The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cadaveric Study Sample
2.2. Measurement of Radial Nerve
2.3. Analysis of Radial Nerve Branches
3. Results
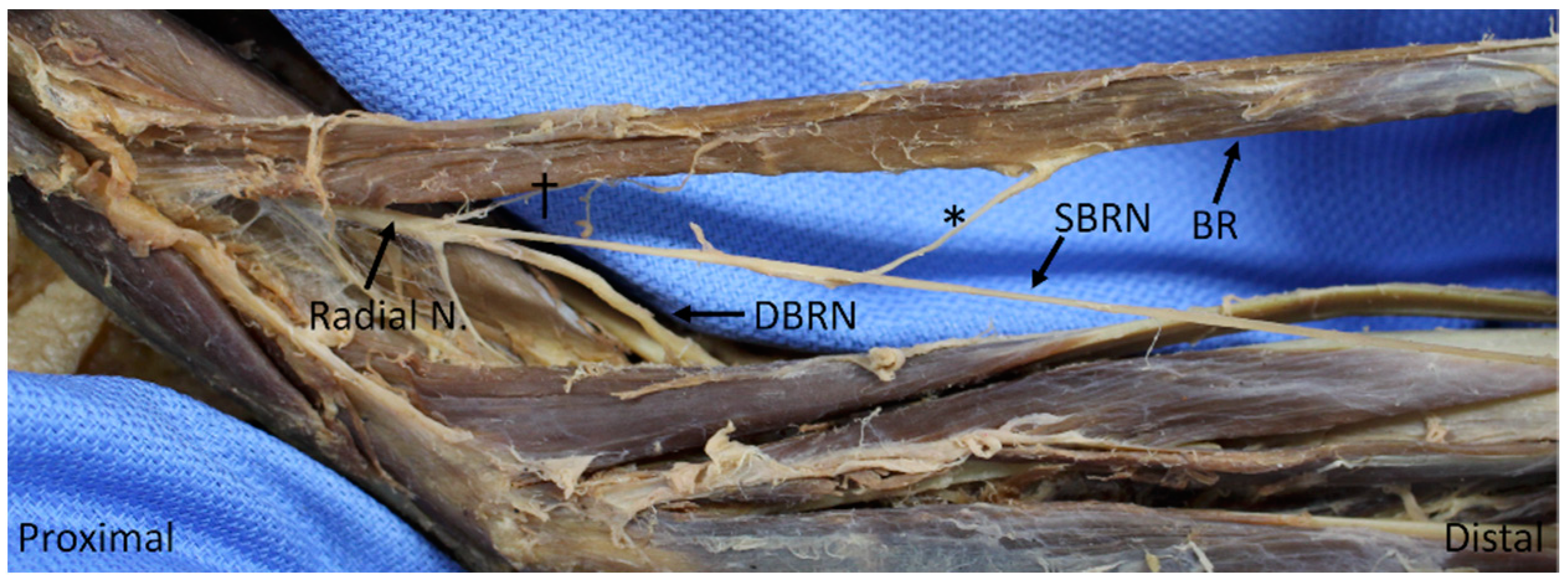
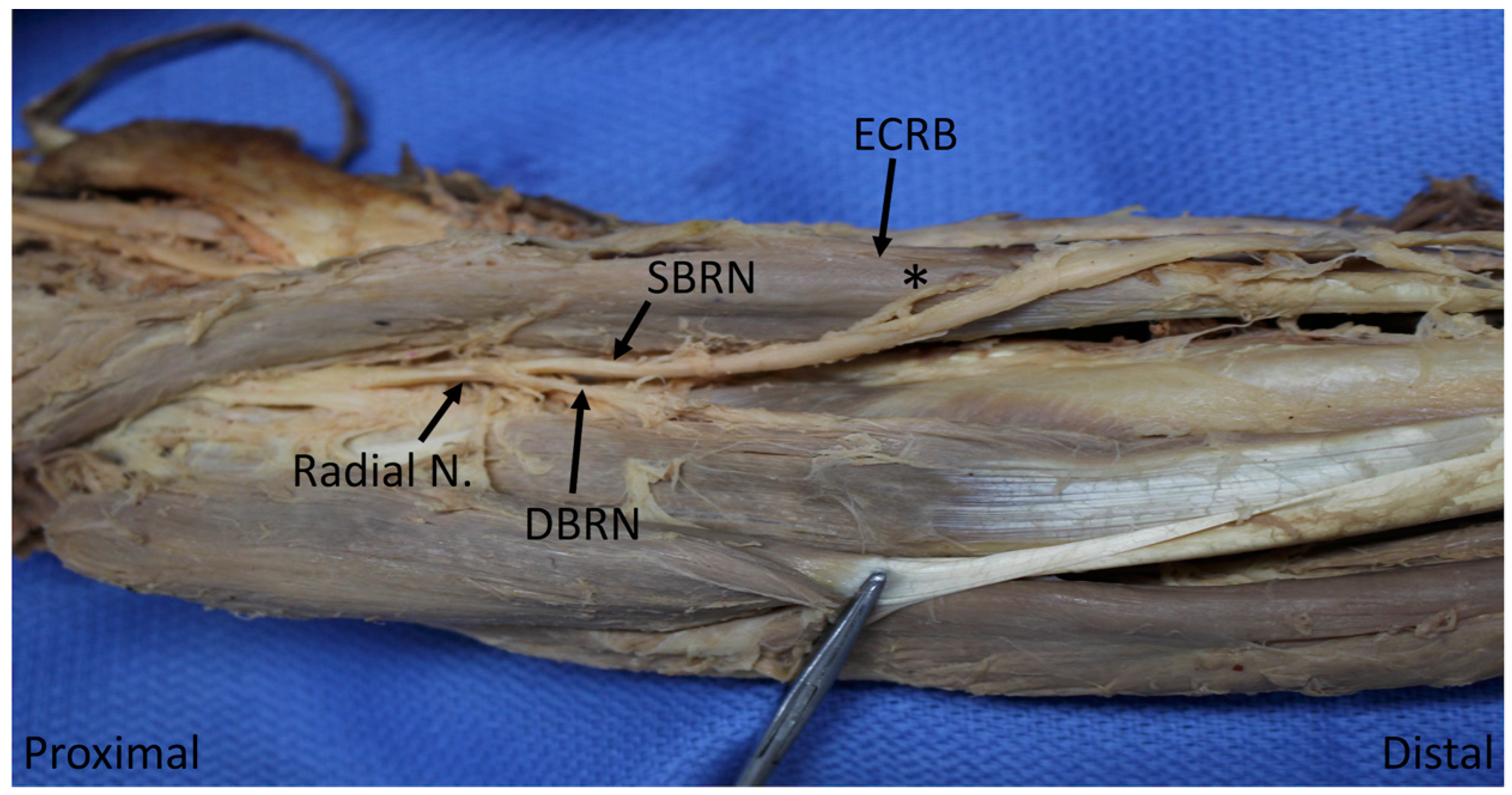
3.1. Branching Order of the Radial Nerve in the Forearm
3.2. Motor Entry Point Order
3.3. Motor Innervation Territories
3.4. Landmarks
4. Discussion
4.1. Branching and Motor Entry Point Orders
4.2. Innervation of Brachialis by Radial Nerve
4.3. Muscular Innervation by Superficial Branch of Radial Nerve
4.4. Inconsistency of Nomenclature and Territories
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sunderland, S. Metrical and non-metrical features of the muscular branches of the radial nerve. J. Comp. Neurol. 1946, 85, 93–111. [Google Scholar] [CrossRef] [PubMed]
- Mazurek, M.T.; Shin, A.Y. Upper extremity peripheral nerve anatomy: Current concepts and applications. Clin. Orthop. Relat. Res. 2001, 383, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Dang, A.C.; Rodner, C.M. Unusual Compression Neuropathies of the Forearm, Part I: Radial Nerve. J. Hand Surg. 2009, 34, 1906–1914. [Google Scholar] [CrossRef] [PubMed]
- Abrams, R.A.; Ziets, R.J.; Lieber, R.L.; Botte, M.J. Anatomy of the radial nerve motor branches in the forearm. J. Hand Surg. 1997, 22, 232–237. [Google Scholar] [CrossRef]
- Branovacki, G.; Hanson, M.; Cash, R.; Gonzalez, M. The innervation pattern of the radial nerve at the elbow and in the forearm. J. Hand Surg. 1998, 23, 167–169. [Google Scholar] [CrossRef]
- Linell, E.A. The Distribution of Nerves in the Upper Limb, with reference to Variabilities and their Clinical Significance. J. Anat. 1921, 55, 79–112. [Google Scholar] [PubMed]
- Blackburn, S.C.; Wood, C.P.J.; Evans, D.J.R.; Watt, D.J. Radial nerve contribution to brachialis in the UK Caucasian population: Position is predictable based on surface landmarks. Clin. Anat. 2007, 20, 64–67. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Lee, H.-Y.; Gil, Y.-C.; Choi, Y.-R.; Yang, H.-J. Topographical anatomy of the radial nerve and its muscular branches related to surface landmarks. Clin. Anat. 2013, 26, 862–869. [Google Scholar] [CrossRef] [PubMed]
- Moore, K.L.; Dalley, A.F.; Agur, A.M.R. Clinically Oriented Anatomy, 7th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013; p. 764. [Google Scholar]
- Abrams, R.A.; Brown, R.A.; Botte, M.J. The superficial branch of the radial nerve: An anatomic study with surgical implications. J. Hand Surg. 1992, 17, 1037–1041. [Google Scholar] [CrossRef]
- Mahakkanukrauh, P.; Somsarp, V. Dual innervation of the brachialis muscle. Clin. Anat. 2002, 15, 206–209. [Google Scholar] [CrossRef]
- Ip, M.C.; Chang, K.S.F. A study on the radial supply of the human brachialis muscle. Anat. Rec. 1968, 162, 363–371. [Google Scholar] [CrossRef]
- Netter, F.H. Atlas of Human Anatomy, 6th ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Moore, K.L.; Agur, A.M.R.; Dalley, A.F. Essential Clinical Anatomy, 5th ed.; Wolters Kluwer Health: Waltham, MA, USA, 2014. [Google Scholar]
- Agur, A.M.R.; Dalley, A.F. Grant’s Atlas of Anatomy, 13th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2009. [Google Scholar]
- Drake, R.; Vogl, A.W.; Mitchell, A.W.M. Gray’s Anatomy for Students, 3rd ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Gilroy, A.M.; MacPherson, B.R.; Ross, L.M. Atlas of Anatomy, 2nd ed.; Thieme: New York, NY, USA, 2012. [Google Scholar]
- Folberg, C.R.; Ulson, H.; Scheidt, R.B. The superficial branch of the radial nerve: A morphologic study. Rev. Bras. De Ortop. 2009, 44, 69–74. [Google Scholar] [CrossRef]
- Haugen, T.W.; Cannady, S.B.; Chalian, A.A.; Shanti, R.M. Anatomical Variations of the Superficial Radial Nerve Encountered during Radial Forearm Free Flap Elevation. ORL J. Otorhinolaryngol. Relat. Spec. 2019, 81, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Dellon, A.L.; Mackinnon, S.E. Susceptibility of the Superficial Sensory Branch of the Radial Nerve to Form Painful Neuromas. J. Hand Surg. 1984, 9, 42–45. [Google Scholar] [CrossRef]
- Federative Committee on Anatomical Terminology. Terminologia Anatomica: International Anatomical Terminology; Thieme: Stuttgart, Germany, 1998. [Google Scholar]
- Stonner, M.M.; Mackinnon, S.E.; Kaskutas, V. Predictors of Disability and Quality of Life With an Upper-Extremity Peripheral Nerve Disorder. Am. J. Occup. 2017, 71, 7101190050p1–7101190050p8. [Google Scholar] [CrossRef] [PubMed]
| Muscle | N | Mean | Standard Deviation | p (To Next Muscle) |
|---|---|---|---|---|
| Brachialis | 21 | −66.41 | 19.63 | <0.0001 * |
| Brachioradialis | 35 | −40.37 | 12.08 | 0.0036 * |
| Extensor carpi radialis longus | 35 | −26.02 | 10.53 | <0.0001 * |
| Extensor carpi radialis brevis | 35 | 17.88 | 18.29 | 0.9553 |
| Supinator | 35 | 22.78 | 11.56 | <0.0001 * |
| Extensor digitorum | 35 | 81.90 | 12.03 | 0.9996 |
| Extensor carpi ulnaris | 35 | 84.60 | 10.60 | 0.1337 |
| Abductor pollicis longus | 35 | 94.92 | 15.26 | 1.0 |
| Extensor digiti minimi | 35 | 94.99 | 15.99 | <0.0001 * |
| Extensor pollicis brevis | 35 | 112.44 | 21.28 | 0.0271 * |
| Extensor pollicis longus | 35 | 124.75 | 16.48 | 1.0 |
| Extensor indicis | 35 | 126.84 | 16.66 | Not Applicable |
| Muscle | N | Mean | Standard Deviation | p (To Next Muscle) |
|---|---|---|---|---|
| Brachialis | 21 | −52.22 | 23.19 | <0.0001 * |
| Brachioradialis | 35 | −20.22 | 17.11 | <0.0001 * |
| Extensor carpi radialis longus | 35 | 5.10 | 10.04 | <0.0001 * |
| Supinator | 35 | 47.67 | 8.42 | 0.4593 |
| Extensor carpi radialis brevis | 35 | 57.13 | 19.60 | <0.0001 * |
| Extensor digitorum | 35 | 94.24 | 13.68 | 0.9896 |
| Extensor carpi ulnaris | 35 | 99.08 | 13.28 | 0.0017 * |
| Extensor digiti minimi | 35 | 116.33 | 17.39 | 0.8526 |
| Abductor pollicis longus | 35 | 123.38 | 13.15 | <0.0001 * |
| Extensor pollicis longus | 35 | 147.56 | 21.91 | 0.5003 |
| Extensor pollicis brevis | 35 | 154.22 | 22.24 | 0.0062 * |
| Extensor indicis | 35 | 163.47 | 20.40 | Not Applicable |
| Muscle | Radial Nerve | Superficial Branch of the Radial Nerve | Deep Branch of the Radial Nerve | Posterior Interosseous Nerve |
|---|---|---|---|---|
| Brachialis | 60 | |||
| Brachioradialis | 100 | 2.86 | ||
| Extensor carpi radialis longus | 100 | |||
| Extensor carpi radialis brevis | 28.57 | 25.71 | 48.57 | |
| Supinator | 11.43 | 88.57 | ||
| Extensor digitorum | 14.29 | 88.57 | ||
| Extensor carpi ulnaris | 17.14 | 82.86 | ||
| Extensor digiti minimi | 2.86 | 97.14 | ||
| Abductor pollicis longus | 8.57 | 91.43 | ||
| Extensor pollicis brevis | 2.86 | 97.14 | ||
| Extensor pollicis longus | 100 | |||
| Extensor indicis | 100 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sawyer, F.K.; Stefanik, J.J.; Lufler, R.S. The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications. Diagnostics 2020, 10, 366. https://doi.org/10.3390/diagnostics10060366
Sawyer FK, Stefanik JJ, Lufler RS. The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications. Diagnostics. 2020; 10(6):366. https://doi.org/10.3390/diagnostics10060366
Chicago/Turabian StyleSawyer, F. Kip, Joshua J. Stefanik, and Rebecca S. Lufler. 2020. "The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications" Diagnostics 10, no. 6: 366. https://doi.org/10.3390/diagnostics10060366
APA StyleSawyer, F. K., Stefanik, J. J., & Lufler, R. S. (2020). The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications. Diagnostics, 10(6), 366. https://doi.org/10.3390/diagnostics10060366





