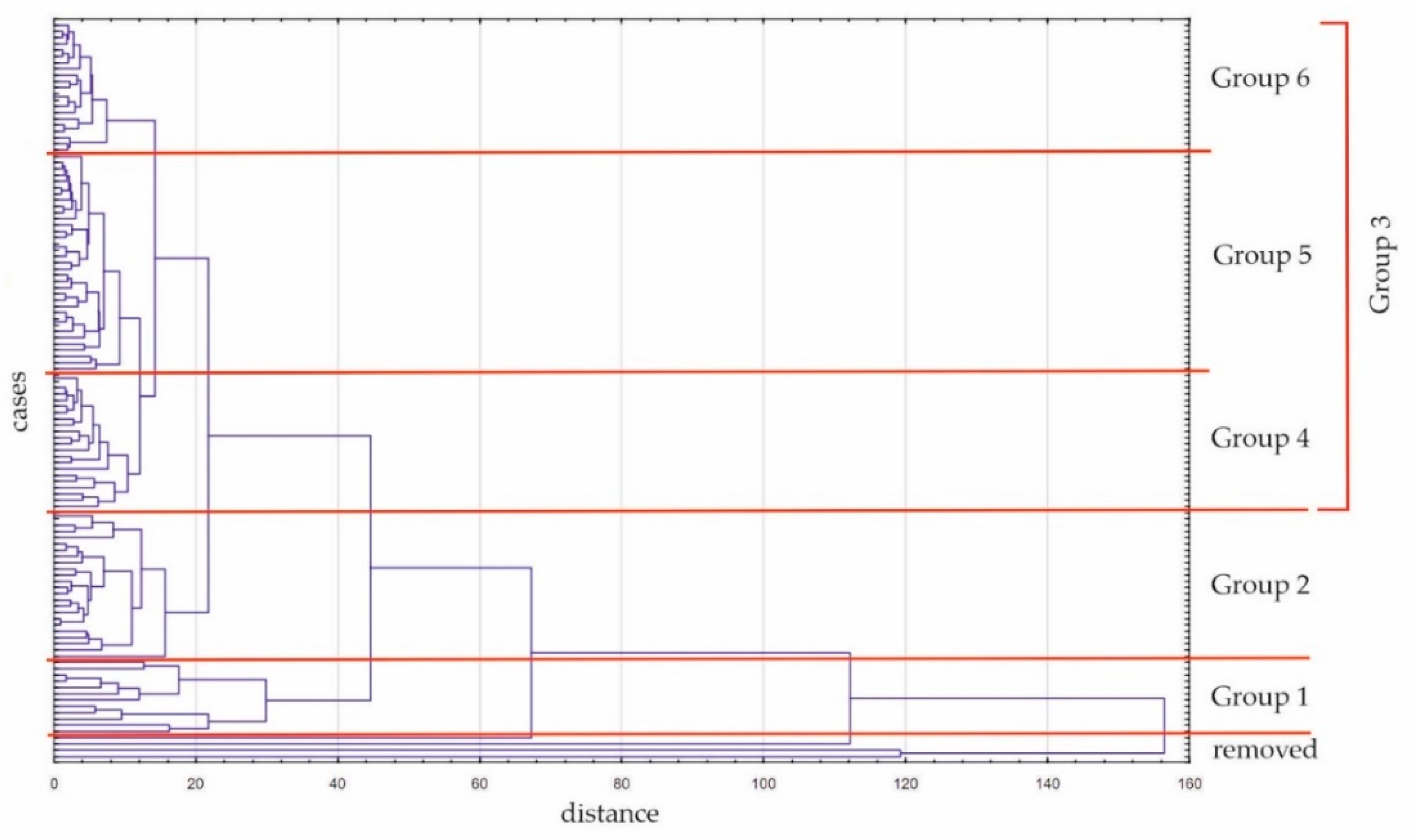
3.1. Cluster Analysis
3.2. Discriminant Analysis
3.3. Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- de Lima, F.; Melo, G.; Fernandes, D.A.; Santos, G.M.; Rosa Neto, F. Effects of total knee arthroplasty for primary knee osteoarthritis on postural balance: A systematic review. Gait Posture 2021, 89, 139–160. [Google Scholar] [CrossRef] [PubMed]
- Gianola, S.; Stucovitz, E.; Castellini, G.; Mascali, M.; Vanni, F.; Tramacere, I.; Banfi, G.; Tornese, D. Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: A randomized controlled trial. Medicine 2020, 99, e19136. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Hunter, D.J.; Vesentini, G.; Pozzobon, D.; Ferreira, M.L. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 506. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA 2021, 325, 568–578. [Google Scholar] [CrossRef]
- Prvu Bettger, J.; Green, C.L.; Holmes, D.N.; Chokshi, A.; Mather, R.C., III; Hoch, B.T.; de Leon, A.J.; Aluisio, F.; Seyler, T.M.; Del Gaizo, D.J.; et al. Effects of Virtual Exercise Rehabilitation In-Home Therapy Compared with Traditional Care After Total Knee Arthroplasty: VERITAS, a Randomized Controlled Trial. JBJS 2020, 102, 101–109. [Google Scholar] [CrossRef]
- Inacio, M.C.S.; Paxton, E.W.; Graves, S.E.; Namba, R.S.; Nemes, S. Projected increase in total knee arthroplasty in the United States—An alternative projection model. Osteoarthr. Cartil. 2017, 25, 1797–1803. [Google Scholar] [CrossRef]
- Hadamus, A.; Białoszewski, D.; Błażkiewicz, M.; Kowalska, A.J.; Urbaniak, E.; Wydra, K.T.; Wiaderna, K.; Boratyński, R.; Kobza, A.; Marczyński, W. Assessment of the Effectiveness of Rehabilitation after Total Knee Replacement Surgery Using Sample Entropy and Classical Measures of Body Balance. Entropy 2021, 23, 164. [Google Scholar] [CrossRef]
- Ohlendorf, D.; Lehmann, C.; Heil, D.; Hörzer, S.; Kopp, S. The impact of a total hip replacement on jaw position, upper body posture and body sway. Cranio J. Craniomandib. Pract. 2015, 33, 107–114. [Google Scholar] [CrossRef]
- Heil, L.; Maltry, L.; Lehmann, S.; Heil, D.; Lehmann, C.; Kopp, S.; Wanke, E.M.; Bendels, M.H.K.; Groneberg, D.A.; Ohlendorf, D. The impact of a total knee arthroplasty on jaw movements, upper body posture, plantar pressure distribution, and postural control. Cranio J. Craniomandib. Pract. 2021, 39, 35–46. [Google Scholar] [CrossRef]
- Truszczyńska-Baszak, A.; Dadura, E.; Drzał-Grabiec, J.; Tarnowski, A. Static balance assessment in patients with severe osteoarthritis of the knee. Knee 2020, 27, 1349–1356. [Google Scholar] [CrossRef]
- Gauchard, G.C.; Vançon, G.; Meyer, P.; Mainard, D.; Perrin, P.P. On the role of knee joint in balance control and postural strategies: Effects of total knee replacement in elderly subjects with knee osteoarthritis. Gait Posture 2010, 32, 155–160. [Google Scholar] [CrossRef] [PubMed]
- de Lima, F.; Fernandes, D.A.; Melo, G.; de Roesler, C.R.M.; Neves, F.D.S.; Neto, F.R. Effects of total hip arthroplasty for primary hip osteoarthritis on postural balance: A systematic review. Gait Posture 2019, 73, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Navarro, F.; Igual-Camacho, C.; Silvestre-Muñoz, A.; Roig-Casasús, S.; Blasco, J.M. Effects of balance and proprioceptive training on total hip and knee replacement rehabilitation: A systematic review and meta-analysis. Gait Posture 2018, 62, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Massion, J. Postural control system. Curr. Opin. Neurobiol. 1994, 4, 877–887. [Google Scholar] [CrossRef]
- Kiemel, T.; Elahi, A.J.; Jeka, J.J. Identification of the plant for upright stance in humans: Multiple movement patterns from a single neural strategy. J. Neurophysiol. 2008, 100, 3394–3406. [Google Scholar] [CrossRef]
- Assländer, L.; Peterka, R.J. Sensory reweighting dynamics in human postural control. J. Neurophysiol. 2014, 111, 1852–1864. [Google Scholar] [CrossRef]
- Ivanenko, Y.; Gurfinkel, V.S. Human Postural Control. Front. Neurosci. 2018, 12, 171. [Google Scholar] [CrossRef]
- Kedziorek, J.; Błażkiewicz, M. Nonlinear Measures to Evaluate Upright Postural Stability: A Systematic Review. Entropy 2020, 22, 1357. [Google Scholar] [CrossRef]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. 2), ii7–ii11. [Google Scholar] [CrossRef]
- Stergiou, N. Nonlinear Analysis for Human Movement Variability; CRC Press: Boca Raton, FL, USA, 2016; pp. 1–388. [Google Scholar]
- Roerdink, M.; Hlavackova, P.; Vuillerme, N. Center-of-pressure regularity as a marker for attentional investment in postural control: A comparison between sitting and standing postures. Hum. Mov. Sci. 2011, 30, 203–212. [Google Scholar] [CrossRef]
- Donker, S.F.; Roerdink, M.; Greven, A.J.; Beek, P.J. Regularity of center-of-pressure trajectories depends on the amount of attention invested in postural control. Exp. Brain Res. 2007, 181, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Potvin-Desrochers, A.R.; Lajoie, Y.N. Cognitive task promote automatization of postural control in young and older adults. Gait Posture 2017, 57, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.; Wei, Q.; Shieh, J.-S.; Fourcade, P.; Isableu, B.; Majed, L. Sample Entropy, Univariate, and Multivariate Multi-Scale Entropy in Comparison with Classical Postural Sway Parameters in Young Healthy Adults. Front. Hum. Neurosci. 2017, 11, 206. [Google Scholar] [CrossRef] [PubMed]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Postural control strategies during single limb stance following acute lateral ankle sprain. Clin. Biomech. 2014, 29, 643–649. [Google Scholar] [CrossRef]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Balance failure in single limb stance due to ankle sprain injury: An analysis of center of pressure using the fractal dimension method. Gait Posture 2014, 40, 172–176. [Google Scholar] [CrossRef]
- Rosenstein, M.T.; Collins, J.J.; De Luca, C.J. A practical method for calculating largest Lyapunov exponents from small data sets. Phys. D Nonlinear Phenom. 1993, 65, 117–134. [Google Scholar] [CrossRef]
- Nagymate, G.; Kiss, R. Parameter Reduction in the Frequency Analysis of Center of Pressure in Stabilometry. Period. Polytech. Mech. Eng. 2016, 60, 238–246. [Google Scholar] [CrossRef]
- Goldberger, A.L.; Amaral, L.A.; Glass, L.; Hausdorff, J.M.; Ivanov, P.C.; Mark, R.G.; Mietus, J.E.; Moody, G.B.; Peng, C.K.; Stanley, H.E. PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals. Circulation 2000, 101, E215–E220. [Google Scholar] [CrossRef]
- Higuchi, T. Approach to an irregular time series on the basis of the fractal theory. Phys. D Nonlinear Phenom. 1988, 31, 277–283. [Google Scholar] [CrossRef]
- Razjouyan, J.; Shahriar, G.; Fallah, A.; Khayat, O.; Ghergherehchi, M.; Afarideh, H.; Moghaddasi, M. A neuro-fuzzy based model for accurate estimation of the Lyapunov exponents of an unknown dynamical system. Int. J. Bifurc. Chaos Appl. Sci. Eng. 2012, 22, 1250043. [Google Scholar] [CrossRef]
- Rigoldi, C.; Cimolin, V.; Camerota, F.; Celletti, C.; Albertini, G.; Mainardi, L.; Galli, M. Measuring regularity of human postural sway using approximate entropy and sample entropy in patients with Ehlers-Danlos syndrome hypermobility type. Res. Dev. Disabil. 2013, 34, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Błażkiewicz, M. Nonlinear measures in posturography compared to linear measures based on yoga poses performance. Acta Bioeng. Biomech. 2020, 22, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Ghofrani, M.; Olyaei, G.; Talebian, S.; Bagheri, H.; Malmir, K. Test-retest reliability of linear and nonlinear measures of postural stability during visual deprivation in healthy subjects. J. Phys. Ther. Sci. 2017, 29, 1766–1771. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huisinga, J.M.; Yentes, J.M.; Filipi, M.L.; Stergiou, N. Postural control strategy during standing is altered in patients with multiple sclerosis. Neurosci. Lett. 2012, 524, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhang, X.; Lockhart, T.E. Fall risk assessments based on postural and dynamic stability using inertial measurement unit. Saf. Health Work 2012, 3, 192–198. [Google Scholar] [CrossRef]
- Szafraniec, R.; Barańska, J.; Kuczyński, M. Acute effects of core stability exercises on balance control. Acta Bioeng. Biomech. 2018, 20, 145–151. [Google Scholar]
- Montesinos, L.; Castaldo, R.; Pecchia, L. On the use of approximate entropy and sample entropy with centre of pressure time-series. J. Neuroeng. Rehabil. 2018, 15, 116. [Google Scholar] [CrossRef]
- Borg, F.G.; Laxaback, G. Entropy of balance—Some recent results. J. Neuroeng. Rehabil. 2010, 7, 38. [Google Scholar] [CrossRef]
- Raffalt, P.C.; Spedden, M.E.; Geertsen, S.S. Dynamics of postural control during bilateral stance—Effect of support area, visual input and age. Hum. Mov. Sci. 2019, 67, 102462. [Google Scholar] [CrossRef]
| H Group (N = 49) | K Group (N = 53) | C Group (N = 19) | |
|---|---|---|---|
| Gender | 28 women, 21 men | 34 women, 19 men | 15 women, 1 man |
| Age (years) | 63.7 ± 8.8 * HKC | 68.4 ± 6.3 * HKC | 53.0 ± 7.6 * HKC |
| Bodyweight (kg) | 81.5 ± 16.0 | 85.7 ± 16.1 * KC | 74.8 ± 16.3 * KC |
| Height (cm) | 167.5 ± 10.1 | 166.1 ± 11.5 | 164.9 ± 4.9 |
| Body Mass Index (kg/m2) | 28.8 ± 4.2 * HK | 30.9 ± 3.9 * HK,KC | 27.4 ± 5.3 * KC |
| Group 1 | Group 2 | Group 3 | |||
|---|---|---|---|---|---|
| Group 4 | Group 5 | Group 6 | |||
| H group | 0 | 8 | 13 | 20 | 8 |
| K group | 12 | 16 | 4 | 14 | 6 |
| C group | 0 | 0 | 5 | 1 | 7 |
| Variable | Wilks’ Lambda | F to Remove (2.108) | p-Value |
|---|---|---|---|
| LyE ML EO | 0.042 | 10.355 | < 0.0001 |
| FD AP EO | 0.039 | 5.671 | 0.0045 |
| CoP path_ML EC | 0.045 | 14.642 | < 0.0001 |
| LyE ML EC | 0.040 | 7.254 | 0.0011 |
| FD ML EC | 0.038 | 3.492 | 0.0339 |
| LyE AP EC | 0.041 | 8.824 | 0.0003 |
| FD AP EC | 0.037 | 1.693 | 0.1889 |
| SampEn AP EC | 0.037 | 2.795 | 0.0656 |
| % Correctly Classified | H Group (N) | K Group (N) | C Group (N) | |
|---|---|---|---|---|
| H group | 73.5 | 36 | 13 | 0 |
| K group | 71.7 | 15 | 38 | 0 |
| C group | 100 | 0 | 0 | 16 |
| together | 76.3 | 51 | 51 | 16 |
| Variable | H Group p = 0.4153 | K Group p = 0.4492 | C Group p = 0.1356 |
|---|---|---|---|
| LyE ML EO | 53.417 | 57.047 | 127.685 |
| FD AP EO | 150.088 | 142.413 | 102.269 |
| CoP path_ML EC | −0.767 | −0.770 | −1.746 |
| LyE ML EC | 37.833 | 38.242 | 99.582 |
| FD ML EC | 98.003 | 98.237 | 129.198 |
| LyE AP EC | −0.788 | 3.063 | 44.772 |
| FD AP EC | 257.086 | 263.192 | 249.053 |
| SampEn AP EC | −225.615 | −220.608 | −177.377 |
| const. | −348.296 | −348.863 | −413.511 |
| ML | AP | |
|---|---|---|
| Test with eyes open (EO) | LyE | FD |
| Test with eyes closed (EC) | LyE, FD | CoP path, LyE, FD, SampEn |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hadamus, A.; Błażkiewicz, M.; Kowalska, A.J.; Wydra, K.T.; Grabowicz, M.; Łukowicz, M.; Białoszewski, D.; Marczyński, W. Nonlinear and Linear Measures in the Differentiation of Postural Control in Patients after Total Hip or Knee Replacement and Healthy Controls. Diagnostics 2022, 12, 1595. https://doi.org/10.3390/diagnostics12071595
Hadamus A, Błażkiewicz M, Kowalska AJ, Wydra KT, Grabowicz M, Łukowicz M, Białoszewski D, Marczyński W. Nonlinear and Linear Measures in the Differentiation of Postural Control in Patients after Total Hip or Knee Replacement and Healthy Controls. Diagnostics. 2022; 12(7):1595. https://doi.org/10.3390/diagnostics12071595
Chicago/Turabian StyleHadamus, Anna, Michalina Błażkiewicz, Aleksandra J. Kowalska, Kamil T. Wydra, Marta Grabowicz, Małgorzata Łukowicz, Dariusz Białoszewski, and Wojciech Marczyński. 2022. "Nonlinear and Linear Measures in the Differentiation of Postural Control in Patients after Total Hip or Knee Replacement and Healthy Controls" Diagnostics 12, no. 7: 1595. https://doi.org/10.3390/diagnostics12071595
APA StyleHadamus, A., Błażkiewicz, M., Kowalska, A. J., Wydra, K. T., Grabowicz, M., Łukowicz, M., Białoszewski, D., & Marczyński, W. (2022). Nonlinear and Linear Measures in the Differentiation of Postural Control in Patients after Total Hip or Knee Replacement and Healthy Controls. Diagnostics, 12(7), 1595. https://doi.org/10.3390/diagnostics12071595







