Serum and Echocardiographic Markers May Synergistically Predict Adverse Cardiac Remodeling after ST-Segment Elevation Myocardial Infarction in Patients with Preserved Ejection Fraction
Abstract
1. Introduction
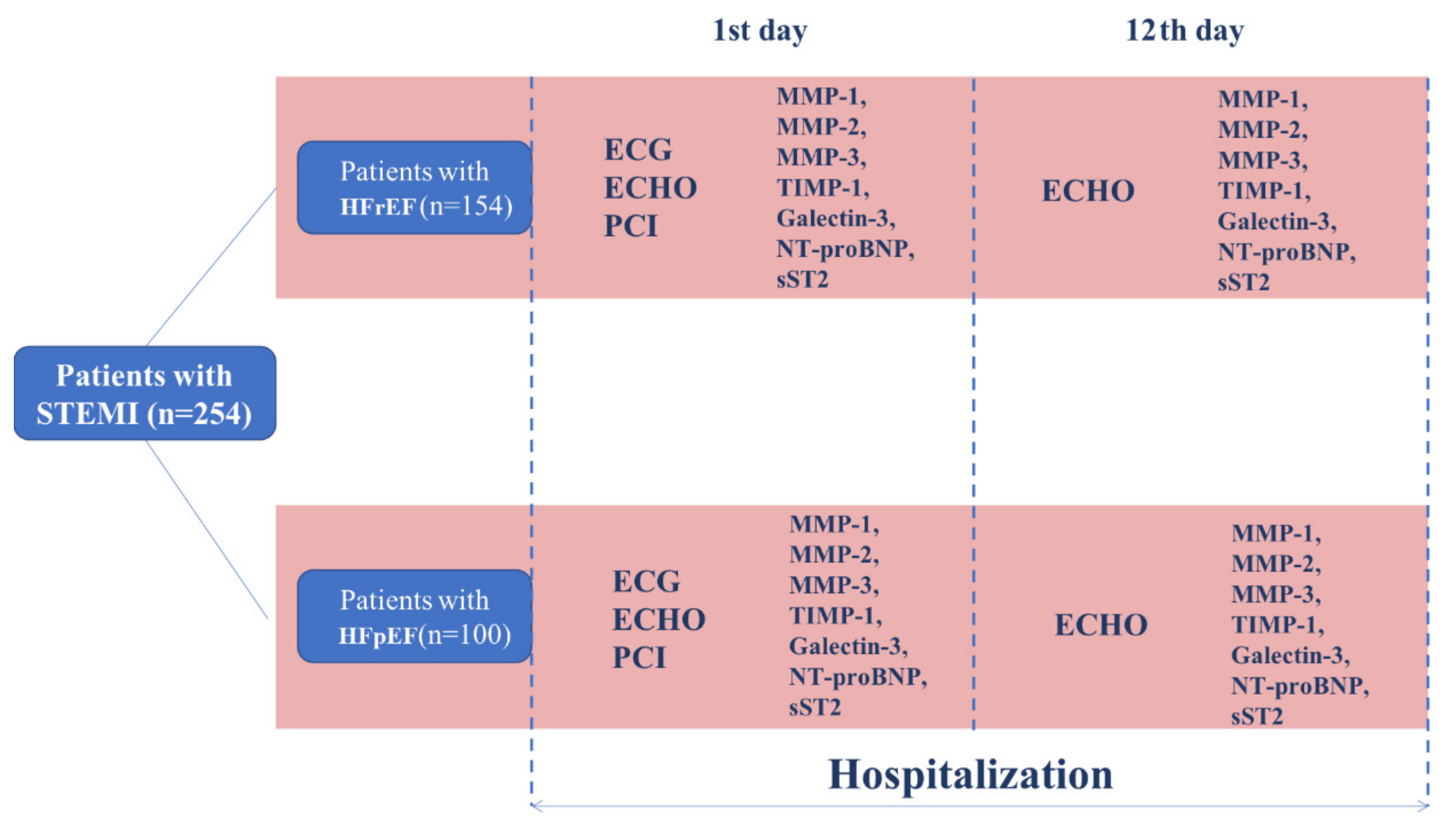
2. Materials and Methods
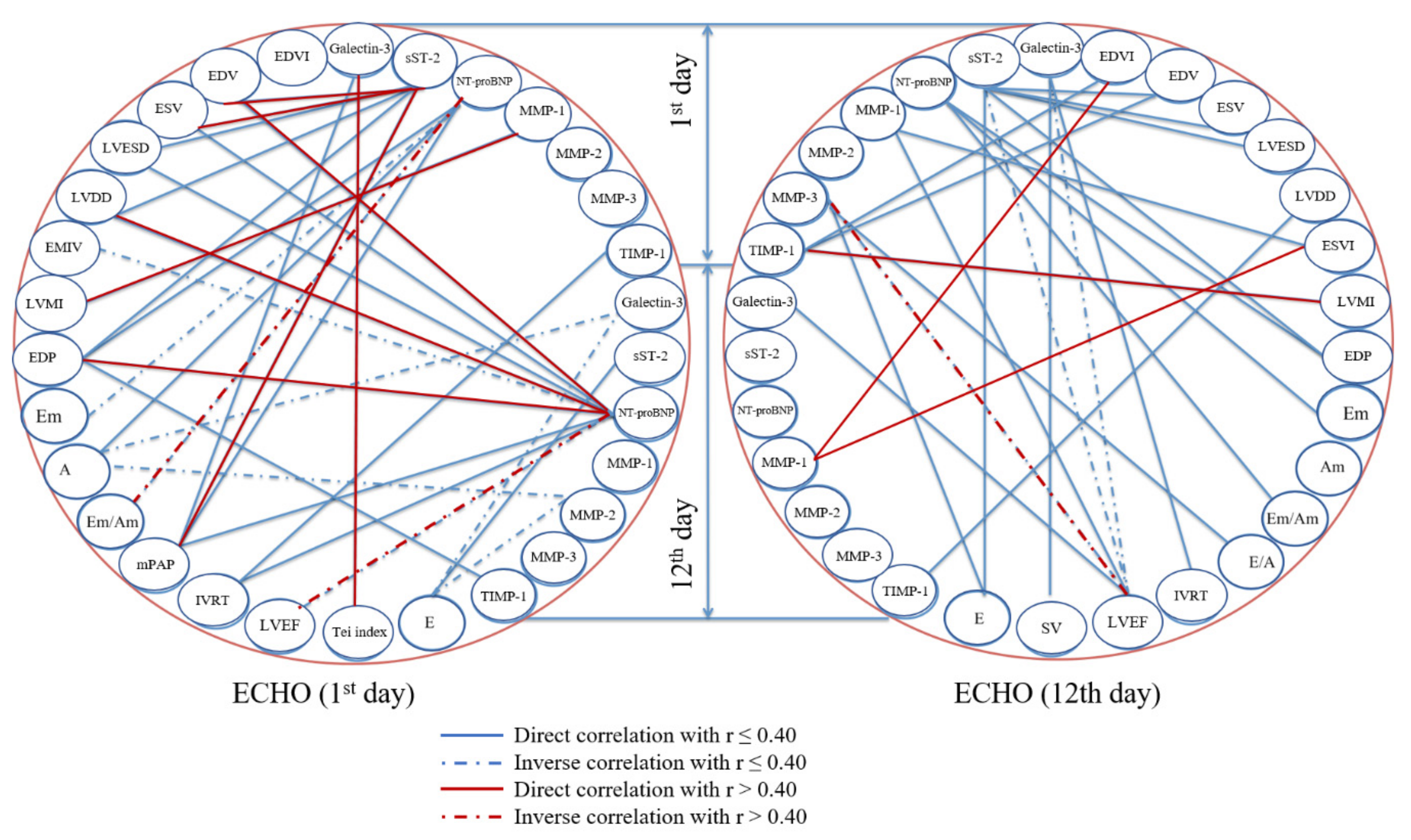
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Ezzati, M.; Obermeyer, Z.; Tzoulaki, I.; Mayosi, B.M.; Elliott, P.; Leon, D.A. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat. Rev. Cardiol. 2015, 12, 508–530. [Google Scholar] [CrossRef] [PubMed]
- Boytsov, S.A.; Shalnova, S.A.; Deev, A.D. Cardiovascular mortality in the Russian Federation and possible mechanisms of its changes. Zh. Nevrol. Psikhiatr. Im. S. S. Korsakova 2018, 118, 98–103. [Google Scholar] [CrossRef]
- Shah, K.S.; Xu, H.; Matsouaka, R.A.; Bhatt, D.L.; Heidenreich, P.A.; Hernandez, A.F.; Devore, A.D.; Yancy, C.W.; Fonarow, G.C. Heart Failure with Preserved, Borderline, and Reduced Ejection Fraction: 5-Year Outcomes. J. Am. Coll. Cardiol. 2017, 70, 2476–2486. [Google Scholar] [CrossRef]
- González, A.; Schelbert, E.B.; Díez, J.; Butler, J. Myocardial Interstitial Fibrosis in Heart Failure: Biological and Translational Perspectives. J. Am. Coll. Cardiol. 2018, 71, 1696–1706. [Google Scholar] [CrossRef] [PubMed]
- Oatmen, K.E.; Cull, E.; Spinale, F.G. Heart failure as interstitial cancer: Emergence of a malignant fibroblast phenotype. Nat. Rev. Cardiol. 2019, 4. [Google Scholar] [CrossRef]
- Carnes, J.; Gordon, G. Biomarkers in Heart Failure with Preserved Ejection Fraction: An Update on Progress and Future Challenges. Heart Lung Circ. 2020, 29, 62–68. [Google Scholar] [CrossRef]
- Sarhene, M.; Wang, Y.; Wei, J.; Huang, Y.; Li, M.; Li, L.; Acheampong, E.; Zhou, Z.; Qin, X.; Yunsheng, X.; et al. Biomarkers in heart failure: The past, current and future. Heart Fail. Rev. 2019, 24, 867–903. [Google Scholar] [CrossRef]
- Ranjan, P.; Kumari, R.; Verma, S.K. Cardiac Fibroblasts and Cardiac Fibrosis: Precise Role of Exosomes. Front. Cell Dev. Biol. 2019, 7, 318. [Google Scholar] [CrossRef]
- Borlaug, B.A. Evaluation and management of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 2020, 30. [Google Scholar] [CrossRef]
- Vinereanu, D.; Mǎrgulescu, A.D. The fallacy of resting echocardiographic parameters of cardiac function in heart failure with preserved ejection fraction: Add global longitudinal strain to the list. Eur. J. Heart Fail. 2017, 19, 901–903. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Špinarová, M.; Meluzín, J.; Podroužková, H.; Štěpánová, R.; Špinarová, L. New echocardiographic parameters in the diagnosis of heart failure with preserved ejection fraction. Int. J. Cardiovasc. Imaging 2018, 34, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, I.M.; Hafez, H.; Al-Shair, M.H.A.; El Zayat, A. Echocardiographic parameters differentiating heart failure with preserved ejection fraction from asymptomatic left ventricular diastolic dysfunction. Echocardiography 2020, 37, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Iyngkaran, P.; Thomas, M.C.; Neil, C.; Jelinek, M.; Cooper, M.; Horowitz, J.D.; Hare, D.L.; Kaye, D.M. The Heart Failure with Preserved Ejection Fraction Conundrum-Redefining the Problem and Finding Common Ground? Curr. Heart Fail. Rep. 2020, 17, 34–42. [Google Scholar] [CrossRef]
- Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology (ESC); Steg, P.G.; James, S.K.; Atar, D.; Badano, L.P.; Blömstrom-Lundqvist, C.; Borger, M.A.; Di Mario, C.; Dickstein, K.; Ducrocq, G.; et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2012, 33, 2569–2619. [Google Scholar] [CrossRef]
- Montalescot, G.; Sechtem, U.; Achenbach, S.; Andreotti, F.; Arden, C.; Budaj, A.; Bugiardini, R.; Crea, F.; Cuisset, T.; Di Mario, C.; et al. 2013 ESC guidelines on the management of stable coronary artery disease: The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur. Heart J. 2013, 34, 2949–3003. [Google Scholar] [CrossRef]
- McMurray, J.J.; Adamopoulos, S.; Anker, S.D.; Auricchio, A.; Böhm, M.; Dickstein, K.; Falk, V.; Filippatos, G.; Fonseca, C.; Gomez-Sanchez, M.A.; et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2012, 14, 803–869. [Google Scholar] [CrossRef]
- Camm, A.J.; Lip, G.Y.; De Caterina, R.; Savelieva, I.; Atar, D.; Hohnloser, S.H.; Hindricks, G.; Kirchhof, P.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: An update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur. Heart J. 2012, 33, 2719–2747. [Google Scholar] [CrossRef]
- Tendera, M.; Aboyans, V.; Bartelink, M.L.; Baumgartner, I.; Clément, D.; Collet, J.P.; Cremonesi, A.; De Carlo, M.; Erbel, R.; Fowkes, F.G.; et al. ESC Committee for Practice Guidelines. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: The Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur. Heart J. 2011, 32, 2851–2906. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef]
- European Association for Cardiovascular Prevention & Rehabilitation; Reiner, Z.; Catapano, A.L.; De Backer, G.; Graham, I.; Taskinen, M.R.; Wiklund, O.; Agewall, S.; Alegria, E.; Chapman, M.J.; et al. ESC Committee for Practice Guidelines (CPG) 2008–2010 and 2010–2012 Committees. ESC/EAS Guidelines for the management of dyslipidaemias: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur. Heart J. 2011, 32, 1769–1818. [Google Scholar] [CrossRef] [PubMed]
- Rydén, L.; Grant, P.J.; Anker, S.D.; Berne, C.; Cosentino, F.; Danchin, N.; Deaton, C.; Escaned, J.; Hammes, H.P.; Huikuri, H.; et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur. Heart J. 2013, 34, 3035–3087. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.Y.; Akizawa, T.; Bavanandan, S.; Hamano, T.; Liew, A.; Lu, K.C.; Lumlertgul, D.; Oh, K.H.; Zhao, M.H.; Ka-Shun Fung, S.; et al. 2017 Kidney Disease: Improving Global Outcomes (KDIGO) Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Guideline Update Implementation: Asia Summit Conference Report. Kidney Int. Rep. 2019, 4, 1523–1537. [Google Scholar] [CrossRef] [PubMed]
- National Clinical Guideline Centre (UK). Obesity: Identification, Assessment and Management of Overweight and Obesity in Children, Young People and Adults: Partial Update of CG43; NICE Clinical Guidelines, No. 189; National Institute for Health and Care Excellence: London, UK, 2014; pp. 1–149. [Google Scholar]
- Xu, M.; Yan, L.; Xu, J.; Yang, X.; Jiang, T. Predictors and prognosis for incident in-hospital heart failure in patients with preserved ejection fraction after first acute myocardial infarction: An observational study. Med. (Baltim.) 2018, 97, e11093. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, R.S.; Tu, J.V.; Lee, D.S.; Austin, P.C.; Fang, J.; Haouzi, A.; Gong, Y.; Liu, P.P. Outcome of heart failure with preserved ejection fraction in a population-based study. N. Engl. J. Med. 2006, 355, 260–269. [Google Scholar] [CrossRef]
- Brunner-La Rocca, H.P.; Sanders-van Wijk, S. Natriuretic Peptides in Chronic Heart Failure. Card. Fail. Rev. 2019, 5, 44–49. [Google Scholar] [CrossRef]
- Pagel-Langenickel, I. Evolving Role of Natriuretic Peptides from Diagnostic Tool to Therapeutic Modality. Adv. Exp. Med. Biol. 2018, 1067, 109–131. [Google Scholar] [CrossRef]
- Salah, K.; Stienen, S.; Pinto, Y.M.; Eurlings, L.W.; Metra, M.; Bayes-Genis, A.; Verdiani, V.; Tijssen, J.G.P.; Kok, W.E. Prognosis and NT-proBNP in heart failure patients with preserved versus reduced ejection fraction. Heart 2019, 105, 1182–1189. [Google Scholar] [CrossRef]
- Savarese, G.; Orsini, N.; Hage, C.; Vedin, O.; Cosentino, F.; Rosano, G.M.C.; Dahlström, U.; Lund, L.H. Utilizing NT-proBNP for Eligibility and Enrichment in Trials in HFpEF, HFmrEF, and HFrEF. JACC Heart Fail. 2018, 6, 246–256. [Google Scholar] [CrossRef]
- Magnussen, C.; Blankenberg, S. Biomarkers for heart failure: Small molecules with high clinical relevance. J. Intern. Med. 2018, 283, 530–543. [Google Scholar] [CrossRef]
- Vianello, E.; Dozio, E.; Tacchini, L.; Frati, L.; Corsi Romanelli, M.M. ST2/IL-33 signaling in cardiac fibrosis. Int. J. Biochem. Cell Biol. 2019, 116, 105619. [Google Scholar] [CrossRef] [PubMed]
- Bartunek, J.; Delrue, L.; Van Durme, F.; Muller, O.; Casselman, F.; De Wiest, B.; Croes, R.; Verstreken, S.; Goethals, M.; de Raedt, H.; et al. Nonmyocardial production of ST2 protein in human hypertrophy and failure is related to diastolic load. J. Am. Coll. Cardiol. 2008, 52, 2166–2174. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Yu, C.C.; Chiu, F.C.; Tsai, C.T.; Lai, L.P.; Hwang, J.J.; Lin, J.L. Soluble ST2 as a biomarker for detecting stable heart failure with a normal ejection fraction in hypertensive patients. J. Card. Fail. 2013, 19, 163–168. [Google Scholar] [CrossRef]
- Song, Y.; Li, F.; Xu, Y.; Liu, Y.; Wang, Y.; Han, X.; Fan, Y.; Cao, J.; Luo, J.; Sun, A.; et al. Prognostic value of sST2 in patients with heart failure with reduced, mid-range and preserved ejection fraction. Int. J. Cardiol. 2020, 304, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Hara, A.; Niwa, M.; Noguchi, K.; Kanayama, T.; Niwa, A.; Matsuo, M.; Hatano, Y.; Tomita, H. Galectin-3 as a Next-Generation Biomarker for Detecting Early Stage of Various Diseases. Biomolecules 2020, 10, 389. [Google Scholar] [CrossRef] [PubMed]
- Felker, G.M.; Fiuzat, M.; Shaw, L.K.; Clare, R.; Whellan, D.J.; Bettari, L.; Shirolkar, S.C.; Donahue, M.; Kitzman, D.W.; Zannad, F.; et al. Galectin-3 in ambulatory patients with heart failure: Results from the HF-ACTION study. Circ. Heart Fail. 2012, 5, 72–78. [Google Scholar] [CrossRef]
- Di Tano, G.; Caretta, G.; De Maria, R. Galectin-3 predicts left ventricular remodelling after anterior-wall myocardial infarction treated by primary percutaneous coronary intervention. Heart 2017, 103, 71–77. [Google Scholar] [CrossRef]
- Ho, J.E.; Liu, C.; Lyass, A. Galectin-3, a marker of cardiac fibrosis, predicts incident heart failure in the community. J. Am. Coll. Cardiol. 2012, 60, 1249–1256. [Google Scholar] [CrossRef]
- Polat, V.; Bozcali, E.; Uygun, T.; Opan, S.; Karakaya, O. Diagnostic significance of serum galectin-3 levels in heart failure with preserved ejection fraction. Acta Cardiol. 2016, 71, 191–197. [Google Scholar] [CrossRef]
- Cui, Y.; Qi, X.; Huang, A.; Li, J.; Hou, W.; Liu, K. Differential and Predictive Value of Galectin-3 and Soluble Suppression of Tumorigenicity-2 (sST2) in Heart Failure with Preserved Ejection Fraction. Med. Sci. Monit. 2018, 24, 5139–5146. [Google Scholar] [CrossRef]
- Wu, C.K.; Su, M.M.; Wu, Y.F.; Hwang, J.J.; Lin, L.Y. Combination of Plasma Biomarkers and Clinical Data for the Detection of Myocardial Fibrosis or Aggravation of Heart Failure Symptoms in Heart Failure with Preserved Ejection Fraction Patients. J. Clin. Med. 2018, 7, 427. [Google Scholar] [CrossRef] [PubMed]
- Edelmann, F.; Holzendorf, V.; Wachter, R.; Nolte, K.; Schmidt, A.G.; Kraigher-Krainer, E.; Duvinage, A.; Unkelbach, I.; Düngen, H.D.; Tschöpe, C.; et al. Galectin-3 in patients with heart failure with preserved ejection fraction: Results from the Aldo-DHF trial. Eur. J. Heart Fail. 2015, 17, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, M.L. Assigning matrix metalloproteinase roles in ischaemic cardiac remodelling. Nat. Rev. Cardiol. 2018, 15, 471–479. [Google Scholar] [CrossRef]
- Kelly, D.; Khan, S.Q.; Thompson, M.; Cockerill, G.; Ng, L.L.; Samani, N.; Squire, I.B. Plasma tissue inhibitor of metalloproteinase-1 and matrix metalloproteinase-9: Novel indicators of left ventricular remodelling and prognosis after acute myocardial infarction. Eur. Heart J. 2008, 29, 2116–2124. [Google Scholar] [CrossRef]
- Jordán, A.; Roldán, V.; García, M.; Monmeneu, J.; de Burgos, F.G.; Lip, G.Y.; Marín, F. Matrix metalloproteinase-1 and its inhibitor, TIMP-1, in systolic heart failure: Relation to functional data and prognosis. J. Intern. Med. 2007, 262, 385–392. [Google Scholar] [CrossRef]
- Orn, S.; Manhenke, C.; Squire, I.B.; Ng, L.; Anand, I.; Dickstein, K. Plasma MMP-2, MMP-9 and N-BNP in long-term survivors following complicated myocardial infarction: Relation to cardiac magnetic resonance imaging measures of left ventricular structure and function. J. Card. Fail. 2007, 13, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Sundström, J.; Evans, J.C.; Benjamin, E.J.; Levy, D.; Larson, M.G.; Sawyer, D.B.; Siwik, D.A.; Colucci, W.S.; Sutherland, P.; Wilson, P.W.; et al. Relations of plasma matrix metalloproteinase-9 to clinical cardiovascular risk factors and echocardiographic left ventricular measures: The Framingham Heart Study. Circulation 2004, 109, 2850–2856. [Google Scholar] [CrossRef] [PubMed]
- Martos, R.; Baugh, J.; Ledwidge, M.; O’Loughlin, C.; Murphy, N.F.; Conlon, C.; Patle, A.; Donnelly, S.C.; McDonald, K. Diagnosis of heart failure with preserved ejection fraction: Improved accuracy with the use of markers of collagen turnover. Eur. J. Heart Fail. 2009, 11, 191–197. [Google Scholar] [CrossRef]

| Features | Patients with HFpEF, n (%) | Patients with HFrEF, n (%) | p Value |
|---|---|---|---|
| Male gender | 74 (74.0%) | 102 (66.2%) | 0.24 |
| Past medical history of myocardial infarction | 5 (5.0%) | 70 (45.4%) | 0.0001 |
| Past medical history of percutaneous coronary intervention | 3 (3.0%) | 2 (1.3%) | 0.62 |
| Past medical history of coronary artery bypass graft surgery | 0 (0.0%) | 1 (0.6%) | 1.0 |
| Past medical history of angina pectoris | 31 (31.0%) | 108 (70.1%) | 0.0001 |
| Past medical history of atrial fibrillation | 4 (4.0%) | 28 (18.2%) | 0.002 |
| Past medical history of chronic heart failure | 12 (12.0%) | 101 (65.6%) | 0.0001 |
| Past medical history of stroke or transient ischemic attack | 4 (4.0%) | 18 (11.7%) | 0.06 |
| Peripheral artery disease | 1 (1.0%) | 10 (6.5%) | 0.07 |
| Arterial hypertension | 70 (70.0%) | 131 (85.1%) | 0.006 |
| Chronic kidney disease, stage 1–3 | 2 (2.0%) | 15 (9.7%) | 0.03 |
| Type 2 diabetes mellitus | 11 (11.0%) | 30 (19.5%) | 0.10 |
| Glucose intolerance | 2 (2.0%) | 0 (0.0%) | 0.15 |
| Smoking | 56 (56.0%) | 57 (37.0%) | 0.004 |
| Hypercholesterolemia | 22 (22.0%) | 69 (44.8%) | 0.0003 |
| Overweight or obesity | 71 (71.0%) | 91 (59.1%) | 0.07 |
| Family history of coronary artery disease | 3 (3.0%) | 37 (24.0%) | <0.0001 |
| Median (Interquartile Range) | |||
| Age, years | 57 (52; 63) | 63 (56; 67) | <0.0001 |
| Body mass index | 26.9 (24.3; 29.8) | 27.9 (25.1; 31.2) | 0.0036 |
| Duration of hospital stay | 14 (12; 18) | 15 (13; 19) | 0.01 |
| Drug | Prior to Myocardial Infarction Number of Patients (Equal to the Proportion as n = 100) | During the Hospital Stay Number of Patients (Equal to the Proportion as n = 100) |
|---|---|---|
| Aspirin | 9 | 99 |
| Clopidogrel | 0 | 83 |
| Ticagrelor | 0 | 25 |
| Beta-blockers | 11 | 97 |
| ACE inhibitors | 11 | 77 |
| Statins | 4 | 94 |
| Coronary Angiography Features | Number of Patients (Equal to the Proportion as n = 100) |
|---|---|
| >50% stenosis | 41 |
| Multivessel coronary artery disease (>3 affected arteries) | 26 |
| Complications during the hospital stay | |
| Arrhythmia or heart block | 8 |
| Pulmonary oedema | 2 |
| Radial artery bleeding | 2 |
| Coronary artery perforation | 2 |
| Early postoperative angina | 1 |
| Recurrent myocardial infarction | 1 |
| Cardiogenic shock | 1 |
| Death | 0 |
| Parameter | 1st Day after STEMI Onset Median (Interquartile Range) | 10th–12th Day after STEMI Onset Median (Interquartile Range) | p Value |
|---|---|---|---|
| Left ventricular ejection fraction, % | 56.0 (48.5; 61.0) | 60.0 (52.0; 64.0) | 0.015 |
| Left ventricular end-diastolic volume, mL | 126.0 (117.25; 142.25) | 118.0 (98.0; 135.0) | 0.003 |
| Left ventricular end-systolic volume, mL | 66.0 (54.0; 83.0) | 62.0 (51.0; 74.0) | 0.015 |
| Left ventricular end-diastolic diameter, cm | 5.5 (5.2; 5.7) | 5.4 (5.23; 5.7) | 0.861 |
| Left ventricular end-systolic diameter, cm | 3.9 (3.6; 4.3) | 3.8 (3.5; 4.1) | 0.038 |
| Left ventricular end-diastolic volume/body surface area, mL/m2 | 10.88 (9.9; 11.84) | 10.4 (9.44; 11.84) | 0.875 |
| Left ventricular end-systolic volume/body surface area, mL/m2 | 37.0 (28.0; 42.75) | 32.0 (26.0; 39.0) | 0.112 |
| Pulmonary artery pressure, mmHg | 25.0 (23.0; 27.5) | 25.0 (23.0; 27.0) | 0.086 |
| Left ventricular end-diastolic pressure, mmHg | 10.88 (9.9; 11.84) | 10.4 (9.44; 11.84) | 0.070 |
| Stroke volume, mL | 79.0 (70.25; 88.0) | 81.0 (74.25; 90.0) | 0.005 |
| Left ventricular mass, g | 241.0 (217.5; 271.0) | 234.0 (213.0; 271.0) | 0.141 |
| Left ventricular mass/body surface area, g/m2 | 130.0 (122.0; 140.75) | 124.0 (116.0; 142.0) | 0.515 |
| Left atrial diameter, cm | 4.1 (3.9; 4.25) | 4.1 (3.9; 4.3) | 0.799 |
| Right atrial diameter, cm | 4.1 (3.9; 4.4) | 4.2 (3.9; 4.4) | 0.411 |
| Right ventricular diameter, cm | 1.8 (1.5; 1.9) | 1.8 (1.5; 1.9) | 0.855 |
| Isovolumic relaxation time, ms | 111.0 (104.0; 118.0) | 110.0 (104.0; 118.0) | 0.171 |
| Early diastolic ventricular filling velocity (E, cm/sec) | 57.0 (49.0; 70.0) | 60.0 (47.0; 71.75) | 0.662 |
| Late diastolic ventricular filling velocity (A, cm/sec) | 69.0 (59.0; 78.0) | 69.5 (54.25; 78.75) | 0.710 |
| Early to late diastolic ventricular filling velocity ratio (E/A) | 0.78 (0.71; 1.17) | 0.79 (0.68; 1.24) | 0.282 |
| Deceleration time, ms | 202.0 (170.0; 223.0) | 195.0 (170.0; 221.75) | 0.025 |
| Acceleration time, ms | 131.0 (114.5; 142.5) | 131.0 (111.0; 137.0) | 0.243 |
| Left ventricular ejection time, ms | 294.0 (279.5; 305.0) | 287.0 (268.0; 300.0) | 0.026 |
| Early diastolic myocardial velocity, cm/sec | 7.0 (6.0; 8.0) | 6.0 (5.0; 8.0) | 0.018 |
| Late diastolic myocardial velocity, cm/sec | 8.0 (6.9; 9.0) | 7.95 (7.0; 9.0) | 0.675 |
| Early to late diastolic myocardial velocity ratio | 0.83 (0.7; 1.14) | 0.75 (0.67; 1.14) | 0.009 |
| Early mitral filling velocity to early diastolic mitral annular velocity ratio | 8.59 (7.36; 10.23) | 9.0 (7.67; 10.42) | 0.038 |
| Early mitral inflow velocity, cm/sec | 37.0 (29.0; 45.0) | 40.0 (32.0; 48.0) | 0.001 |
| Early diastolic myocardial velocity to early mitral inflow velocity ratio | 1.56 (1.3; 2.0) | 1.36 (1.03; 1.87) | 0.001 |
| Tei index (myocardial performance index) | 0.7 (0.65; 0.77) | 0.71 (0.65; 0.78) | 0.758 |
| Parameter | Reference Range | 1st Day after STEMI Onset Median (Interquartile Range) | 10th–12th day after STEMI Onset Median (Interquartile Range) | p Value |
|---|---|---|---|---|
| Patients with HFpEF | ||||
| NT-proBNP, fmol/mL | 5.0–12.0 | 17.84 (6.36; 60.4) | 4.68 (2.5; 8.35) | 0.0361 |
| sST2, ng/mL | 14.0–22.5 | 40.75 (26.98; 64.6) | 22.19 (18.11; 25.3) | 0.0001 |
| Galectin-3, ng/mL | 0.62–6.25 | 11.37 (9.49; 14.0) | 9.05 (6.0; 10.41) | 0.0001 |
| MMP-1, ng/mL | 0.91–9.34 | 2.14 (1.43; 5.39) | 2.59 (1.72; 4.0) | 0.2372 |
| MMP-2, ng/mL | 139.0–356.0 | 254.9 (217.2; 283.83) | 295.2 (267.3; 326.65) | 0.0003 |
| MMP-3, ng/mL | 2.0–36.6 | 7.22 (5.29; 10.6) | 11.89 (8.99; 13.63) | 0.0001 |
| TIMP-1, ng/mL | 11.0–743.0 | 899.25 (592.5; 1080.0) | 853.5 (559.75; 1017.5) | 0.7332 |
| Patients with HFrEF | ||||
| NT-proBNP, fmol/mL | 5.0–12.0 | 29.87 (10.65; 84.91) | 18.69 (8.65; 42.76) | 0.0265 |
| sST2, ng/mL | 14.0–22.5 | 56.45 (33.77; 75.88) | 35.33 (22.79; 47.16) | 0.0020 |
| Galectin-3, ng/mL | 0.62–6.25 | 14.59 (10.64; 16.45) | 12.17 (9.12; 14.89) | 0.0231 |
| MMP-1, ng/mL | 0.91–9.34 | 1.66 (0.73; 3.02) | 2.20 (1.32; 4.51) | 0.0001 |
| MMP-2, ng/mL | 139.0–356.0 | 289.3 (222.92; 315.31) | 332.12 (297.7; 423.59) | 0.0032 |
| MMP-3, ng/mL | 2.0–36.6 | 12.48 (10.19; 16.97) | 14.67 (12.34; 17.93) | 0.0035 |
| TIMP-1, ng/mL | 11.0–743.0 | 567.32 (412.9; 787.32) | 414.22 (324.23; 668.45) | 0.0039 |
| HFpEF vs. HFrEF (p Value) | ||||
| NT-proBNP, fmol/mL | 5.0–12.0 | 0.0056 | 0.0001 | |
| sST2, ng/mL | 14.0–22.5 | 0.0001 | 0.0001 | |
| Galectin-3, ng/mL | 0.62–6.25 | 0.0001 | 0.0001 | |
| MMP-1, ng/mL | 0.91–9.34 | 0.0075 | 0.82 | |
| MMP-2, ng/mL | 139.0–356.0 | 0.0001 | 0.0001 | |
| MMP-3, ng/mL | 2.0–36.6 | 0.0001 | 0.0001 | |
| TIMP-1, ng/mL | 11.0–743.0 | 0.0001 | 0.0001 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pecherina, T.; Kutikhin, A.; Kashtalap, V.; Karetnikova, V.; Gruzdeva, O.; Hryachkova, O.; Barbarash, O. Serum and Echocardiographic Markers May Synergistically Predict Adverse Cardiac Remodeling after ST-Segment Elevation Myocardial Infarction in Patients with Preserved Ejection Fraction. Diagnostics 2020, 10, 301. https://doi.org/10.3390/diagnostics10050301
Pecherina T, Kutikhin A, Kashtalap V, Karetnikova V, Gruzdeva O, Hryachkova O, Barbarash O. Serum and Echocardiographic Markers May Synergistically Predict Adverse Cardiac Remodeling after ST-Segment Elevation Myocardial Infarction in Patients with Preserved Ejection Fraction. Diagnostics. 2020; 10(5):301. https://doi.org/10.3390/diagnostics10050301
Chicago/Turabian StylePecherina, Tamara, Anton Kutikhin, Vasily Kashtalap, Victoria Karetnikova, Olga Gruzdeva, Oksana Hryachkova, and Olga Barbarash. 2020. "Serum and Echocardiographic Markers May Synergistically Predict Adverse Cardiac Remodeling after ST-Segment Elevation Myocardial Infarction in Patients with Preserved Ejection Fraction" Diagnostics 10, no. 5: 301. https://doi.org/10.3390/diagnostics10050301
APA StylePecherina, T., Kutikhin, A., Kashtalap, V., Karetnikova, V., Gruzdeva, O., Hryachkova, O., & Barbarash, O. (2020). Serum and Echocardiographic Markers May Synergistically Predict Adverse Cardiac Remodeling after ST-Segment Elevation Myocardial Infarction in Patients with Preserved Ejection Fraction. Diagnostics, 10(5), 301. https://doi.org/10.3390/diagnostics10050301






