Insights on Hysteroscopic Procedures and Their Place in Romanian Gynecologic Practice—The Experience of Two Medical Units
Abstract
1. Introduction
2. Materials and Methods
- Women aged over 18 years;
- Admitted to “St. Pantelimon” Emergency Hospital during January 2014–October 2019 or at Timisoara Municipal Clinical Hospital during October 2018–October 2019;
- Underwent hysteroscopic procedure.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AUB | Abnormal uterine bleeding |
| IUD | Intrauterine device |
| HP | Histopathologic |
| CIN | Cervical intraepithelial neoplasm |
| FIGO | International Federation of Gynecology and Obstetrics |
| TV-US | Transvaginal Ultrasound |
| WHO | World Health Organization |
References
- Eurostat Statistics Explained. Hospital discharges and Length of Stay Statistics. Available online: https://ec.europa.eu/eurostat/statisticsexplained/index.php?title=Hospital_discharges_and_length_of_stay_statistics#Average_length_of_hospital_stay_for_in-patients (accessed on 20 January 2020).
- Chapter 7: Health. In 2017 Romanian Statistical Yearbook; Andrei, T., Ed.; National Institute of Statistics: Bucharest, Romania, 2017; pp. 296–301. ISSN 1220-3246. [Google Scholar]
- Angioni, S.; Loddo, A.; Milano, F.; Piras, B.; Minerba, L.; Melis, G.B. Detection of benign intracavitary lesions in postmenopausal women with abnormal uterine bleeding: A prospective comparative study on outpatient hysteroscopy and blind biopsy. J. Minim. Invasive Gynecol 2008, 15, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Kolhe, S. Management of abnormal uterine bleeding—focus on ambulatory hysteroscopy. Int J. Womens Health 2018, 10, 127–136. [Google Scholar] [CrossRef] [PubMed]
- The World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 22 January 2020).
- International Federation of Gynecology and Obstetrics. FIGO Committee for Menstrual Disorders. Available online: https://www.figo.org/figo-committee-mdc (accessed on 22 January 2020).
- Haththotuwa, R.; Goonewardene, M.; Desai, S.; Senanayake, L.; Tank, J.; Fraser, I.S. Management of abnormal uterine bleeding in low- and high- resource settings: Consideration of cultural issues. Semin Reprod Med. 2011, 29, 446–458. [Google Scholar] [CrossRef] [PubMed]
- Munro, M.; Critchley, H.O.D.; Broder, M.; Fraser, I.S.; FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J. Gynecol. Obstet. 2011, 113, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.J.; Stevenson, H. Endometrial Polyps and Abnormal Uterine Bleeding (AUB-P)—What is the relationship; how are they diagnosed and how are they treated? Best Pract Res. Clin. Obstet. Gynaecol. 2017, 40, 89–104. [Google Scholar] [CrossRef] [PubMed]
- Al Chami, A.; Saridogan, E. Endometrial polyps and subfertility. Invited review article. J. Obstet. Gynaecol India 2017, 67, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Mouhayar, Y.; Yin, O.; Mumford, S.L.; Segars, J.H. Hysteroscopic polypectomy prior to infertility treatment: A cost analysis and systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 213, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Bittencourt, C.A.; Dos Santos, S.R.; Bernardo, W.M.; Fuchs, L.F.P.; Soares, J.M., Jr.; Pastore, A.R.; Baracat, E.C. Accuracy of saline contrast sonohysterography in detection of endometrial polyps and submucosal leiomyomas in women of reproductive age with abnormal uterine bleeding: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2017, 50, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, S.R.; Lumsden, M.A. Abnormal uterine bleeding in perimenopause. Climacteric 2017, 20, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Lieng, M.; Istre, O.; Qvigstad, E. Treatment of endometrial polyps: A systematic review. Acta Obstet Gynecol. Scand. 2010, 89, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Salazar, C.A.; Isaacson, K. Office operative hysteroscopy—An update. J. Minim. Invasive Gynecol. 2018, 25, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Bosteels, J.; Kasius, J.; Weyers, S.; Broekmans, F.J.; D’Hooghe, T.M.; Bongers, M.Y.; Mol, B.W.J. Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities (Review). Cochrane Database Syst. Rev. 2018, 12, CD009461. [Google Scholar] [CrossRef]
- Finco, A.; Centini, G.; Lazzeri, L.; Zupi, E. Surgical management of abnormal uterine bleeding in fertile age women. Womens Health (Lond) 2015, 11, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Peltecu, G. (Ed.) Cervical Cancer—National Guideline; Romanian Society of Obstetrics and Gynecology and Romanian Medical Council: Bucharest, Romania, 2019. [Google Scholar]
- Suciu, N. (Ed.) Endometrial Cancer—National Guideline; Romanian Society of Obstetrics and Gynecology and Romanian Medical Council: Bucharest, Romania, 2019. [Google Scholar]
- Levy-Zauberman, Y.; Pourcelot, A.G.; Capmas, P.; Fernandez, H. Update on the management of abnormal uterine bleeding. J. Gynecol. Obstet. Hum. Reprod 2017, 46, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Maheux-Lacroix, S.; Li, F.; Laberge, P.; Abbott, J. Imaging for polyps and leiomyomas in women with abnormal uterine bleeding. Obstet. Gynecol. 2016, 128, 1425–1436. [Google Scholar] [CrossRef] [PubMed]
- Valentine, L.; Bradley, L. Hysteroscopy for abnormal uterine bleeding and fibroids. Clin. Obstet. Gynecol. 2017, 60, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Bohiltea, R.E.; Sajin, M.; Furtunescu, F.; Bohîlțea, L.C.; Mihart, A.; Baros, A.; Anca, A.F. Clinical and pathological correlations in endometrial pathology. J. Med. Life 2015, 8, 552–562. [Google Scholar] [PubMed]
- WHO. The Global Prevalence of Anaemia in 2011; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Kremer, T.G.; Ghiorzi, I.B.; Dibi, R.P. Isthmocele: An overview of diagnosis and treatment. Rev. Assoc. Med. Bras. 2019, 65, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Ionescu, C.A.; Dimitriu, M.; Poenaru, E.; Bănacu, M.; Furău, G.O.; Navolan, D.; Ples, L. Defensive caesarean section: A reality and a recommended health care improvement for Romanian obstetrics. J. Eval Clin. Pract. 2019, 25, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Van der Voet, L.F.; Vervoort, A.J.; Veersema, S.; BijdeVaate, A.J.; Brölmann, H.A.; Huirne, J.A. Minimally invasive therapy for gynaecological symptoms related to a niche in the caesarean scar: A systematic review. BJOG 2014, 121, 145–156. [Google Scholar] [CrossRef]
| Total | Bucharest | Timișoara | |
|---|---|---|---|
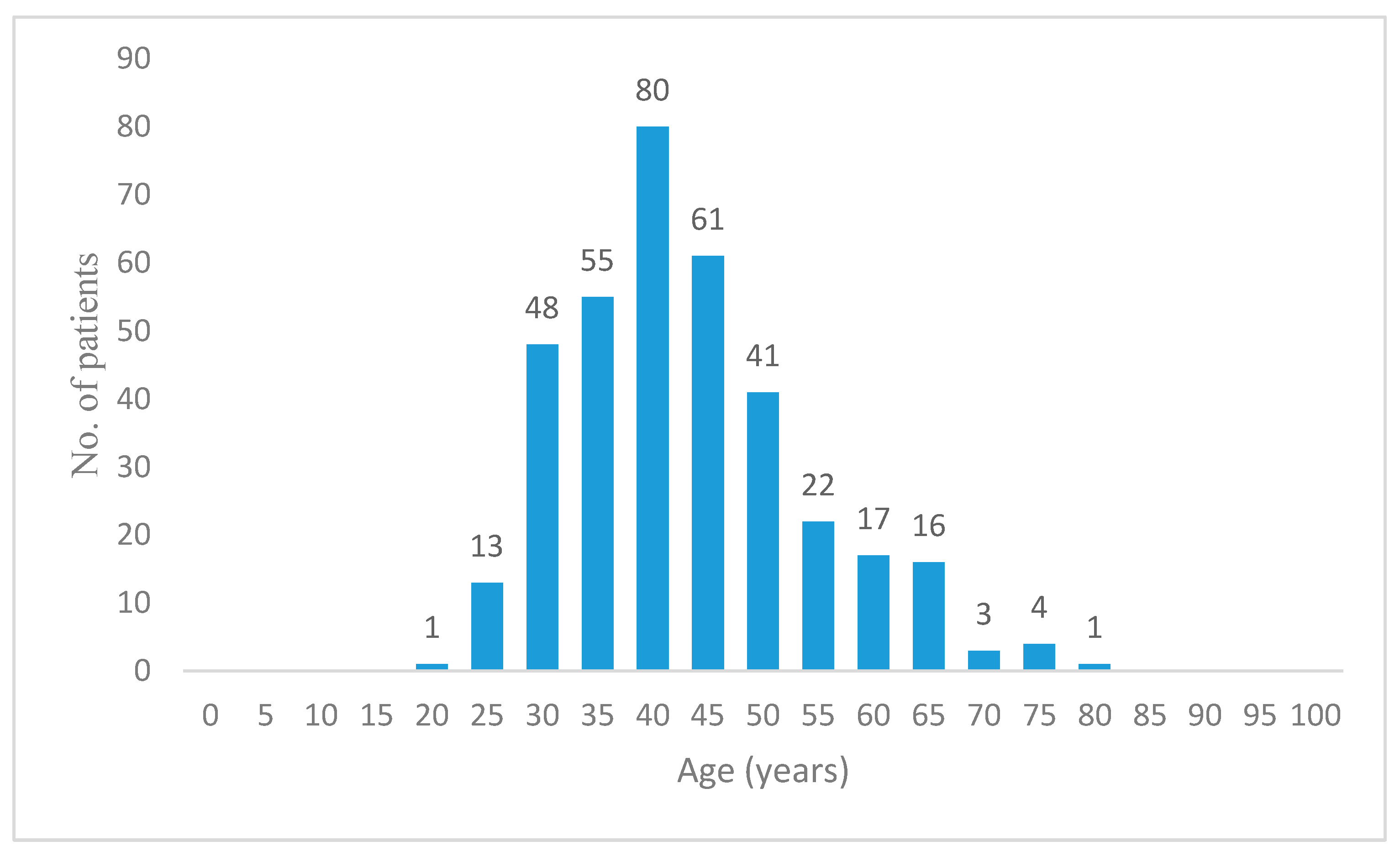
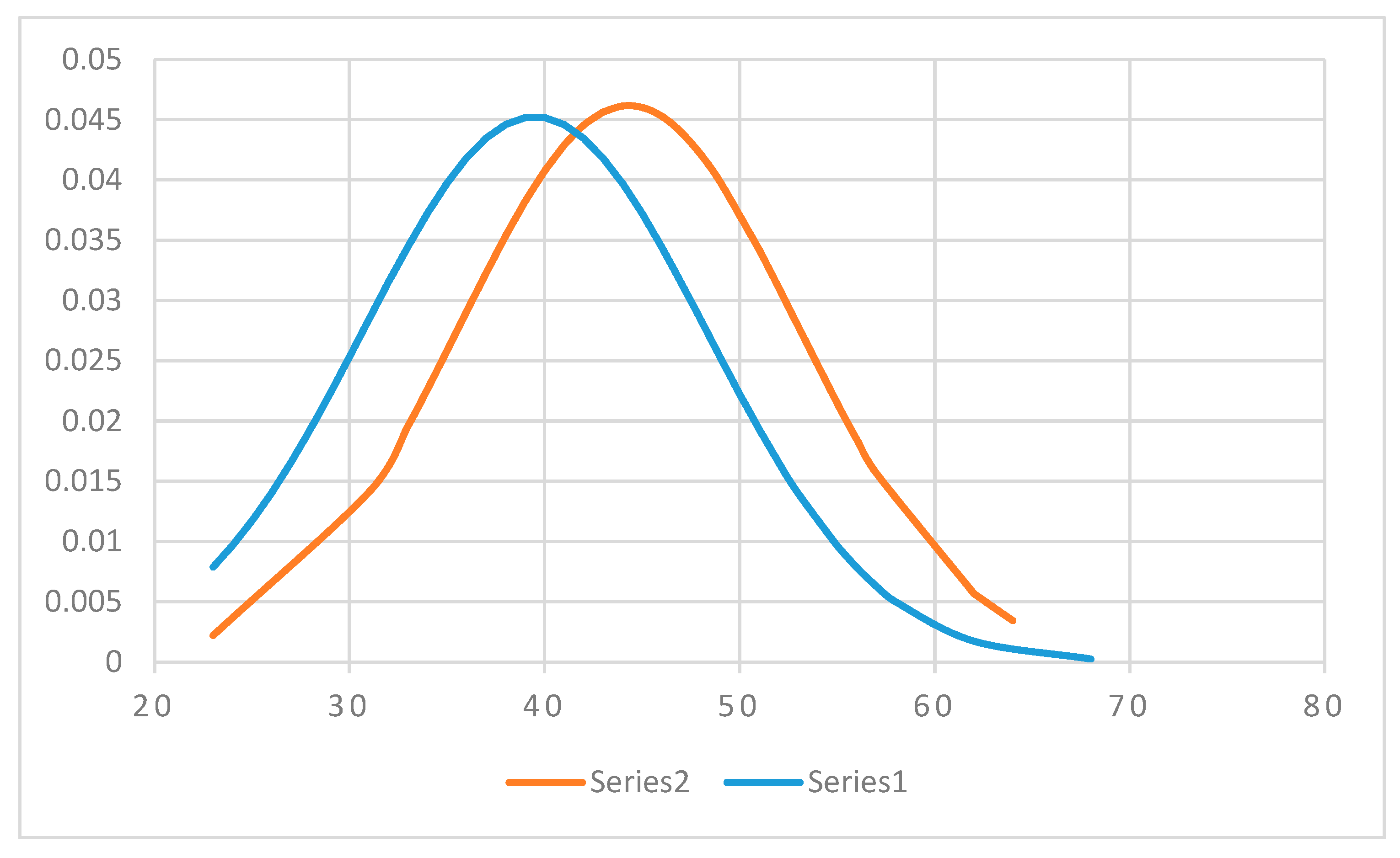
| Average age (years) | 41 | 39 | 41 |
| Min (years) | 20 | 20 | 22 |
| Max (years) | 76 | 63 | 76 |
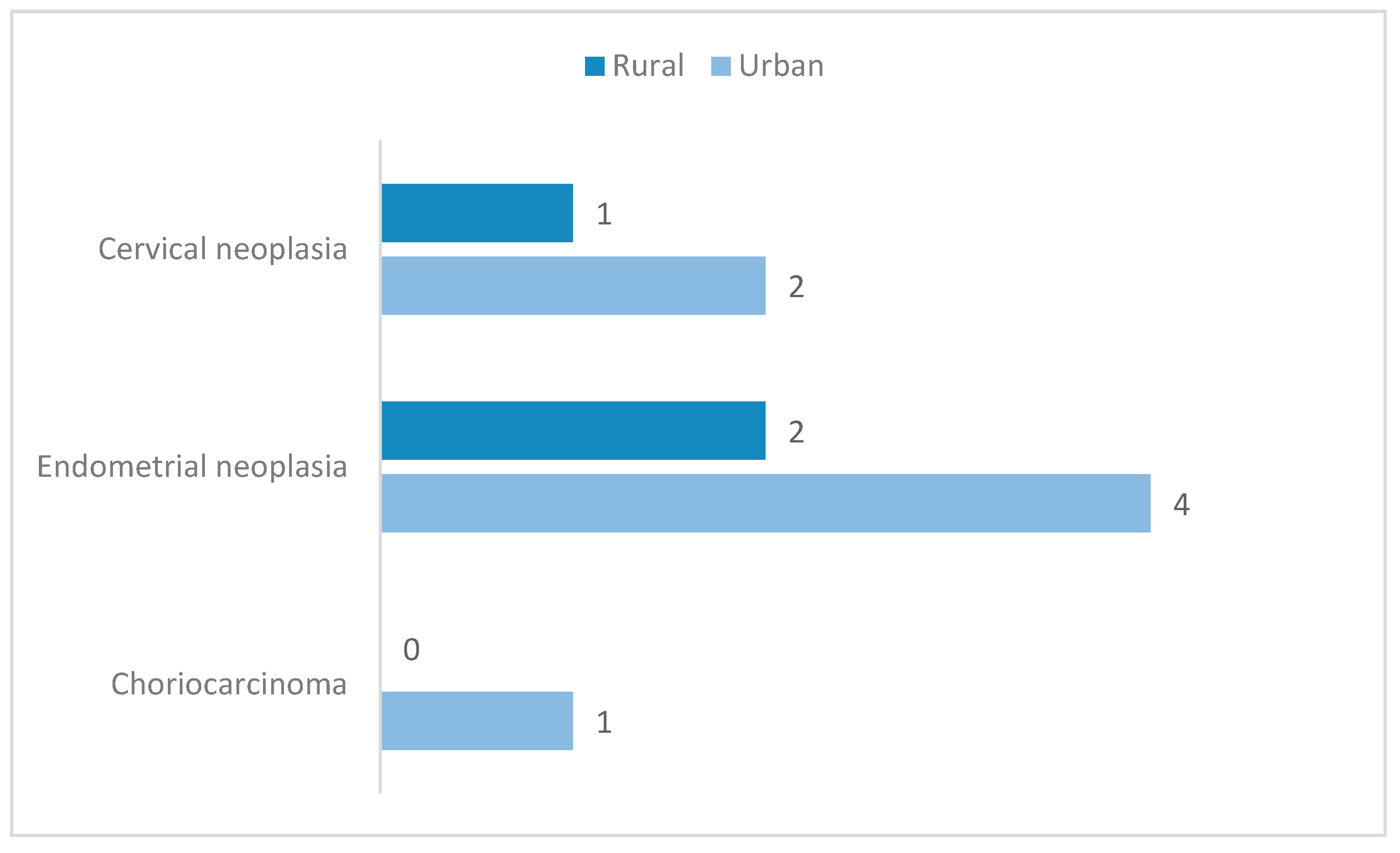
| Area of residence | |||
| Rural | 33.05% | 11.11% | 36.2% |
| Urban | 66.95% | 88.88% | 63.8% |
| Menopausal status | |||
| Menopause | 17.67% | 4.44 % | 19.55% |
| Reproductive age | 82.33% | 95.56% | 80.45% |
| Total 1 | Bucharest | Timișoara | |
|---|---|---|---|
| (N = 368) (100%) | (N = 45) (100%) | (N = 323) (100%) | |
| IUD retention 2 | 19 (5.16%) | 0 (0.00%) | 19 (5.88%) |
| AUB 3 | 131 (35.59%) | 36 (80.00%) | 95 (29.41%) |
| Postmenopausal | 15 (4.07%) | 1 (2.22%) | 14 (4.33%) |
| Endometrial thickening | 41 (11.14%) | 7 (15.55%) | 34 (10.52%) |
| Hypertrophy | 17 (4.61%) | 0 (0.00%) | 17 (5.26%) |
| Hyperplasia | 24 (6.52%) | 7 (15.55%) | 17 (5.26%) |
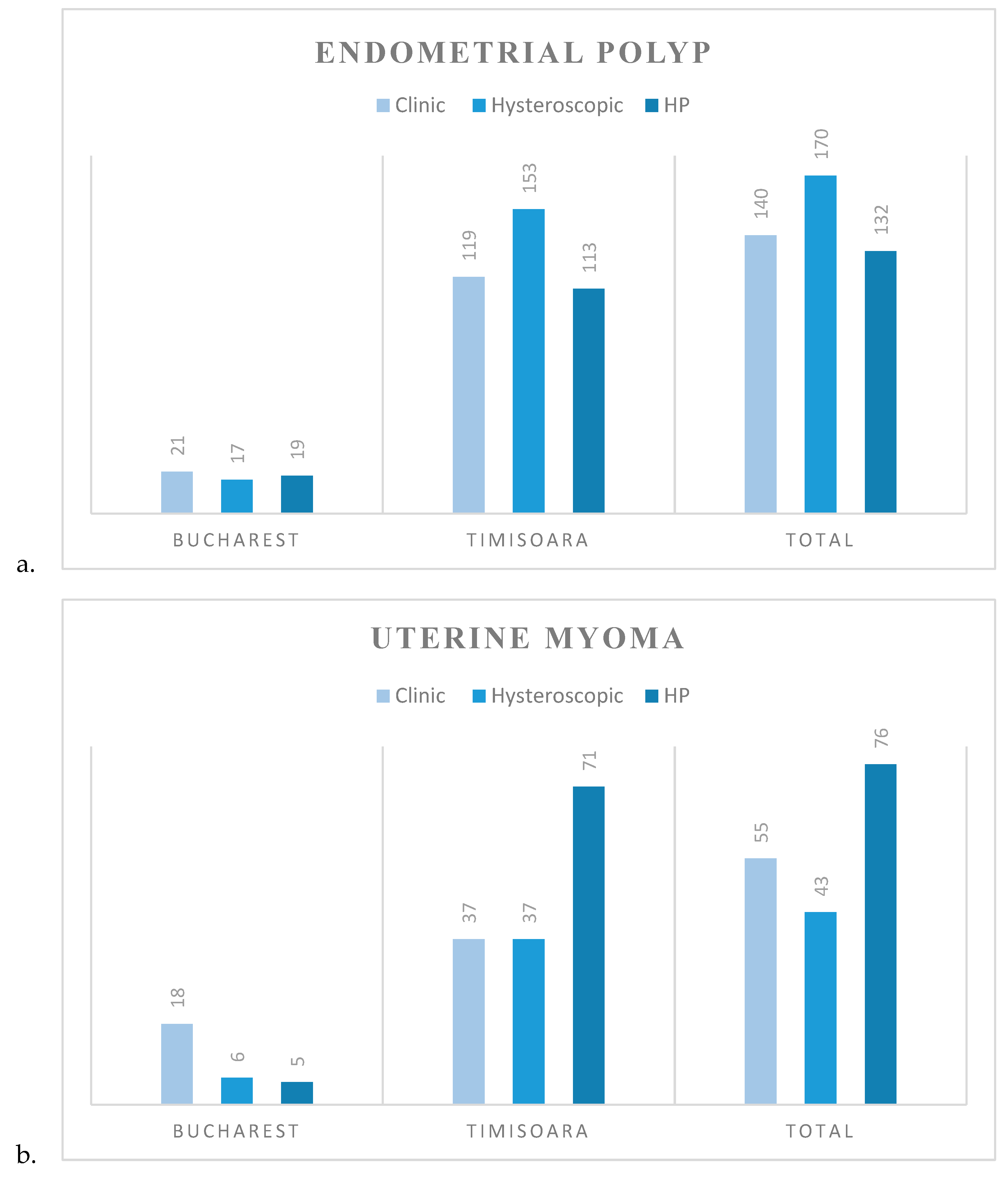
| Uterine myoma | 55 (14.94%) | 18 (40.00%) | 37 (11.45%) |
| Intracavitary | 19 (5.16%) | 1 (2.22%) | 18 (5.57%) |
| Chronic pelvic pain | 11 (2.98%) | 3 (6.66%) | 8 (2.47%) |
| Adenomyosis | 6 (1.63%) | 2 (4.44%) | 4 (1.23%) |
| Infertility | 68 (18.47%) | 7 (15.55%) | 61 (18.88%) |
| primary | 36 (9.78%) | 2 (4.44%) | 34 (10.52%) |
| secondary | 25 (6.79%) | 5 (11.11%) | 20 (6.19%) |
| Uterine septum | 3 (0.81%) | 0 (0.00%) | 3 (0.92%) |
| Polyps | 153 (41.57%) | 25 (55.55%) | 128 (39.62%) |
| Cervical polyp | 12 (3.26%) | 4 (8.88%) | 8 (2.47%) |
| Endometrial polyp | 140 (38.04%) | 21 (46.66%) | 119 (36.84%) |
| Isthmocele | 2 (0.54%) | 0 (0.00%) | 2 (0.61%) |
| Total 1 | Bucharest | Timișoara | |
|---|---|---|---|
| (N = 368) (100%) | (N = 45) (100%) | (N = 323) (100%) | |
| IUD retention 2 | 16 (4.34%) | 0 (0.00%) | 16 (4.95%) |
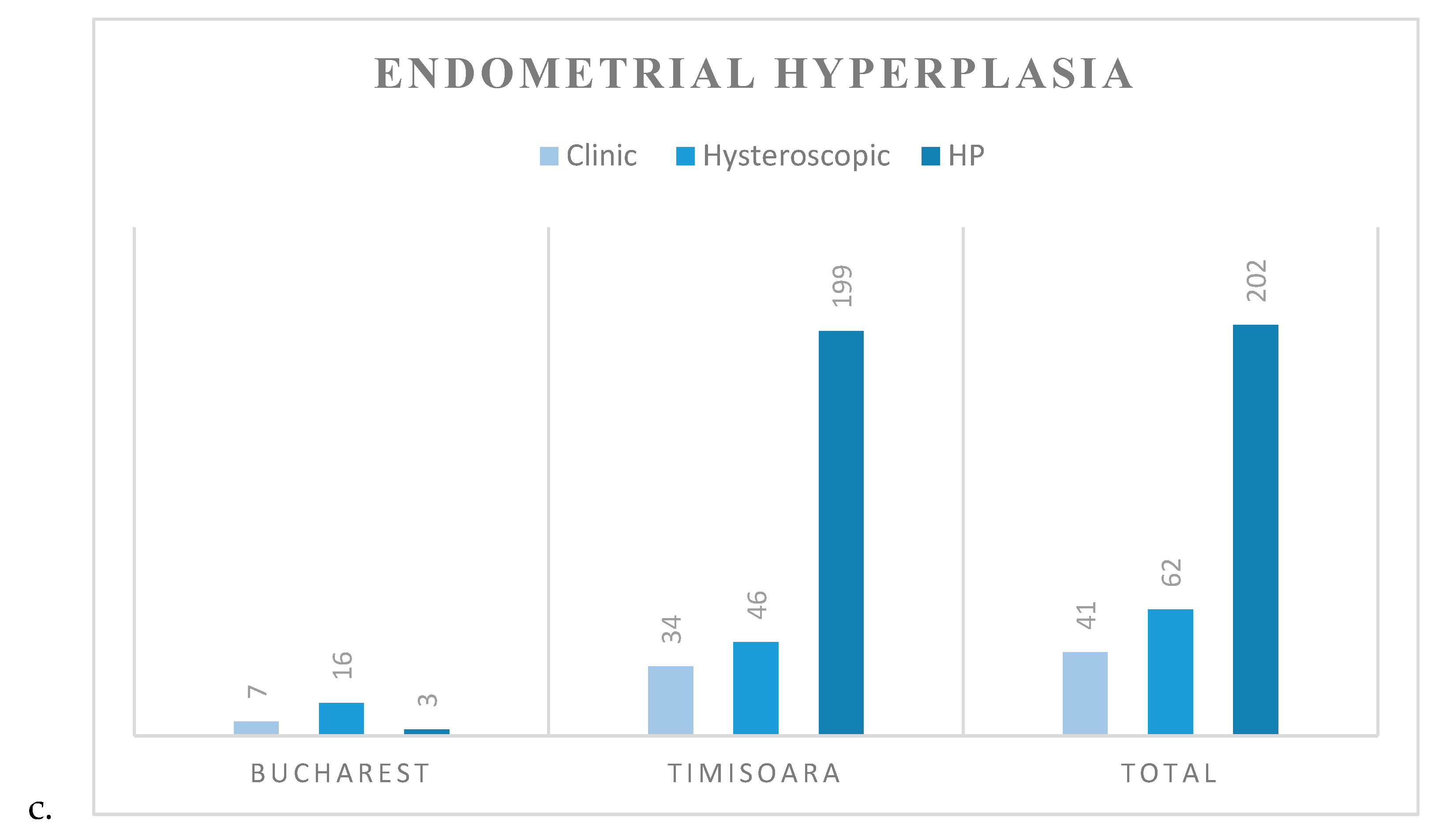
| Endometrial thickening | 63 (17.11%) | 16 (35.55%) | 47 (14.55%) |
| Hypertrophy | 28 (7.60%) | 3 (6.66%) | 25 (7.73%) |
| Hyperplasia | 32 (8.69%) | 11 (24.44%) | 21 (6.50%) |
| Neoplasia | 1 (0.27%) | 0 (0.00%) | 1 (0.30%) |
| Uterine myoma | 43 (11.68%) | 6 (13.33%) | 37 (11.45%) |
| Intracavitary myoma | 19 (5.16%) | 3 (6.66%) | 16 (4.95%) |
| Adenomyosis | 2 (0.54%) | 2 (4.44%) | 0 (0.00%) |
| Uterine septum | 3 (0.81%) | 0 (0.00%) | 3 (0.92%) |
| Synechia | 34 (9.23%) | 0 (0.00%) | 34 (10.52%) |
| Uterine | 26 (7.06%) | 0 (0.00%) | 26 (8.04%) |
| Cervical | 8 (2.17%) | 0 (0.00%) | 8 (2.47%) |
| Polyp | 186 (50.54%) | 21 (46.66%) | 165 (51.08%) |
| Cervical | 16 (4.34%) | 4 (8.88%%) | 12 (3.71%) |
| Endometrial | 170 (46.19%) | 17 (37.77%) | 153 (47.36%) |
| Isthmocele | 1 (0.27%) | 0 (0.00%) | 1 (0.30%) |
| Normal uterine cavity | 34 (9.23%) | 1 (2.22%) | 33 (10.21%) |
| Total 1 | Bucharest | Timișoara | |
|---|---|---|---|
| (N = 368) (100%) | (N = 45) (100%) | (N = 323) (100%) | |
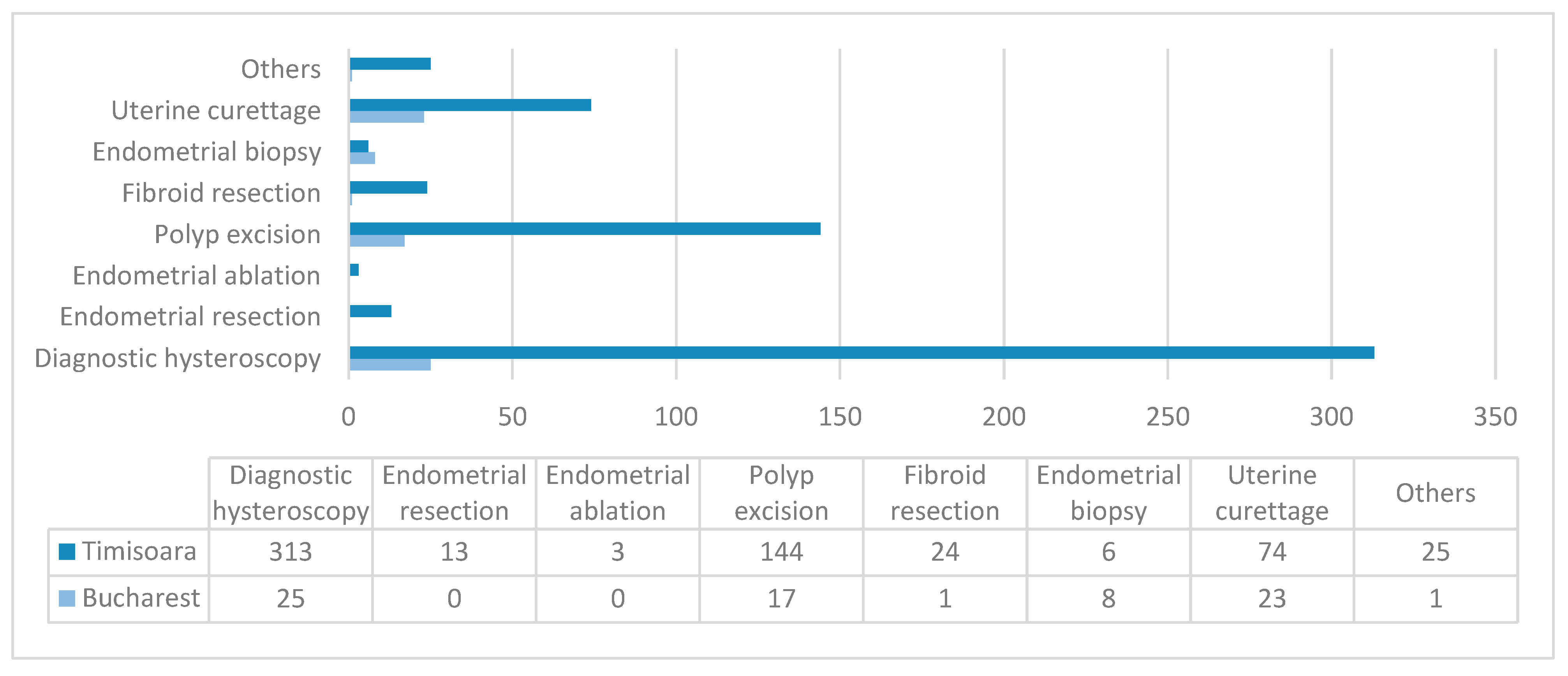
| Diagnostic hysteroscopy | 338 (91.84%) | 25 (55.55%) | 313 (96.90%) |
| Uterine curettage | 97 (26.35%) | 23 (51.11%) | 74 (22.91%) |
| Endometrial biopsy | 14 (3.80%) | 8 (17.77%) | 6 (1.85%) |
| Endometrial resection | 13 (3.53%) | 0 (0.00%) | 13 (4.02%) |
| Endometrial ablation | 3 (0.81%) | 0 (0.00%) | 3 (0.92%) |
| Excision of polyps | 161 (43.75%) | 17 (37.77%) | 144 (44.58%) |
| Fibroid resection | 25 (6.79%) | 1 (2.22%) | 24 (7.43%) |
| Uterine synechia lysis | 7 (1.90%) | 1 (2.22%) | 6 (1.85%) |
| IUD extraction 2 | 16 (4.34%) | 0 (0.00%) | 16 (4.95%) |
| IUD insertion 2 | 2 (0.54%) | 0 (0.00%) | 2 (0.61%) |
| Isthmocele repair | 1 (0.27%) | 0 (0.00%) | 1 (0.30%) |
| Total | Bucharest | Timișoara | |
|---|---|---|---|
| (N = 368) (100%) | (N = 45) (100%) | (N = 323) (100%) | |
| Endometritis | 17 (4.61%) | 10 (22.22%) | 7 (2.16%) |
| Secretory endometrium | 11 (2.98%) | 7 (15.55%) | 4 (1.23%) |
| Proliferative endometrium | 24 (6.52%) | 5 (11.11%) | 19 (5.88%) |
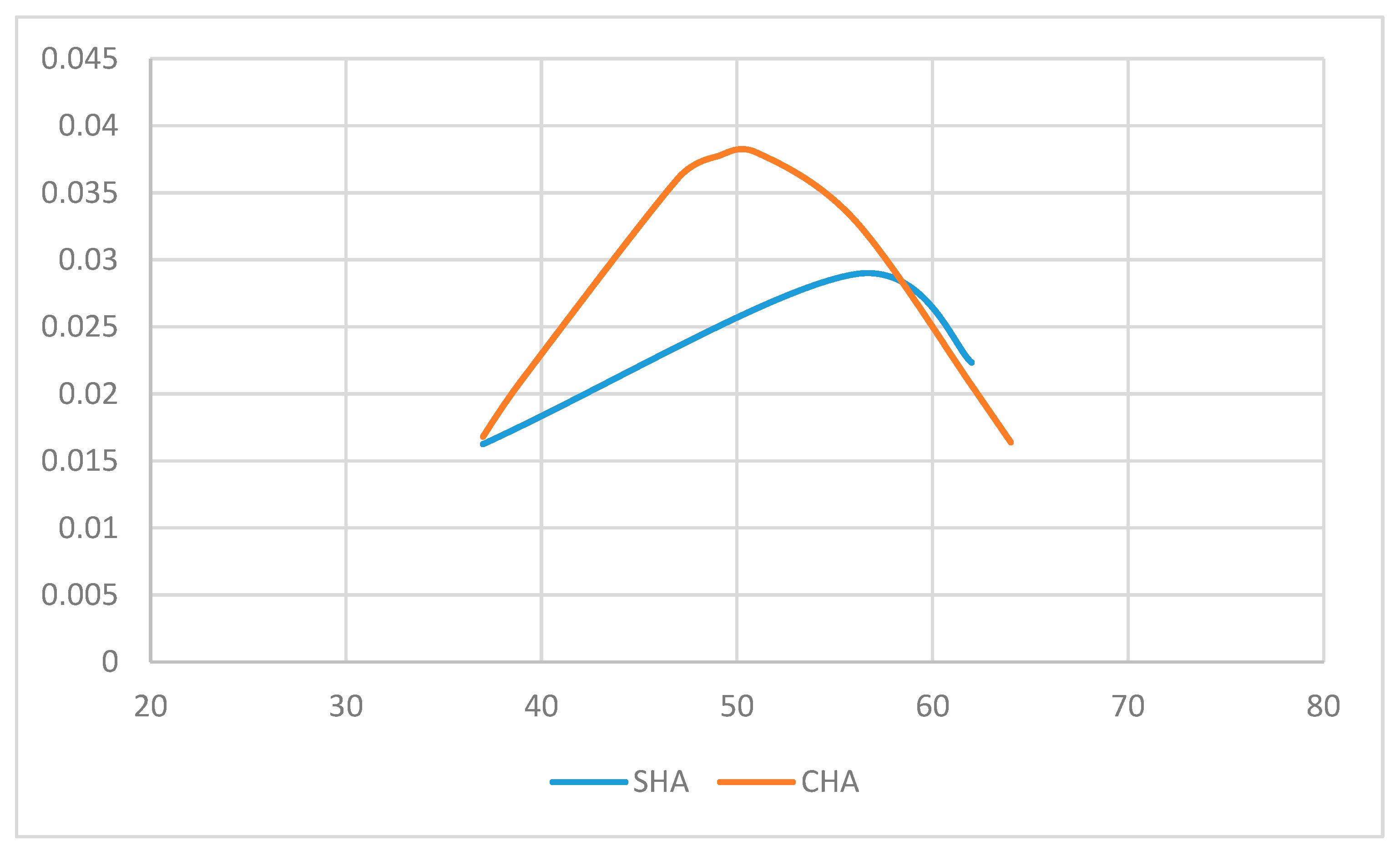
| Simple endometrial hyperplasia | 156 (42.39%) | 3 (6.66%) | 153 (47.36%) |
| without atypia | 49 (13.31%) | 1 (2.22%) | 48 (14.86%) |
| with atypia | 3 (0.81%) | 0 (0.00%) | 3 (0.92%) |
| not specified | 104 (28.26%) | 2 (4.44%) | 102 (31.57%) |
| Complex endometrial hyperplasia | 43 (11.68%) | 0 (0.00%) | 43 (13.31%) |
| without atypia | 12 (3.26%) | 0 (0.00%) | 12 (3.71%) |
| with atypia | 10 (2.71%) | 0 (0.00%) | 10 (3.09%) |
| not specified | 21 (5.70%) | 0 (0.00%) | 21 (6.50%) |
| Cervicitis | 14 (3.80%) | 3 (6.66%) | 11 (3.40%) |
| Polyps | 139 (37.77%) | 21 (46.66%) | 118 (36.53%) |
| Cervical polyp | 7 (1.90%) | 2 (4.44%) | 5 (1.54%) |
| Endometrial polyp | 132 (35.86%) | 19 (42.22%) | 113 (34.98%) |
| Uterine myoma | 76 (20.65%) | 5 (11.11%) | 71 (21.98%) |
| Adenomyosis | 26 (7.06%) | 0 (0.00%) | 26 (8.04%) |
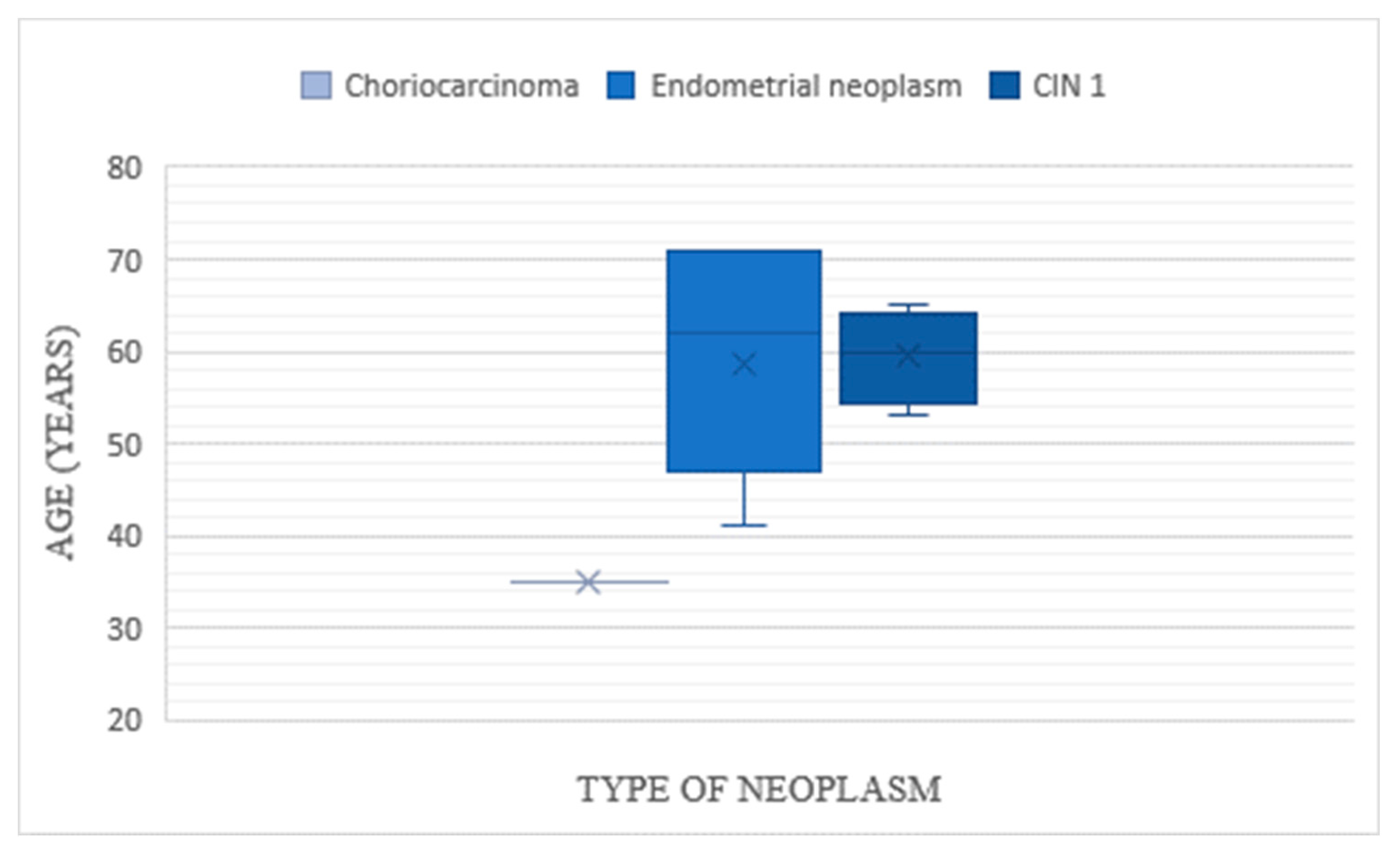
| Endometrial neoplasm | 7 (1.90%) | 1 (2.22%) | 6 (1.85%) |
| Cervical neoplasm | 4 (1.08%) | 0 (0.00%) | 4 (1.23%) |
| Choriocarcinoma | 1 (0.27%) | 0 (0.00%) | 1 (0.30%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matei, A.; Ionescu, C.; Gorun, F.; Gheorghiu, D.; Rosu, G.-A.; Dan, A.; Sima, R.-M.; Furau, C.G.; Ilinca, C.; Navolan, D. Insights on Hysteroscopic Procedures and Their Place in Romanian Gynecologic Practice—The Experience of Two Medical Units. Diagnostics 2020, 10, 281. https://doi.org/10.3390/diagnostics10050281
Matei A, Ionescu C, Gorun F, Gheorghiu D, Rosu G-A, Dan A, Sima R-M, Furau CG, Ilinca C, Navolan D. Insights on Hysteroscopic Procedures and Their Place in Romanian Gynecologic Practice—The Experience of Two Medical Units. Diagnostics. 2020; 10(5):281. https://doi.org/10.3390/diagnostics10050281
Chicago/Turabian StyleMatei, Alexandra, Cringu Ionescu, Florin Gorun, Diana Gheorghiu, George-Alexandru Rosu, Adelina Dan, Romina-Marina Sima, Cristian George Furau, Corina Ilinca, and Dan Navolan. 2020. "Insights on Hysteroscopic Procedures and Their Place in Romanian Gynecologic Practice—The Experience of Two Medical Units" Diagnostics 10, no. 5: 281. https://doi.org/10.3390/diagnostics10050281
APA StyleMatei, A., Ionescu, C., Gorun, F., Gheorghiu, D., Rosu, G.-A., Dan, A., Sima, R.-M., Furau, C. G., Ilinca, C., & Navolan, D. (2020). Insights on Hysteroscopic Procedures and Their Place in Romanian Gynecologic Practice—The Experience of Two Medical Units. Diagnostics, 10(5), 281. https://doi.org/10.3390/diagnostics10050281






