A Novel and Simple Exercise Test Parameter to Assess Responsiveness to Cardiac Resynchronization Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Strategy Implantation
2.2. ECG Evaluation
2.3. Transthoracic Echocardiography (TTE)
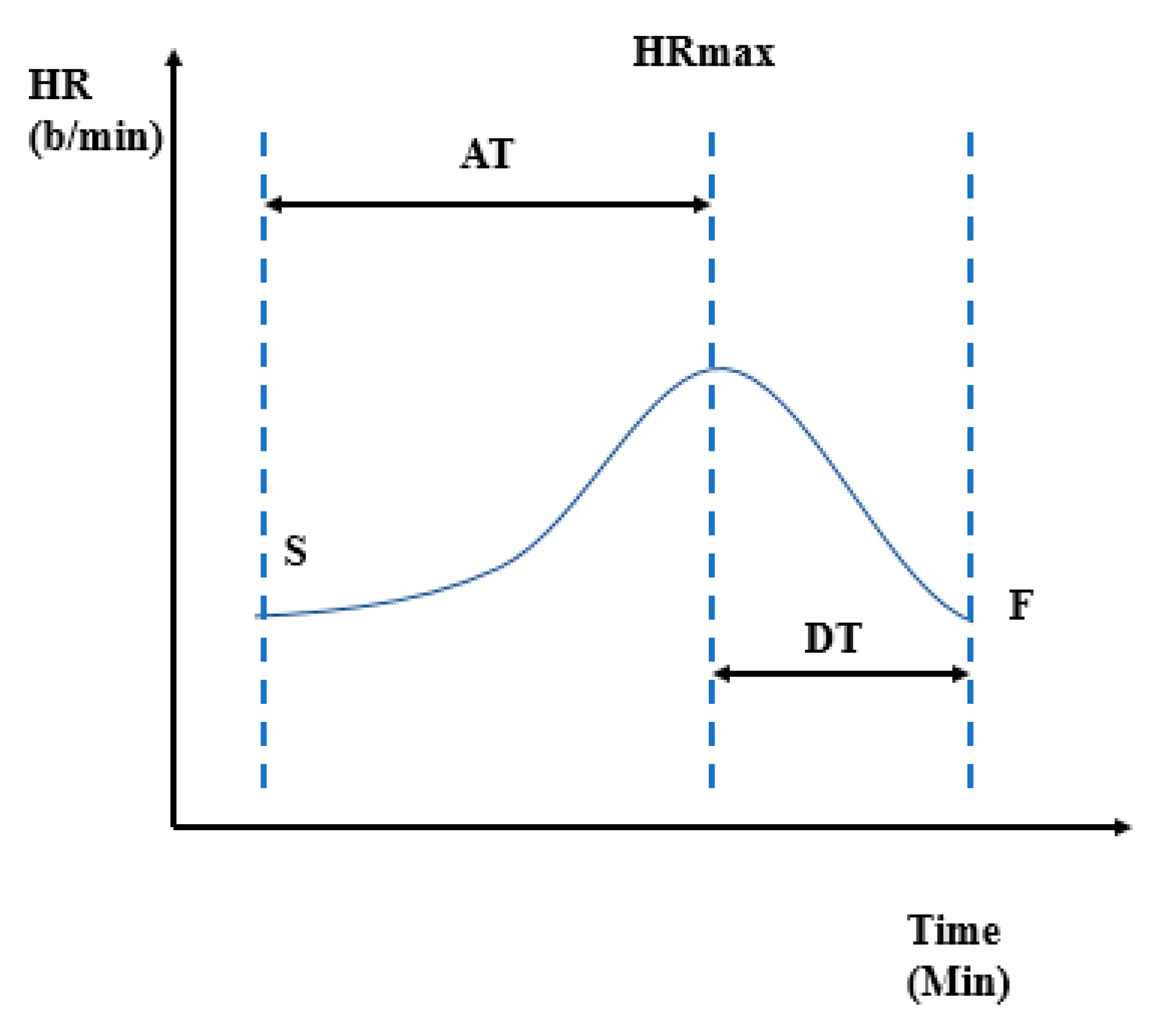
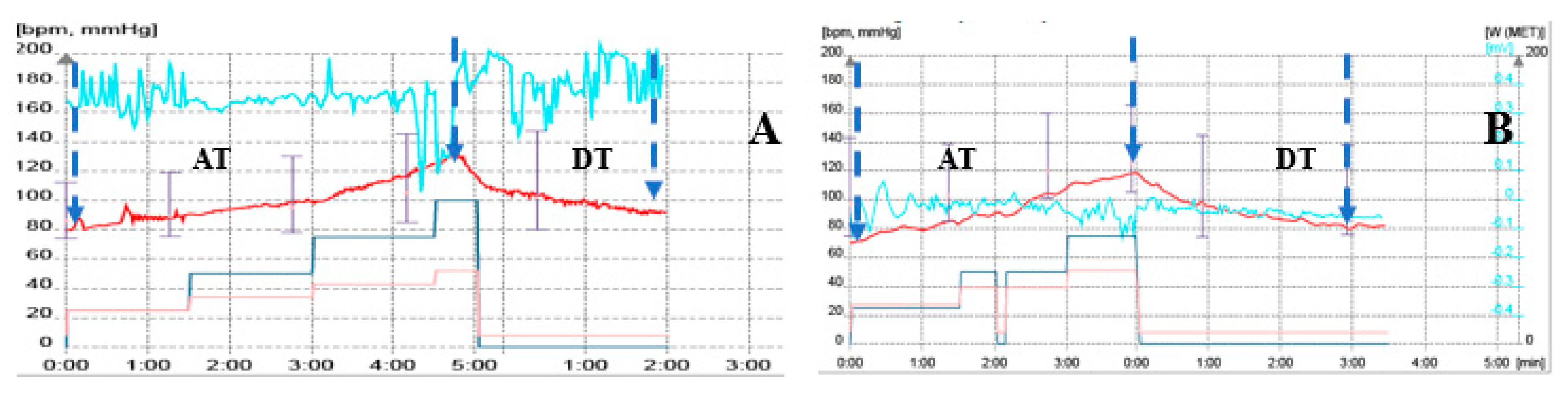
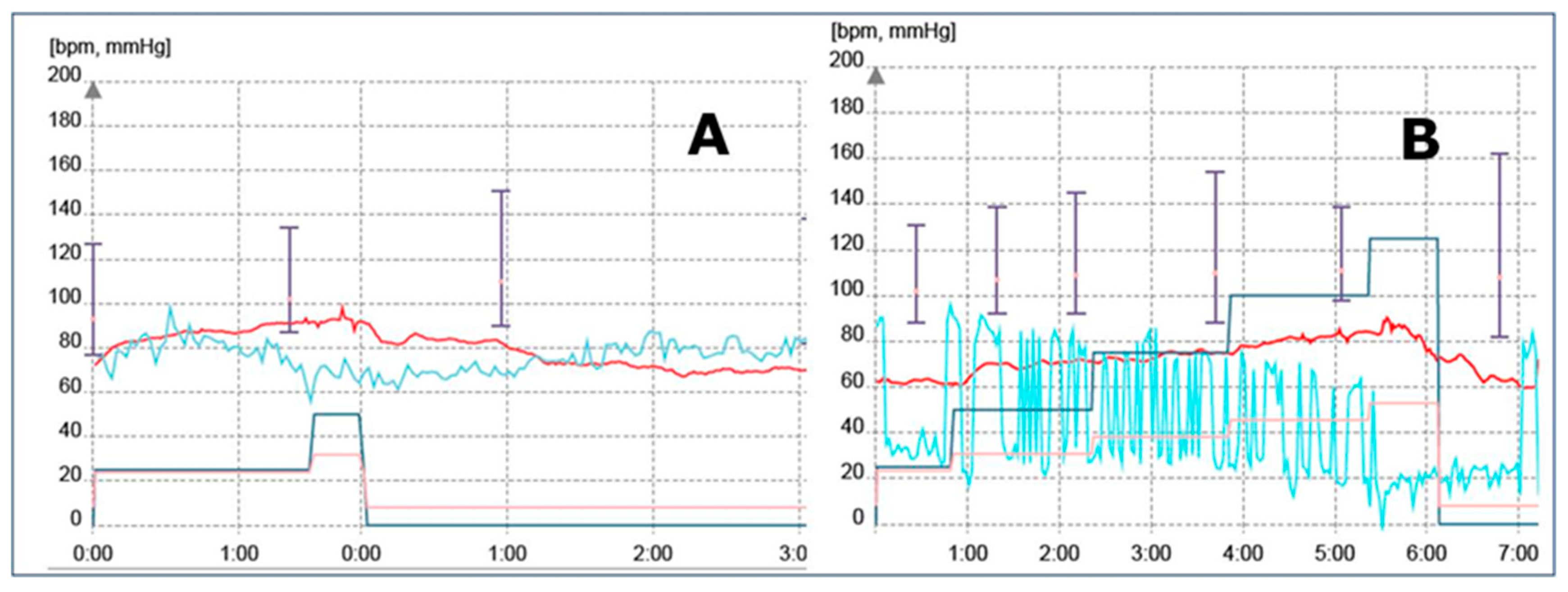
2.4. Exercise Test (ET)
2.5. Device Programming
2.6. Response to CRT
- -
- Clinical response to CRT, defined as improvement in NYHA functional class, ET duration, and workload.
- -
- Echocardiographic response (defined as >5% increase in LVEF, 15% decrease in LV end-systolic/diastolic volume, and decreased mitral regurgitation degree).
- -
- Assessment of outcomes: number of hospitalizations due to worsening heart failure, all-cause mortality, and morbidity.
2.7. Statistical Analysis
3. Results
3.1. Baseline Demographic Data
3.2. Results: ECG and Echocardiography
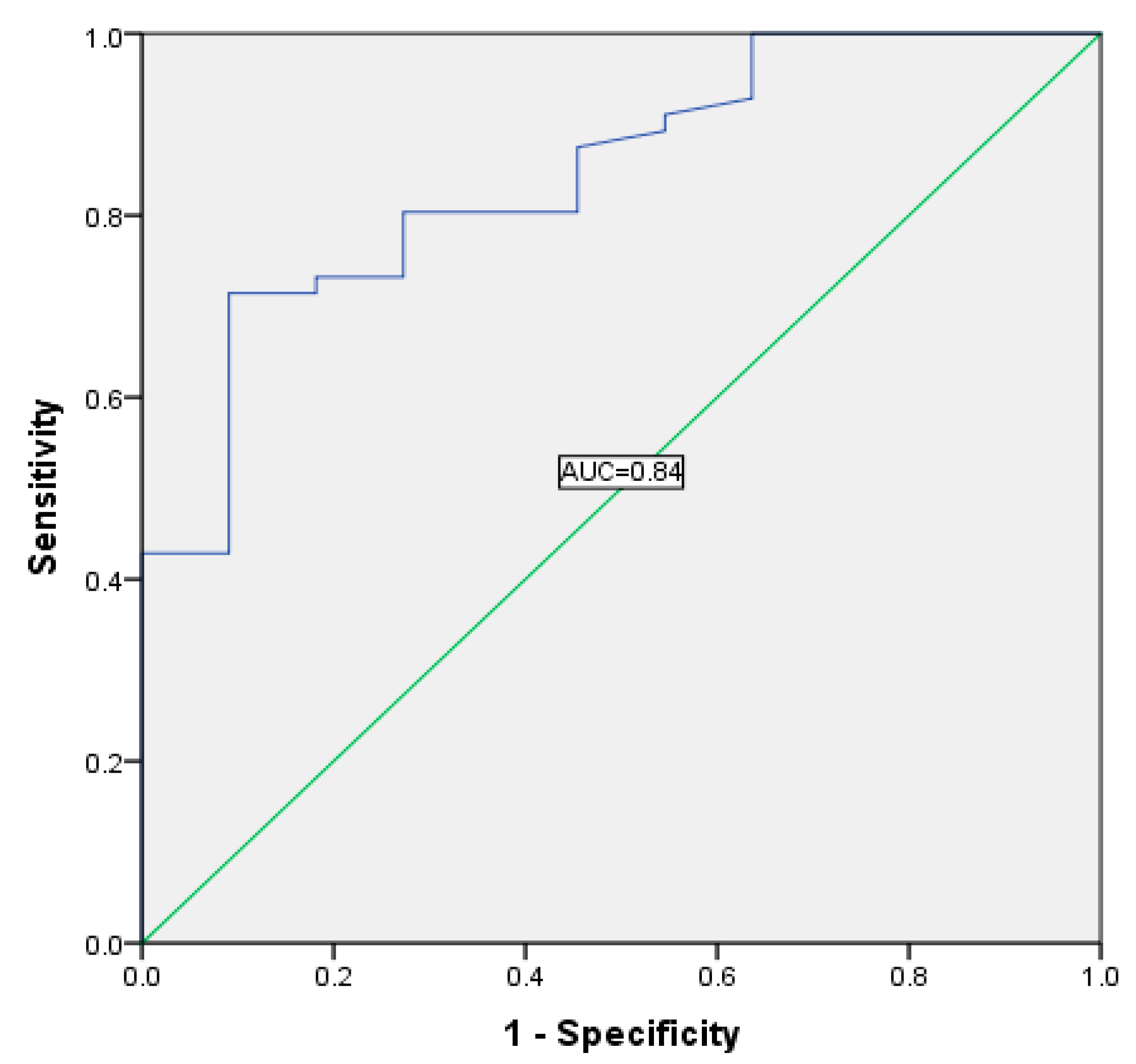
3.3. Exercise Test Results
3.4. Device Programming
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Daubert, J.-C.; Behar, N.; Martins, R.P.; Mabo, P.; Leclercq, C. Avoiding non-responders to cardiac resynchronization therapy: A practical guide. Eur. Heart J. 2016, 38, 1463–1472. [Google Scholar] [CrossRef] [PubMed]
- Vacarescu, C.; Cozma, A.; Petrescu, L.; Dragan, S.; Mornos, C.; Crisan, S.; Feier, H.; Lazar, M.-A.; Cozlac, R.A.; Luca, C.T. Exercise test is essential in LV-only fusion CRT pacing without right ventricle lead. Clin. Interv. Aging 2019, 14, 969–975. [Google Scholar] [CrossRef] [PubMed]
- De Riva-Silva, M.; Lopez-Gil, M.; Fontenla, A.; Salgado-Aranda, R.; Salguero-Bodes, R.; Arribas-Ynsaurriaga, F. Usefulness of Exercise Test in Cardiac Resynchronization Therapy Follow-up. Revista Española de Cardiología (Engl. Ed.) 2013, 66, 912–913. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.-D.; Dewland, T.A.; Wencker, D.; Katz, S. Post-Exercise Heart Rate Recovery Independently Predicts Mortality Risk in Patients with Chronic Heart Failure. J. Card. Fail. 2009, 15, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Snader, C.E.; Lauer, M.S. Heart-Rate Recovery Immediately after Exercise as a Predictor of Mortality. N. Engl. J. Med. 1999, 341, 1351–1357. [Google Scholar] [CrossRef]
- Cole, C.R.; Foody, J.M.; Blackstone, E.H.; Lauer, M.S. Heart rate recovery after submaximal exercise testing as a predictor of mortality in a cardiovascularly healthy cohort. Ann. Intern. Med. 2000, 132, 552–555. [Google Scholar] [CrossRef]
- Nishime, E.O.; Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Lauer, M.S. Heart Rate Recovery and Treadmill Exercise Score as Predictors of Mortality in Patients Referred for Exercise ECG. JAMA 2000, 284, 1392–1398. [Google Scholar] [CrossRef]
- Gibbons, R.J. Abnormal heart-rate recovery after exercise. Lancet 2002, 359, 1536–1537. [Google Scholar] [CrossRef]
- Watanabe, J.; Thamilarasan, M.; Blackstone, E.H.; Thomas, J.D.; Lauer, M.S. Heart rate recovery immediately after treadmill exercise and left ventricular systolic dysfunction as predictors of mortality: The case of stress echocardiography. Circulation 2001, 104, 1911–1916. [Google Scholar] [CrossRef]
- Pitsavos, C.H.; Chrysohoou, C.; Panagiotakos, D.B.; Kokkinos, P.; Skoumas, J.; Papaioannou, I.; Michaelides, A.P.; Singh, S.; Stefanadis, C.I. Exercise capacity and heart rate as predictor of coronary heart disease events in patients with heterozygous familial hypercholesterolemia. Atherosclerosis 2004, 173, 347–352. [Google Scholar] [CrossRef]
- Cheng, Y.J.; Lauer, M.S.; Earnest, C.P.; Church, T.S.; Kampert, J.B.; Gibbons, L.W.; Blair, S.N. Heart Rate Recovery Following Maximal Exercise Testing as a Predictor of Cardiovascular Disease and All-Cause Mortality in Men with Diabetes. Diabetes Care 2003, 26, 2052–2057. [Google Scholar] [CrossRef]
- Imai, K.; Sato, H.; Hori, M.; Kusuoka, H.; Ozaki, H.; Yokoyama, H.; Takeda, H.; Inoue, M.; Kamada, T. Vagally mediated heart rate recovery after exercise is accelerated in athletes but blunted in patients with chronic heart failure. J. Am. Coll. Cardiol. 1994, 24, 1529–1535. [Google Scholar] [CrossRef]
- Daubert, J.-C.; Saxon, L.; Adamson, P.B.; Auricchio, A.; Berger, R.D.; Beshai, J.F.; Breithard, O.; Brignole, M.; Cleland, J.; De Lurgio, D.B.; et al. 2012 EHRA/HRS expert consensus statement on cardiac resynchronization therapy in heart failure: Implant and follow-up recommendations and management. Heart Rhythm. 2012, 9, 1524–1576. [Google Scholar] [CrossRef]
- Abraham, W.T.; Fisher, W.G.; Smith, A.L.; Delurgio, D.B.; Leon, A.R.; Loh, E.; Kocovic, D.Z.; Packer, M.; Clavell, A.L.; Hayes, D.L.; et al. Cardiac Resynchronization in Chronic Heart Failure. N. Engl. J. Med. 2002, 346, 1845–1853. [Google Scholar] [CrossRef]
- Crișan, S.; Petrescu, L.; Lazăr, M.A.; Vacarescu, C.; Nicola, A.-R.; Cozma, A.; Mornos, C.; Luca, C.T. Reduced ejection fraction heart failure—New data from multicenter studies and national registries regarding general and elderly populations: Hopes and disappointments. Clin. Interv. Aging 2018, 13, 651–656. [Google Scholar] [CrossRef]
- Cleland, J.G.; Daubert, J.C.; Erdmann, E.; Freemantle, N.; Gras, D.; Kappenberger, L.; Tavazzi, L. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 2005, 352, 1539–1549. [Google Scholar] [CrossRef] [PubMed]
- van de Vegte, Y.J.; van der Harst, P.; Verweij, N. Heart rate recovery 10 s after cessation of exercise predicts death. J. Am. Heart Assoc. 2018, 7, e008341. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.E.; Exton, S.A.; Yousef, Z.R. Heart rate deceleration after exercise predicts patients most likely to respond to cardiac resynchronisation therapy. Heart 2010, 96, 1385–1389. [Google Scholar] [CrossRef] [PubMed]
- Tomaselli, G.F.; Zipes, D.P. What Causes Sudden Death in Heart Failure? Circ. Res. 2004, 95, 754–763. [Google Scholar] [CrossRef]
- Lahiri, M.K.; Kannankeril, P.J.; Goldberger, J.J. Assessment of Autonomic Function in Cardiovascular Disease. J. Am. Coll. Cardiol. 2008, 51, 1725–1733. [Google Scholar] [CrossRef] [PubMed]
- Goldberger, J.J.; Arora, R.; Buckley, U.; Shivkumar, K. Autonomic Nervous System Dysfunction. J. Am. Coll. Cardiol. 2019, 73, 1189–1206. [Google Scholar] [CrossRef]
- Gademan, M.G.J.; Van Bommel, R.J.; Borleffs, C.J.W.; Man, S.; Haest, J.C.W.; Schalij, M.; Van Der Wall, E.E.; Bax, J.J.; Swenne, C. Biventricular pacing-induced acute response in baroreflex sensitivity has predictive value for midterm response to cardiac resynchronization therapy. Am. J. Physiol. Circ. Physiol. 2009, 297, H233–H237. [Google Scholar] [CrossRef][Green Version]
- Mlynarska, A.; Mlynarski, R.; Marcisz, C.; Golba, K.S. Modified frailty as a novel factor in predicting the response to cardiac resynchronization in the elderly population. Clin. Interv. Aging 2019, 14, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Doltra, A.; Bijnens, B.; Tolosana, J.M.; Gabrielli, L.; Ángeles Castel, M.; Berruezo, A.; Brugada, J.; Mont, L.; Sitges, M. Effect of cardiac resynchronization therapy on left ventricular diastolic function: Implications for clinical outcome. J. Card. Fail. 2013, 19, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Młynarska, A.; Mlynarski, R.; Gołba, K. Frailty as a predictor of negative outcomes after cardiac resynchronization therapy. Pacing Clin. Electrophysiol. 2018, 41, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Cozma, D.; Vacarescu, C.; Petrescu, L.; Mornos, C.; Goanta, E.; Feier, H.; Luca, C.T.; Gusetu, G.; Vatasescu, R. CRT pacing: Midterm follow-up in LV only pacing without RV lead in patients with normal AV conduction. J. Clin. Med. 2018, 7, 531. [Google Scholar] [CrossRef]
- Zweerink, A.; Van Der Lingen, A.-L.C.; Handoko, M.L.; Van Rossum, A.C.; Allaart, C.P. Chronotropic Incompetence in Chronic Heart Failure. Circ. Heart Fail. 2018, 11, 004969. [Google Scholar] [CrossRef]
| All Patients (n = 109) | |
|---|---|
| Mean age (years) | 63.32 ± 9.8 |
| Male, n (%) | 74 (68) |
| NYHA functional class n (%) | |
| II | 9 (8) |
| III | 83 (76) |
| IV | 18 (16) |
| Hypertension, n (%) | 85 (77.3) |
| Chronic kidney disease, n (%) * | 61 (56) |
| Diabetes mellitus, n (%) | 40 (36) |
| Dyslipidemia, n (%) | 89 (81.3) |
| Medication, n (%) | |
| ACEI/ARB | 99 (90.7) |
| Beta-blockers | 90 (82.7) |
| Ivabradine | 31 (28) |
| Diuretics | 102 (93.3) |
| Aldosterone receptor antagonists | 89 (81.3) |
| Digoxin | 5 (4) |
| All Patients (n = 109) | Range | ||
|---|---|---|---|
| LVEDD (cm), mean ± SD | 6.44 ± 0.95 | 4.5–8.9 | |
| LVEDV (mL), mean ± SD | 240.32 ± 90.7 | 90–560 | |
| LVESV (mL), mean ± SD | 176.45 ± 72.6 | 43–414 | |
| EF (%), mean ± SD | 26.75 ± 5.8 | 15–40 | |
| LAV (mL), mean ± SD | 120.73 ± 58.7 | 49–440 | |
| Valvular disease, n (%) | Mild | Moderate | Severe |
| Mitral regurgitation | 64 (58.7) | 24 (21.3) | 22 (20) |
| Tricuspid regurgitation | 85 (77.4) | 22 (20) | 3 (2.7) |
| Aortic regurgitation | 24 (21.3) | 2 (1.3) | 0 |
| Aortic stenosis | 3 (2.7) | 0 | 0 |
| Asynchronism parameters | Interventricular asynchronism n (%) | ||
| 50 (46) | |||
| Intraventricular asynchronism n (%) | |||
| 42 (38) | |||
| Septal flash n (%) | |||
| 58 (53) | |||
| Before CRT | After CRT | p-Value | |
|---|---|---|---|
| LVEF (%) | 26 ± 5.8 | 35 ± 8.7 | <0.001 |
| LVESV (mL) | 176 ± 72 | 145 ± 73 | <0.001 |
| LVEDV (mL) | 240 ± 90 | 217 ± 89 | <0.001 |
| LVEDD (cm) | 6.4 ± 0.95 | 6.1 ± 1.1 | <0.001 |
| QRS interval (ms) | 168.89 ± 30.4 | 134.22 ± 20.4 | <0.001 |
| QRS axis (°) | −18 ± 36 | +38 ± 105 | <0.001 |
| Parameter | Responders (n = 98) | Non-Responders (n = 11) | p-Value |
|---|---|---|---|
| METs | 6.43 ± 1.2 | 6.04 ± 1.0 | 0.3 |
| Watt | 111.16 ± 32.6 | 102.27 ± 23.5 | 0.4 |
| Basal HR | 67.55 ± 10.2 | 63.64 ± 7.2 | 0.2 |
| Maximum HR | 100.55 ± 21.8 | 88.90 ± 10.7 | 0.09 |
| AT | 303.66 ± 125.9 | 303.7 ± 96.9 | 0.9 |
| DT | 125.86 ± 77.4 | 241.68 ± 116.6 | <0.001 |
| HRRI = AT/DT | 3.16 ± 2.0 | 1.4 ± 0.5 | 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cozlac, A.-R.; Petrescu, L.; Crisan, S.; Luca, C.T.; Vacarescu, C.; Streian, C.G.; Lazar, M.-A.; Gurgu, A.; Dragomir, A.; Goanta, E.V.; et al. A Novel and Simple Exercise Test Parameter to Assess Responsiveness to Cardiac Resynchronization Therapy. Diagnostics 2020, 10, 920. https://doi.org/10.3390/diagnostics10110920
Cozlac A-R, Petrescu L, Crisan S, Luca CT, Vacarescu C, Streian CG, Lazar M-A, Gurgu A, Dragomir A, Goanta EV, et al. A Novel and Simple Exercise Test Parameter to Assess Responsiveness to Cardiac Resynchronization Therapy. Diagnostics. 2020; 10(11):920. https://doi.org/10.3390/diagnostics10110920
Chicago/Turabian StyleCozlac, Alina-Ramona, Lucian Petrescu, Simina Crisan, Constantin Tudor Luca, Cristina Vacarescu, Caius Glad Streian, Mihai-Andrei Lazar, Andra Gurgu, Angela Dragomir, Emilia Violeta Goanta, and et al. 2020. "A Novel and Simple Exercise Test Parameter to Assess Responsiveness to Cardiac Resynchronization Therapy" Diagnostics 10, no. 11: 920. https://doi.org/10.3390/diagnostics10110920
APA StyleCozlac, A.-R., Petrescu, L., Crisan, S., Luca, C. T., Vacarescu, C., Streian, C. G., Lazar, M.-A., Gurgu, A., Dragomir, A., Goanta, E. V., Vatasescu, R., Chahine, K. M., Rachieru, C., & Cozma, D. (2020). A Novel and Simple Exercise Test Parameter to Assess Responsiveness to Cardiac Resynchronization Therapy. Diagnostics, 10(11), 920. https://doi.org/10.3390/diagnostics10110920






