Detection of EGFR Mutations in Plasma Cell-Free Tumor DNA of TKI-Treated Advanced-NSCLC Patients by Three Methodologies: Scorpion-ARMS, PNAClamp, and Digital PCR
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Tissue and Blood Sample Collection and cftDNA Extraction
2.3. Detection of EGFR Mutations in Tumor Tissue
2.4. Detection of EGFR Mutations in Plasma
2.5. Scorpion-ARMS EGFR Plasma RGQ
2.6. PNAClamp EGFR
2.7. QuantStudio 3D Digital PCR
2.8. Statistical Analysis
3. Results
3.1. Patient Characteristics
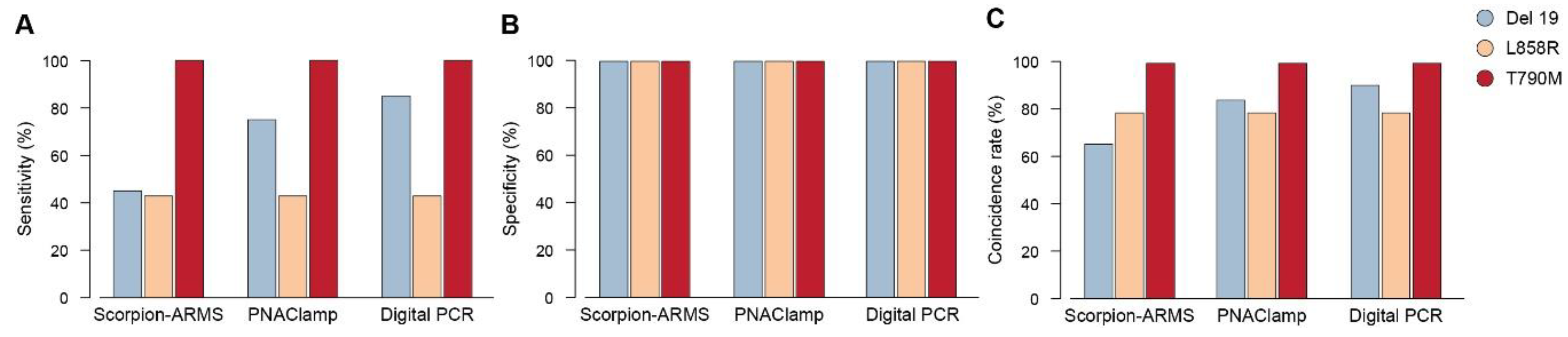
3.2. Sensibility, Specificity and Coincidence Rate of the Three Methods for the Three EGFR Mutations
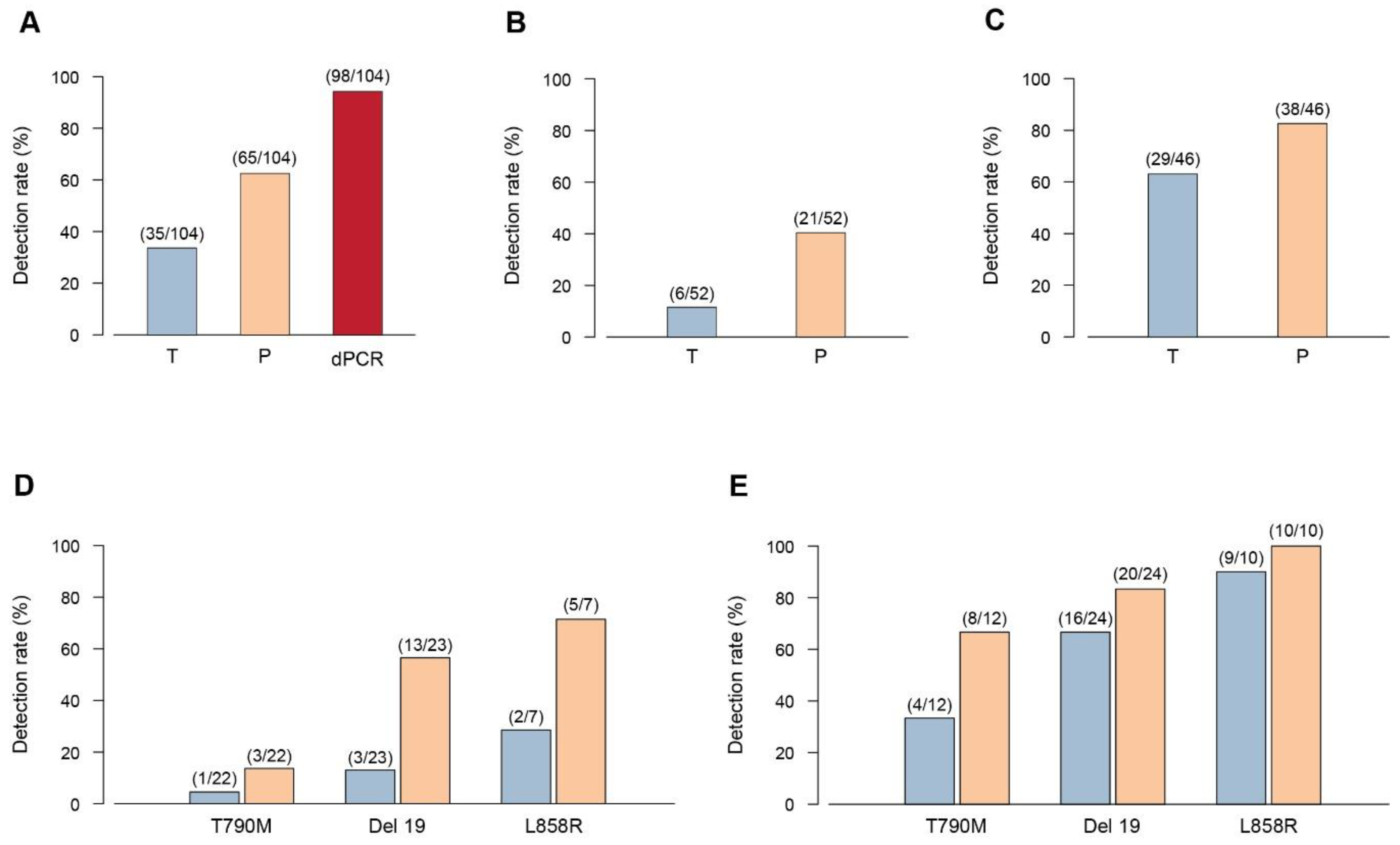
3.3. Comparison of the Three Methodologies in Detecting EGFR Mutations in Plasma versus Tissue
3.4. Limit of Detection of the Three Methods for Three Mutations
3.5. EGFR Mutation Detection Rate in Plasma
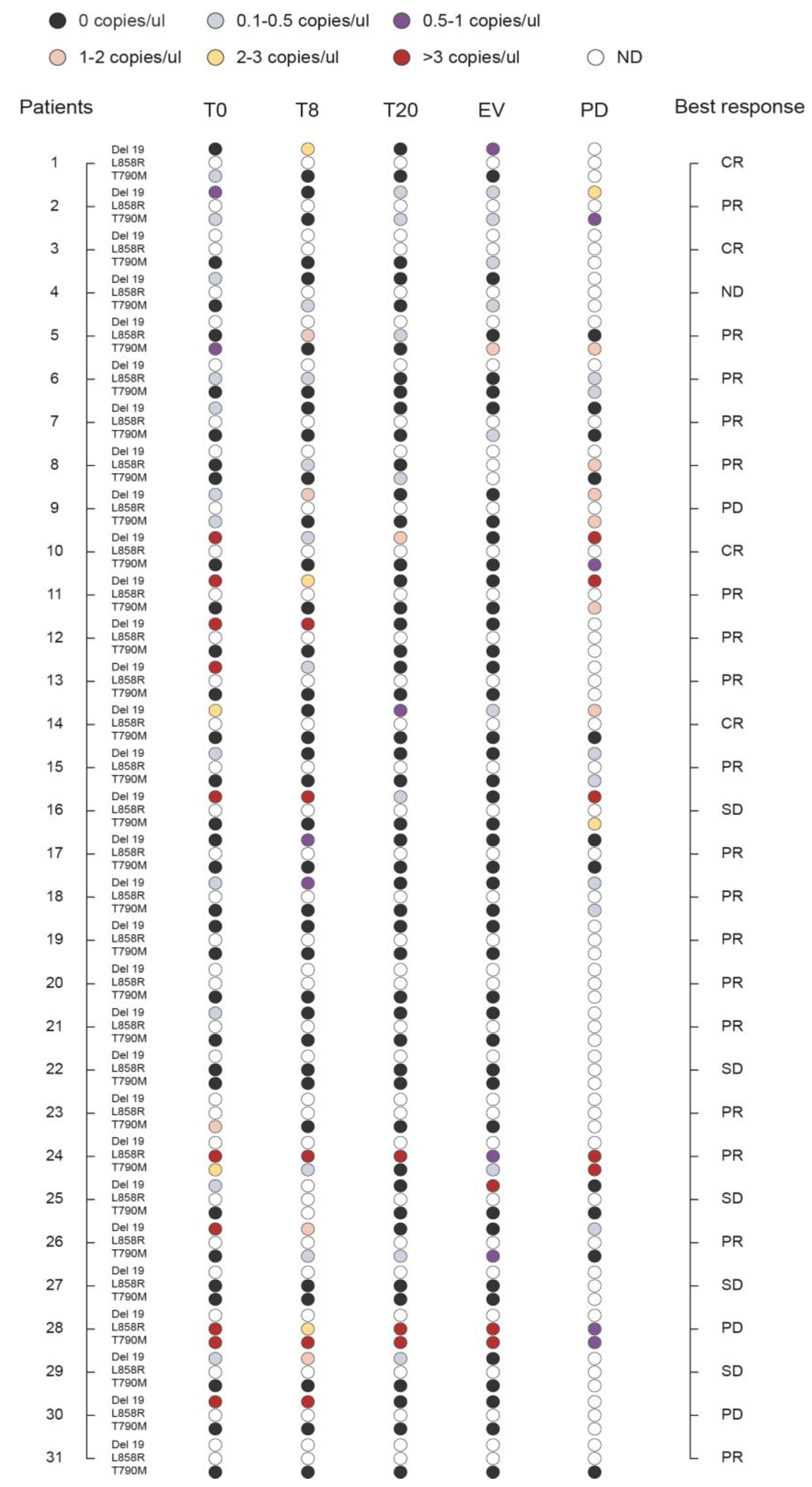
3.6. Monitoring the Plasma Levels of T790M, Del 19, and L858R during Therapy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| EGFR | epidermal growth factor receptor |
| TKIs | tyrosine kinase inhibitors |
| cftDNA | cell-free tumor DNA |
| NSCLC | non-small cell lung cancer |
References
- Lynch, T.J.; Bell, D.W.; Sordella, R.; Gurubhagavatula, S.; Okimoto, R.A.; Brannigan, B.W.; Harris, P.L.; Haserlat, S.M.; Supko, J.G.; Haluska, F.G.; et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 2004, 350, 2129–2139. [Google Scholar] [CrossRef]
- Wang, J.; Ramakrishnan, R.; Tang, Z.; Fan, W.; Kluge, A.; Dowlati, A.; Jones, R.C.; Ma, P.C. Quantifying EGFR Alterations in the Lung Cancer Genome with Nanofluidic Digital PCR Arrays. Clin. Chem. 2010, 56, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Pao, W.; Miller, V.A.; Politi, K.A.; Riely, G.J.; Somwar, R.; Zakowski, M.F.; Kris, M.G.; Varmus, H. Acquired Resistance of Lung Adenocarcinomas to Gefitinib or Erlotinib Is Associated with a Second Mutation in the EGFR Kinase Domain. PLoS Med. 2005, 2, e73. [Google Scholar] [CrossRef] [PubMed]
- Arcila, M.E.; Oxnard, G.R.; Nafa, K.; Riely, G.J.; Solomon, S.B.; Zakowski, M.F.; Kris, M.G.; Pao, W.; Miller, V.A.; Ladanyi, M. Rebiopsy of Lung Cancer Patients with Acquired Resistance to EGFR Inhibitors and Enhanced Detection of the T790M Mutation Using a Locked Nucleic Acid-Based Assay. Clin. Cancer Res. 2011, 17, 1169–1180. [Google Scholar] [CrossRef]
- Sequist, L.V.; Waltman, B.A.; Dias-Santagata, D.; Digumarthy, S.; Turke, A.B.; Fidias, P.; Bergethon, K.; Shaw, A.T.; Gettinger, S.; Cosper, A.K.; et al. Genotypic and Histological Evolution of Lung Cancers Acquiring Resistance to EGFR Inhibitors. Sci. Transl. Med. 2011, 3, 75ra26. [Google Scholar] [CrossRef] [PubMed]
- Rosell, R.; Molina, M.A.; Costa, C.; Simonetti, S.; Gimenez-Capitan, A.; Bertran-Alamillo, J.; Mayo, C.; Moran, T.; Mendez, P.; Cardenal, F.; et al. Pretreatment EGFR T790M Mutation and BRCA1 mRNA Expression in Erlotinib-Treated Advanced Non-Small-Cell Lung Cancer Patients with EGFR Mutations. Clin. Cancer Res. 2011, 17, 1160–1168. [Google Scholar] [CrossRef] [PubMed]
- Su, K.-Y.; Chen, H.-Y.; Li, K.-C.; Kuo, M.-L.; Yang, J.C.-H.; Chan, W.-K.; Ho, B.-C.; Chang, G.-C.; Shih, J.-Y.; Yu, S.-L.; et al. Pretreatment Epidermal Growth Factor Receptor (EGFR) T790M Mutation Predicts Shorter EGFR Tyrosine Kinase Inhibitor Response Duration in Patients With Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2012, 30, 433–440. [Google Scholar] [CrossRef]
- Maheswaran, S.; Sequist, L.V.; Nagrath, S.; Ulkus, L.; Brannigan, B.; Collura, C.V.; Inserra, E.; Diederichs, S.; Iafrate, A.J.; Bell, D.W.; et al. Detection of Mutations inEGFRin Circulating Lung-Cancer Cells. N. Engl. J. Med. 2008, 359, 366–377. [Google Scholar] [CrossRef]
- Jänne, P.A.; Yang, J.C.-H.; Kim, D.-W.; Planchard, D.; Ohe, Y.; Ramalingam, S.S.; Ahn, M.-J.; Kim, S.-W.; Su, W.-C.; Horn, L.; et al. AZD9291 in EGFR Inhibitor–Resistant Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 372, 1689–1699. [Google Scholar] [CrossRef]
- He, Y. Rociletinib in EGFR-Mutated Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 373, 578–579. [Google Scholar] [CrossRef]
- Bintanja, R.; Selten, F.M. Future increases in Arctic precipitation linked to local evaporation and sea-ice retreat. Nat. Cell Biol. 2014, 509, 479–482. [Google Scholar] [CrossRef] [PubMed]
- Weber, B.; Meldgaard, P.; Hager, H.; Wu, L.; Wei, W.; Tsai, J.; Khalil, A.A.; Nexo, E.; Sorensen, B.S. Detection of EGFR mutations in plasma and biopsies from non-small cell lung cancer patients by allele-specific PCR assays. BMC Cancer 2014, 14, 294. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Shen, L.; Zheng, D. Diagnostic value of circulating free DNA for the detection of EGFR mutation status in NSCLC: A systematic review and meta-analysis. Sci. Rep. 2015, 4, srep06269. [Google Scholar] [CrossRef] [PubMed]
- Douillard, J.-Y.; Ostoros, G.; Cobo, M.; Ciuleanu, T.; Cole, R.; McWalter, G.; Walker, J.; Dearden, S.; Webster, A.; Milenkova, T.; et al. Gefitinib Treatment in EGFR Mutated Caucasian NSCLC: Circulating-Free Tumor DNA as a Surrogate for Determination of EGFR Status. J. Thorac. Oncol. 2014, 9, 1345–1353. [Google Scholar] [CrossRef]
- Huang, Z.; Wang, Z.; Bai, H.; Wu, M.; An, T.; Zhao, J.; Yang, L.; Duan, J.; Zhuo, M.; Wang, Y.; et al. The detection of EGFR mutation status in plasma is reproducible and can dynamically predict the efficacy of EGFR-TKI. Thorac. Cancer 2012, 3, 334–340. [Google Scholar] [CrossRef]
- Vallee, A.; Marcq, M.; Bizieux, A.; El Kouri, C.; Lacroix, H.; Bennouna, J.; Douillard, J.-Y.; Denis, M.G. Plasma is a better source of tumor-derived circulating cell-free DNA than serum for the detection of EGFR alterations in lung tumor patients. Lung Cancer 2013, 82, 373–374. [Google Scholar] [CrossRef]
- Minari, R.; Mazzaschi, G.; Bordi, P.; Gnetti, L.; Alberti, G.; Altimari, A.; Gruppioni, E.; Sperandi, F.; Parisi, C.; Guaitoli, G.; et al. Detection of EGFR-Activating and T790M Mutations Using Liquid Biopsy in Patients With EGFR-Mutated Non–Small-Cell Lung Cancer Whose Disease Has Progressed During Treatment With First- and Second-Generation Tyrosine Kinase Inhibitors: A Multicenter Real-Life Retrospective Study. Clin. Lung Cancer 2020, 21, e464–e473. [Google Scholar] [CrossRef]
- Kim, J.-O.; Shin, J.-Y.; Kim, S.R.; Shin, K.S.; Kim, J.; Kim, M.-Y.; Lee, M.-R.; Kim, Y.; Kim, M.; Hong, S.-H.; et al. Evaluation of Two EGFR Mutation Tests on Tumor and Plasma from Patients with Non-Small Cell Lung Cancer. Cancers 2020, 12, 785. [Google Scholar] [CrossRef]
- Li, B.T.; Janku, F.; Jung, B.; Hou, C.; Madwani, K.; Alden, R.; Razavi, P.; Reis-Filho, J.; Shen, R.; Isbell, J.; et al. Ultra-deep next-generation sequencing of plasma cell-free DNA in patients with advanced lung cancers: Results from the Actionable Genome Consortium. Ann. Oncol. 2019, 30, 597–603. [Google Scholar] [CrossRef]
- Crowley, E.H.; Di Nicolantonio, F.; Loupakis, F.; Bardelli, A. Liquid biopsy: Monitoring cancer-genetics in the blood. Nat. Rev. Clin. Oncol. 2013, 10, 472–484. [Google Scholar] [CrossRef]
- Diehl, F.; Li, M.; Dressman, D.; He, Y.; Shen, D.; Szabo, S.; Diaz, L.A.; Goodman, S.N.; David, K.A.; Juhl, H.; et al. Detection and quantification of mutations in the plasma of patients with colorectal tumors. Proc. Natl. Acad. Sci. USA 2005, 102, 16368–16373. [Google Scholar] [CrossRef] [PubMed]
- Holdhoff, M.; Schmidt, K.; Donehower, R.; Diaz, L.A. Analysis of Circulating Tumor DNA to Confirm Somatic KRAS Mutations. J. Natl. Cancer Inst. 2009, 101, 1284–1285. [Google Scholar] [CrossRef]
- Douillard, J.-Y.; Ostoros, G.; Cobo, M.; Ciuleanu, T.; McCormack, R.; Webster, A.R.; Milenkova, T. First-line gefitinib in Caucasian EGFR mutation-positive NSCLC patients: A phase-IV, open-label, single-arm study. Br. J. Cancer 2014, 110, 55–62. [Google Scholar] [CrossRef] [PubMed]
- A Punnoose, E.; Atwal, S.; Liu, W.; Raja, R.; Fine, B.M.; Hughes, B.G.M.; Hicks, R.J.; Hampton, G.M.; Amler, L.C.; Pirzkall, A.; et al. Evaluation of Circulating Tumor Cells and Circulating Tumor DNA in Non-Small Cell Lung Cancer: Association with Clinical Endpoints in a Phase II Clinical Trial of Pertuzumab and Erlotinib. Clin. Cancer Res. 2012, 18, 2391–2401. [Google Scholar] [CrossRef] [PubMed]
- Soria-Comes, T.; Palomar-Abril, V.; Ureste, M.M.; Guerola, M.T.; Maiques, I.C.M. Real-World Data of the Correlation between EGFR Determination by Liquid Biopsy in Non-squamous Non-small Cell Lung Cancer (NSCLC) and the EGFR Profile in Tumor Biopsy. Pathol. Oncol. Res. 2019, 26, 845–851. [Google Scholar] [CrossRef]
- Liu, H.E.; Vuppalapaty, M.; Wilkerson, C.; Renier, C.; Chiu, M.; Lemaire, C.; Che, J.; Matsumoto, M.; Carroll, J.; Crouse, S.; et al. Detection of EGFR Mutations in cfDNA and CTCs, and Comparison to Tumor Tissue in Non-Small-Cell-Lung-Cancer (NSCLC) Patients. Front. Oncol. 2020, 10, 572895. [Google Scholar] [CrossRef]
- Zhang, L.; Xu, F.; Wu, J.; Xue, C.; Zhao, Y.; Jiang, W.; Lin, L.; Wu, X.; Lu, Y.; Bai, H.; et al. Comparison of different methods for detecting epidermal growth factor receptor mutations in peripheral blood and tumor tissue of non-small cell lung cancer as a predictor of response to gefitinib. OncoTargets Ther. 2012, 5, 439–447. [Google Scholar] [CrossRef]
- Taniguchi, K.; Uchida, J.; Nishino, K.; Kumagai, T.; Okuyama, T.; Okami, J.; Higashiyama, M.; Kodama, K.; Imamura, F.; Kato, K. Quantitative Detection of EGFR Mutations in Circulating Tumor DNA Derived from Lung Adenocarcinomas. Clin. Cancer Res. 2011, 17, 7808–7815. [Google Scholar] [CrossRef]
- Forshew, T.; Murtaza, M.; Parkinson, C.; Gale, D.; Tsui, D.W.Y.; Kaper, F.; Dawson, S.-J.; Piskorz, A.M.; Jimenez-Linan, M.; Bentley, D.; et al. Noninvasive Identification and Monitoring of Cancer Mutations by Targeted Deep Sequencing of Plasma DNA. Sci. Transl. Med. 2012, 4, 136ra68. [Google Scholar] [CrossRef]
- Goldstraw, P.; Crowley, J.; Chansky, K.; Giroux, D.J.; Groome, P.A.; Rami-Porta, R.; Postmus, P.E.; Rusch, V.; Sobin, L. The IASLC Lung Cancer Staging Project: Proposals for the Revision of the TNM Stage Groupings in the Forthcoming (Seventh) Edition of the TNM Classification of Malignant Tumours. J. Thorac. Oncol. 2007, 2, 706–714. [Google Scholar] [CrossRef]
- Lindeman, N.I.; Cagle, P.T.; Aisner, D.L.; Arcila, M.E.; Beasley, M.B.; Bernicker, E.H.; Colasacco, C.; Dacic, S.; Hirsch, F.R.; Kerr, K.; et al. Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors: Guideline From the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. Arch. Pathol. Lab. Med. 2018, 142, 321–346. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Kang, X.; You, X.; Dai, L.; Tian, D.; Yan, W.; Yang, Y.; Xiong, H.; Liang, Z.; Zhao, G.Q.; et al. Cross-Platform Comparison of Four Leading Technologies for Detecting EGFR Mutations in Circulating Tumor DNA from Non-Small Cell Lung Carcinoma Patient Plasma. Theranostics 2017, 7, 1437–1446. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhou, C. Comparison of cross-platform technologies for EGFR T790M testing in patients with non-small cell lung cancer. Oncotarget 2017, 8, 100801–100818. [Google Scholar] [CrossRef]
- Thress, K.S.; Brant, R.; Carr, T.H.; Dearden, S.; Jenkins, S.; Brown, H.; Hammett, T.; Cantarini, M.; Barrett, J.C. EGFR mutation detection in ctDNA from NSCLC patient plasma: A cross-platform comparison of leading technologies to support the clinical development of AZD9291. Lung Cancer 2015, 90, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Feng, W.-N.; Gu, W.-Q.; Zhao, N.; Pan, Y.-M.; Luo, W.; Zhang, H.; Liang, J.-M.; Yang, J.; Deng, Y. Comparison of the SuperARMS and Droplet Digital PCR for Detecting EGFR Mutation in ctDNA From NSCLC Patients. Transl. Oncol. 2018, 11, 542–545. [Google Scholar] [CrossRef]
- Zhang, X.; Chang, N.; Yang, G.; Zhang, Y.; Ye, M.; Cao, J.; Xiong, J.; Han, Z.; Wu, S.; Shang, L.; et al. A comparison of ARMS-Plus and droplet digital PCR for detecting EGFR activating mutations in plasma. Oncotarget 2017, 8, 112014–112023. [Google Scholar] [CrossRef]
- Wang, W.; Song, Z.; Zhang, Y. A Comparison of ddPCR and ARMS for detecting EGFR T790M status in ctDNA from advanced NSCLC patients with acquired EGFR-TKI resistance. Cancer Med. 2016, 6, 154–162. [Google Scholar] [CrossRef]
- Wang, L.; Guo, Q.; Yu, W.; Qiao, L.; Zhao, M.; Zhang, C.; Hu, X.; Yang, G.; Xiong, L.; Lou, J. Quantification of plasma EGFR mutations in patients with lung cancers: Comparison of the performance of ARMS-Plus and droplet digital PCR. Lung Cancer 2017, 114, 31–37. [Google Scholar] [CrossRef]
- Duan, H.; Lu, J.; Lu, T.; Gao, J.; Zhang, J.; Xu, Y.; Wang, M.; Wu, H.; Liang, Z.; Liu, T. Comparison of EGFR mutation status between plasma and tumor tissue in non-small cell lung cancer using the Scorpion ARMS method and the possible prognostic significance of plasma EGFR mutation status. Int. J. Clin. Exp. Pathol. 2015, 8, 13136–13145. Available online: http://www.ncbi.nlm.nih.gov/pubmed/26722512 (accessed on 22 January 2019).
- Goto, K.; Ichinose, Y.; Ohe, Y.; Yamamoto, N.; Negoro, S.; Nishio, K.; Itoh, Y.; Jiang, H.; Duffield, E.; McCormack, R.; et al. Epidermal Growth Factor Receptor Mutation Status in Circulating Free DNA in Serum: From IPASS, a Phase III Study of Gefitinib or Carboplatin/Paclitaxel in Non-small Cell Lung Cancer. J. Thorac. Oncol. 2012, 7, 115–121. [Google Scholar] [CrossRef]
- Pasquale, R.; Fenizia, F.; Abate, R.E.; Sacco, A.; Esposito, C.; Forgione, L.; Rachiglio, A.M.; Bevilacqua, S.; Montanino, A.; Franco, R.; et al. Assessment of high-sensitive methods for the detection of EGFR mutations in circulating free tumor DNA from NSCLC patients. Pharmacogenomics 2015, 16, 1135–1148. [Google Scholar] [CrossRef] [PubMed]
- Bai, H.; Mao, L.; Wang, H.S.; Zhao, J.; Yang, L.; An, T.T.; Wang, X.; Duan, C.J.; Wu, N.M.; Guo, Z.Q.; et al. Epidermal Growth Factor Receptor Mutations in Plasma DNA Samples Predict Tumor Response in Chinese Patients With Stages IIIB to IV Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2009, 27, 2653–2659. [Google Scholar] [CrossRef]
- Zhu, G.; Ye, X.; Dong, Z.; Lu, Y.C.; Sun, Y.; Liu, Y.; McCormack, R.; Guanshan, Z.; Liu, X. Highly Sensitive Droplet Digital PCR Method for Detection of EGFR-Activating Mutations in Plasma Cell–Free DNA from Patients with Advanced Non–Small Cell Lung Cancer. J. Mol. Diagn. 2015, 17, 265–272. [Google Scholar] [CrossRef]
- Feng, Q.; Gai, F.; Sang, Y.; Zhang, J.; Wang, P.; Wang, Y.; Liu, B.; Lin, N.; Yu, Y.; Fang, J. A comparison of QuantStudio™ 3D Digital PCR and ARMS-PCR for measuring plasma EGFR T790M mutations of NSCLC patients. Cancer Manag. Res. 2018, 10, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-L.; Tsuboi, M.; He, J.; John, T.; Grohe, C.; Majem, M.; Goldman, J.W.; Laktionov, K.; Kim, S.-W.; Kato, T.; et al. Osimertinib in Resected EGFR-Mutated Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2020, 383, 1711–1723. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Patients | |
|---|---|---|
| n = 31 | % | |
| Median Age, Years (range) | 68 (38–88) | |
| Sex | ||
| Female | 23 | 74.2 |
| Male | 8 | 25.8 |
| Performance Status | ||
| 0 | 19 | 61.3 |
| 1 | 10 | 32.3 |
| 2 | 2 | 6.4 |
| Smoking History | ||
| Never smoker | 20 | 64.5 |
| Former | 3 | 9.7 |
| Smoker | 8 | 25.8 |
| Histology | ||
| Adenocarcinoma | 28 | 90.4 |
| Squamous-cell carcinoma | 1 | 3.2 |
| Adenosquamous | 1 | 3.2 |
| NSCLC | 1 | 3.2 |
| Stage | ||
| IIIA R2 | 1 | 3.2 |
| IIIB | 1 | 3.2 |
| IV | 29 | 93.6 |
| EGFR mutations (tissue) | ||
| L858R | 6 | 19.4 |
| L858R+T790M | 1 | 3.2 |
| Del 19 | 20 | 64.5 |
| Other | 4 | 12.9 |
| EGFR-TKI | ||
| Gefitinib | 11 | 35.5 |
| Erlotinib | 4 | 12.9 |
| Afatinib | 16 | 51.6 |
| Progression | ||
| Yes | 26 | 83.8 |
| No | 5 | 16.2 |
| Exitus | ||
| Alive | 10 | 32.3 |
| Dead | 21 | 67.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siggillino, A.; Ulivi, P.; Pasini, L.; Reda, M.S.; Chiadini, E.; Tofanetti, F.R.; Baglivo, S.; Metro, G.; Crinó, L.; Delmonte, A.; et al. Detection of EGFR Mutations in Plasma Cell-Free Tumor DNA of TKI-Treated Advanced-NSCLC Patients by Three Methodologies: Scorpion-ARMS, PNAClamp, and Digital PCR. Diagnostics 2020, 10, 1062. https://doi.org/10.3390/diagnostics10121062
Siggillino A, Ulivi P, Pasini L, Reda MS, Chiadini E, Tofanetti FR, Baglivo S, Metro G, Crinó L, Delmonte A, et al. Detection of EGFR Mutations in Plasma Cell-Free Tumor DNA of TKI-Treated Advanced-NSCLC Patients by Three Methodologies: Scorpion-ARMS, PNAClamp, and Digital PCR. Diagnostics. 2020; 10(12):1062. https://doi.org/10.3390/diagnostics10121062
Chicago/Turabian StyleSiggillino, Annamaria, Paola Ulivi, Luigi Pasini, Maria Sole Reda, Elisa Chiadini, Francesca Romana Tofanetti, Sara Baglivo, Giulio Metro, Lucio Crinó, Angelo Delmonte, and et al. 2020. "Detection of EGFR Mutations in Plasma Cell-Free Tumor DNA of TKI-Treated Advanced-NSCLC Patients by Three Methodologies: Scorpion-ARMS, PNAClamp, and Digital PCR" Diagnostics 10, no. 12: 1062. https://doi.org/10.3390/diagnostics10121062
APA StyleSiggillino, A., Ulivi, P., Pasini, L., Reda, M. S., Chiadini, E., Tofanetti, F. R., Baglivo, S., Metro, G., Crinó, L., Delmonte, A., Minotti, V., Roila, F., & Ludovini, V. (2020). Detection of EGFR Mutations in Plasma Cell-Free Tumor DNA of TKI-Treated Advanced-NSCLC Patients by Three Methodologies: Scorpion-ARMS, PNAClamp, and Digital PCR. Diagnostics, 10(12), 1062. https://doi.org/10.3390/diagnostics10121062







