Role of Contrast-Enhanced Ultrasonography in Hepatocellular Carcinoma by Using LI-RADS and Ancillary Features: A Single Tertiary Centre Experience
Abstract
:1. Introduction
2. Materials and Methods
2.1. CEUS Interpretation
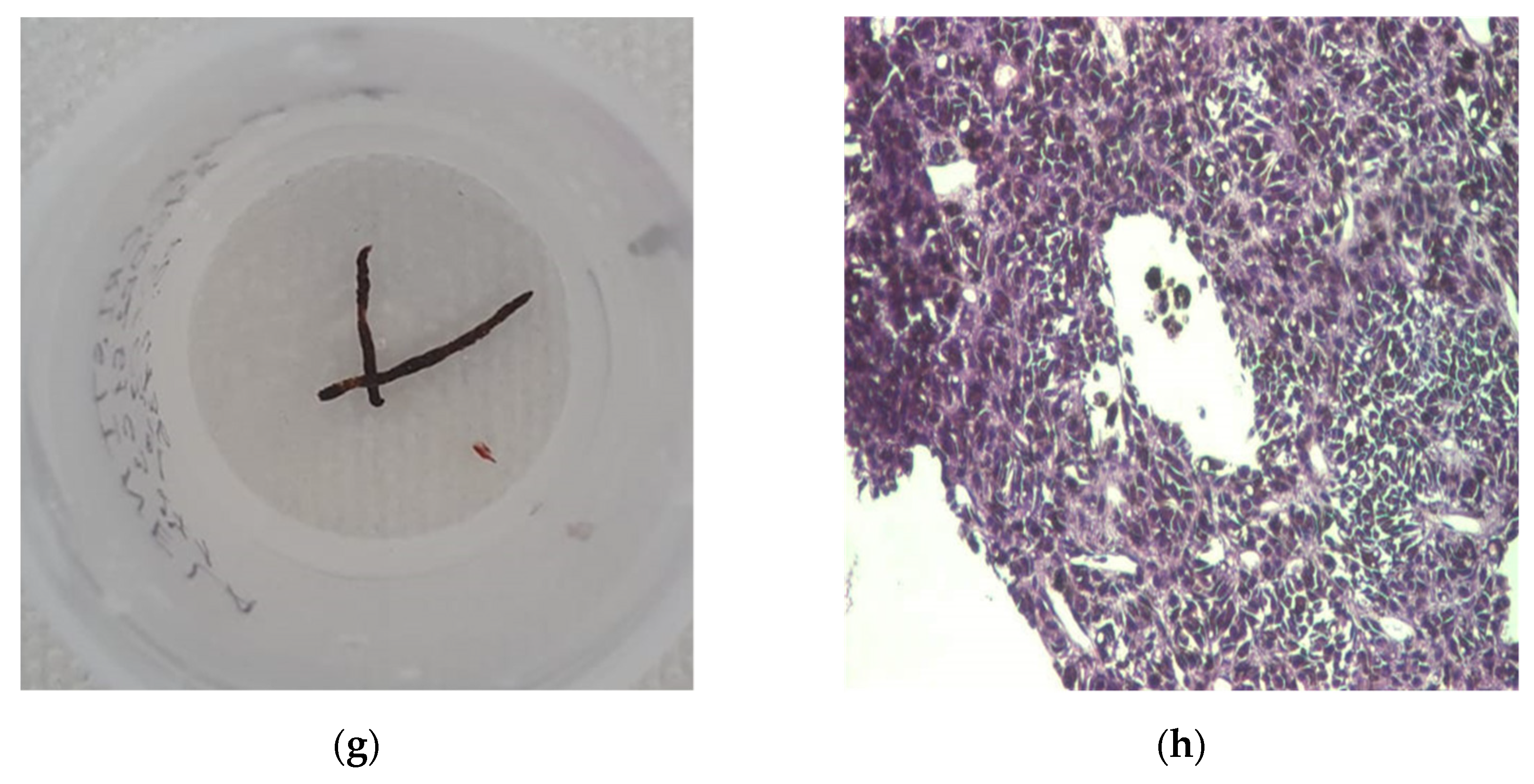
2.2. Histopathological Assessment
2.3. Statistical Analysis
3. Results
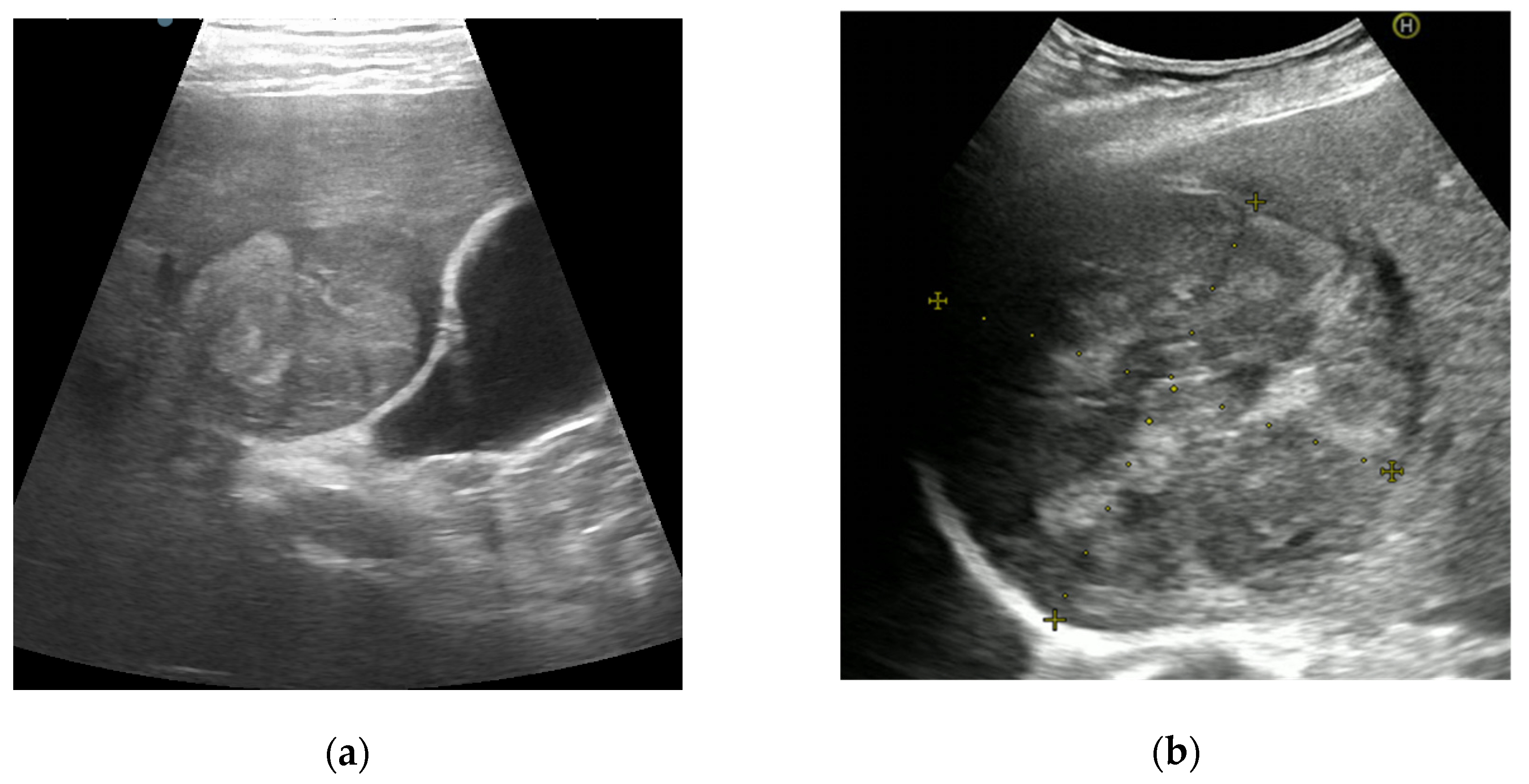
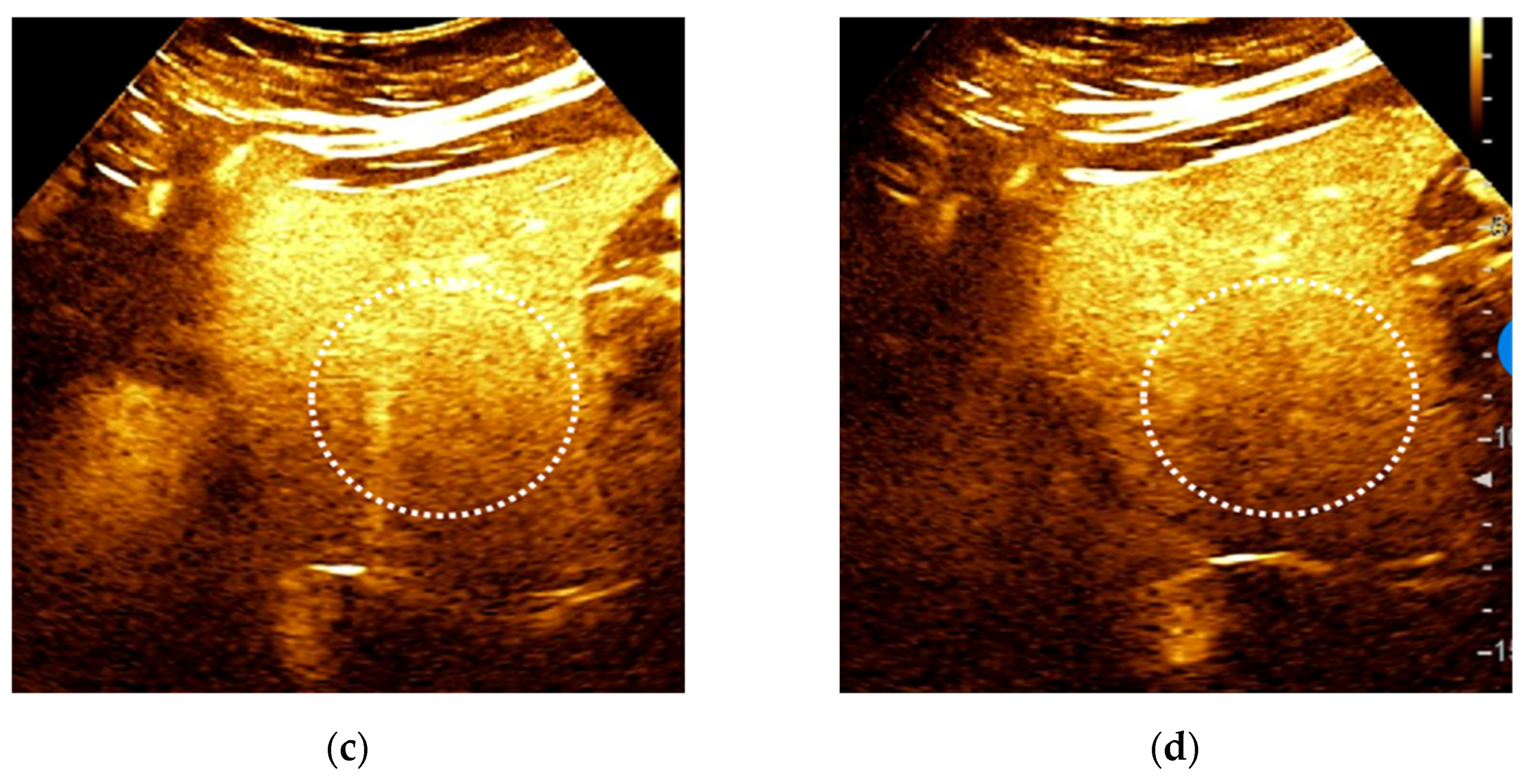
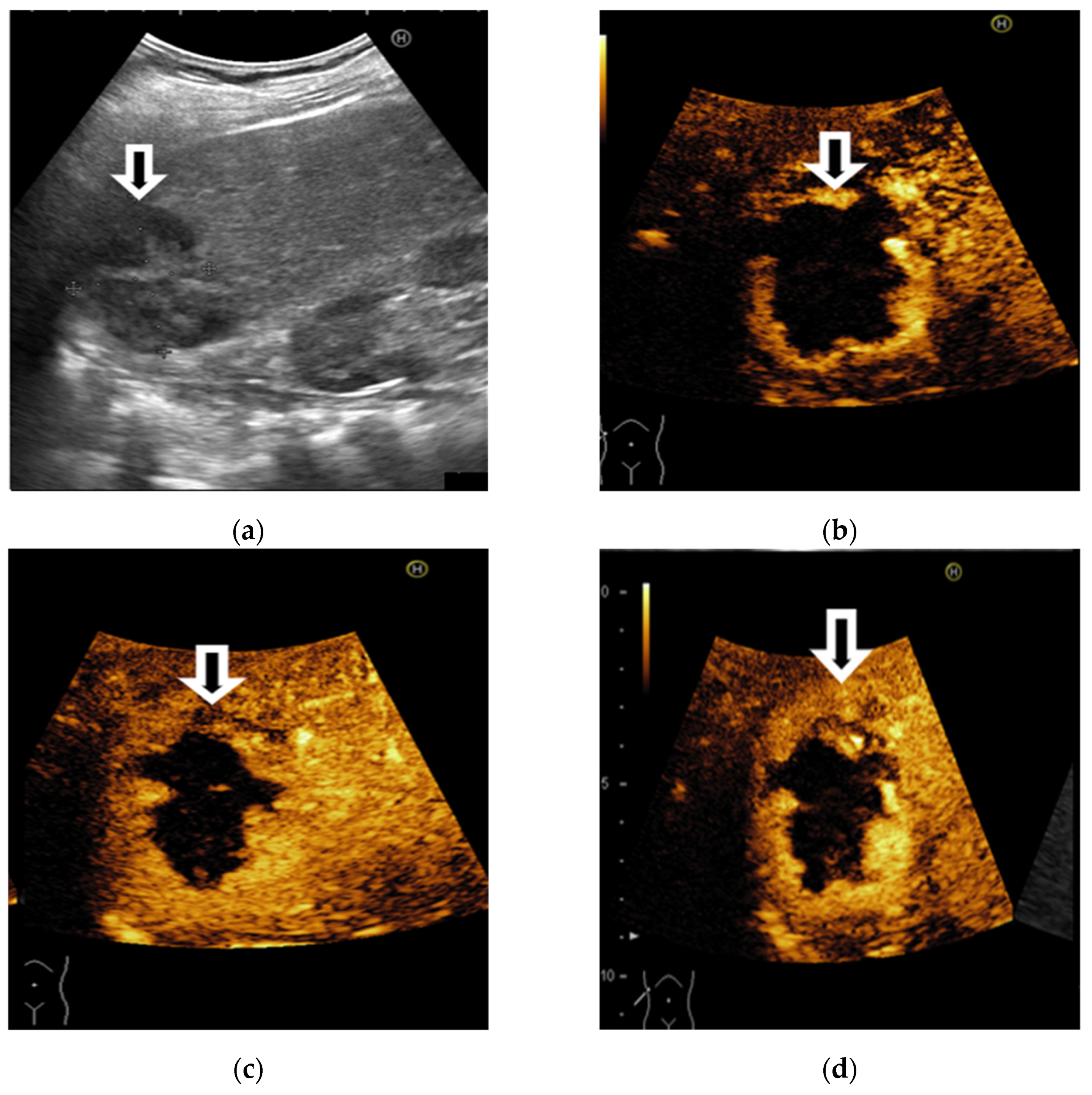
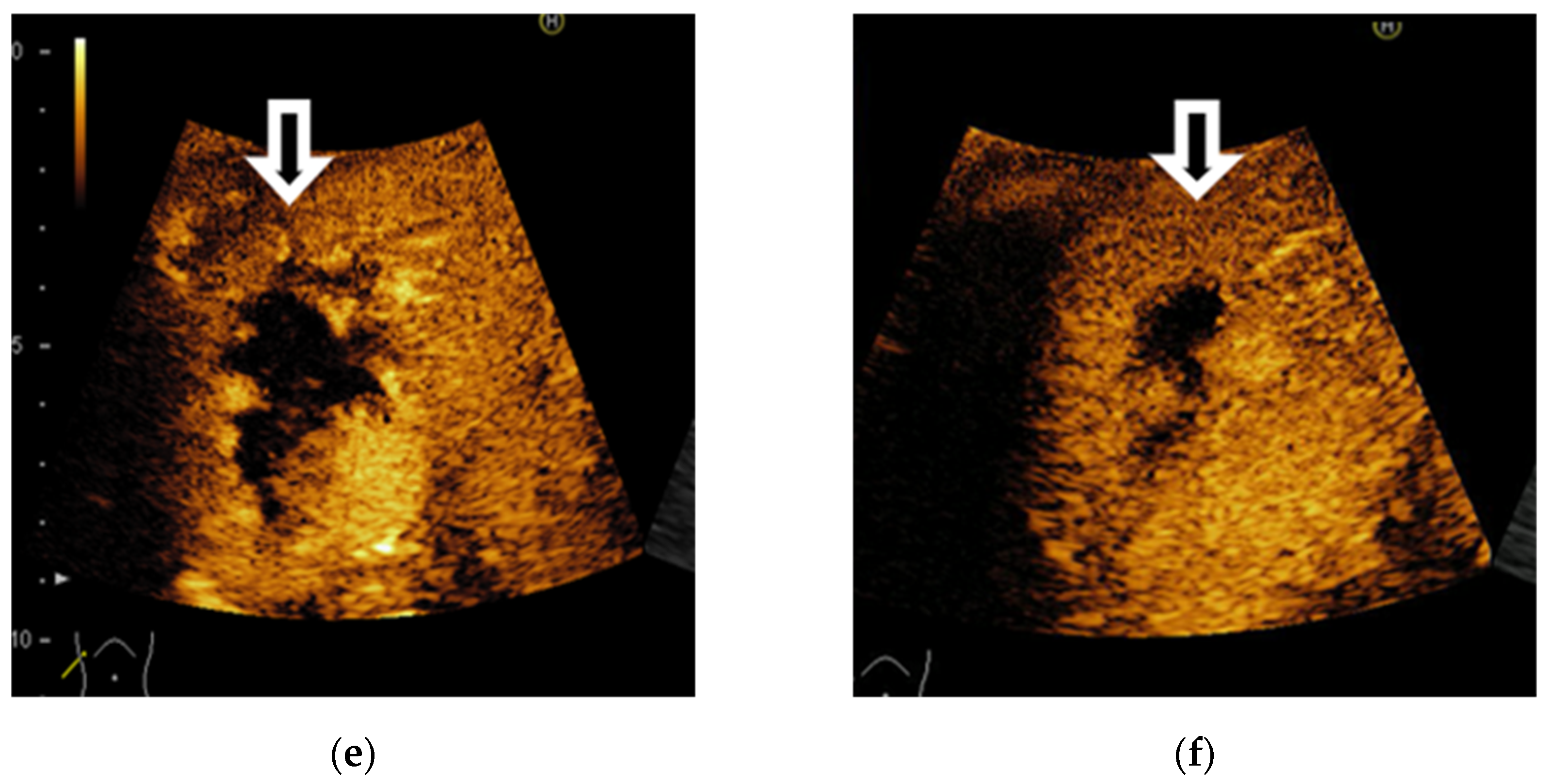
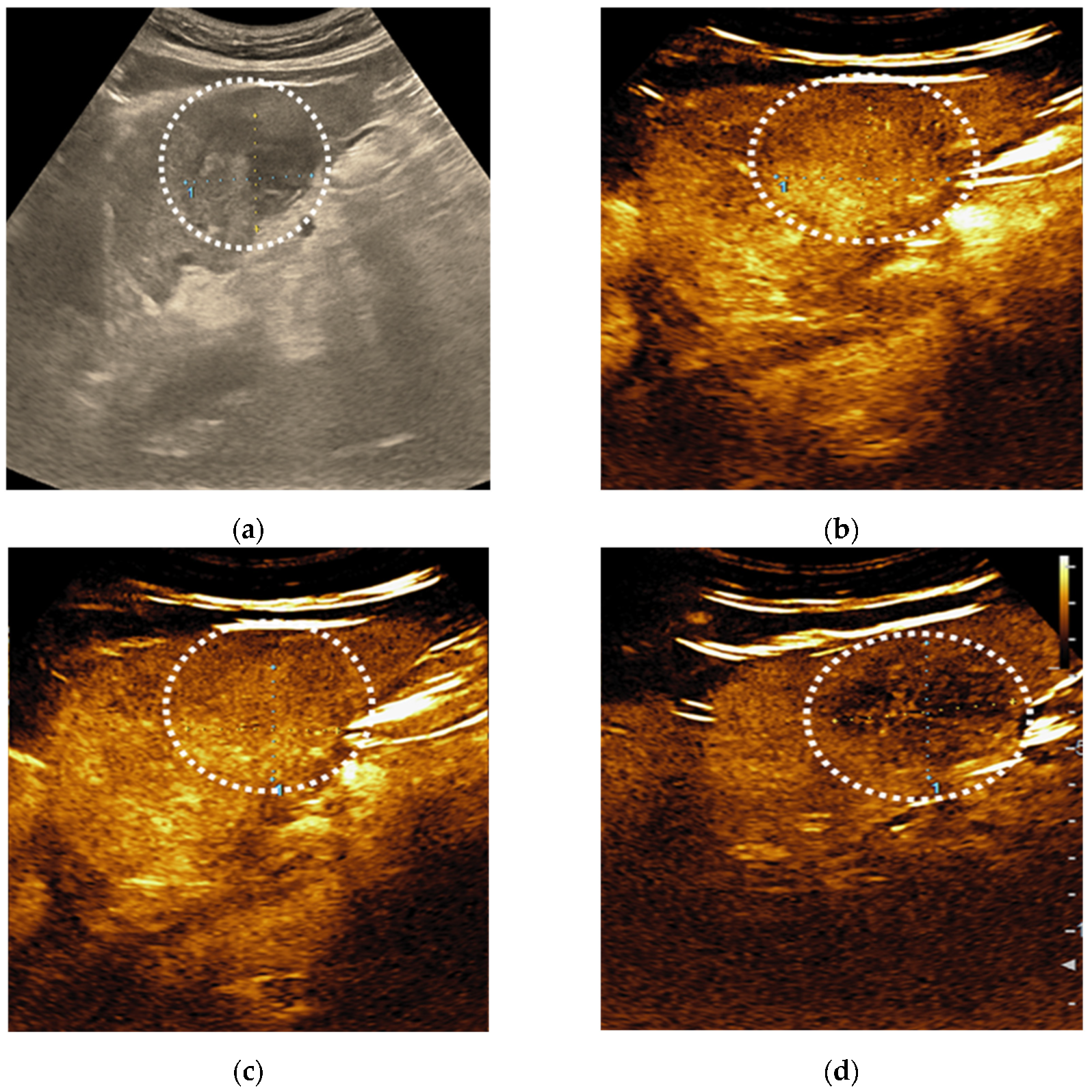
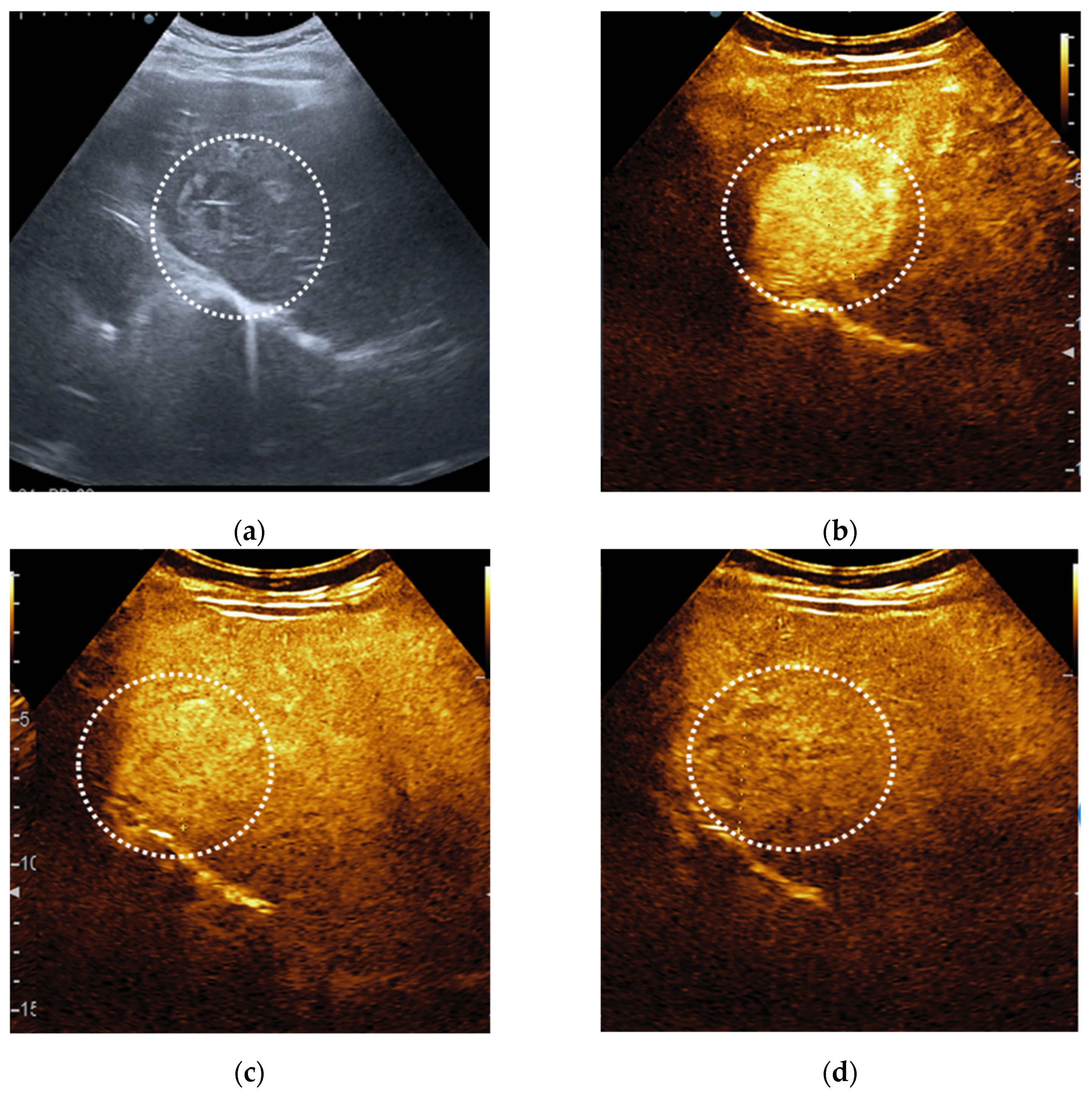
3.1. CEUS
3.1.1. CEUS Patterns According to LI-RADS Recommendations
3.1.2. CEUS Accuracy
3.2. Histopathologic Diagnosis
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Altekruse, S.F.; McGlynn, K.A.; Reichman, M.E. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J. Clin. Oncol. 2009, 27, 1485–1491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forner, A.; Llovet, J.M.; Bruix, J. Hepatocellular carcinoma. Lancet 2012, 379, 1245–1255. [Google Scholar] [CrossRef]
- Galassi, M.; Iavarone, M.; Rossi, S.; Bota, S.; Vavassori, S.; Rosa, L.; Leoni, S.; Venerandi, L.; Marinelli, S.; Sangiovanni, A.; et al. Patterns of appearance and risk of misdiagnosis of intrahepatic cholangiocarcinoma in cirrhosis at contrast enhanced ultrasound. Liver Int. 2013, 33, 771–779. [Google Scholar] [CrossRef]
- Jang, H.J.; Yu, H.; Kim, T.K. Contrast-enhanced ultrasound in the detection and characterization of liver tumors. Cancer Imaging 2009, 9, 96–103. [Google Scholar]
- Xu, J.F.; Liu, H.Y.; Shi, Y.; Wei, Z.H.; Wu, Y. Evaluation of hepatocellular carcinoma by contrast-enhanced sonography: Correlation with pathologic differentiation. J. Ultrasound Med. 2011, 30, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Nolsøe, C.P.; Barr, R.G.; Berzigotti, A.; Burns, P.N.; Cantisani, V.; Chammas, M.C.; Chaubal, N.; Choi, B.I.; Clevert, D.A.; et al. Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the Liver—Update 2020—WFUMB in Cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultraschall Med. 2020, 41, 562–585. [Google Scholar] [CrossRef]
- Salvatore, V.; Gianstefani, A.; Negrini, G.; Allegretti, G.; Galassi, M.; Piscaglia, F. Imaging diagnosis of hepatocellular carcinoma: Recent advances of contrast-enhanced ultrasonography with SonoVue. Liver Cancer 2016, 5, 55–66. [Google Scholar] [CrossRef]
- Cunha, G.M.; Sirlin, C.B.; Fowler, K.J. Imaging diagnosis of hepatocellular carcinoma: LI-RADS. Chin. Clin. Oncol. 2021, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Hu, Y.; Han, J.; Li, Q.; Peng, C.; Zhou, J. Clinical Application of Liver Imaging Reporting and Data System for Characterizing Liver Neoplasms: A Meta-Analysis. Diagnostics 2021, 11, 323. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Dong, Y.; Kono, Y.; Caraiani, C.; Sirlin, C.B.; Cui, X.-W.; Tang, A. LI-RADS ancillary features on contrast-enhanced ultrasonography. Ultrasonography 2020, 39, 221–228. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [Green Version]
- Kono, Y.; Lyshchik, A.; Cosgrove, D.; Dietrich, C.F.; Jang, H.-J.; Kim, T.K.; Piscaglia, F.; Willmann, J.K.; Wilson, S.R.; Santillan, C.; et al. Contrast Enhanced Ultrasound (CEUS) Liver Imaging Reporting and Data System (LI-RADS(R)): The official version by the American College of Radiology (ACR). Ultraschall Med. 2017, 38, 85–86. [Google Scholar] [CrossRef] [Green Version]
- Seitz, K.; Bernatik, T.; Strobel, D.; Blank, W.; Friedrich-Rust, M.; Strunk, H.; Greis, C.; Kratzer, W.; Schuler, A. Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM Multicenter Trial): CEUS vs. MRI—A prospective comparison in 269 patients. Ultraschall Med. 2010, 31, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Popa, P.; Streba, C.T.; Caliţă, M.; Iovănescu, V.F.; Florescu, D.N.; Ungureanu, B.S.; Stănculescu, A.D.; Ciurea, R.N.; Oancea, C.N.; Georgescu, D.; et al. Value of endoscopy with narrow-band imaging and probe-based confocal laser endomicroscopy in the diagnosis of preneoplastic lesions of gastrointestinal tract. Rom. J. Morphol. Embryol. 2020, 61, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Terzi, E.; Iavarone, M.; Pompili, M.; Veronese, L.; Cabibbo, G.; Fraquelli, M.; Riccardi, L.; De Bonis, L.; Sangiovanni, A.; Leoni, S.; et al. Contrast ultrasound LI-RADS LR-5 identifies hepatocellular carcinoma in cirrhosis in a multicenter restropective study of 1006 nodules. J. Hepatol. 2018, 68, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Darnell, A.; Forner, A.; Rimola, J.; Reig, M.; Garcia-Criado, A.; Ayuso, C.; Bruix, J. Liver Imaging Reporting and Data System with MR imaging: Evaluation in nodules 20 mm or smaller detected in cirrhosis at screening US. Radiol. 2015, 275, 698–707. [Google Scholar] [CrossRef]
- Schellhaas, B.; Görtz, R.S.; Pfeifer, L.; Kielisch, C.; Neurath, M.F.; Strobel, D. Diagnostic accuracy of contrast-enhanced ultrasound for the differential diagnosis of hepatocellular carcinoma: ESCULAP versus CEUS-LI-RADS. Eur. J. Gastroenterol. Hepatol. 2017, 29, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Ghiuchici, A.M.; Dănilă, M.; Popescu, A.; Șirli, R.; Moga, T.; Topan, M.; Bende, F.; Sporea, I. Contrast-enhanced ultrasound algorithm (ACR CEUS LI-RADSv 2017)—A valuable tool for the noninvasive diagnosis of hepatocellular carcinoma in patients with chronic liver disease. Med. Ultrason. 2021, 23, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Sporea, I.; Sandulescu, D.L.; Sirli, R.; Popescu, A.; Danilă, M.; Spârchez, Z.; Mihai, C.; Ioanițescu, S.; Moga, T.; Timar, B.; et al. Contrast Enhanced Ultrasound for the characterization of malignant versus benign focal liver lesion in a prospectiv multicenter experience—The SRUMB Study. J. Gastrointest. Liver Dis. 2019, 28, 191–196. [Google Scholar] [CrossRef]
- Kim, T.H.; Kim, S.Y.; Tang, A.; Lee, J.M. Comparison of international guidelines for noninvasive diagnosis of hepatocellular carcinoma: 2018 update. Clin. Mol. Hepatol. 2019, 25, 245–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wildner, D.; Bernatik, T.; Greis, C.; Seitz, K.; Neurath, M.F.; Strobel, D. CEUS in Hepatocellular Carcinoma and Intrahepatic Cholangiocellular Carcinoma in 320 Patients—Early or Late Washout Matters: A Subanalysis of the DEGUM Multicenter Trial. Ultraschall Med. 2015, 36, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Şerbănescu, M.S.; Oancea, C.N.; Streba, C.T.; Pleşea, I.E.; Pirici, D.; Streba, L.; Pleşea, R.M. Agreement of two pre-trained deep-learning neural networks built with transfer learning with six pathologists on 6000 patches of prostate cancer from Gleason2019 Challenge. Rom. J. Morphol. Embryol. 2020, 61, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.X.; Shen, J.X.; Han, J.; Mao, S.Y.; Mao, R.S.; Li, Q.; Li, F.; Guo, Z.X.; Zhou, J.H. Diagnosis of Non-Hepatocellular Carcinoma Malignancies in Patients with Risks for Hepatocellular Carcinoma: CEUS LI-RADS Versus CT/MRI LI-RADS. Front. Oncol. 2021, 11, 641195. [Google Scholar] [CrossRef]
- Turcu-Stiolica, A.; Popescu, M.; Bubulica, M.; Oancea, C.; Nicolicescu, C.; Manda, C.; Neamtu, J.; Croitoru, O. Optimization of Gold Nanoparticles Synthesis using Design of Experiments Technique. Rev. Chim. 2017, 68, 1518–1523. [Google Scholar] [CrossRef]
- Wilson, S.R.; Lyshchik, A.; Piscaglia, F.; Cosgrove, D.; Jang, H.J.; Sirlin, C.; Dietrich, C.F.; Kim, T.K.; Willmann, J.K.; Kono, Y. CEUS LI-RADS: Algorithm, implementation, and key differences from CT/MRI. Abdom. Radiol. 2018, 43, 127–142. [Google Scholar] [CrossRef] [PubMed]
- Yue, W.W.; Wang, S.; Xu, H.X.; Sun, L.-P.; Guo, L.-H.; Bo, X.-W.; Li, X.-L.; Zhao, C.-K.; Wang, D.; Liu, B.-J. Parametric imaging with contrast-enhanced ultrasound for differentiating hepatocellular carcinoma from metastatic liver cancer. Clin. Hemorheol. Microcirc. 2016, 64, 177–188. [Google Scholar] [CrossRef] [PubMed]
- van der Pol, C.B.; Lim, C.S.; Sirlin, C.B.; McGrath, T.A.; Salameh, J.P.; Bashir, M.R.; Tang, A.; Singal, A.G.; Costa, A.F.; Fowler, K.; et al. Accuracy of the Liver Imaging Reporting and Data System in computed tomography and magnetic resonance image analysis of hepatocellular carcinoma or overall malignancy: A systematic review. Gastroenterology 2019, 156, 976–986. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugimoto, K.; Kakegawa, T.; Takahashi, H.; Tomita, Y.; Abe, M.; Yoshimasu, Y.; Takeuchi, H.; Kasai, Y.; Itoi, T. Usefulness of Modified CEUS LI-RADS for the Diagnosis of Hepatocellular Carcinoma Using Sonazoid. Diagnostics 2020, 10, 828. [Google Scholar] [CrossRef]
- Shin, J.; Lee, S.; Kim, Y.Y.; Chung, Y.E.; Choi, J.Y.; Park, M.S. Contrast-enhanced ultrasound Liver Imaging Reporting and Data System category M: A systematic review and meta-analysis. Ultrasonography 2021. published online ahead of print, 19 May 2021. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kim, S.S.; Roh, Y.H.; Choi, J.Y.; Park, M.S.; Kim, M.J. Diagnostic performance of CT/MRI Liver Imaging Reporting and Data System v2017 for hepatocellular carcinoma: A systematic review and meta-analysis. Liver Int. 2020, 40, 1488–1497. [Google Scholar] [CrossRef]
- Ignee, A.; Weiper, D.; Schuessler, G.; Teuber, G.; Faust, D.; Dietrich, C.F. Sonographic characterisation of hepatocellular carcinoma at time of diagnosis. Z. Gastroenterol. 2005, 43, 289–294. [Google Scholar] [CrossRef] [PubMed]







| Patient Characteristics (n = 143) | |
|---|---|
| Variable | n (%) |
| Patient’s gender, male | 97 (67.8%) |
| Patient’s age, median (years) (±SD) | 65.7 ± 8.17 |
| Liver cirrhosis | 129 (90.2%) |
| Etiology of liver disease, n (%) | |
| 29 (20.2%) |
| 5 (3.49%) |
| 55 (38.4) |
| 41 (28.7) |
| 6 (4.1%) |
| 4 (2.7%) |
| History of extrahepatic malignancy | 8 (5.5%) |
| Number of lesions | |
| 111 (77.6%) |
| 27 (18.8%) |
| 3 (2.09%) |
| 2 (1.39%) |
| Ultrasound Features (n = 191) | |
|---|---|
| size of index lesion (n = 191) | (mean ± SD) 41.6 ± 27.1 mm |
| 45 (23.5%) |
| 96 (50.2%) |
| 50 (26.1%) |
| echo texture of index lesion (n = 191) | |
| 77 (40.3%) |
| 20 (10.4%) |
| 94 (49.2%) |
| homogeneity of index lesion (n = 191) | 66 (34.5%) |
| presence of hypoechoic rim | 38 (19.8%) |
| noduleinnodule architecture | 32 (16.7%) |
| mosaic architecture | 34 (17.8%) |
| macroinvasion of liver veins/portal vein (B-mode, color mode) | 26 (13.6%) |
| LI-RADS Classes (n = 191) | ||
|---|---|---|
| The Final Diagnosis | n (%) | LI-RADS Classes |
| Malignant | 159 (83.2%) | |
| HCC | 141 (73.83%) | LR-5 = 81 (57.4%) LR-4 = 37 (26.2%) LR-3 = 3 (2.12%) LR-M = 13 (9.21%) LR-NC = 7 (4.96%) |
| ICC | 4 (2.09%) | LR-M = 3 LR-5 = 1 |
| mixed tumor (HCC/ICC) | 3 (1.57%) | LR-M = 3 |
| metastases | 10 (5.23%) | LR-M = 10 |
| malignant transformation of hepatocellular adenomas | 1 (0.52%) | LR-5 = 1 |
| Benign | 32 (16.7%) | |
| regenerative/dysplastic nodule | 19 (9.9%) | LR-1 = 3 LR-2 = 6 LR-3 = 5 LR-4 = 2 LR-NC = 3 |
| FNH | 1 (0.5%) | LR-2 = 1 |
| hemangioma | 6 (3.1%) | LR-1 = 5 LR-5 = 1 |
| complex cyst | 6 (3.1%) | LR-1 = 6 |
| LI-RADS | Number of Lesions (n = 191) | Diagnosis |
|---|---|---|
| LR-1 | 14 | Complicated cysts = 6 Hemangioma = 5 Regenerative Nodules = 3 |
| LR-2 | 7 | FNH = 1 Regenerative Nodules = 6 |
| LR-3 | 8 | HCC = 3 Regenerative Nodules = 5 |
| LR-4 | 39 | HCC = 37 Regenerative Nodules = 2 |
| LR-5 | 84 | HCC = 81 ICC = 1 Flash-filling hemangioma = 1 Adenoma with malignant transformation = 1 |
| LR-M | 29 | HCC = 13 Mixed tumor = 3 ICC = 3 Metastases = 10 |
| LR-NC | 10 | HCC = 7 Regenerative Nodules = 10 |
| Statistic | Value | 95% CI |
|---|---|---|
| Sensitivity | 60.45% | 51.64–68.78% |
| Specificity | 93.62% | 82.46–98.66% |
| Positive likelihood ratio | 9.47 | 3.14–28.55 |
| Negative likelihood ratio | 0.42 | 0.34–0.53 |
| Disease prevalence | 73.00% | |
| PPV | 96.24% | 89.47–98.72% |
| NPV | 46.68% | 41.21–52.23% |
| Accuracy | 69.40% | 62.13–76.02% |
| Statistic | Value | 95% CI |
|---|---|---|
| Sensitivity | 88.06% | 81.33–93.02% |
| Specificity | 89.36% | 76.90–96.45% |
| Positive likelihood ratio | 8.28 | 3.61–19.00 |
| Negative likelihood ratio | 0.13 | 0.08–0.21 |
| Disease prevalence | 73.00% | |
| PPV | 95.72% | 90.70–98.09% |
| NPV | 73.46% | 63.36–81.58% |
| Accuracy | 88.41% | 82.83–92.68% |
| CEUS LI-RADS | Sensitivity (%) | PPV (%) |
|---|---|---|
| LR-3 | 2.10 | 41.02 |
| LR-4 | 26.20 | 94.87 |
| LR-5 | 60.45 | 96.24 |
| LR 4 + 5 | 88.06 | 95.72 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciocalteu, A.; Iordache, S.; Cazacu, S.M.; Urhut, C.M.; Sandulescu, S.M.; Ciurea, A.-M.; Saftoiu, A.; Sandulescu, L.D. Role of Contrast-Enhanced Ultrasonography in Hepatocellular Carcinoma by Using LI-RADS and Ancillary Features: A Single Tertiary Centre Experience. Diagnostics 2021, 11, 2232. https://doi.org/10.3390/diagnostics11122232
Ciocalteu A, Iordache S, Cazacu SM, Urhut CM, Sandulescu SM, Ciurea A-M, Saftoiu A, Sandulescu LD. Role of Contrast-Enhanced Ultrasonography in Hepatocellular Carcinoma by Using LI-RADS and Ancillary Features: A Single Tertiary Centre Experience. Diagnostics. 2021; 11(12):2232. https://doi.org/10.3390/diagnostics11122232
Chicago/Turabian StyleCiocalteu, Adriana, Sevastita Iordache, Sergiu Marian Cazacu, Cristiana Marinela Urhut, Sarmis Marian Sandulescu, Ana-Maria Ciurea, Adrian Saftoiu, and Larisa Daniela Sandulescu. 2021. "Role of Contrast-Enhanced Ultrasonography in Hepatocellular Carcinoma by Using LI-RADS and Ancillary Features: A Single Tertiary Centre Experience" Diagnostics 11, no. 12: 2232. https://doi.org/10.3390/diagnostics11122232
APA StyleCiocalteu, A., Iordache, S., Cazacu, S. M., Urhut, C. M., Sandulescu, S. M., Ciurea, A.-M., Saftoiu, A., & Sandulescu, L. D. (2021). Role of Contrast-Enhanced Ultrasonography in Hepatocellular Carcinoma by Using LI-RADS and Ancillary Features: A Single Tertiary Centre Experience. Diagnostics, 11(12), 2232. https://doi.org/10.3390/diagnostics11122232







