The Association between Dynamic Changes in Serum Presepsin Levels and Mortality in Immunocompromised Patients with Sepsis: A Prospective Cohort Study
Abstract
:1. Introduction
2. Results
2.1. Baseline Characteristics
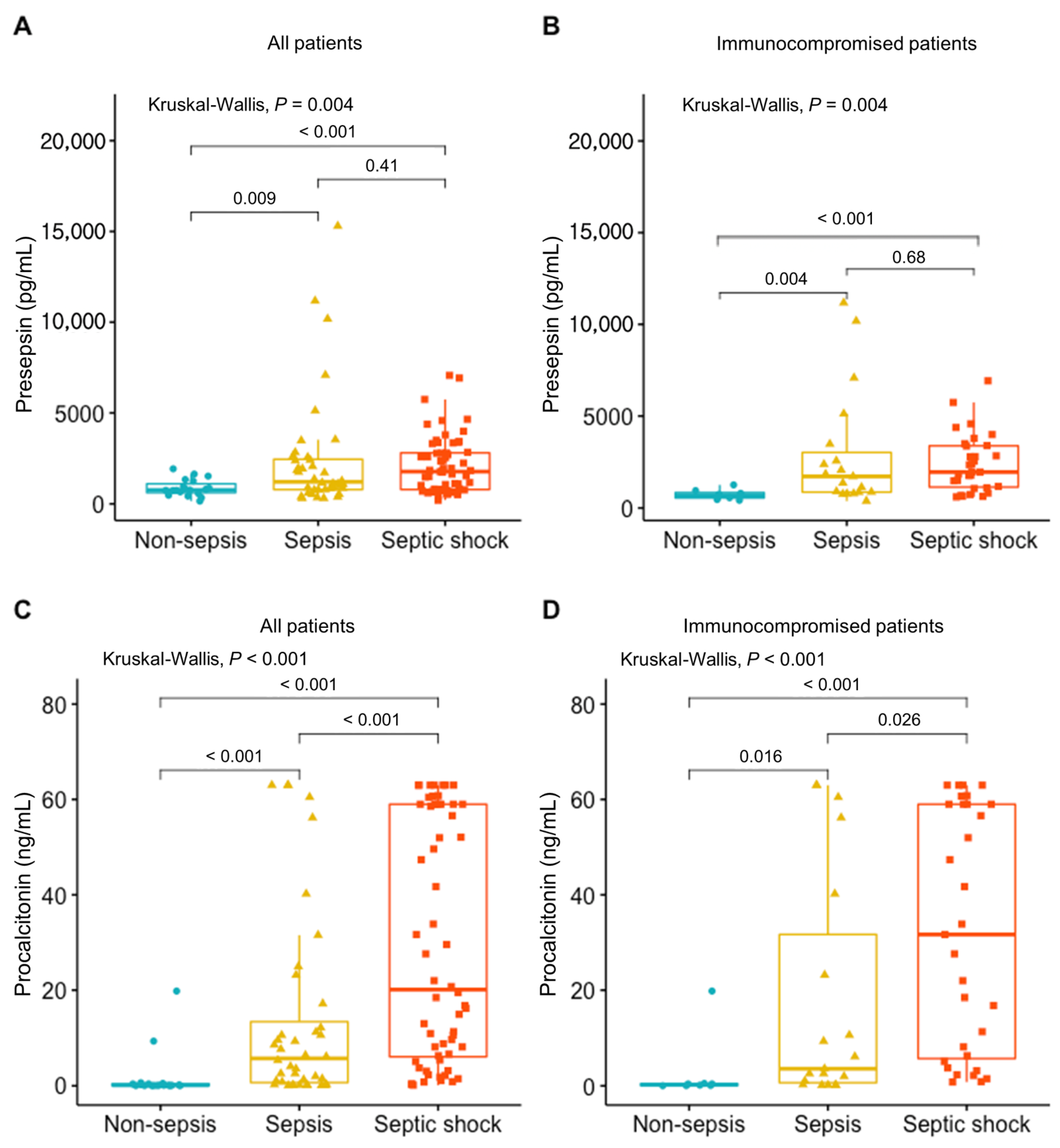
2.2. Presepsin and Procalcitonin Changes in Sepsis Patients
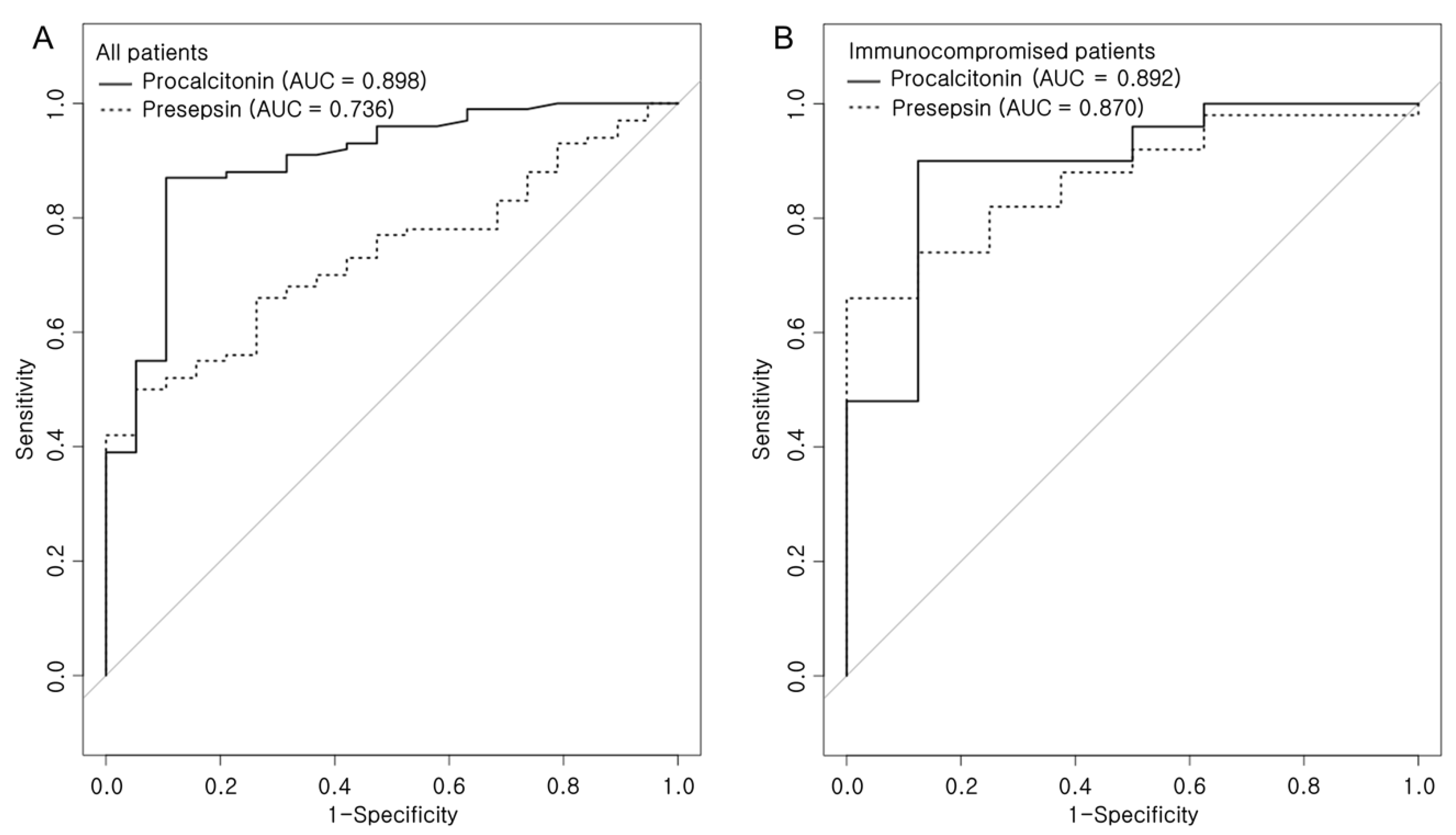
2.3. Correlations of Presepsin and Procalcitonin in Patients with Sepsis
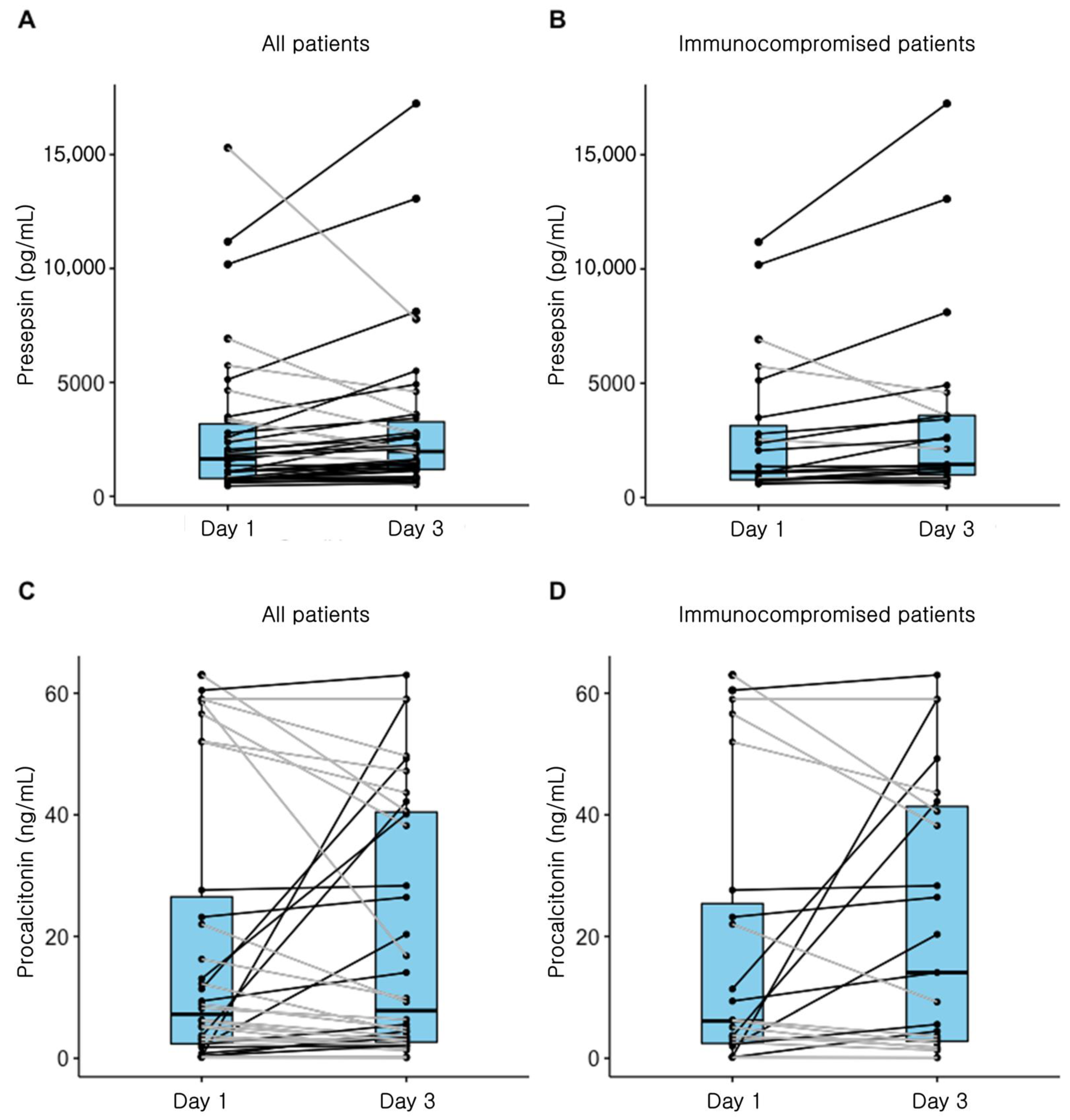
2.4. Presepsin Change and Mortality
2.5. Subgroup Analysis for Non-Survivors
3. Discussion
4. Materials and Methods
4.1. Ethics Approval and Consent to Participate
4.2. Study Population
4.3. Presepsin Assay
4.4. Procalcitonin Assay
4.5. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APACHE | Acute Physiology and Chronic Health Evaluation |
| AUC | Area under curve |
| CI | Confidence interval |
| GPI | Glycosylphosphatidylinositol |
| ICU | Intensive care unit |
| IQR | Interquartile range |
| LPS | lipopolysaccharide |
| OR | Odds ratio |
| ROC | Receiver operating curve |
| SAPS 3 | Simplified Acute Physiology Score 3 |
| SOFA | Sequential Organ Failure Assessment |
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Shozushima, T.; Takahashi, G.; Matsumoto, N.; Kojika, M.; Okamura, Y.; Endo, S. Usefulness of presepsin (sCD14-ST) measurements as a marker for the diagnosis and severity of sepsis that satisfied diagnostic criteria of systemic inflammatory response syndrome. J. Infect. Chemother. 2011, 17, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, T.N.; Viriyakosol, S. Structure-function analysis of soluble and membrane-bound CD14. Prog. Clin. Biol. Res. 1998, 397, 79–87. [Google Scholar] [PubMed]
- Camussi, G.; Mariano, F.; Biancone, L.; De Martino, A.; Bussolati, B.; Montrucchio, G.; Tobias, P.S. Lipopolysaccharide binding protein and CD14 modulate the synthesis of platelet-activating factor by human monocytes and mesangial and endothelial cells stimulated with lipopolysaccharide. J. Immunol. 1995, 155, 316–324. [Google Scholar]
- Chenevier-Gobeaux, C.; Bardet, V.; Poupet, H.; Poyart, C.; Borderie, D.; Claessens, Y.E. Presepsin (sCD14-ST) secretion and kinetics by peripheral blood mononuclear cells and monocytic THP-1 cell line. Ann. Biol. Clin. (Paris) 2016, 74, 93–97. [Google Scholar] [CrossRef]
- Yaegashi, Y.; Shirakawa, K.; Sato, N.; Suzuki, Y.; Kojika, M.; Imai, S.; Takahashi, G.; Miyata, M.; Furusako, S.; Endo, S. Evaluation of a newly identified soluble CD14 subtype as a marker for sepsis. J. Infect. Chemother. 2005, 11, 234–238. [Google Scholar] [CrossRef]
- Kondo, Y.; Umemura, Y.; Hayashida, K.; Hara, Y.; Aihara, M.; Yamakawa, K. Diagnostic value of procalcitonin and presepsin for sepsis in critically ill adult patients: A systematic review and meta-analysis. J. Intensive Care 2019, 7, 22. [Google Scholar] [CrossRef] [Green Version]
- Ali, F.T.; Ali, M.A.; Elnakeeb, M.M.; Bendary, H.N. Presepsin is an early monitoring biomarker for predicting clinical outcome in patients with sepsis. Clin. Chim. Acta 2016, 460, 93–101. [Google Scholar] [CrossRef]
- Behnes, M.; Bertsch, T.; Lepiorz, D.; Lang, S.; Trinkmann, F.; Brueckmann, M.; Borggrefe, M.; Hoffmann, U. Diagnostic and prognostic utility of soluble CD 14 subtype (presepsin) for severe sepsis and septic shock during the first week of intensive care treatment. Crit. Care 2014, 18, 507. [Google Scholar] [CrossRef] [Green Version]
- Endo, S.; Suzuki, Y.; Takahashi, G.; Shozushima, T.; Ishikura, H.; Murai, A.; Nishida, T.; Irie, Y.; Miura, M.; Iguchi, H.; et al. Usefulness of presepsin in the diagnosis of sepsis in a multicenter prospective study. J. Infect. Chemother. 2012, 18, 891–897. [Google Scholar] [CrossRef]
- Endo, S.; Suzuki, Y.; Takahashi, G.; Shozushima, T.; Ishikura, H.; Murai, A.; Nishida, T.; Irie, Y.; Miura, M.; Iguchi, H.; et al. Presepsin as a powerful monitoring tool for the prognosis and treatment of sepsis: A multicenter prospective study. J. Infect. Chemother. 2014, 20, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, G.; Shibata, S.; Ishikura, H.; Miura, M.; Fukui, Y.; Inoue, Y.; Endo, S. Presepsin in the prognosis of infectious diseases and diagnosis of infectious disseminated intravascular coagulation: A prospective, multicentre, observational study. Eur. J. Anaesthesiol. 2015, 32, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Baraka, A.; Zakaria, M. Presepsin as a diagnostic marker of bacterial infections in febrile neutropenic pediatric patients with hematological malignancies. Int. J. Hematol. 2018, 108, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Koizumi, Y.; Shimizu, K.; Shigeta, M.; Okuno, T.; Minamiguchi, H.; Kito, K.; Hodohara, K.; Yamagishi, Y.; Andoh, A.; Fujiyama, Y.; et al. Plasma presepsin level is an early diagnostic marker of severe febrile neutropenia in hematologic malignancy patients. BMC Infect. Dis. 2017, 17, 27. [Google Scholar] [CrossRef] [Green Version]
- Tsuji, S.; Kitatoube, A.; Kikuchi-Taura, A.; Oguro, E.; Shigesaka, M.; Okita, Y.; Shimizu, T.; Nii, T.; Teshigawara, S.; Tanaka, E.; et al. Elevated soluble CD14-subtype (PRESEPSIN; P-SEP) levels in rheumatoid arthritis (RA) patients with bacterial infection. Mod. Rheumatol. 2017, 27, 718–720. [Google Scholar] [CrossRef]
- Clec’h, C.; Ferriere, F.; Karoubi, P.; Fosse, J.P.; Cupa, M.; Hoang, P.; Cohen, Y. Diagnostic and prognostic value of procalcitonin in patients with septic shock. Crit. Care Med. 2004, 32, 1166–1169. [Google Scholar] [CrossRef]
- Pettila, V.; Hynninen, M.; Takkunen, O.; Kuusela, P.; Valtonen, M. Predictive value of procalcitonin and interleukin 6 in critically ill patients with suspected sepsis. Intensive Care Med. 2002, 28, 1220–1225. [Google Scholar] [CrossRef]
- Gibot, S.; Cravoisy, A.; Kolopp-Sarda, M.N.; Bene, M.C.; Faure, G.; Bollaert, P.E.; Levy, B. Time-course of sTREM (soluble triggering receptor expressed on myeloid cells)-1, procalcitonin, and C-reactive protein plasma concentrations during sepsis. Crit. Care Med. 2005, 33, 792–796. [Google Scholar] [CrossRef]
- Vijayan, A.L.; Ravindran, S.; Saikant, R.; Lakshmi, S.; Kartik, R. Procalcitonin: A promising diagnostic marker for sepsis and antibiotic therapy. J. Intensive Care 2017, 5, 51. [Google Scholar] [CrossRef]
- Zou, Q.; Wen, W.; Zhang, X.C. Presepsin as a novel sepsis biomarker. World J. Emerg. Med. 2014, 5, 16–19. [Google Scholar] [CrossRef] [Green Version]
- Shirakawa, K.; Naitou, K.; Hirose, J.; Nakamura, M.; Takeuchi, T.; Hosaka, Y.; Furusako, S. The new sepsis marker, sCD14-ST, induction mechanism in the rabbit sepsis models. Crit. Care 2010, 14 (Suppl. 2), P19. [Google Scholar] [CrossRef] [Green Version]
- Bele, N.; Darmon, M.; Coquet, I.; Feugeas, J.P.; Legriel, S.; Adaoui, N.; Schlemmer, B.; Azoulay, E. Diagnostic accuracy of procalcitonin in critically ill immunocompromised patients. BMC Infect. Dis. 2011, 11, 224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- De Long, E.R.; De Long, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
| Total (n = 119) | Immunocompetent (n = 61) | Immunocompromised (n = 58) | p Value | |
|---|---|---|---|---|
| Age, years | 70.0 (58.0–79.5) | 77.0 (68.0–83.0) | 61.5 (51.0–70.0) | <0.001 |
| Sex, male | 62 (52.1) | 34 (55.7) | 28 (48.3) | 0.528 |
| Sepsis severity | ||||
| No sepsis | 19 (16.0) | 11 (18) | 8 (13.8) | 0.754 |
| Sepsis | 40 (33.6) | 21 (34.4) | 19 (32.8) | |
| Septic shock | 60 (50.4) | 29 (47.5) | 31 (53.4) | |
| SOFA score | 9.0 (6.5–11.5) | 8.2 ± 4.1 | 9.9 ± 3.9 | 0.019 |
| SAPS3 score | 75.5 ± 14.9 | 71.7 ± 15.2 | 79.5 ± 13.5 | 0.004 |
| Lactic acid | 2.5 (1.3–4.8) | 2.2 (1.3–4.1) | 3.0 (1.5–7.5) | 0.169 |
| Presepsin | 1254.0 (730.5–2569.5) | 1065.0 (670.0–1935.0) | 1734.5 (789.0–2831.0) | 0.024 |
| Procalcitonin | 8.2 (0.6–32.8) | 8.2 (0.3–19.5) | 8.8 (0.9–56.2) | 0.213 |
| Charlson comorbidity index | 5.0 (4.0–7.0) | 5.0 (4.0–7.0) | 5.0 (3.0–7.0) | 0.509 |
| Invasive ventilation on Day 1 | 53 (44.5) | 27 (44.3) | 26 (44.8) | 1.000 |
| Vasopressor on Day 1 | 77 (64.7) | 38 (62.3) | 39 (67.2) | 0.710 |
| Hospital mortality, (%) | 53 (44.5) | 19 (31.1) | 34 (58.6) | 0.005 |
| Variable | Cutoff | AUC | Sensitivity | Specificity | + PV | − PV | p Value |
|---|---|---|---|---|---|---|---|
| In all patients | |||||||
| Presepsin | 1632 | 0.736 | 50.0 | 94.7 | 96.2 | 25.4 | <0.001 |
| Procalcitonin | 0.64 | 0.898 | 87.0 | 89.5 | 96.7 | 55.2 | <0.001 |
| In immunocompromised patients | |||||||
| Presepsin | 1248 | 0.870 | 66.0 | 100 | 100 | 32.0 | <0.001 |
| Procalcitonin | 0.5 | 0.892 | 90.0 | 87.5 | 97.8 | 58.3 | <0.001 |
| Survived Patient (n = 50) | Died Patient (n = 38) | p Value | |
|---|---|---|---|
| Sex, male | 29 (58.0) | 18 (47.4) | 0.439 |
| Age, yrs | 71.0 (61.0–79.0) | 69.5 (54.0–83.0) | 0.879 |
| Immunocompromised patients | 18 (36.0) | 23 (60.5) | 0.039 |
| Charlson comorbidity index | 6.0 (4.0–8.0) | 5.0 (4.0–7.0) | 0.589 |
| SAPS3 score | 72.2 ± 11.6 | 83.6 ± 12.9 | <0.001 |
| SOFA score | 8.0 (7.0–11.0) | 11.0 (8.0–13.0) | 0.002 |
| Use of vasopressor on Day 1 | 35 (70.0) | 29 (76.3) | 0.676 |
| Use of invasive ventilation on Day 1 | 15 (30.0) | 21 (55.3) | 0.030 |
| Systolic BP at ICU admission | 79.0 (70.0–89.0) | 82.0 (71.0–90.0) | 0.787 |
| Diastolic BP at ICU admission | 47.5 (41.0–55.0) | 50.0 (41.0–56.0) | 0.385 |
| Heart rate at ICU admission | 124.2 ± 25.8 | 138.6 ± 28.2 | 0.014 |
| Respiratory rate at ICU admission | 28.0 (23.0–34.0) | 31.5 (26.0–38.0) | 0.076 |
| Leukocyte count, Day 1 | 8.9 (4.3–17.3) | 10.0 (3.0–16.5) | 0.768 |
| Neutrophil count, Day 1 | 7.1 (3.3–15.2) | 8.6 (2.8–14.1) | 0.714 |
| Platelet count, Day 1 | 156.5 (52.0–235.0) | 64.0 (34.0–143.0) | 0.006 |
| Lactate, Day 1 | 2.4 (1.3–3.9) | 3.4 (1.9–7.1) | 0.078 |
| Lactate, Day 3 | 1.4 (1.0–2.2) | 2.6 (1.6–5.8) | <0.001 |
| Procalcitonin, Day 1 | 10.6 (1.5–49.6) | 7.2 (2.3–27.6) | 0.383 |
| Procalcitonin, Day 3 | 3.5 (0.7–13.8) | 7.8 (2.5–40.6) | 0.022 |
| ΔProcalcitonin+ | 4 (8.0) | 14 (36.8) | 0.002 |
| Presepsin, Day 1 | 1209.0 (623.0–2559.0) | 1643.0 (777.0–3310.0) | 0.135 |
| Presepsin, Day 3 | 933.0 (638.0–1571.0) | 1965.0 (1149.0–3423.0) | 0.001 |
| ΔPresepsin+ | 16 (32.0) | 28 (73.7) | <0.001 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| SAPS3 score | 1.04 (0.98–1.09) | 0.212 | ||
| SOFA score | 1.08 (0.87–1.34) | 0.480 | ||
| Systolic BP at ICU admission | 1.04 (0.99–1.10) | 0.092 | ||
| Diastolic BP at ICU admission | 1.05 (0.99–1.12) | 0.076 | ||
| Heart rate at ICU admission | 1.01 (0.98–1.03) | 0.510 | ||
| Respiratory rate at ICU admission | 1.01 (0.92–1.11) | 0.800 | ||
| Procalcitonin, Day 1 | 0.98 (0.96–1.01) | 0.140 | ||
| Procalcitonin, Day 3 | 1.02 (0.98–1.05) | 0.331 | ||
| ΔProcalcitonin+ | 6.15 (1.14–33.20) | 0.035 | 5.45 (0.72–41.17) | 0.100 |
| Presepsin, Day 1 | 1.00 (1.00–1.00) | 0.661 | ||
| Presepsin, Day 3 | 1.00 (1.00–1.00) | 0.313 | ||
| ΔPresepsin+ | 7.20 (1.79–29.01) | 0.006 | 6.22 (1.33–29.06) | 0.020 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Kim, S.; Kim, K.H.; Jeong, N.R.; Kim, S.C.; Oh, E.-J. The Association between Dynamic Changes in Serum Presepsin Levels and Mortality in Immunocompromised Patients with Sepsis: A Prospective Cohort Study. Diagnostics 2021, 11, 60. https://doi.org/10.3390/diagnostics11010060
Lee J, Kim S, Kim KH, Jeong NR, Kim SC, Oh E-J. The Association between Dynamic Changes in Serum Presepsin Levels and Mortality in Immunocompromised Patients with Sepsis: A Prospective Cohort Study. Diagnostics. 2021; 11(1):60. https://doi.org/10.3390/diagnostics11010060
Chicago/Turabian StyleLee, Jongmin, Seohyun Kim, Kyung Hoon Kim, Na Ri Jeong, Seok Chan Kim, and Eun-Jee Oh. 2021. "The Association between Dynamic Changes in Serum Presepsin Levels and Mortality in Immunocompromised Patients with Sepsis: A Prospective Cohort Study" Diagnostics 11, no. 1: 60. https://doi.org/10.3390/diagnostics11010060
APA StyleLee, J., Kim, S., Kim, K. H., Jeong, N. R., Kim, S. C., & Oh, E.-J. (2021). The Association between Dynamic Changes in Serum Presepsin Levels and Mortality in Immunocompromised Patients with Sepsis: A Prospective Cohort Study. Diagnostics, 11(1), 60. https://doi.org/10.3390/diagnostics11010060






