PET-Based Imaging with 18F-FDG and 18F-NaF to Assess Inflammation and Microcalcification in Atherosclerosis and Other Vascular and Thrombotic Disorders
Abstract
1. Introduction
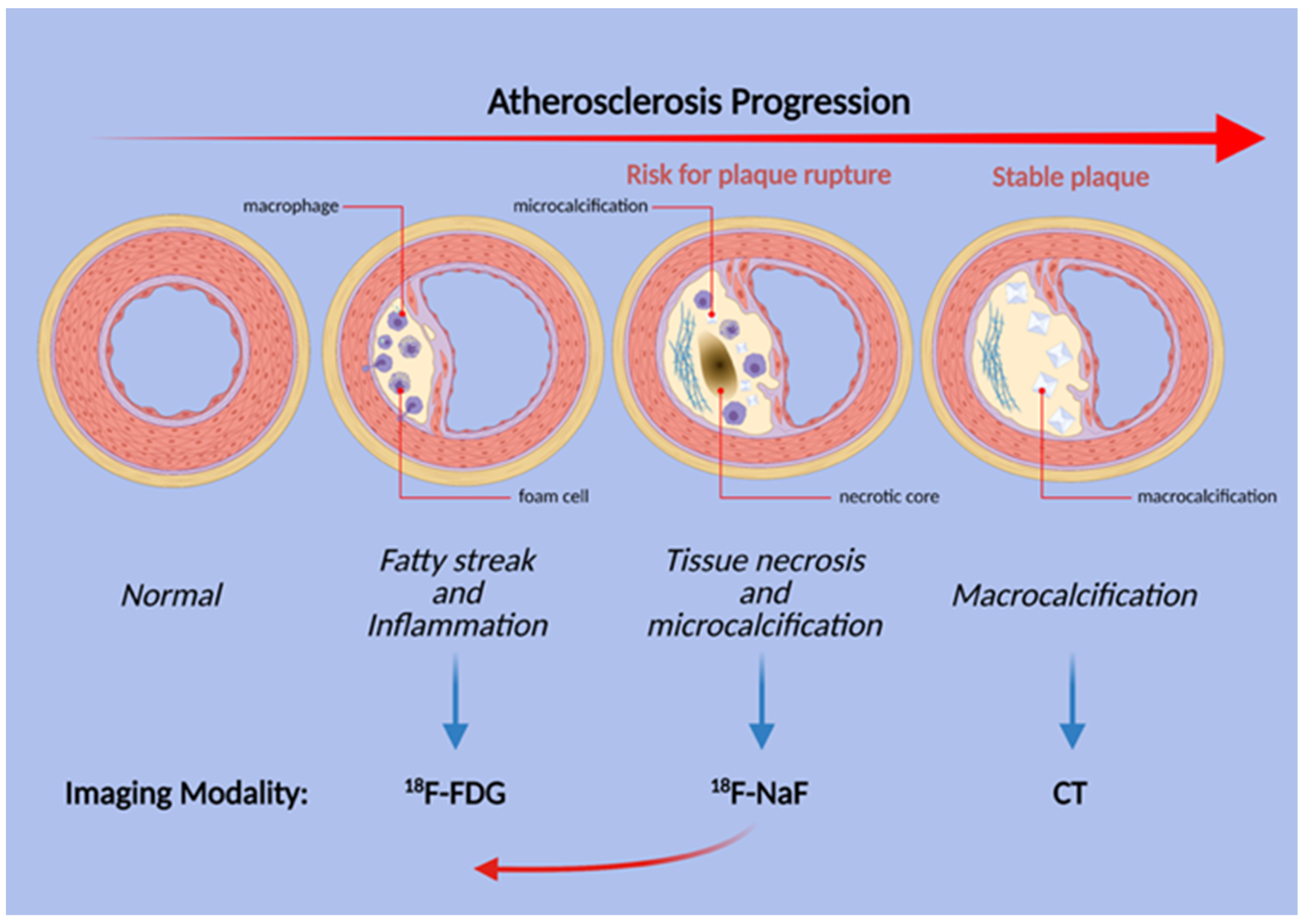
2. Atherosclerosis
2.1. Role of FDG in Atherosclerosis
2.2. Role of NaF in Atherosclerosis
2.3. Alavi-Carlsen Calcification Score (ACCS)
2.4. Other PET Tracers in Atherosclerosis
3. Thrombotic Disorders
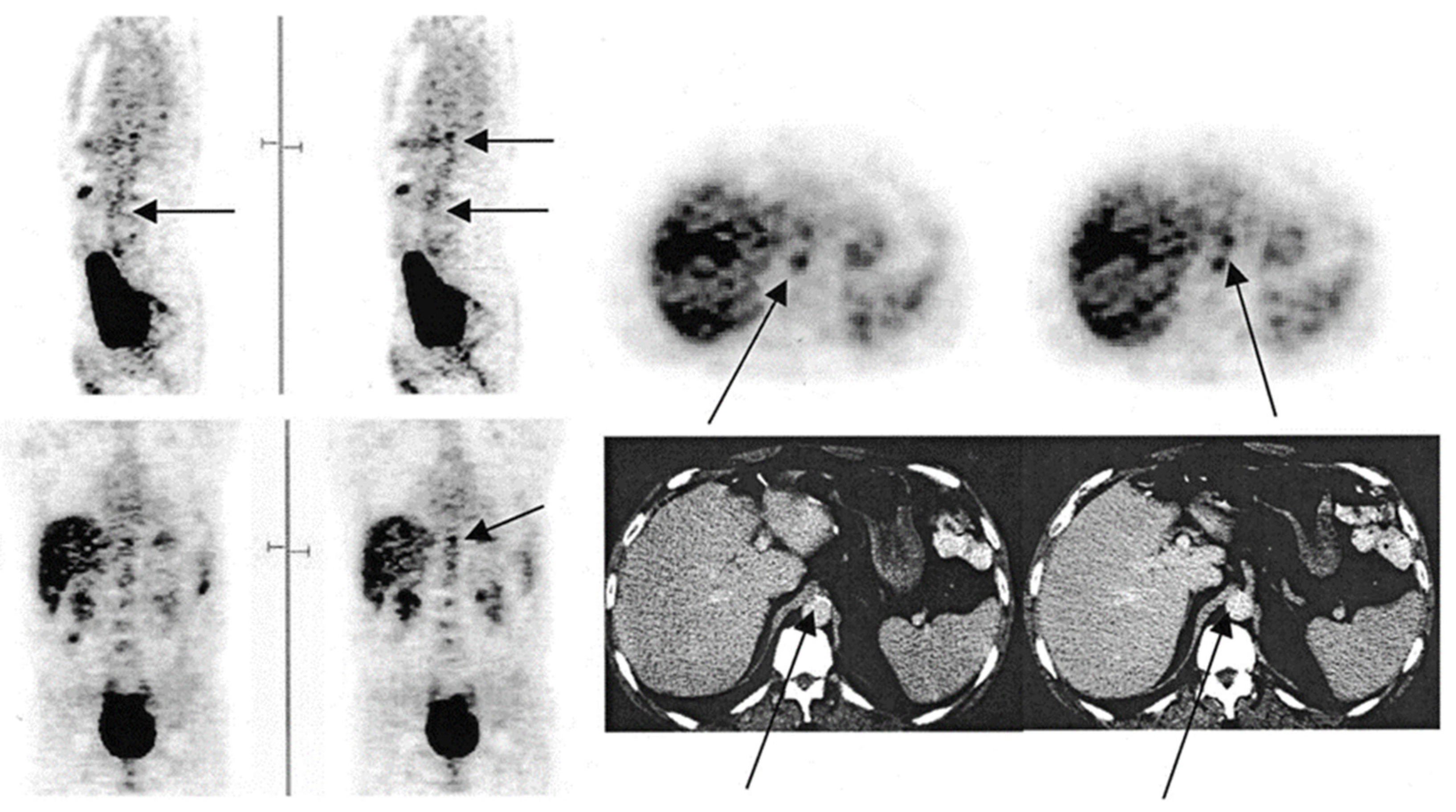
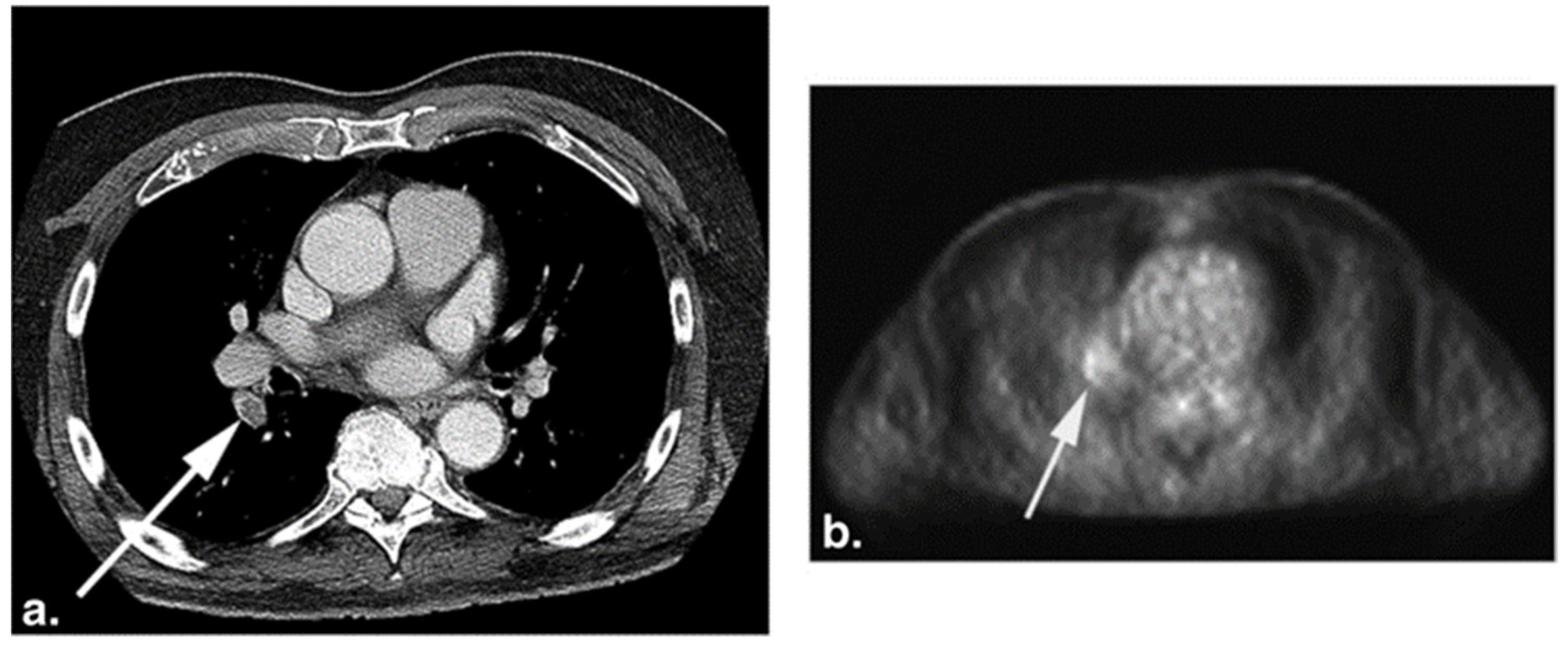
3.1. FDG-PET in Pulmonary Embolism
3.2. FDG-PET in Deep Vein Thrombosis and Venous Thromboembolism
4. FDG beyond CVDs
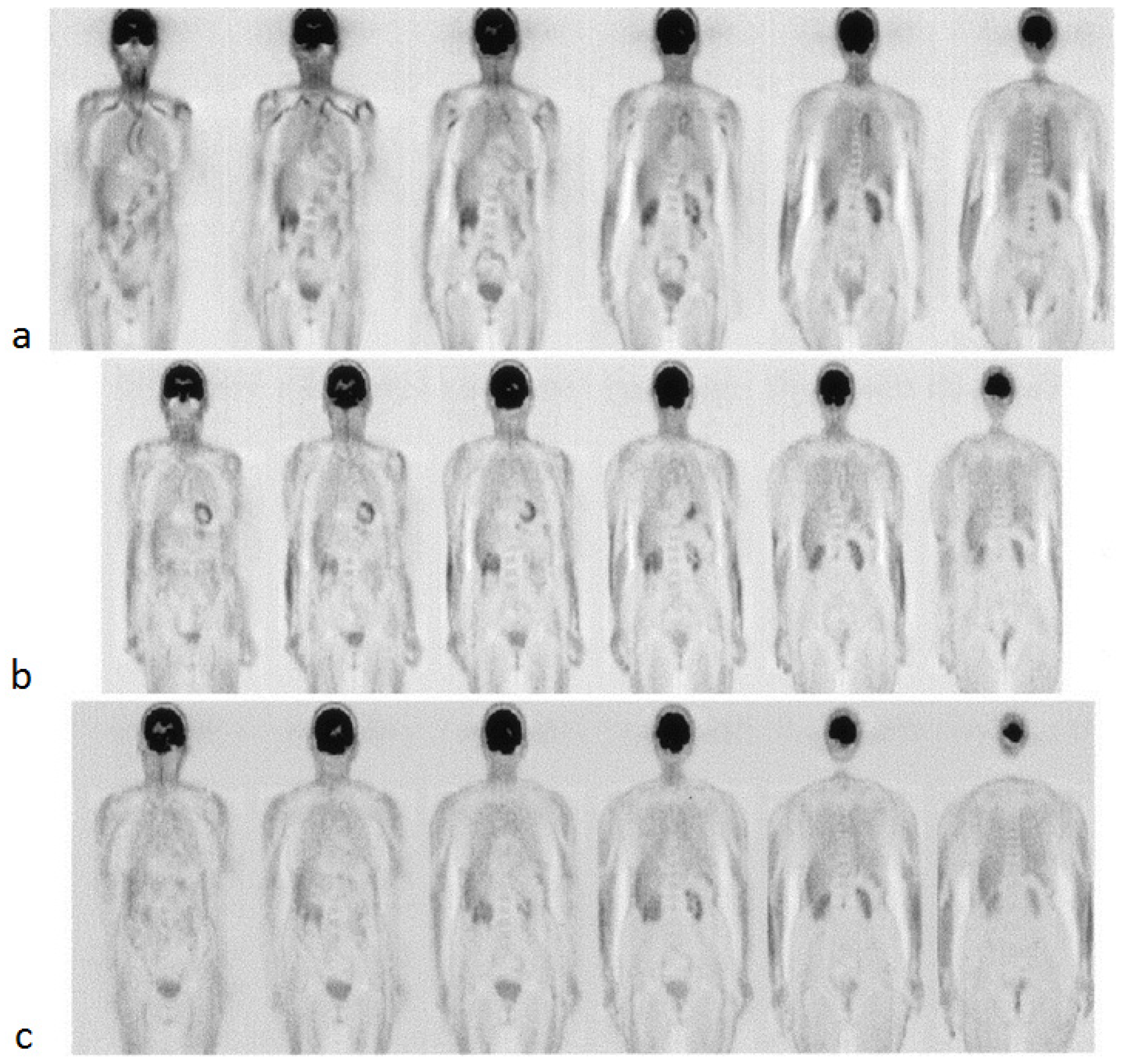
4.1. FDG-PET in Large Vessel Vasculitis
4.2. FDG-PET in Vascular Diseases of Infectious Etiology
4.3. FDG-PET in Vascular Diseases of Immunoglobulin G4-Related Disease (IgG4-RD)
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Libby, P.; Buring, J.E.; Badimon, L.; Hansson, G.K.; Deanfield, J.; Bittencourt, M.S.; Tokgozoglu, L.; Lewis, E.F. Atherosclerosis. Nat. Rev. Dis. Primers 2019, 5, 56. [Google Scholar] [CrossRef] [PubMed]
- Van Hooser, J.C.; Rouse, K.L.; Meyer, M.L.; Siegler, A.M.; Fruehauf, B.M.; Ballance, E.H.; Solberg, S.M.; Dibble, M.J.; Lutfiyya, M.N. Knowledge of heart attack and stroke symptoms among US Native American Adults: A cross-sectional population-based study analyzing a multi-year BRFSS database. BMC Public Health 2020, 20, 1–10. [Google Scholar] [CrossRef]
- Mayer, M.; Borja, A.J.; Hancin, E.C.; Auslander, T.; Revheim, M.-E.; Moghbel, M.C.; Werner, T.J.; Alavi, A.; Rajapakse, C.S. Imaging Atherosclerosis by PET, With Emphasis on the Role of FDG and NaF as Potential Biomarkers for This Disorder. Front. Physiol. 2020, 11, 511391. [Google Scholar] [CrossRef]
- Paydary, K.; Revheim, M.E.; Emamzadehfard, S.; Gholami, S.; Pourhassan, S.; Werner, T.J.; Hoilund-Carlsen, P.F.; Alavi, A. Quantitative thoracic aorta calcification assessment by (18)F-NaF PET/CT and its correlation with atherosclerotic cardiovascular disorders and increasing age. Eur. Radiol. 2020, 31, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Moghbel, M.; Al-Zaghal, A.; Werner, T.J.; Constantinescu, C.M.; Høilund-Carlsen, P.F.; Alavi, A. The Role of PET in Evaluating Atherosclerosis: A Critical Review. Semin. Nucl. Med. 2018, 48, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Agatston, A.S.; Janowitz, F.W.R.; Hildner, F.J.; Zusmer, N.R.; Viamonte, M., Jr.; Detrano, R. Quantification of coronary artery calcium using ultrafast computed tomography. J. Am. Coll. Cardiol. 1990, 15, 827–832. [Google Scholar] [CrossRef]
- Bergström, G.; Persson, M.; Adiels, M.; Björnson, E.; Bonander, C.; Ahlström, H.; Alfredsson, J.; Angerås, O.; Berglund, G.; Blomberg, A.; et al. Prevalence of Subclinical Coronary Artery Atherosclerosis in the General Population. Circulation 2021, 144, 916–929. [Google Scholar] [CrossRef]
- Oikonomou, E.; Marwan, M.; Desai, M.Y.; Mancio, J.; Alashi, A.; Centeno, E.H.; Thomas, S.; Herdman, L.; Kotanidis, C.; E Thomas, K.; et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): A post-hoc analysis of prospective outcome data. Lancet 2018, 392, 929–939. [Google Scholar] [CrossRef]
- Giusca, S.; Schütz, M.; Kronbach, F.; Wolf, D.; Nunninger, P.; Korosoglou, G. Coronary Computer Tomography Angiography in 2021—Acquisition Protocols, Tips and Tricks and Heading beyond the Possible. Diagnostics 2021, 11, 1072. [Google Scholar] [CrossRef]
- Nakahara, T.; Narula, J.; Strauss, H.W. Molecular Imaging of Vulnerable Plaque. Semin. Nucl. Med. 2018, 48, 291–298. [Google Scholar] [CrossRef]
- Nakahara, T.; Dweck, M.R.; Narula, N.; Pisapia, D.; Narula, J.; Strauss, H.W. Coronary Artery Calcification: From Mechanism to Molecular Imaging. JACC Cardiovasc. Imaging 2017, 10, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Hansson, G.K. From Focal Lipid Storage to Systemic Inflammation. J. Am. Coll. Cardiol. 2019, 74, 1594–1607. [Google Scholar] [CrossRef] [PubMed]
- Libby, P. Inflammation in atherosclerosis. Nature 2002, 420, 868–874. [Google Scholar] [CrossRef]
- Joshi, N.V.; Vesey, A.T.; Williams, M.C.; Shah, A.S.V.; A Calvert, P.; Craighead, F.H.M.; Yeoh, S.E.; Wallace, W.; Salter, D.; Fletcher, A.M.; et al. 18F-fluoride positron emission tomography for identification of ruptured and high-risk coronary atherosclerotic plaques: A prospective clinical trial. Lancet 2014, 383, 705–713. [Google Scholar] [CrossRef]
- Arbab-Zadeh, A.; Fuster, V. The myth of the “vulnerable plaque”: Transitioning from a focus on individual lesions to atherosclerotic disease burden for coronary artery disease risk assessment. J. Am. Coll. Cardiol. 2015, 65, 846–855. [Google Scholar] [CrossRef] [PubMed]
- Stefanadis, C.; Antoniou, C.; Tsiachris, D.; Pietri, P. Coronary Atherosclerotic Vulnerable Plaque: Current Perspectives. J. Am. Hear. Assoc. 2017, 6, e005543. [Google Scholar] [CrossRef]
- Chowdhury, M.; Tarkin, J.; Evans, N.; Le, E.; Warburton, L.; Hayes, P.; Rudd, J.; A Coughlin, P. 18F-FDG Uptake on PET/CT in Symptomatic versus Asymptomatic Carotid Disease: A Meta-Analysis. Eur J Vasc Endovasc Surg 2018, 56, 172–179. [Google Scholar] [CrossRef]
- Skagen, K.; Johnsrud, K.; Evensen, K.; Scott, H.; Krohg-Sørensen, K.; Reier-Nilsen, F.; Revheim, M.-E.; Fjeld, J.G.; Skjelland, M.; Russell, D. Carotid Plaque Inflammation Assessed with 18F-FDG PET/CT is Higher in Symptomatic Compared with Asymptomatic Patients. Int. J. Stroke 2015, 10, 730–736. [Google Scholar] [CrossRef]
- McKenney-Drake, M.L.; Territo, P.R.; Salavati, A.; Houshmand, S.; Persohn, S.; Liang, Y.; Alloosh, M.; Moe, S.M.; Weaver, C.M.; Alavi, A.; et al. 18F-NaF PET Imaging of Early Coronary Artery Calcification. JACC Cardiovasc. Imaging 2016, 9, 627–628. [Google Scholar] [CrossRef]
- Nakahara, T.; Narula, J.; Strauss, H.W. NaF uptake in unstable plaque: What does fluoride uptake mean? Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 2250–2252. [Google Scholar] [CrossRef]
- Grant, F.D.; Fahey, F.H.; Packard, A.B.; Davis, R.T.; Alavi, A.; Treves, S.T. Skeletal PET with 18F-Fluoride: Applying New Technology to an Old Tracer. J. Nucl. Med. 2008, 49, 68–78. [Google Scholar] [CrossRef]
- Park, P.; Raynor, W.; Sun, Y.; Werner, T.; Rajapakse, C.; Alavi, A. 18F-Sodium Fluoride PET as a Diagnostic Modality for Metabolic, Autoimmune, and Osteogenic Bone Disorders: Cellular Mechanisms and Clinical Applications. Int. J. Mol. Sci. 2021, 22, 6504. [Google Scholar] [CrossRef] [PubMed]
- Yun, M.; Yeh, D.; Araujo, L.I.; Jang, S.; Newberg, A.; Alavi, A. F-18 FDG uptake in the large arteries: A new observation. Clin. Nucl. Med. 2001, 26, 314–319. [Google Scholar] [CrossRef]
- van der Valk, F.M.; Verweij, S.L.; Zwinderman, K.A.; Strang, A.C.; Kaiser, Y.; Marquering, H.A.; Nederveen, A.J.; Stroes, E.S.; Verberne, H.J.; Rudd, J.H. Thresholds for Arterial Wall Inflammation Quantified by (18)F-FDG PET Imaging: Implications for Vascular Interventional Studies. JACC Cardiovasc. Imaging 2016, 9, 1198–1207. [Google Scholar] [CrossRef] [PubMed]
- Tawakol, A.; Migrino, R.Q.; Bashian, G.G.; Bedri, S.; Vermylen, D.; Cury, R.C.; Yates, D.; LaMuraglia, G.M.; Furie, K.; Houser, S.; et al. In Vivo 18F-Fluorodeoxyglucose Positron Emission Tomography Imaging Provides a Noninvasive Measure of Carotid Plaque Inflammation in Patients. J. Am. Coll. Cardiol. 2006, 48, 1818–1824. [Google Scholar] [CrossRef]
- Myers, K.S.; Rudd, J.H.; Hailman, E.P.; Bolognese, J.A.; Burke, J.; Pinto, C.A.; Klimas, M.; Hargreaves, R.; Dansky, H.M.; Fayad, Z.A. Correlation Between Arterial FDG Uptake and Biomarkers in Peripheral Artery Disease. JACC Cardiovasc. Imaging 2012, 5, 38–45. [Google Scholar] [CrossRef]
- Yun, M.; Jang, S.; Cucchiara, A.; Newberg, A.B.; Alavi, A. 18F FDG uptake in the large arteries: A correlation study with the atherogenic risk factors. Semin. Nucl. Med. 2002, 32, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Bural, G.G.; Torigian, D.A.; Chamroonrat, W.; Houseni, M.; Chen, W.; Basu, S.; Kumar, R.; Alavi, A. FDG-PET is an effective imaging modality to detect and quantify age-related atherosclerosis in large arteries. Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 562–569. [Google Scholar] [CrossRef]
- Strobl, F.F.; Rominger, A.; Wolpers, S.; Rist, C.; Bamberg, F.; Thierfelder, K.M.; Nikolaou, K.; Uebleis, C.; Hacker, M.; Reiser, M.F.; et al. Impact of cardiovascular risk factors on vessel wall inflammation and calcified plaque burden differs across vascular beds: A PET-CT study. Int. J. Cardiovasc. Imaging 2013, 29, 1899–1908. [Google Scholar] [CrossRef]
- Pasha, A.K.; Moghbel, M.; Saboury, B.; Gharavi, M.H.; A Blomberg, B.; A Torigian, D.; Kwee, T.C.; Basu, S.; Iii, E.R.M.; Alavi, A. Effects of age and cardiovascular risk factors on 18F-FDG PET/CT quantification of atherosclerosis in the aorta and peripheral arteries. Hell. J. Nucl. Med. 2015, 18, 5–10. [Google Scholar] [CrossRef]
- Rudd, J.H.; Warburton, E.A.; Fryer, T.D.; Jones, H.A.; Clark, J.C.; Antoun, N.; Johnström, P.; Davenport, A.P.; Kirkpatrick, P.J.; Arch, B.N.; et al. Imaging atherosclerotic plaque inflammation with [18F]-fluorodeoxyglucose positron emission tomography. Circulation 2002, 105, 2708–2711. [Google Scholar] [CrossRef] [PubMed]
- Al-Zaghal, A.; Aras, M.; Borja, A.J.; Moghbel, M.; Demir, Y.; Houshmand, S.; Ciftci, E.; Werner, T.J.; Høilund-Carlsen, P.F.; A Torigian, D.; et al. Detection of pulmonary artery atherosclerosis by FDG-PET/CT: A new observation. Am. J. Nucl. Med. Mol. Imaging 2020, 10, 127–134. [Google Scholar] [PubMed]
- Arani, L.S.; Gharavi, M.H.; Zadeh, M.Z.; Raynor, W.; Seraj, S.M.; Constantinescu, C.; Gerke, O.; Werner, T.J.; Høilund-Carlsen, P.F.; Alavi, A. Association between age, uptake of 18F-fluorodeoxyglucose and of 18F-sodium fluoride, as cardiovascular risk factors in the abdominal aorta. Hell. J. Nucl. Med. 2019, 22, 14–19. [Google Scholar]
- Blomberg, B.A.; De Jong, P.A.; Thomassen, A.; Lam, M.G.E.; Vach, W.; Olsen, M.H.; Mali, W.P.T.M.; Narula, J.; Alavi, A.; Høilund-Carlsen, P.F. Thoracic aorta calcification but not inflammation is associated with increased cardiovascular disease risk: Results of the CAMONA study. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 249–258. [Google Scholar] [CrossRef]
- Ben-Haim, S.; Kupzov, E.; Tamir, A.; Israel, O. Evaluation of 18F-FDG uptake and arterial wall calcifications using 18F-FDG PET/CT. J. Nucl. Med. 2004, 45, 1816–1821. [Google Scholar]
- Tatsumi, M.; Cohade, C.; Nakamoto, Y.; Wahl, R.L. Fluorodeoxyglucose Uptake in the Aortic Wall at PET/CT: Possible Finding for Active Atherosclerosis. Radiology 2003, 229, 831–837. [Google Scholar] [CrossRef] [PubMed]
- Meirelles, G.S.; Gonen, M.; Strauss, H.W. 18F-FDG uptake and calcifications in the thoracic aorta on positron emission tomography/computed tomography examinations: Frequency and stability on serial scans. J. Thorac. Imaging 2011, 26, 54–62. [Google Scholar] [CrossRef]
- Tawakol, A.; Ishai, A.; AP Takx, R.; Figueroa, A.L.; Ali, A.; Kaiser, Y.; A Truong, Q.; Solomon, C.J.; Calcagno, C.; Mani, V.; et al. Relation between resting amygdalar activity and cardiovascular events: A longitudinal and cohort study. Lancet 2017, 389, 834–845. [Google Scholar] [CrossRef]
- Blomberg, B.A.; Thomassen, A.; Takx, R.A.P.; Hildebrandt, M.G.; Simonsen, J.A.; Buch-Olsen, K.M.; Diederichsen, A.C.P.; Mickley, H.; Alavi, A.; Høilund-Carlsen, P.F. Delayed 18F-fluorodeoxyglucose PET/CT imaging improves quantitation of atherosclerotic plaque inflammation: Results from the CAMONA study. J. Nucl. Cardiol. 2014, 21, 588–597. [Google Scholar] [CrossRef]
- Derlin, T.; Richter, U.; Bannas, P.; Begemann, P.; Buchert, R.; Mester, J.; Klutmann, S. Feasibility of 18F-Sodium Fluoride PET/CT for Imaging of Atherosclerotic Plaque. J. Nucl. Med. 2010, 51, 862–865. [Google Scholar] [CrossRef]
- Derlin, T.; Wisotzki, C.; Richter, U.; Apostolova, I.; Bannas, P.; Weber, C.; Mester, J.; Klutmann, S. In Vivo Imaging of Mineral Deposition in Carotid Plaque Using 18F-Sodium Fluoride PET/CT: Correlation with Atherogenic Risk Factors. J. Nucl. Med. 2011, 52, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Beheshti, M.; Saboury, B.; Mehta, N.N.; A Torigian, D.; Werner, T.; Mohler, E.; Wilensky, R.; Newberg, A.; Basu, S.; Langsteger, W.; et al. Detection and global quantification of cardiovascular molecular calcification by fluoro18-fluoride positron emission tomography/computed tomography—A novel concept. Hell. J. Nucl. Med. 2011, 14, 114–120. [Google Scholar] [PubMed]
- Piri, R.; Lici, G.; Riyahimanesh, P.; Gerke, O.; Alavi, A.; Høilund-Carlsen, P.F. Two-year change in 18F-sodium fluoride uptake in major arteries of healthy subjects and angina pectoris patients. Int. J. Cardiovasc. Imaging 2021, 37, 3115–3126. [Google Scholar] [CrossRef] [PubMed]
- Blomberg, B.A.; Thomassen, A.; de Jong, P.A.; Lam, M.G.E.; Diederichsen, A.C.P.; Olsen, M.H.; Mickley, H.; Mali, W.; Alavi, A.; Høilund-Carlsen, P.F. Coronary fluorine-18-sodium fluoride uptake is increased in healthy adults with an unfavorable cardiovascular risk profile: Results from the CAMONA study. Nucl. Med. Commun. 2017, 38, 1007–1014. [Google Scholar] [CrossRef]
- Janssen, T.; Bannas, P.; Herrmann, J.; Veldhoen, S.; Busch, J.D.; Treszl, A.; Münster, S.; Mester, J.; Derlin, T. Association of linear 18F-sodium fluoride accumulation in femoral arteries as a measure of diffuse calcification with cardiovascular risk factors: A PET/CT study. J. Nucl. Cardiol. 2013, 20, 569–577. [Google Scholar] [CrossRef]
- Zhang, V.; Borja, A.J.; Rojulpote, C.; Padmanabhan, S.; Patil, S.; Gonuguntla, K.; Revheim, M.-E.; Werner, T.J.; Høilund-Carlsen, P.F.; Alavi, A. Global quantification of pulmonary artery atherosclerosis using 18F-sodium fluoride PET/CT in at-risk subjects. Am. J. Nucl. Med. Mol. Imaging 2020, 10, 119–126. [Google Scholar]
- Kwiecinski, J.; Tzolos, E.; Adamson, P.D.; Cadet, S.; Moss, A.J.; Joshi, N.; Williams, M.C.; van Beek, E.J.; Dey, D.; Berman, D.S.; et al. Coronary 18F-Sodium Fluoride Uptake Predicts Outcomes in Patients with Coronary Artery Disease. J. Am. Coll. Cardiol. 2020, 75, 3061–3074. [Google Scholar] [CrossRef]
- Kitagawa, T.; Yamamoto, H.; Nakamoto, Y.; Sasaki, K.; Toshimitsu, S.; Tatsugami, F.; Awai, K.; Hirokawa, Y.; Kihara, Y. Predictive Value of 18 F-Sodium Fluoride Positron Emission Tomography in Detecting High-Risk Coronary Artery Disease in Combination With Computed Tomography. J. Am. Hear. Assoc. 2018, 7, e010224. [Google Scholar] [CrossRef]
- Patil, S.; Rojulpote, C.; Gonuguntla, K.; Karambelkar, P.; Bhattaru, A.; Raynor, W.; Borja, A.J.; Vuthaluru, K.; Zhang, V.; Werner, T.J.; et al. Association of triglyceride to high density lipoprotein ratio with global cardiac microcalcification to evaluate subclinical coronary atherosclerosis in non-diabetic individuals. Am. J. Cardiovasc. Dis. 2020, 10, 241–246. [Google Scholar]
- Rojulpote, C.; Patil, S.; Gonuguntla, K.; Karambelkar, P.; Bravo, P.E.; Seraj, S.M.; Asadollahi, S.; Raynor, W.Y.; Bhattaru, A.; Borja, A.J.; et al. NaF-PET/CT global assessment in detecting and quantifying subclinical cardiac atherosclerosis and its association with blood pressure in non-dyslipidemic individuals. Am. J. Cardiovasc. Dis. 2020, 10, 101–107. [Google Scholar]
- Borja, A.J.; Bhattaru, A.; Rojulpote, C.; Hancin, E.C.; Detchou, D.K.; Patil, S.; Gonuguntla, K.; Karambelkar, P.; Chinta, S.; Vuthaluru, K.; et al. Association between atherosclerotic cardiovascular disease risk score estimated by pooled cohort equation and coronary plaque burden as assessed by NaF-PET/CT. Am. J. Nucl. Med. Mol. Imaging 2020, 10, 312–318. [Google Scholar]
- Gonuguntla, K.; Rojulpote, C.; Patil, S.; Bhattaru, A.; Karambelkar, P.; Vuthaluru, K.; Raynor, W.Y.; Borja, A.J.; Zhang, V.; Werner, T.J.; et al. Utilization of NaF-PET/CT in assessing global cardiovascular calcification using CHADS2 and CHADS2-VASc scoring systems in high risk individuals for cardiovascular disease. Am. J. Nucl. Med. Mol. Imaging 2020, 10, 293–300. [Google Scholar] [PubMed]
- Dweck, M.R.; Chow, M.W.; Joshi, N.V.; Williams, M.C.; Jones, C.; Fletcher, A.M.; Richardson, H.; White, A.; McKillop, G.; van Beek, E.J.; et al. Coronary Arterial 18F-Sodium Fluoride Uptake: A Novel Marker of Plaque Biology. J. Am. Coll. Cardiol. 2012, 59, 1539–1548. [Google Scholar] [CrossRef] [PubMed]
- Morbelli, S.; Fiz, F.; Piccardo, A.; Picori, L.; Massollo, M.; Pestarino, E.; Marini, C.; Cabria, M.; Democrito, A.; Cittadini, G.; et al. Divergent determinants of 18F-NaF uptake and visible calcium deposition in large arteries: Relationship with Framingham risk score. Int. J. Cardiovasc. Imaging 2014, 30, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Heber, D.; Gonzalez, J.C.; Karanikas, G.; Mayerhoefer, M.E.; Rasul, S.; Beitzke, D.; Zhang, X.; Agis, H.; Mitterhauser, M.; et al. Association Between Osteogenesis and Inflammation During the Progression of Calcified Plaque Evaluated by 18F-Fluoride and 18F-FDG. J. Nucl. Med. 2017, 58, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Bang, J.-I.; Koo, B.-K.; Hwang, D.; Park, J.; Zhang, J.; Yaliang, T.; Suh, M.; Paeng, J.C.; Shiono, Y.; et al. Clinical Relevance of 18 F-Sodium Fluoride Positron-Emission Tomography in Noninvasive Identification of High-Risk Plaque in Patients with Coronary Artery Disease. Circ. Cardiovasc. Imaging 2017, 10. [Google Scholar] [CrossRef]
- Marchesseau, S.; Seneviratna, A.; Sjöholm, T.; Qin, D.L.; Ho, J.X.M.; Hausenloy, D.J.; Townsend, D.W.; Richards, A.M.; Totman, J.J.; Chan, M.Y.Y. Hybrid PET/CT and PET/MRI imaging of vulnerable coronary plaque and myocardial scar tissue in acute myocardial infarction. J. Nucl. Cardiol. 2017, 25, 2001–2011. [Google Scholar] [CrossRef]
- Ishiwata, Y.; Kaneta, T.; Nawata, S.; Hino-Shishikura, A.; Yoshida, K.; Inoue, T. Quantification of temporal changes in calcium score in active atherosclerotic plaque in major vessels by 18F-sodium fluoride PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 1529–1537. [Google Scholar] [CrossRef]
- Fiz, F.; Morbelli, S.; Bauckneht, M.; Piccardo, A.; Ferrarazzo, G.; Nieri, A.; Artom, N.; Cabria, M.; Marini, C.; Canepa, M.; et al. Correlation between thoracic aorta 18F-natrium fluoride uptake and cardiovascular risk. World J. Radiol. 2016, 8, 82–89. [Google Scholar] [CrossRef]
- Arani, L.S.; Zadeh, M.Z.; Saboury, B.; Revheim, M.-E.; Øestergaard, B.; Borja, A.J.; Samarin, D.S.; Seraj, S.M.; Kalbush, E.; Ayubcha, C.; et al. Assessment of atherosclerosis in multiple myeloma and smoldering myeloma patients using 18F- sodium fluoride PET/CT. J. Nucl. Cardiol. 2021, 1–11. [Google Scholar] [CrossRef]
- Takx, R.A.P.; van Asperen, R.; Bartstra, J.W.; Zwakenberg, S.R.; Wolterink, J.M.; Celeng, C.; de Jong, P.A.; Beulens, J.W. Determinants of (18)F-NaF uptake in femoral arteries in patients with type 2 diabetes mellitus. J. Nucl. Cardiol. 2020, 1–6. [Google Scholar] [CrossRef]
- Sorci, O.; Batzdorf, A.S.; Mayer, M.; Rhodes, S.; Peng, M.; Jankelovits, A.R.; Hornyak, J.; Gerke, O.; Høilund-Carlsen, P.F.; Alavi, A.; et al. 18F-sodium fluoride PET/CT provides prognostic clarity compared to calcium and Framingham risk scoring when addressing whole-heart arterial calcification. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1678–1687. [Google Scholar] [CrossRef]
- Piri, R.; Edenbrandt, L.; Larsson, M.; Enqvist, O.; Nøddeskou-Fink, A.H.; Gerke, O.; Høilund-Carlsen, P.F. Aortic wall segmentation in 18F-sodium fluoride PET/CT scans: Head-to-head comparison of artificial intelligence-based versus manual segmentation. J. Nucl. Cardiol. 2021, 1–10. [Google Scholar] [CrossRef]
- Piri, R.; Edenbrandt, L.; Larsson, M.; Enqvist, O.; Skovrup, S.; Iversen, K.K.; Saboury, B.; Alavi, A.; Gerke, O.; Høilund-Carlsen, P.F. “Global” cardiac atherosclerotic burden assessed by artificial intelligence-based versus manual segmentation in 18F-sodium fluoride PET/CT scans: Head-to-head comparison. J. Nucl. Cardiol. 2021, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Crowther, M.A. Pathogenesis of Atherosclerosis. Hematology 2005, 2005, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Cybulsky, M.; A Gimbrone, M.; Libby, P. An atherogenic diet rapidly induces VCAM-1, a cytokine-regulatable mononuclear leukocyte adhesion molecule, in rabbit aortic endothelium. Arter. Thromb. A J. Vasc. Biol. 1993, 13, 197–204. [Google Scholar] [CrossRef]
- Wenger, N.K. Prevention of Cardiovascular Disease: Highlights for the Clinician of the 2013 American College of Cardiology/American Heart Association Guidelines. Clin. Cardiol. 2014, 37, 239–251. [Google Scholar] [CrossRef][Green Version]
- Heidenreich, P.A.; Trogdon, J.G.; Khavjou, O.A.; Butler, J.; Dracup, K.; Ezekowitz, M.D.; Finkelstein, E.A.; Hong, Y.; Johnston, S.C.; Khera, A.; et al. Forecasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation 2011, 123, 933–944. [Google Scholar] [CrossRef] [PubMed]
- Sidney, S.; Quesenberry, C.P.; Jaffe, M.G.; Sorel, M.; Nguyen-Huynh, M.N.; Kushi, L.H.; Go, A.S.; Rana, J.S. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA Cardiol. 2016, 1, 594–599. [Google Scholar] [CrossRef]
- Herrington, W.; Lacey, B.; Sherliker, P.; Armitage, J.; Lewington, S. Epidemiology of Atherosclerosis and the Potential to Reduce the Global Burden of Atherothrombotic Disease. Circ. Res. 2016, 118, 535–546. [Google Scholar] [CrossRef]
- Syed, M.B.; Fletcher, A.; O Forsythe, R.; Kaczynski, J.; E Newby, D.; Dweck, M.R.; Van Beek, E.J. Emerging techniques in atherosclerosis imaging. Br. J. Radiol. 2019, 92, 20180309. [Google Scholar] [CrossRef]
- Takx, R.A.; Partovi, S.; Ghoshhajra, B.B. Imaging of atherosclerosis. Int. J. Cardiovasc. Imaging 2016, 32, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Raynor, W.; Borja, A.J.; Rojulpote, C.; Høilund-Carlsen, P.F.; Alavi, A. 18F-sodium fluoride: An emerging tracer to assess active vascular microcalcification. J. Nucl. Cardiol. 2020, 1–6. [Google Scholar] [CrossRef]
- Høilund-Carlsen, P.F.; Moghbel, M.C.; Gerke, O.; Alavi, A. Evolving Role of PET in Detecting and Characterizing Atherosclerosis. PET Clin. 2019, 14, 197–209. [Google Scholar] [CrossRef]
- Blomberg, B.A.; Bashyam, A.; Ramachandran, A.; Gholami, S.; Houshmand, S.; Salavati, A.; Werner, T.; Zaidi, H.; Alavi, A. Quantifying [18F]fluorodeoxyglucose uptake in the arterial wall: The effects of dual time-point imaging and partial volume effect correction. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 1414–1422. [Google Scholar] [CrossRef] [PubMed]
- McKenney-Drake, M.L.; Moghbel, M.C.; Paydary, K.; Alloosh, M.; Houshmand, S.; Moe, S.; Salavati, A.; Sturek, J.M.; Territo, P.R.; Weaver, C.; et al. 18F-NaF and 18F-FDG as molecular probes in the evaluation of atherosclerosis. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 2190–2200. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, D.; Millon, A.; Fayad, Z.A. Molecular imaging in atherosclerosis: FDG PET. Curr. Atheroscler. Rep. 2012, 14, 429–437. [Google Scholar] [CrossRef]
- Evans, N.R.; Tarkin, J.M.; Chowdhury, M.M.; Warburton, E.A.; Rudd, J.H.F. PET Imaging of Atherosclerotic Disease: Advancing Plaque Assessment from Anatomy to Pathophysiology. Curr. Atheroscler. Rep. 2016, 18, 30. [Google Scholar] [CrossRef]
- Mb, M.M.; Merwick, A.; Mb, O.C.S.; Hannon, N.; Foran, P.; Grant, T.; Dolan, E.; Moroney, J.; Murphy, S.; O’Rourke, K.; et al. Carotid plaque inflammation on 18F-fluorodeoxyglucose positron emission tomography predicts early stroke recurrence. Ann. Neurol. 2012, 71, 709–718. [Google Scholar] [CrossRef]
- Figueroa, A.L.; Subramanian, S.S.; Cury, R.C.; Truong, Q.A.; Gardecki, J.A.; Tearney, G.J.; Hoffmann, U.; Brady, T.J.; Tawakol, A. Distribution of inflammation within carotid atherosclerotic plaques with high-risk morphological features: A comparison between positron emission tomography activity, plaque morphology, and histopathology. Circ. Cardiovasc. Imaging 2012, 5, 69–77. [Google Scholar] [CrossRef]
- Alavi, A.; Werner, T.J.; Høilund-Carlsen, P.F. What can be and what cannot be accomplished with PET to detect and characterize atherosclerotic plaques. J. Nucl. Cardiol. 2017, 25, 2012–2015. [Google Scholar] [CrossRef]
- Wykrzykowska, J.; Lehman, S.; Williams, G.; Parker, J.A.; Palmer, M.R.; Varkey, S.; Kolodny, G.; Laham, R. Imaging of Inflamed and Vulnerable Plaque in Coronary Arteries with 18F-FDG PET/CT in Patients with Suppression of Myocardial Uptake Using a Low-Carbohydrate, High-Fat Preparation. J. Nucl. Med. 2009, 50, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.; Kolodny, G.M. Suppression of Myocardial18F-FDG Uptake by Preparing Patients with a High-Fat, Low-Carbohydrate Diet. Am. J. Roentgenol. 2008, 190, W151–W156. [Google Scholar] [CrossRef]
- Sheikine, Y.; Akram, K. FDG–PET imaging of atherosclerosis: Do we know what we see? Atherosclerosis 2010, 211, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Stiekema, L.C.A.; Schnitzler, J.G.; Nahrendorf, M.; Stroes, E.S.G. The maturation of a ‘neural-hematopoietic’ inflammatory axis in cardiovascular disease. Curr. Opin. Lipidol. 2017, 28, 507–512. [Google Scholar] [CrossRef]
- Heidt, T.; Sager, H.B.; Courties, G.; Dutta, P.; Iwamoto, Y.; Zaltsman, A.; Muhlen, C.V.Z.; Bode, C.; Fricchione, G.L.; Denninger, J.; et al. Chronic variable stress activates hematopoietic stem cells. Nat. Med. 2014, 20, 754–758. [Google Scholar] [CrossRef] [PubMed]
- Blebea, J.S.; Houseni, M.; Torigian, D.A.; Fan, C.; Mavi, A.; Zhuge, Y.; Iwanaga, T.; Mishra, S.; Udupa, J.; Zhuang, J.; et al. Structural and Functional Imaging of Normal Bone Marrow and Evaluation of Its Age-Related Changes. Semin. Nucl. Med. 2007, 37, 185–194. [Google Scholar] [CrossRef]
- Basu, S.; Houseni, M.; Bural, G.; Chamroonat, W.; Udupa, J.; Mishra, S.; Alavi, A. Magnetic Resonance Imaging Based Bone Marrow Segmentation for Quantitative Calculation of Pure Red Marrow Metabolism Using 2-Deoxy-2-[F-18]fluoro-d-glucose- Positron Emission Tomography: A Novel Application with Significant Implications for Combined Structure–Function Approach. Mol. Imaging Biol. 2007, 9, 361–365. [Google Scholar] [CrossRef]
- Fan, C.; Hernandez-Pampaloni, M.; Houseni, M.; Chamroonrat, W.; Basu, S.; Kumar, R.; Dadparvar, S.; Torigian, D.A.; Alavi, A. Age-Related Changes in the Metabolic Activity and Distribution of the Red Marrow as Demonstrated by 2-Deoxy-2-[F-18]fluoro-d-glucose-Positron Emission Tomography. Mol. Imaging Biol. 2007, 9, 300–307. [Google Scholar] [CrossRef]
- Liu, Y. Clinical significance of diffusely increased splenic uptake on FDG-PET. Nucl. Med. Commun. 2009, 30, 763–769. [Google Scholar] [CrossRef]
- Saboury, B.; Edenbrandt, L.; Piri, R.; Gerke, O.; Werner, T.; Arbab-Zadeh, A.; Alavi, A.; Høilund-Carlsen, P. Alavi–Carlsen Calcification Score (ACCS): A Simple Measure of Global Cardiac Atherosclerosis Burden. Diagnostics 2021, 11, 1421. [Google Scholar] [CrossRef]
- Huet, P.; Burg, S.; Le Guludec, D.; Hyafil, F.; Buvat, I. Variability and Uncertainty of 18F-FDG PET Imaging Protocols for Assessing Inflammation in Atherosclerosis: Suggestions for Improvement. J. Nucl. Med. 2015, 56, 552–559. [Google Scholar] [CrossRef]
- Irkle, A.; Vesey, A.T.; Lewis, D.; Skepper, J.N.; Bird, J.; Dweck, M.; Joshi, F.R.; Gallagher, F.A.; Warburton, E.A.; Bennett, M.; et al. Identifying active vascular microcalcification by 18F-sodium fluoride positron emission tomography. Nat. Commun. 2015, 6, 7495. [Google Scholar] [CrossRef]
- Raynor, W.; Houshmand, S.; Gholami, S.; Emamzadehfard, S.; Rajapakse, C.S.; Blomberg, B.A.; Werner, T.J.; Høilund-Carlsen, P.F.; Baker, J.F.; Alavi, A. Evolving Role of Molecular Imaging with 18F-Sodium Fluoride PET as a Biomarker for Calcium Metabolism. Curr. Osteoporos. Rep. 2016, 14, 115–125. [Google Scholar] [CrossRef]
- Høilund-Carlsen, P.F.; Sturek, M.; Alavi, A.; Gerke, O. Atherosclerosis imaging with 18F-sodium fluoride PET: State-of-the-art review. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1538–1551. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Dilsizian, V. PET Assessment of Vascular Inflammation and Atherosclerotic Plaques: SUV or TBR? J. Nucl. Med. 2015, 56, 503–504. [Google Scholar] [CrossRef]
- Høilund-Carlsen, P.F.; Piri, R.; Gerke, O.; Edenbrandt, L.; Alavi, A. Assessment of Total-Body Atherosclerosis by PET/Computed Tomography. PET Clin. 2021, 16, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Slomka, P.J.; Pan, T.; Berman, D.S.; Germano, G. Advances in SPECT and PET Hardware. Prog. Cardiovasc. Dis. 2015, 57, 566–578. [Google Scholar] [CrossRef] [PubMed]
- Tison, G.H.; Guo, M.; Blaha, M.J.; McClelland, R.L.; Allison, M.A.; Szklo, M.; Wong, N.D.; Blumenthal, R.S.; Budoff, M.J.; Nasir, K. Multisite extracoronary calcification indicates increased risk of coronary heart disease and all-cause mortality: The Multi-Ethnic Study of Atherosclerosis. J. Cardiovasc. Comput. Tomogr. 2015, 9, 406–414. [Google Scholar] [CrossRef]
- Adar, A.; Erkan, H.; Gokdeniz, T.; Karadeniz, A.; Cavusoglu, I.G.; Onalan, O. Aortic arch calcification is strongly associated with coronary artery calcification. Vasa 2015, 44, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Høilund-Carlsen, P.F.; Edenbrandt, L.; Alavi, A. Global disease score (GDS) is the name of the game! Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1768–1772. [Google Scholar] [CrossRef]
- Tarkin, J.M.; Joshi, F.R.; Evans, N.R.; Chowdhury, M.M.; Figg, N.L.; Shah, A.V.; Starks, L.T.; Martin-Garrido, A.; Manavaki, R.; Yu, E.; et al. Detection of Atherosclerotic Inflammation by (68)Ga-DOTATATE PET Compared to [(18)F]FDG PET Imaging. J Am. Coll. Cardiol. 2017, 69, 1774–1791. [Google Scholar] [CrossRef]
- Laitinen, I.; Marjamäki, P.; Någren, K.; Laine, V.J.O.; Wilson, I.; Leppänen, P.; Ylä-Herttuala, S.; Roivainen, A.; Knuuti, J. Uptake of inflammatory cell marker [11C]PK11195 into mouse atherosclerotic plaques. Eur. J. Nucl. Med. Mol. Imaging 2008, 36, 73–80. [Google Scholar] [CrossRef]
- Pillarisetti, K.; Gupta, S.K. Cloning and Relative Expression Analysis of Rat Stromal Cell Derived Factor-1 (SDF-1): SDF-1 α mRNA Is Selectively Induced in Rat Model of Myocardial Infarction. Inflammation 2001, 25, 293–300. [Google Scholar] [CrossRef]
- Hu, X.; Dai, S.; Wu, W.J.; Tan, W.; Zhu, X.; Mu, J.; Guo, Y.; Bolli, R.; Rokosh, G. Stromal cell derived factor-1 alpha confers protection against myocardial ischemia/reperfusion injury: Role of the cardiac stromal cell derived factor-1 alpha CXCR4 axis. Circulation 2007, 116, 654–663. [Google Scholar] [CrossRef] [PubMed]
- Derlin, T.; Sedding, D.G.; Dutzmann, J.; Haghikia, A.; König, T.; Napp, L.C.; Schütze, C.; Owsianski-Hille, N.; Wester, H.-J.; Kropf, S.; et al. Imaging of chemokine receptor CXCR4 expression in culprit and nonculprit coronary atherosclerotic plaque using motion-corrected [68Ga]pentixafor PET/CT. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1934–1944. [Google Scholar] [CrossRef] [PubMed]
- Hyafil, F.; Pelisek, J.; Laitinen, I.; Schottelius, M.; Mohring, M.; Döring, Y.; van der Vorst, E.P.; Kallmayer, M.; Steiger, K.; Poschenrieder, A.; et al. Imaging the Cytokine Receptor CXCR4 in Atherosclerotic Plaques with the Radiotracer 68Ga-Pentixafor for PET. J. Nucl. Med. 2017, 58, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Lapa, C.; Reiter, T.; Werner, R.A.; Ertl, G.; Wester, H.-J.; Buck, A.; Bauer, W.; Herrmann, K. [68Ga]Pentixafor-PET/CT for Imaging of Chemokine Receptor 4 Expression After Myocardial Infarction. JACC: Cardiovasc. Imaging 2015, 8, 1466–1468. [Google Scholar] [CrossRef] [PubMed]
- Kircher, M.; Tran-Gia, J.; Kemmer, L.; Zhang, X.; Schirbel, A.; Werner, R.A.; Buck, A.K.; Wester, H.-J.; Hacker, M.; Lapa, C.; et al. Imaging Inflammation in Atherosclerosis with CXCR4-Directed 68Ga-Pentixafor PET/CT: Correlation with 18F-FDG PET/CT. J. Nucl. Med. 2019, 61, 751–756. [Google Scholar] [CrossRef] [PubMed]
- Weiberg, D.; Thackeray, J.T.; Daum, G.; Sohns, J.S.; Kropf, S.; Wester, H.-J.; Ross, T.L.; Bengel, F.; Derlin, T. Clinical Molecular Imaging of Chemokine Receptor CXCR4 Expression in Atherosclerotic Plaque Using 68Ga-Pentixafor PET: Correlation with Cardiovascular Risk Factors and Calcified Plaque Burden. J. Nucl. Med. 2017, 59, 266–272. [Google Scholar] [CrossRef]
- Huisman, M.V.; Barco, S.; Cannegieter, S.C.; Le Gal, G.; Konstantinides, S.V.; Reitsma, P.H.; Rodger, M.; Vonk Noordegraaf, A.; Klok, F.A. Pulmonary embolism. Nat. Rev. Dis. Primers 2018, 4, 18028. [Google Scholar] [CrossRef]
- Goethals, I.; Smeets, P.; De Winter, O.; Noens, L. Focally Enhanced F-18 Fluorodeoxyglucose (FDG) Uptake in Incidentally Detected Pulmonary Embolism on PET/CT Scanning. Clin. Nucl. Med. 2006, 31, 497–498. [Google Scholar] [CrossRef]
- Badr, A.; Joyce, J.M.; Durick, J. Rim of FDG Uptake Around a Pulmonary Infarct on PET/CT in a Patient With Unsuspected Pulmonary Embolism. Clin. Nucl. Med. 2009, 34, 285–286. [Google Scholar] [CrossRef]
- Khandelwal, A.R.; Li, G.; Takalkar, A.M. Incidental Detection of Unsuspected Pulmonary Embolism on Oncologic FDG PET/CT Imaging. Clin. Nucl. Med. 2011, 36, 720–722. [Google Scholar] [CrossRef]
- Nielsen, A.L.; Thomassen, A.; Hess, S.; Alavi, A.; Høilund-Carlsen, P.F. Deep Venous Thrombosis and Pulmonary Embolism Detected by FDG PET/CT in a Patient With Bacteremia. Clin. Nucl. Med. 2013, 38, 276–277. [Google Scholar] [CrossRef]
- Liu, Q.; Zuo, C.; Lv, T.; Cui, B. Pulmonary Embolism Caused by Right Atrial Myxoma on FDG PET/CT. Clin. Nucl. Med. 2013, 38, 928–930. [Google Scholar] [CrossRef] [PubMed]
- Wittram, C.; Scott, J.A. 18F-FDG PET of Pulmonary Embolism. Am. J. Roentgenol. 2007, 189, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Kubota, K.; Morooka, M.; Shida, Y.; Hasuo, K.; Endo, H.; Matsuda, H. Diagnostic usefulness of 18F-FDG PET/CT in the differentiation of pulmonary artery sarcoma and pulmonary embolism. Ann. Nucl. Med. 2009, 23, 671–676. [Google Scholar] [CrossRef] [PubMed]
- Flavell, R.R.; Behr, S.C.; Brunsing, R.L.; Naeger, D.M.; Pampaloni, M.H. The Incidence of Pulmonary Embolism and Associated FDG-PET Findings in IV Contrast-Enhanced PET/CT. Acad. Radiol. 2014, 21, 718–725. [Google Scholar] [CrossRef]
- Al-Mehisen, R.; Al-Halees, Z.; Alnemri, K.; Al-Hemayed, W.; Al-Mohaissen, M. Primary pulmonary artery sarcoma: A rare and overlooked differential diagnosis of pulmonary embolism. Clues to diagnosis. Int. J. Surg. Case Rep. 2019, 65, 15–19. [Google Scholar] [CrossRef]
- Lee, E.J.; Moon, S.H.; Choi, J.Y.; Lee, K.S.; Choi, Y.S.; Choe, Y.S.; Kim, B.-T. Usefulness of fluorodeoxyglucose positron emission tomography in malignancy of pulmonary artery mimicking pulmonary embolism. ANZ J. Surg. 2013, 83, 342–347. [Google Scholar] [CrossRef]
- Xi, X.-Y.; Gao, W.; Gong, J.-N.; Guo, X.-J.; Wu, J.-Y.; Yang, Y.-H.; Yang, M.-F. Value of 18F-FDG PET/CT in differentiating malignancy of pulmonary artery from pulmonary thromboembolism: A cohort study and literature review. Int. J. Cardiovasc. Imaging 2019, 35, 1395–1403. [Google Scholar] [CrossRef]
- Stone, J.; Hangge, P.; Albadawi, H.; Wallace, A.; Shamoun, F.; Knuttien, M.G.; Naidu, S.; Oklu, R. Deep vein thrombosis: Pathogenesis, diagnosis, and medical management. Cardiovasc. Diagn. Ther. 2017, 7, S276–S284. [Google Scholar] [CrossRef] [PubMed]
- Dronkers, C.E.; Klok, E.; Huisman, M.V. Current and future perspectives in imaging of venous thromboembolism. J. Thromb. Haemost. 2016, 14, 1696–1710. [Google Scholar] [CrossRef] [PubMed]
- Rondina, M.T.; Lam, U.T.; Pendleton, R.C.; Kraiss, L.W.; Wanner, N.; Zimmerman, G.A.; Hoffman, J.M.; Hanrahan, C.; Boucher, K.; Christian, P.E.; et al. 18F-FDG PET in the Evaluation of Acuity of Deep Vein Thrombosis. Clin. Nucl. Med. 2012, 37, 1139–1145. [Google Scholar] [CrossRef]
- Hara, T.; Truelove, J.; Tawakol, A.; Wojtkiewicz, G.R.; Hucker, W.J.; MacNabb, M.H.; Brownell, A.-L.; Jokivarsi, K.; Kessinger, C.W.; Jaff, M.R.; et al. 18F-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography Enables the Detection of Recurrent Same-Site Deep Vein Thrombosis by Illuminating Recently Formed, Neutrophil-Rich Thrombus. Circulation 2014, 130, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Hess, S.; Madsen, P.H.; Iversen, E.D.; Frifelt, J.J.; Hoilund-Carlsen, P.F.; Alavi, A. Efficacy of FDG PET/CT imaging for venous thromboembolic disorders: Preliminary results from a prospective, observational pilot study. Clin. Nucl. Med. 2015, 40, e23–e26. [Google Scholar] [CrossRef]
- Zhu, H.J.; Hess, S.; Rubello, D.; Goris, M.L.; Alavi, A. The strong but nonspecific relationship between 18F-FDG uptake in the lower-extremity veins and venous thromboembolism. Nucl. Med. Commun. 2016, 37, 322–328. [Google Scholar] [CrossRef]
- Le Roux, P.-Y.; Robin, P.; Delluc, A.; Tardy, B.; Abgral, R.; Couturaud, F.; Reffad, A.; Le Gal, G.; Salaun, P.-Y. Performance of 18F fluoro-2-désoxy-D-glucose positron emission tomography/computed tomography for the diagnosis of venous thromboembolism. Thromb. Res. 2015, 135, 31–35. [Google Scholar] [CrossRef]
- Miceli, M.; Atoui, R.; Walker, R.; Mahfouz, T.; Mirza, N.; Diaz, J.; Tricot, G.; Barlogie, B.; Anaissie, E. Diagnosis of Deep Septic Thrombophlebitis in Cancer Patients by Fluorine-18 Fluorodeoxyglucose Positron Emission Tomography Scanning: A Preliminary Report. J. Clin. Oncol. 2004, 22, 1949–1956. [Google Scholar] [CrossRef] [PubMed]
- Davidson, T.; Goitein, O.; Avigdor, A.; Zwas, S.T.; Goshen, E. 18F- FDG-PET/CT for the diagnosis of tumor thrombosis. Isr. Med Assoc. J.: IMAJ 2009, 11, 69–73. [Google Scholar] [PubMed]
- Hess, S.; Madsen, P.H.; Basu, S.; Høilund-Carlsen, P.F.; Alavi, A. Potential Role of FDG PET/CT Imaging for Assessing Venous Thromboembolic Disorders. Clin. Nucl. Med. 2012, 37, 1170–1172. [Google Scholar] [CrossRef]
- Kaghazchi, F.; Borja, A.J.; Hancin, E.C.; Bhattaru, A.; E Detchou, D.K.; Seraj, S.M.; Rojulpote, C.; Hess, S.; Nardo, L.; E Gabriel, P.; et al. Venous thromboembolism detected by FDG-PET/CT in cancer patients: A common, yet life-threatening observation. Am. J. Nucl. Med. Mol. Imaging 2021, 11, 99–106. [Google Scholar] [PubMed]
- Gulati, A.; Bagga, A. Large vessel vasculitis. Pediatr. Nephrol. 2010, 25, 1037–1048. [Google Scholar] [CrossRef]
- Schäfer, V.S.; Jin, L.; Schmidt, W.A. Imaging for Diagnosis, Monitoring, and Outcome Prediction of Large Vessel Vasculitides. Curr. Rheumatol. Rep. 2020, 22, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Tateishi, U.; Tsuchiya, J.; Yokoyama, K. Large vessel vasculitis: Imaging standards of 18F-FDG PET/CT. Jpn. J. Radiol. 2020, 39, 225–232. [Google Scholar] [CrossRef]
- Liddy, S.; Mallia, A.; Collins, C.D.; Killeen, R.P.; Skehan, S.; Dodd, J.D.; Subesinghe, M.; Murphy, D.J. Vascular findings on FDG PET/CT. Br. J. Radiol. 2020, 93, 20200103. [Google Scholar] [CrossRef] [PubMed]
- Bucerius, J. Monitoring Vasculitis with 18F-FDG PET. Q J Nucl Med Mol Imaging 2016, 60, 219–235. [Google Scholar]
- Sammel, A.M.; Hsiao, E.; Schembri, G.; Nguyen, K.; Brewer, J.; Schrieber, L.; Janssen, B.; Youssef, P.; Fraser, C.; Bailey, E.; et al. Diagnostic Accuracy of Positron Emission Tomography/Computed Tomography of the Head, Neck, and Chest for Giant Cell Arteritis: A Prospective, Double-Blind, Cross-Sectional Study. Arthritis Rheumatol. 2019, 71, 1319–1328. [Google Scholar] [CrossRef]
- Hay, B.; Mariano-Goulart, D.; Bourdon, A.; Benkiran, M.; Vauchot, F.; De Verbizier, D.; Ben Bouallègue, F. Diagnostic performance of 18F-FDG PET-CT for large vessel involvement assessment in patients with suspected giant cell arteritis and negative temporal artery biopsy. Ann. Nucl. Med. 2019, 33, 512–520. [Google Scholar] [CrossRef]
- Nielsen, B.D.; Hansen, I.T.; Kramer, S.; Haraldsen, A.; Hjorthaug, K.; Bogsrud, T.V.; Ejlersen, J.A.; Stolle, L.B.; Keller, K.K.; Therkildsen, P.; et al. Simple dichotomous assessment of cranial artery inflammation by conventional 18F-FDG PET/CT shows high accuracy for the diagnosis of giant cell arteritis: A case-control study. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Blockmans, D.E.; De Ceuninck, L.; Vanderschueren, S.; Knockaert, D.; Mortelmans, L.; Bobbaers, H. Repetitive 18F-fluorodeoxyglucose positron emission tomography in giant cell arteritis: A prospective study of 35 patients. Arthritis Rheum. 2006, 55, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Keser, G.; Aksu, K. Diagnosis and differential diagnosis of large-vessel vasculitides. Rheumatol. Int. 2019, 39, 169–185. [Google Scholar] [CrossRef] [PubMed]
- Incerti, E.; Tombetti, E.; Fallanca, F.; Baldissera, E.M.; Alongi, P.; Tombolini, E.; Sartorelli, S.; Sabbadini, M.G.; Papa, M.; DE Cobelli, F.; et al. 18F-FDG PET reveals unique features of large vessel inflammation in patients with Takayasu’s arteritis. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Soussan, M.; Nicolas, P.; Schramm, C.; Katsahian, S.; Pop, G.; Fain, O.; Mekinian, A. Management of large-vessel vasculitis with FDG-PET: A systematic literature review and meta-analysis. Medicine (Baltimore) 2015, 94, e622. [Google Scholar] [CrossRef]
- Salvarani, C.; Gabriel, S.E.; O’Fallon, W.M.; Hunder, G.G. The incidence of giant cell arteritis in Olmsted County, Minnesota: Apparent fluctuations in a cyclic pattern. Ann. Intern. Med. 1995, 123, 192–194. [Google Scholar] [CrossRef]
- Henckaerts, L.; Gheysens, O.; Vanderschueren, S.; Goffin, K.; Blockmans, D. Use of 18F-fluorodeoxyglucose positron emission tomography in the diagnosis of polymyalgia rheumatica—A prospective study of 99 patients. Rheumatology 2018, 57, 1908–1916. [Google Scholar] [CrossRef] [PubMed]
- Yuge, S.; Nakatani, K.; Yoshino, K.; Koyama, T. Diagnosing polymyalgia rheumatica on 18F-FDG PET/CT: Typical uptake patterns. Ann. Nucl. Med. 2018, 32, 573–577. [Google Scholar] [CrossRef]
- van der Geest, K.S.M.; Treglia, G.; Glaudemans, A.W.J.M.; Brouwer, E.; Jamar, F.; Slart, R.H.J.A.; Gheysens, O. Diagnostic value of [18F]FDG-PET/CT in polymyalgia rheumatica: A systematic review and meta-analysis. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1876–1889. [Google Scholar] [CrossRef]
- Vitiello, G.; Battaglini, C.O.; Carli, G.; Radice, A.; Matucci, A.; Vultaggio, A.; Olianti, C.; Parronchi, P.; Maggi, E.; Cammelli, D. Tocilizumab in Giant Cell Arteritis: A Real-Life Retrospective Study. Angiology 2018, 69, 763–769. [Google Scholar] [CrossRef]
- Grayson, P.C.; Alehashemi, S.; Bs, A.A.B.; Civelek, A.C.; Cupps, T.R.; Kaplan, M.J.; Malayeri, A.A.; Merkel, P.A.; Rn, E.N.; Bluemke, D.A.; et al. 18F-Fluorodeoxyglucose-Positron Emission Tomography As an Imaging Biomarker in a Prospective, Longitudinal Cohort of Patients With Large Vessel Vasculitis. Arthritis Rheumatol. 2018, 70, 439–449. [Google Scholar] [CrossRef] [PubMed]
- DellaVedova, L.; Carletto, M.; Faggioli, P.; Sciascera, A.; Del Sole, A.; Mazzone, A.; Maffioli, L.S. The prognostic value of baseline 18F-FDG PET/CT in steroid-naïve large-vessel vasculitis: Introduction of volume-based parameters. Eur. J. Nucl. Med. Mol. Imaging 2015, 43, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Muratore, F.; Crescentini, F.; Spaggiari, L.; Pazzola, G.; Casali, M.; Boiardi, L.; Pipitone, N.; Croci, S.; Galli, E.; Aldigeri, R.; et al. Aortic dilatation in patients with large vessel vasculitis: A longitudinal case control study using PET/CT. Semin. Arthritis Rheum. 2019, 48, 1074–1082. [Google Scholar] [CrossRef]
- Schmall, J.P.; Karp, J.S.; Alavi, A. The Potential Role of Total Body PET Imaging in Assessment of Atherosclerosis. PET Clin. 2019, 14, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Bedmutha, A.S.; Singh, N.; Shivdasani, D. Metabolic imaging as a novel strategy in evaluation of mycotic abdominal aortic aneurysm: A case report and brief clinical review. Indian J. Nucl. Med. IJNM Off. J. Soc. Nucl. Med. India 2017, 32, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.J.; Lee, J.S.; Cheong, M.H.; Byun, S.S.; Hyun, I.Y. F-18 FDG PET/CT in the Management of Infected Abdominal Aortic Aneurysm Due To Salmonella. Clin. Nucl. Med. 2008, 33, 492–495. [Google Scholar] [CrossRef]
- Murakami, M.; Morikage, N.; Samura, M.; Yamashita, O.; Suehiro, K.; Hamano, K. Fluorine-18-Fluorodeoxyglucose Positron Emission Tomography–Computed Tomography for Diagnosis of Infected Aortic Aneurysms. Ann. Vasc. Surg. 2014, 28, 575–578. [Google Scholar] [CrossRef]
- Kim, S.-J.; Lee, S.-W.; Jeong, S.Y.; Pak, K.; Kim, K. A systematic review and meta-analysis of 18F-fluorodeoxyglucose positron emission tomography or positron emission tomography/computed tomography for detection of infected prosthetic vascular grafts. J. Vasc. Surg. 2019, 70, 307–313. [Google Scholar] [CrossRef]
- Pacella, S. Mycotic coronary aneurysm detected by 18F-FDG PET/CT: A case report. J. Nucl. Cardiol. 2020, 1–2. [Google Scholar] [CrossRef]
- Calais, J.; Pasi, N.; Nguyen, V.; Hyafil, F. Mycotic aneurysm in a pulmonary artery detected with 18F-fluorodeoxyglucose positron emission tomography/computed tomography imaging. Eur. Heart J. 2017, 46, 3474. [Google Scholar] [CrossRef]
- Morimoto, M.; Norikane, T.; Yamamoto, Y.; Mitamura, K.; Nishiyama, Y. Early infected aneurysm with 18F-FDG uptake prior to substantial anatomical changes. J. Nucl. Cardiol. 2018, 26, 1373–1375. [Google Scholar] [CrossRef]
- Inoue, D.; Yoshida, K.; Yoneda, N.; Ozaki, K.; Matsubara, T.; Nagai, K.; Okumura, K.; Toshima, F.; Toyama, J.; Minami, T.; et al. IgG4-related disease: Dataset of 235 consecutive patients. Medicine 2015, 94, e680. [Google Scholar] [CrossRef] [PubMed]
- Kamisawa, T.; Zen, Y.; Pillai, S.; Stone, J.H. IgG4-related disease. Lancet 2015, 385, 1460–1471. [Google Scholar] [CrossRef]
- Nikiphorou, E.; Galloway, J.; Fragoulis, G.E. Overview of IgG4-related aortitis and periaortitis. A decade since their first description. Autoimmun. Rev. 2020, 19, 102694. [Google Scholar] [CrossRef] [PubMed]
- Ferfar, Y.; Charlotte, F.; Cacoub, P.; Saadoun, D. Temporal arteritis in IgG4 related disease. Jt. Bone Spine 2021, 88, 105087. [Google Scholar] [CrossRef]
- Huang, H.L.; Fong, W.; Peh, W.M.; A Niraj, K.; Lam, W.W. The Utility of FDG PET/CT in IgG4-Related Disease with a Focus on Coronary Artery Involvement. Nucl. Med. Mol. Imaging 2017, 52, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Tajima, M.; Nagai, R.; Hiroi, Y. IgG4-Related Cardiovascular Disorders. Int. Heart J. 2014, 55, 287–295. [Google Scholar] [CrossRef]
- Tang, C.Y.L.; Chua, W.M.; Cheng, L.T.J.; Fong, W.; Zaheer, S.; Lam, W.W.-C. 18F-FDG PET/CT Manifestations of IgG4-related Disease. Br. J. Radiol. 2021, 20210105. [Google Scholar] [CrossRef]
- Zhang, J.; Chen, H.; Ma, Y.; Xiao, Y.; Niu, N.; Lin, W.; Wang, X.; Liang, Z.; Zhang, F.; Li, F.; et al. Characterizing IgG4-related disease with 18F-FDG PET/CT: A prospective cohort study. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 1624–1634. [Google Scholar] [CrossRef]
- Tong, A.K.-T.; Tan, S.-Y.; Go, Y.-Y.; Lam, W.W.-C. Cardiac Structural Abnormalities Associated With IgG4-Related Coronary Periarteritis and Inflammation Revealed by Multimodality Imaging. Can. J. Cardiol. 2014, 30, 956.e15–956.e17. [Google Scholar] [CrossRef]
- Orozco-Gálvez, O.; Fernández-Codina, A.; Simó-Perdigo, M.; Pinal-Fernández, I.; Martínez-Valle, F. Response to Treatment in IgG4-Related Disease Assessed by Quantitative PET/CT Scan. Clin. Nucl. Med. 2021, 46, e307–e311. [Google Scholar] [CrossRef] [PubMed]

| Author Publication Year Country [Ref. #] | Subjects | Objectives | n (Female) Age in Years, Mean ± SD or Range | Arterial Segments | Findings |
|---|---|---|---|---|---|
| Yun et al. April 2001. PA, USA. [23] | Patients who have undergone FDG-PET scans. | To evaluate the vascular uptake in FDG-PET imaging in different age groups. | 137 (74) 20–80 | Abdominal aorta, iliac, femoral, and popliteal arteries. | There was a significant difference in vascular uptake in FDG imaging between patients who were older than 60 years old (61%; 33/54) and those who were younger than 40 years old (34%; 12/35), with the p-value of 0.017. There was strong positive correlation between age groups and the prevalence of FDG vascular uptake (r = 0.99) as well. |
| Van der Valk et al. April 2016. Amsterdam, The Netherlands. [24] | Healthy subjects, patients with risk factors, and patients with CVD. | To compare the uptake of FDG in healthy subjects and patients with risk factors or with CVD. | 83 (24) 61 ± 8 | Carotid arteries and ascending aorta. | SUVmax gradually increased from healthy subjects to subjects with CVD. 96% of the patients with CVD risk factors and all patients with known CVD had at least one active slice on the imaging while only 48% of healthy subjects had the similar findings. |
| Tawakol et al. May 2006. Boston, Massachusetts. [25] | Patients with 70% to 99% carotid artery stenosis who were planned for CEA | To identify the correlation between FDG uptake and atherosclerotic plaque inflammation. | 17 (6) 62 ± 6 | Carotid arteries. | Macrophage staining and CD68 staining were used to assess the inflammation of atherosclerotic plaques, and TBR was used to assess FDG uptake. There was significant correlation between TBR and the macrophage staining (r = 0.70; p < 0.0001), as well as with the CD68 staining (r = 0.85; p < 0.0001). |
| Myers et al. Jan 2012. New York, USA. [26] | Patients with symptomatic femoral arterial disease. | To determine correlation between arterial FDG uptake and atherosclerotic plaque biomarkers. | 30 67 ± 10 | Aorta, carotid and femoral arteries. | There was no significant correlation between CD68 level which is the measure of macrophage content and TBR in the peripheral arteries (r = 0.21). The mean TBR of the carotid artery was 45% higher than that of peripheral artery (p < 0.05). |
| Yun et al. Jan 2002. PA, USA. [27] | Patients who were referred for various clinical evaluations. | To assess the FDG uptake in the different large arteries and the relationship with CVD risk factors. | 156 (86) 0–96 | Abdominal aorta, iliac, and proximal femoral arteries. | Age was the most significant risk factor in all three arteries studied. Hypercholesterolemia was another risk factor that had significant correlation FDG uptake in abdominal aorta and iliac arteries. |
| Bural et at. March 2008. PA, USA. [28] | Subjects who underwent FDG-PET imaging for the assessment of disease other than CVD. | To study how aging affects the changes of FDG uptake in large arteries. | 149 (88) 5–83 | Aorta, iliac and femoral arteries. | As patients aged, the mean SUVs of all arterial segments except abdominal aorta increased significantly (p < 0.01). |
| Strobl et al. Aug 2013. Munich, Germany. [29] | Subjects who underwent PET/CT scan for a noncardiovascular indication. | To evaluate the effect of age, gender and cardiovascular risk factors on vessel wall inflammation and calcified plaque burden. | 315 (192) 57.8 ± 13.7 | Thoracic and abdominal aorta, common carotid, and iliac arteries. | In all vessels studied, the inflammation of the vessel wall and the calcified plaque burden were significantly associated with age > 65 years (p < 0.05). However, the impact of other CVD risk factors differs depending on site. |
| Pasha et al. Feb 2015. PA, USA. [30] | Patients with melanoma. | To quantify FDG uptake in the aorta and peripheral arteries and evaluate the impact of age and CVD risk factors on the uptake of FDG. | 76 (30) 22–91 | Aorta, iliac, and femoral arteries. | Increasing age was significantly associated with increasing FDG uptake in the aorta and peripheral arteries. Nonetheless, the impact of cardiovascular risk factors on FDG uptake was only significant in the aorta (p < 0.05). |
| Rudd et al. April 2002. Cambridge, UK. [31] | Patients with symptomatic carotid atherosclerosis | To assess plaque inflammation in patients with symptomatic carotid artery disease using FDG-PET. | 8 (2) 48–71 | Carotid artery. | FDG-PET was able to visualize all symptomatic carotid plaques and no measurable uptake detected in normal carotid arteries. The accumulation rate of FDG was 27% higher in symptomatic lesions than in contralateral asymptomatic lesions. |
| Al-Zaghal et al. June 2020. PA, USA. [32] | Healthy controls and subjects with suspected lung malignancy. | To investigate the feasibility of FDG-PET/CT to detect pulmonary artery atherosclerosis and its correlation with abnormal PFT. | 29 (0) 57–75 | Pulmonary artery | Although the FDG uptake was higher in patients than in the control group, there was no statistically significant difference between non-COPD and COPD patients, indicating that the atherosclerotic process is a focal process. |
| Arani et al. April 2019. PA, USA. [33] | Healthy volunteers and patients with chest pain syndrome. | To study the association of FDG and NaF uptake with age and CVD risk factors. | 123 (61) 48 ± 14 | Abdominal aorta. | There was a positive correlation between NaF uptake with age (r = 0.35, p < 0.001) and 10 years FRS (r = 0.30, p < 0.001); however, no correlation was seen in the global uptake of FDG. |
| Blomberg et al. Oct 2016. Odense, Denmark. [34] | Healthy volunteers and patients with chest pain syndrome. | To identify the association between CVD risk with arterial inflammation, vascular calcification metabolism, and vascular calcium burden in a population at low CVD risk. | 139 (67) 49 ± 14 | Thoracic aorta. | Increased vascular calcification metabolism and vascular calcium burden were noted in subjects with unfavourable CVD risk profile. No association was noted with arterial inflammation. |
| Ben-Haim et al. Nov 2004. Haifa, Israel. [35] | Cancer patients who are 50 years or older. | To assess the imaging patterns of vascular-wall FDG uptake and CT calcifications in the wall of large arteries. | 122 (47) 66 ± 9 | Thoracic aorta, abdominal and carotid arteries. | Increased FDG uptake was present in 6% of sites (16% of patients) with concomitant vascular calcifications observed on CT and in 7% of sites (21% of patients) with no corresponding structural findings. |
| Tatsumi et al. Dec 2003. MD, USA. [36] | Patients who were known to have or were suspected of having cancers. | To evaluate the FDG uptake in the thoracic aortic wall by PET/CT imaging and compare the FDG uptake with the aortic wall calcification. | 85 (39) 55 ± 16 | Thoracic aorta and descending aorta | PET/CT depicted FDG uptake commonly in the thoracic aortic wall. The FDG uptake site was mostly distinct from the calcification site and may possibly be located in areas of metabolic activity of atherosclerotic changes. |
| Mierelles et al. Feb 2011. NY, USA. [37] | Patients with cancer. | To evaluate the stability of 18F-FDG uptake and vascular calcification using serial FDG scans. | 100 (49) 20–80 | Thoracic aorta. | Seventy percent of patients have positive 18F-FDG uptake on the first scan, however it was positive only in 55% of the patients on second scans. The co-existence of calcification and 18F-FDG uptake were only present in two cases. |
| Tawakol et al. Jan 2017. MA, USA. [38] | Individuals aged 30 years or older without known CVD or active cancer disorders. | To study the association of metabolic activity of amygdala with hematopoietic activity, arterial inflammation, and risk of future CVD. | 293 (169) 45–65 | Amygdala. | There was significant association between amygdalar activity with increased bone marrow activity, arterial inflammation, and risk of CVD events. |
| Blombery et al. June 2014. Odense, Denmark. [39] | Healthy controls and patients with chest pain. | To determine if delayed 18-FDG scans improves the evaluation of atherosclerotic plaque inflammation. | 40 48.0 ± 14.9 | Carotid arteries and thoracic aorta. | Delayed FDG imaging improves the evaluation, evidenced by significant positive relations observed between SCORE % and carotid and aortic SUVmax at 180 min but not at 90 min. |
| Author Publication Year Country [Ref. #] | Subjects | Objectives | n (Female) Age in Years, Mean ± SD or Range | Arterial Segments | Findings |
|---|---|---|---|---|---|
| Joshi et al. Feb 2014. Edinburgh, UK. [14] | Patients with MI and stable angina. | To study the ability of NaF and FDG to identify ruptured and high-risk atherosclerotic plaques. | 80 (7) 62 ± 8 (MI) 67 ± 8 (stable angina) | Proximal and mid-portions of the coronary arteries. | In 93% of the patients with MI, there was increased NaF uptake in the culprit plaque compared with non-culprit plaque (p < 0.0001) while there were no differences in coronary FDG uptake between culprit and nonculprit plaques. |
| Derlin et al. June 2010. Hamburg, Germany. [40] | Subjects who have undergone NaF PET/CT for the exclusion of bone metastases. | To study the relationship of vascular NaF uptake and arterial calcification in major arteries. | 75 (48) 65.2 ± 12.3 | Thoracic aorta, abdominal aorta, common carotid, iliac, and femoral arteries. | There was significant association between the vascular NaF uptake with the arterial calcification of the vessels studied (p < 0.0001). |
| Derlin et al. March 2011. Hamburg, Germany. [41] | Oncologic patients. | To correlate NaF accumulation in the common carotid arteries of neurologically asymptomatic patients with cardiovascular risk factors and carotid calcified plaque burden. | 269 (166) 66.1 ± 12.4 | Common carotid arteries. | There was significant association between NaF uptake with patients’ age (p < 0.0001), male (p < 0.0001), hypertension (p < 0.002), and hypercholesterolemia (p < 0.05). In conclusion, the correlation between the NaF uptake and number of present cardiovascular risk factors was strong (r = 0.30, p < 0.0001). |
| Behesti et al. August 2011. Linz, Austria. [42] | Patients who had undergone 18F-NaF-PET/CT for evaluation of malignancies. | To study the prevalence of regional (aorta) and global (cardiac) NaF uptake and the association with age. | 51 (34) 29–90 | Heart and aorta. | As patients aged, there was a significant increase in NaF uptake in the heart and aorta (p <0.01). |
| Piri et al. May 2021. Odense, Denmark. [43] | Healthy subjects and patients with angina pectoris. | To study the changes of carotid and aortic NaF uptake in 2 years. | 49 (23) 21–75 | Carotid arteries and aorta. | For both carotid arteries and aorta, patients with chest pain have slightly higher NaF uptake than the control group at baseline and after 2 years. However, the 2-year changes in both groups are very small and not significant. |
| Blomberg et al. Aug 2017. Odense, Denmark. [44] | Healthy subjects with low CVD risk. | To study the relationship between NaF uptake and CVD risk. | 89 (42) 21–75 | Coronary artery. | There were significant association between NaF uptake with female sex (p = 0.009), age (p = 0.002), and BMI (p < 0.001). The uptake of NaF increased linearly with the number of cardiovascular risk factors present (p < 0.001). |
| Janssen et al. Aug 2013. Hamburg, Germany. [45] | Oncologic patients. | To assess the correlation of NaF with cardiovascular risk factors and CPB. | 409 (233) 25.1 ± 4.2 | Femoral arteries. | As the number of CVD risk factors increased, the prevalence of NaF increased (p < 0.0001). There was a significant correlation between the NaF uptake with age, hypertension, hypercholesterolemia, diabetes, history of smoking, prior CVD, and CPB. |
| Zhang et al. April 2020. PA, USA. [46] | Healthy controls and subjects with suspected stable angina pectoris. | To assess the calcification of pulmonary arteries through NaF-PET/CT. | 30 (6) 45 ± 8 (healthy controls) 56 ± 11 (at risk subjects) | Pulmonary arteries. | Patients at-risk demonstrated significantly higher NaF uptake compared to healthy controls (p < 0.05). |
| Kwiecinski et al. June 2020. CA, USA. [47] | Patients with known CAD. | To study the prediction of MI using NaF PET. | 293 (46) 65 ± 9 | Coronary artery. | There was an increase in NaF activity in 69% (203/293) of the patients and MI occurred only in these patients. |
| Kitagawa et al. Oct 2018. Hiroshima, Japan. [48] | Patients with ≥1 coronary atherosclerotic lesion detected on CCTA. | To investigate the utility of NaF uptake for predicting coronary events. | 41 (8) 66 ± 9 | Coronary artery. | Patients with coronary events had higher uptake than those without (p = 0.0034). |
| Patil et al. Aug 2020. PA, USA. [49] | Healthy, nondiabetic individuals. | To assess the correlation of TG/HDL ratio and subclinical coronary atherosclerosis. | 68 (35) 41.7 ± 13.5 | Coronary artery. | There was independent association between TG/HDL ratio and global cardiac aSUVmean (95% CI: 0.007–0.114, p = 0.027). |
| Rojulpote et al. Jun 2020. PA, USA. [50] | Healthy, non-dyslipidemic individuals. | To assess early atherosclerosis in individuals with a coronary calcium score of zero. | 20 (8) 41.6 ± 13.8 | Coronary artery. | Diastolic blood pressure and mean arterial pressure were correlated with cardiac NaF uptake independently. |
| Borja et al. Dec 2020. PA, USA. [51] | Individuals without known ASCVD. | To study the correlation of global coronary NaF quantification with ASCVD risk score. | 61 (32) 53.4 ± 8.9 | Coronary artery. | ASCVD risk score was significantly correlated to aSUVmean (r = 0.27, p = 0.03). |
| Gonuguntla et al. Sep 2020. PA, USA. [52] | Individuals with high risk factors of developing CVD events. | To evaluate the correlation of CHADS2 and CHA2DS2-VASc scores with NaF uptake in atherosclerotic plaque. | 40 ( 22) 55 ± 11.9 SD | Coronary artery. | A higher CHADS2 and CHA2DS2-VASc scores correlate with a higher atherosclerotic burden, posting a greater risk of CVD events. |
| Dweck et al. April 2012. Cambridge, UK. [53] | Subjects with or without aortic valve disease. | To study the uptake of NaF as a marker of calcification and 18F-FDG as a marker of inflammation. | 119 (38) 72 ± 8 | Coronary arteries and aorta. | There was no increase in FDG uptake in both patients with atherosclerosis and control groups. However, higher rates of prior CVD events, angina, and higher FRS were noted in patients with increased coronary NaF activity. |
| Morbelli et al. Nov 2013. Genoa, Italy. [54] | Individuals with a history of breast or prostate cancer. | To investigate the relationship of the NaF uptake with FRS. | 80 (60) 65.3 ± 8.2 | Aorta, iliac, femoral, subclavian, and carotid arteries. | There was significant correlation between NaF uptake with all cardiovascular risk (age, diabetes, smoking, and systolic blood pressure), except the body mass index. |
| Li et al. June 2017. Vienna, Austria. [55] | Individuals with myeloma. | To investigate association between osteogenesis and inflammation during the progression of calcified plaque. | 34 (8) 68 ± 9 | Carotid arteries, aorta, and iliac arteries. | Noncalcified lesions have significant higher FDG uptakes than mildly or severely calcified lesions. During plaque progression, there was a concordant progression of inflammation and osteogenesis in 86% of noncalcified lesions, 81% of mildly calcified lesions, and less than 50% in severely calcified lesions. |
| Lee et al. Nov 2017. Seoul, Republic of Korea. [56] | Patients with suspected CAD. | To evaluate the NaF uptake in patients with CAD. | 51 (6) 62.3 ± 8.2 | Coronary artery. | The uptake of NaF in plaques with high-risk characteristics was significantly higher than in those without. |
| Marchesseau et al. Apr 2017. Singapore. [57] | Patients with STEMI undergoing primary PCI. | To study the combination of CT and NaF in detecting coronary lesions. | 10 (1) 48 ± 7 | Coronary artery. | NaF was able to detect myocardial scar tissues concurrently and its uptake was greater in high risk lesions than stable plaques. |
| Ishiwata et al. Aug 2017. Kanagawa, Japan. [58] | Patients with malignancy or orthopaedic disease. | To assess whether NaF PET/CT is able to predict progression of the CT calcium score. | 34 (18) 57.5 ± 13.9 | Aorta and common iliac artery. | There was a strong correlation between NaF uptake with calcium score progression, which was a predictor of future CVD risk, but no correlation was found between 18F-NaF uptake and calcification. |
| Fiz et al. Jan 2016. Genoa, Italy. [59] | Patients with breast or prostate cancer. | To study the correlation between thoracic and cardiac NaF uptake. | 78 (44) 63.3 ± 8.2 | Thoracic aorta. | Although there was correlation between TBR and CVR in the whole thoracic aorta (r = 0.67), the correlation was stronger in the descending thoracic segment (r = 0.75), compared to the aortic arch (r = 0.55) and the ascending segment (r = 0.53). |
| Arani et al. Nov 2020 PA, USA. [60] | Individuals with multiple myeloma and smoldering myeloma. | To assess the atherosclerosis risk in multiple myeloma and smoldering myeloma patients using NaF. | 44 (14) 50–75 | Aorta and whole heart. | Compared to controlled groups, patients with multiple myeloma demonstrated higher NaF uptake in the thoracic aorta and whole heart. |
| Takx et al. March 2020. Utrecht, The Netherlands. [61] | Subjects with type 2 diabetes and known arterial disease. | To evaluate the potential of NaF uptake as a determinant of arterial calcification in femoral arteries. | 68 (16) 69 ± 8 | Femoral arteries. | Higher NaF uptake was associated with higher CT calcium mass, total cholesterol, and HbA1c but not with smokers, male sex, or other medications. |
| Sorci et al. May 2020. Odense, Denmark. [62] | Healthy controls and patients who had experienced persistent chest pain. | To evaluate the benefit of utilizing NaF over calcium and FRS for potential preventive CAD intervention. | 136 (68) 21–75 | Coronary arteries. | In NaF PET/CT, patients have higher aSUVmeans compared to the control group, which is different from using the calcium score. Although FRS echoed the same, it was not sensitive enough to predict the patient status. |
| Piri et al. May 2021. Odense, Denmark. [63] | Healthy subjects with low CVD risk. | To evaluate the accuracy of CNN-based method for automated segmentation of the aortic wall in PET/CT scans. | 49 (23) 52 ± 12 | Aorta. | The automated CNN-based approach was faster than the manually obtained value and the SUV- mean values of both were comparable. |
| Piri et al. Aug 2021. Odense, Denmark. [64] | Healthy subjects and patients with chest pain. | To compare an AI- based method for cardiac segmentation in PET/CT scans with manual segmentation to assess global cardiac atherosclerosis burden. | 49 (23) 52 ± 12 | Heart. | The CNN-based method was faster and provided comparable values to the manually obtained value. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raynor, W.Y.; Park, P.S.U.; Borja, A.J.; Sun, Y.; Werner, T.J.; Ng, S.J.; Lau, H.C.; Høilund-Carlsen, P.F.; Alavi, A.; Revheim, M.-E. PET-Based Imaging with 18F-FDG and 18F-NaF to Assess Inflammation and Microcalcification in Atherosclerosis and Other Vascular and Thrombotic Disorders. Diagnostics 2021, 11, 2234. https://doi.org/10.3390/diagnostics11122234
Raynor WY, Park PSU, Borja AJ, Sun Y, Werner TJ, Ng SJ, Lau HC, Høilund-Carlsen PF, Alavi A, Revheim M-E. PET-Based Imaging with 18F-FDG and 18F-NaF to Assess Inflammation and Microcalcification in Atherosclerosis and Other Vascular and Thrombotic Disorders. Diagnostics. 2021; 11(12):2234. https://doi.org/10.3390/diagnostics11122234
Chicago/Turabian StyleRaynor, William Y., Peter Sang Uk Park, Austin J. Borja, Yusha Sun, Thomas J. Werner, Sze Jia Ng, Hui Chong Lau, Poul Flemming Høilund-Carlsen, Abass Alavi, and Mona-Elisabeth Revheim. 2021. "PET-Based Imaging with 18F-FDG and 18F-NaF to Assess Inflammation and Microcalcification in Atherosclerosis and Other Vascular and Thrombotic Disorders" Diagnostics 11, no. 12: 2234. https://doi.org/10.3390/diagnostics11122234
APA StyleRaynor, W. Y., Park, P. S. U., Borja, A. J., Sun, Y., Werner, T. J., Ng, S. J., Lau, H. C., Høilund-Carlsen, P. F., Alavi, A., & Revheim, M.-E. (2021). PET-Based Imaging with 18F-FDG and 18F-NaF to Assess Inflammation and Microcalcification in Atherosclerosis and Other Vascular and Thrombotic Disorders. Diagnostics, 11(12), 2234. https://doi.org/10.3390/diagnostics11122234









