The Effectiveness of Spinal, Diaphragmatic, and Specific Stabilization Exercise Manual Therapy and Respiratory-Related Interventions in Patients with Chronic Nonspecific Neck Pain: Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Search Strategy
2.3. Assessment of Methodological Quality
2.4. Data Extraction
2.5. Data Synthesis and Analysis
2.6. Quality of Evidence
3. Results
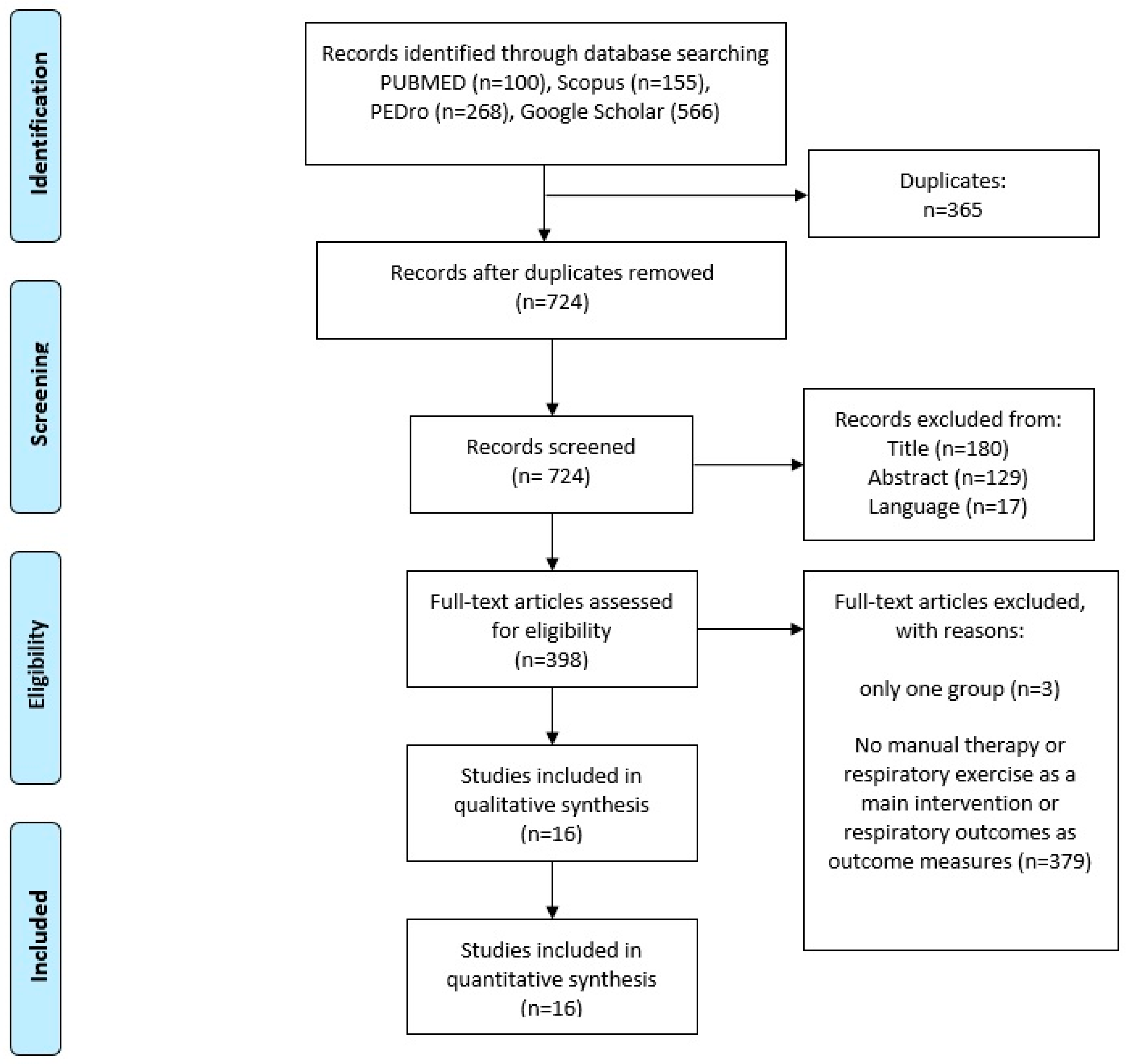
3.1. Identification of Studies
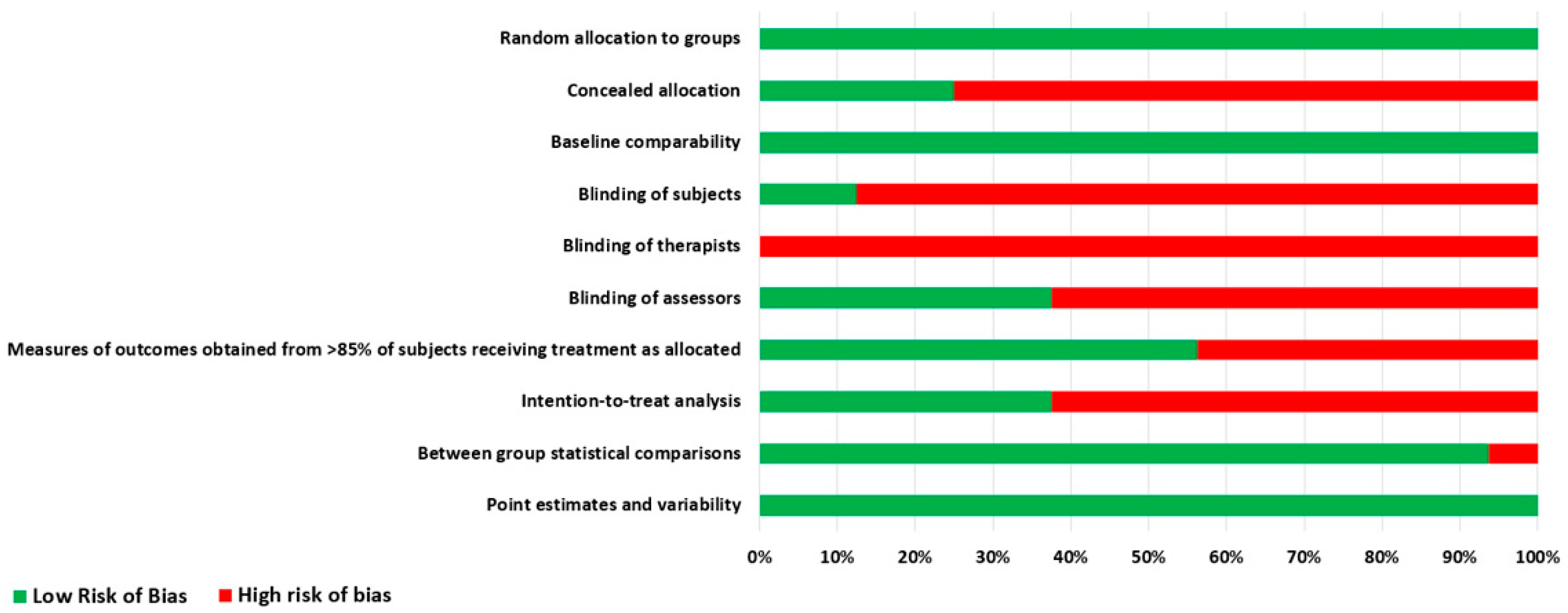
3.2. Methodological Quality
3.3. Participants
3.4. Interventions and Control Group Content
3.5. Intervention Comparability
3.6. Effects of Interventions
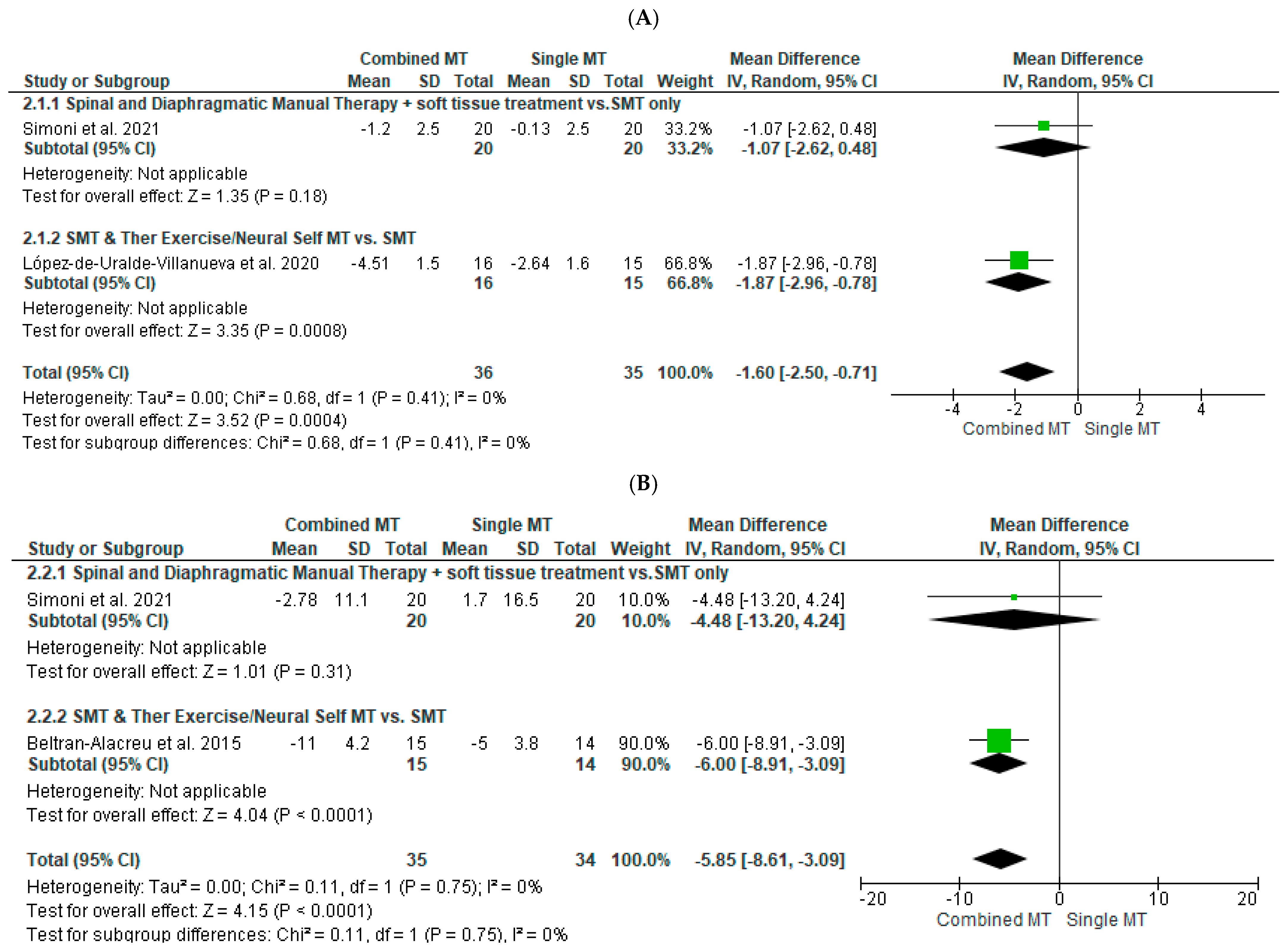
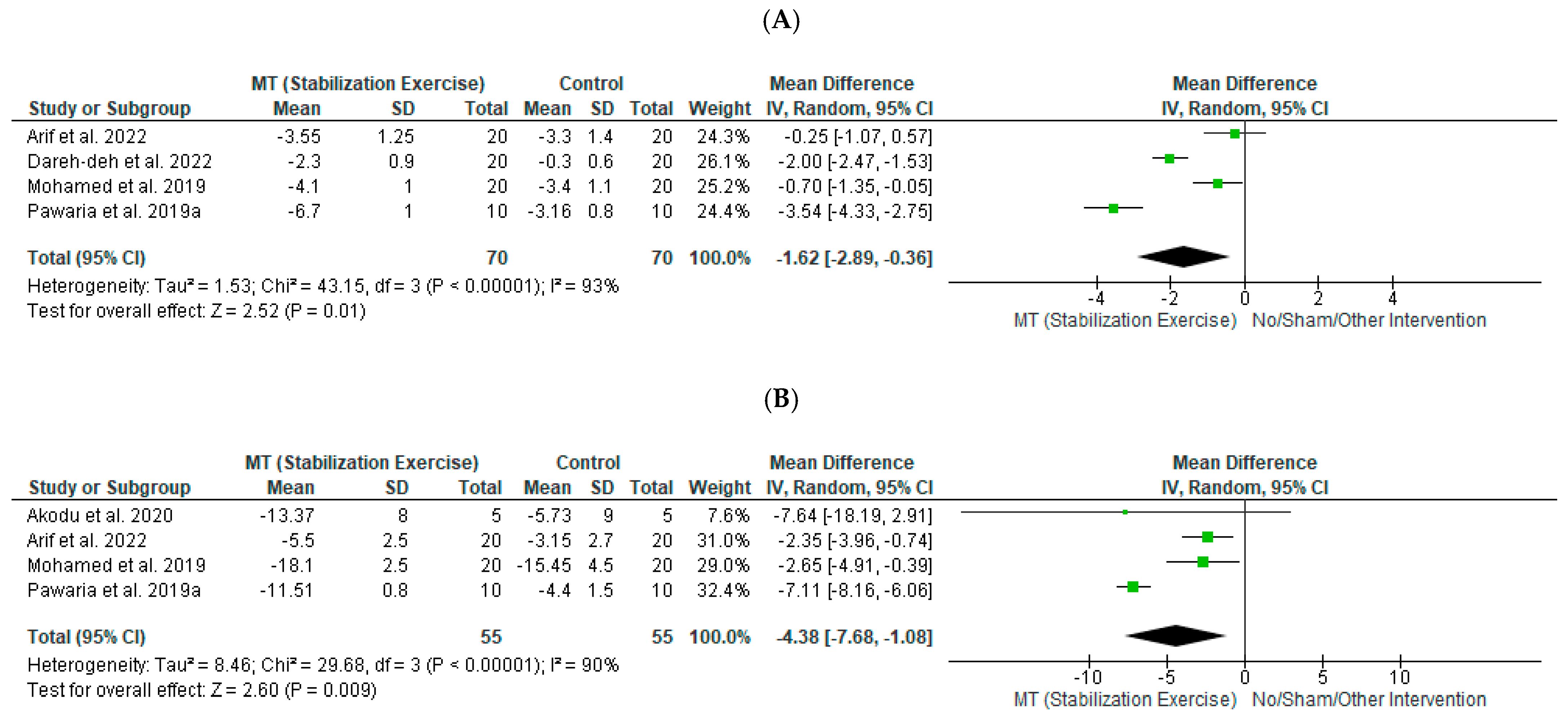
3.6.1. Effects of MT on Pain
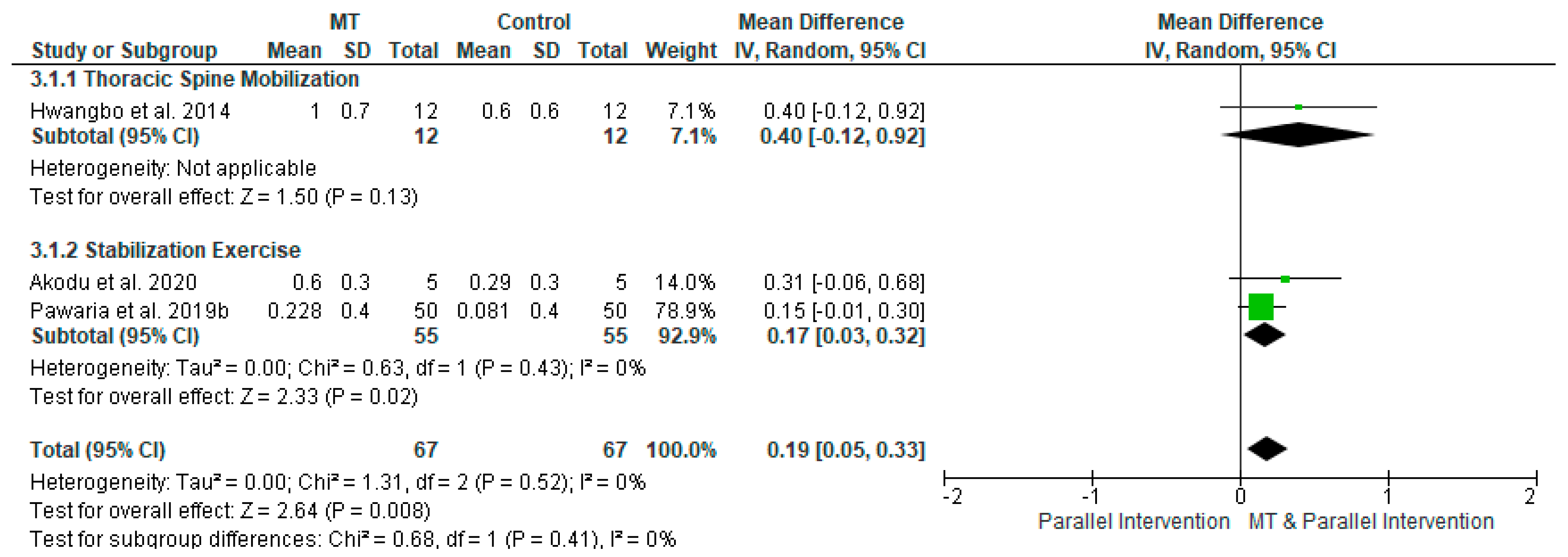
3.6.2. Effects of MT on Disability
3.6.3. Effects of MT on Respiratory Outcomes
3.6.4. Effects of RRI on Pain
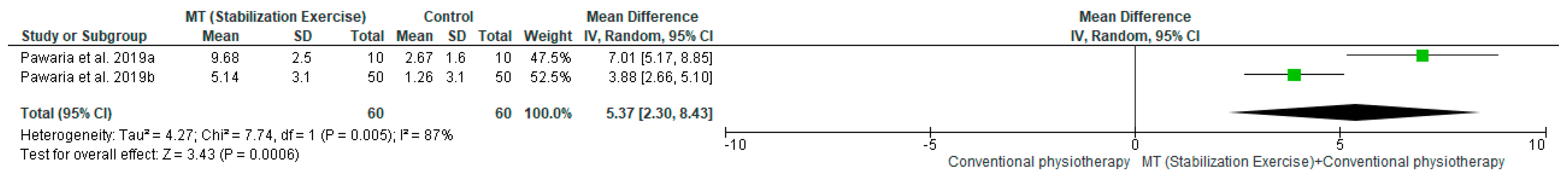
3.6.5. Effects of RRI on Disability
3.6.6. Effects of RRI on Respiratory Outcomes
4. Discussion
4.1. Clinical Considerations
4.2. Effectiveness According to Different Therapeutic Approaches
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Genebra, C.V.D.S.; Maciel, N.M.; Bento, T.P.F.; Simeão, S.F.A.P.; De Vitta, A. Prevalence and factors associated with neck pain: A population-based study. Braz. J. Phys. Ther. 2017, 21, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for Rehabil. based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019 [published correction appears in Lancet. 2020 Dec 4]. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Peng, B.; Yang, L.; Li, Y.; Liu, T.; Liu, Y. Cervical Proprioception Impairment in Neck Pain-Pathophysiology, Clinical Evaluation, and Management: A Narrative Review. Pain Ther. 2021, 10, 143–164. [Google Scholar] [CrossRef]
- MacDermid, J.C.; Walton, D.M.; Bobos, P.; Lomotan, M.; Carlesso, L. A Qualitative Description of Chronic Neck Pain has Implications for Outcome Assessment and Classification. Open Orthop. J. 2016, 10, 746–756. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A classification of chronic pain for ICD-11. Pain 2015, 156, 1003–1007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rampazo, P.; da Silva, V.R.; de Andrade, A.L.M.; Back, C.G.N.; Madeleine, P.M.; Arendt-Nielsen, L.; Liebano, R.E. Sensory, Motor, and Psychosocial Characteristics of Individuals With Chronic Neck Pain: A Case–Control Study. Phys. Ther. 2021, 101, pzab104. [Google Scholar] [CrossRef]
- Obayashi, H.; Urabe, Y.; Yamanaka, Y.; Okuma, R. Effects of respiratory-muscle exercise on spinal curvature. J. Sport Rehabil. 2012, 21, 63–68. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, L.; Goldsmith, C.H.; Coleman, K. Breathing evaluation and retraining as an adjunct to manual therapy. Man. Ther. 2011, 16, 51–52. [Google Scholar] [CrossRef] [PubMed]
- Dimitriadis, Z.; Kapreli, E.; Strimpakos, N.; Oldham, J. Respiratory dysfunction in patients with chronic neck pain: What is the current evidence? J. Bodyw. Mov. Ther. 2016, 20, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Coulter, I.D.; Crawford, C.; Vernon, H.; Hurwitz, E.L.; Khorsan, R.; Booth, M.S.; Herman, P.M. Manipulation and Mobilization for Treating Chronic Nonspecific Neck Pain: A Systematic Review and Meta-Analysis for an Appropriateness Panel. Pain Physician 2019, 2, E55–E70. [Google Scholar] [CrossRef] [PubMed]
- Tatsios, P.; Koumantakis, G.; Karakasidou, P.; Philippou, A. The effectiveness of manual therapy on musculoskeletal and respiratory parameters in patients with chronic low back pain: A systematic review. Crit. Rev. Phys. Rehabil. Med. 2021, 33, 71–101. [Google Scholar] [CrossRef]
- Kahlaee, A.H.; Ghamkhar, L.; Arab, A.M. The Association Between Neck Pain and Pulmonary Function: A Systematic Review. Am. J. Phys. Med. Rehabil. 2017, 96, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- da Costa, B.R.; Hilfiker, R.; Egger, M. PEDro’s bias: Summary quality scores should not be used in meta-analysis. J. Clin. Epidemiol. 2013, 66, 75–77. [Google Scholar] [CrossRef] [PubMed]
- Paraskevopoulos, E.; Karanasios, S.; Gioftsos, G.; Tatsios, P.; Koumantakis, G.; Papandreou, M. The effectiveness of neuromobilization exercises in carpal tunnel syndrome: Systematic review and meta-analysis. Physiother. Theory Pract. 2022, 1–40. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0; Cochrane: London, UK, 2019. [Google Scholar]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; De Beer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Pearson Education Ltd.: Harlow, UK, 2014. [Google Scholar]
- Simoni, G.; Bozzolan, M.; Bonnini, S.; Grassi, A.; Zucchini, A.; Mazzanti, C.; Oliva, D.; Caterino, F.; Gallo, A.; Da Roit, M. Effectiveness of standard cervical physiotherapy plus diaphragm manual therapy on pain in patients with chronic neck pain: A randomized controlled trial. J. Bodyw. Mov. Ther. 2021, 26, 481–491. [Google Scholar] [CrossRef] [PubMed]
- López-De-Uralde-Villanueva, I.; Beltran-Alacreu, H.; Fernández-Carnero, J.; La Touche, R. Pain management using a multimodal physiotherapy program including a biobehavioral approach for chronic nonspecific neck pain: A randomized controlled trial. Physiother. Theory Pract. 2018, 36, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Dareh-Deh, H.R.; Hadadnezhad, M.; Letafatkar, A. Therapeutic routine with respiratory exercises improves posture, muscle activity, and respiratory pattern of patients with neck pain: A randomized controlled trial. Sci. Rep. 2022, 12, 4149. [Google Scholar] [CrossRef]
- Beltran-Alacreu, H.; López-De-Uralde-Villanueva, I.; Fernandez-Carnero, J.; La Touche, R. Manual Therapy, Therapeutic Patient Education, and Therapeutic Exercise, an Effective Multimodal Treatment of Nonspecific Chronic Neck Pain: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2015, 94, 887–897. [Google Scholar] [CrossRef] [PubMed]
- Özer Kaya, D.; Toprak Çelenay, Ş. Effectiveness of Relaxation Training in Addition to Stabilization Exercises in Chronic Neck Pain: A Randomized Clinical Trial. Turk. J. Physiother. Rehabil. 2019, 30, 145–153. [Google Scholar] [CrossRef] [Green Version]
- Sakuna, M.; Mekhora, K.; Jalajondeja, W.; Jalajondeja, C. Breathing retraining with chest wall mobilization improves respiratory reserve and decreases hyperactivity of accessory breathing muscles during respiratory excursions: A randomized controlled trial. Acta Bioeng. Biomech. 2020, 22, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Arif, T.; Rehman, S.S.U.; Ikram, M. Effects of cervical stabilisation exercises on respiratory strength in chronic neck pain patients with forward head posture. J. Pak. Med. Assoc. 2022. Ahead of Print. [Google Scholar] [CrossRef]
- Anwar, S.; Arsalan, S.A.; Ahmad, A.; Zafar, H.; Gillani, S.A.; Hanif, A. Effects of breathing re-education on clinical outcomes in patients with nonspecific chronic neck pain. J. Pak. Med. Assoc. 2022. Ahead of Print. [Google Scholar] [CrossRef]
- Hwangbo, P.-N.; Hwangbo, G.; Park, J.; Lee, S. The Effect of Thoracic Joint Mobilization and Self-stretching Exercise on Pulmonary Functions of Patients with Chronic Neck Pain. J. Phys. Ther. Sci. 2014, 26, 1783–1786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Metikaridis, D.T.; Hadjipavlou, A.; Artemiadis, A.; Chrousos, G.P.; Darviri, C. Effect of a stress management program on subjects with neck pain: A pilot randomized controlled trial. J. Back Musculoskelet. Rehabil. 2017, 30, 23–33. [Google Scholar] [CrossRef]
- Mohamed, S.S.; Hagag, A.; Mohamed AShendy MAEl-Batanony, M.M. Ventilatory function response to training of cervical muscles in mechanical neck pain: A randomized controlled study. IJRAMR 2019, 6, 4617–4622. [Google Scholar]
- Akodu, A.Κ.; Ajepe, T.O.; Sorunke, M.A. Effects of neck stabilization and isometric exercises on non-specific chronic neck pain: A pilot study. J. Riphah Coll. Rehabil. Sci. 2020, 8, 9–17. [Google Scholar] [CrossRef]
- Mohan, V.; Ahmad, N.B.; Tambi, N.B. Effect of respiratory exercises on neck pain patients: A pilot study. Pol. Ann. Med. 2016, 23, 15–20. [Google Scholar] [CrossRef]
- Pawaria, S.; Sudan, D.S.; Kalra, S.; Yadav, J. Effectiveness of cervical stabilization exercises with feedback on respiratory status in chronic neck pain patients with forward head posture. Int. J. Physiother. 2019, 6, 70–75. [Google Scholar] [CrossRef]
- Pawaria, S.; Sudhan, D.; Kalra, S. Effectiveness of Cervical Stabilisation Exercises on Respiratory Strength in Chronic Neck Pain Patients with Forward Head Posture-A Pilot Study. J. Clin. Diagn. Res. 2019, 13, 6–9. [Google Scholar] [CrossRef]
- Thongtipmak, S.; Buranruk, O.; Eungpinichpong, W.; Konharn, K. Immediate effects and acceptability of an application-based stretching exercise incorporating deep slow breathing for neck pain self-management. Healthc. Inform. Res. 2020, 26, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Chaitow, L. Breathing pattern disorders, motor control, and low back pain. J. Osteopat. Med. 2004, 7, 33–40. [Google Scholar] [CrossRef]
- Maitland, G.; Banks, K.; English, K.; Hengeveld, E. Maitland’s Vertebral Manipulation, 7th ed.; Butterworth-Heinemann: Oxford, UK, 2005. [Google Scholar]
- Kaltenborn, F.M. The Spinal Basic: Evaluation and Mobilization Techniques, 3rd ed.; OPTP: Plymouth, MN, USA, 1993. [Google Scholar]
- Yeampattanaporn, O.; Mekhora, K.; Jalayondeja, W.; Wongsathikun, J. Immediate effects of breathing re-education on respiratory function and range of motion in chronic neck pain. J. Med. Assoc. Thail. 2014, 97 (Suppl. 7), S55–S59. [Google Scholar]
- Paccione, C.E.; Jacobsen, H.B. Motivational Non-directive Resonance Breathing as a Treatment for Chronic Widespread Pain. Front. Psychol. 2019, 10, 1207. [Google Scholar] [CrossRef] [Green Version]
| Patient/ClientGroup: | “neck pain” OR “chronic neck pain” OR “mechanical neck pain” |
| Intervention: | “manual therapy” OR “respiratory exercises” OR “breathing retraining” OR “diaphragm manual therapy” OR “relaxation” OR “diaphragm exercises” AND |
| Comparison: | “control group” OR “traditional physiotherapy” OR “sham” AND |
| Outcomes: | “pain” OR “function” OR “respiratory outcomes” OR “breathing dysfunction” OR “respiratory function” AND |
| Study: | “randomized clinical trial” OR “systematic review” |
| Studies | Items | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total Score | |
| Hwangbo et al., 2014 [28] | + | + | + | + | + | 5/10 | |||||
| Beltran-Alacreu et al., 2015 [23] | + | + | + | + | + | + | 6/10 | ||||
| Mohan et al., 2016 [32] | + | + | + | + | 4/10 | ||||||
| Metikaridis et al., 2017 [29] | + | + | + | + | + | 5/10 | |||||
| Pawaria et al., 2019a [33] | + | + | + | + | 4/10 | ||||||
| Pawaria et al., 2019b [34] | + | + | + | + | 4/10 | ||||||
| Özer Kaya et al., 2019 [24] | + | + | + | + | + | + | 6/10 | ||||
| Thongtipmak et al., 2019 [35] | + | + | + | + | 4/10 | ||||||
| Mohamed et al., 2019 [30] | + | + | + | + | + | 5/10 | |||||
| López-de-Uralde-Villanueva et al., 2020 [21] | + | + | + | + | + | + | + | + | 8/10 | ||
| Akodu et al., 2020 [31] | + | + | + | + | 4/10 | ||||||
| Sakuna et al., 2020 [25] | + | + | + | + | + | + | 6/10 | ||||
| Simoni et al., 2021 [20] | + | + | + | + | + | + | + | + | + | 9/10 | |
| Arif et al., 2022 [26] | + | + | + | + | + | + | 6/10 | ||||
| Anwar et al., 2022 [27] | + | + | + | + | + | + | 6/10 | ||||
| Dareh-deh et al., 2022 [22] | + | + | + | + | + | + | + | + | 8/10 | ||
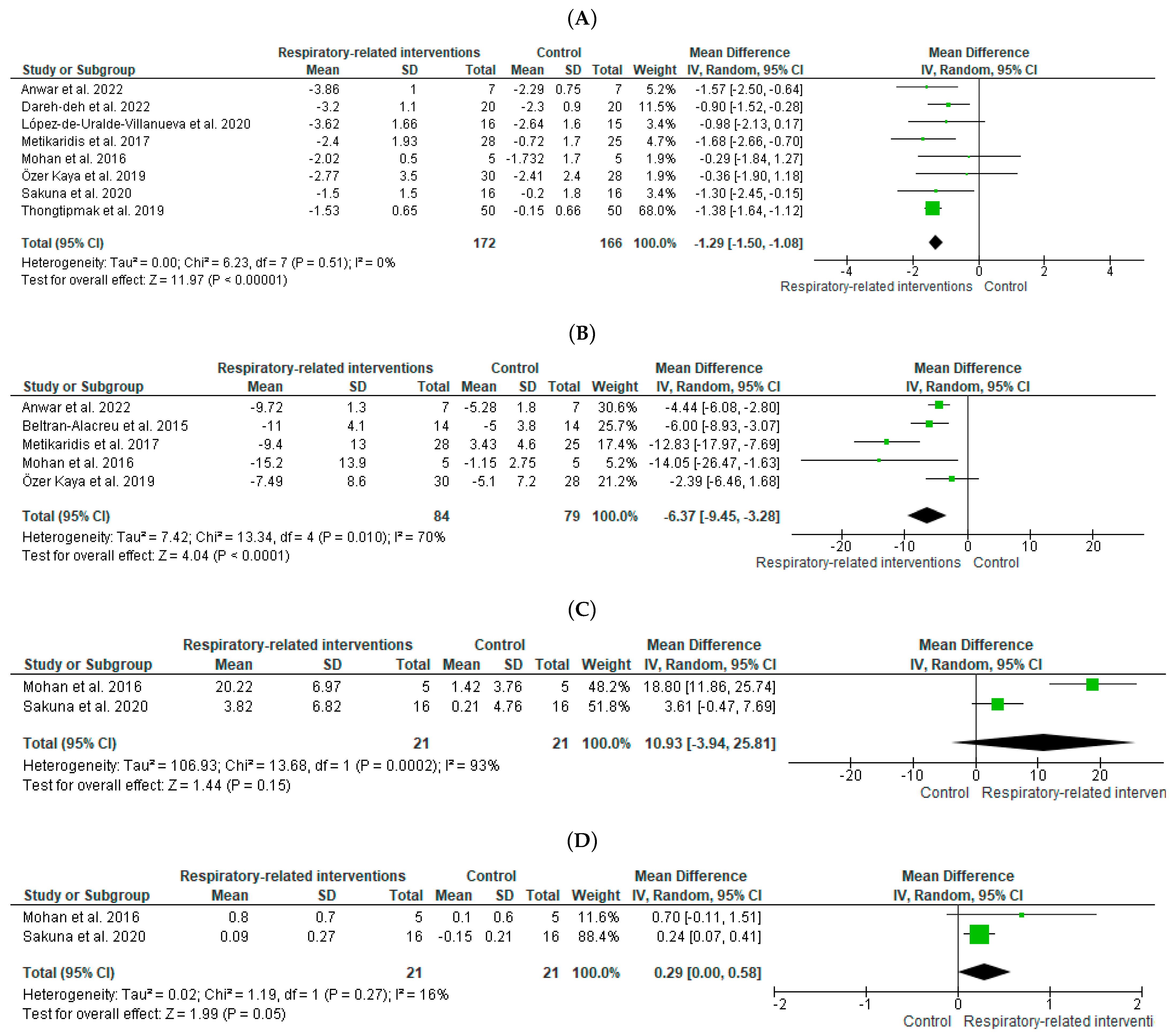
| (A) | ||||||||||
| Certainty Assessment | No. of Patients | Effect | Certainty | |||||||
| No. of Studies per Outcome | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Combined MT | Single MT | Absolute (95% CI) | |
| Pain | ||||||||||
| 2 | randomized trials | not serious | not serious | not serious | very serious a | none | 36 | 35 | SMD −0.76 (−1.5 to −0.03) | ⊕⊕◯◯ Low |
| Disability | ||||||||||
| 2 | randomized trials | not serious | not serious | not serious | very serious a | none | 35 | 34 | SMD −0.85 (−1.96 to −0.27) | ⊕⊕◯◯ Low |
| (B) | ||||||||||
| Certainty Assessment | No. of Patients | Effect | Certainty | |||||||
| No. of Studies per Outcome | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | MT | Parallel Intervention | Absolute (95% CI) | |
| FEV1 | ||||||||||
| 3 | randomized trials | very serious a | not serious | not serious | very serious b | none | 67 | 67 | SMD 0.44 (0.1 to 0.79) | ⊕◯◯◯ Very low |
| (C) | ||||||||||
| Certainty Assessment | No. of Patients | Effect | Certainty | |||||||
| No. of Studies per Outcome | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | SEMT | Control/Other Intervention | Absolute (95% CI) | |
| Pain | ||||||||||
| 4 | randomized trials | serious a | very serious b | not serious | very serious c,d | none | 70 | 70 | SMD −1.65 (−2.99 to −0.31) | ⊕◯◯◯ Very low |
| Disability | ||||||||||
| 4 | randomized trials | very serious a | very serious b | not serious | very serious c,d | none | 55 | 55 | SMD −1.6 (−2.83 to −0.37) | ⊕◯◯◯ Very low |
| PImax | ||||||||||
| 2 | randomized trials | very serious a | very serious b | not serious | very serious c,d | none | 60 | 60 | SMD 2.1 (0.2 to 4) | ⊕◯◯◯ Very low |
| (D) | ||||||||||
| Certainty Assessment | No. of Patients | Effect | Certainty | |||||||
| No. of Studies per Outcome | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | RRI | Control/Other Intervention | Absolute (95% CI) | |
| Pain | ||||||||||
| 8 | randomized trials | serious a | not serious | not serious | serious b | none | 172 | 166 | SMD −0.91 (−1.45 to −0.36) | ⊕⊕◯◯ Low |
| Disability | ||||||||||
| 5 | randomized trials | serious a | serious c | not serious | serious b | none | 84 | 79 | SMD −1.22 (−1.92 to −0.52) | ⊕◯◯◯ Very low |
| MVV | ||||||||||
| 2 | randomized trials | serious a | very serious c | not serious | very serious b | none | 21 | 21 | SMD 1.6 (0.74 l to 3.95) | ⊕◯◯◯ Very low |
| CWE | ||||||||||
| 2 | randomized trials | serious a | not serious | not serious | very serious b | none | 21 | 21 | SMD 0.97 (0.32 to 1.62) | ⊕◯◯◯ Very low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tatsios, P.I.; Grammatopoulou, E.; Dimitriadis, Z.; Papandreou, M.; Paraskevopoulos, E.; Spanos, S.; Karakasidou, P.; Koumantakis, G.A. The Effectiveness of Spinal, Diaphragmatic, and Specific Stabilization Exercise Manual Therapy and Respiratory-Related Interventions in Patients with Chronic Nonspecific Neck Pain: Systematic Review and Meta-Analysis. Diagnostics 2022, 12, 1598. https://doi.org/10.3390/diagnostics12071598
Tatsios PI, Grammatopoulou E, Dimitriadis Z, Papandreou M, Paraskevopoulos E, Spanos S, Karakasidou P, Koumantakis GA. The Effectiveness of Spinal, Diaphragmatic, and Specific Stabilization Exercise Manual Therapy and Respiratory-Related Interventions in Patients with Chronic Nonspecific Neck Pain: Systematic Review and Meta-Analysis. Diagnostics. 2022; 12(7):1598. https://doi.org/10.3390/diagnostics12071598
Chicago/Turabian StyleTatsios, Petros I., Eirini Grammatopoulou, Zacharias Dimitriadis, Maria Papandreou, Eleftherios Paraskevopoulos, Savvas Spanos, Palina Karakasidou, and George A. Koumantakis. 2022. "The Effectiveness of Spinal, Diaphragmatic, and Specific Stabilization Exercise Manual Therapy and Respiratory-Related Interventions in Patients with Chronic Nonspecific Neck Pain: Systematic Review and Meta-Analysis" Diagnostics 12, no. 7: 1598. https://doi.org/10.3390/diagnostics12071598
APA StyleTatsios, P. I., Grammatopoulou, E., Dimitriadis, Z., Papandreou, M., Paraskevopoulos, E., Spanos, S., Karakasidou, P., & Koumantakis, G. A. (2022). The Effectiveness of Spinal, Diaphragmatic, and Specific Stabilization Exercise Manual Therapy and Respiratory-Related Interventions in Patients with Chronic Nonspecific Neck Pain: Systematic Review and Meta-Analysis. Diagnostics, 12(7), 1598. https://doi.org/10.3390/diagnostics12071598








