Endometriosis and the Urinary Tract: From Diagnosis to Surgical Treatment
Abstract
:1. Introduction
2. Epidemiology of UTE
3. Pathogenesis of UTE
4. Bladder Endometriosis
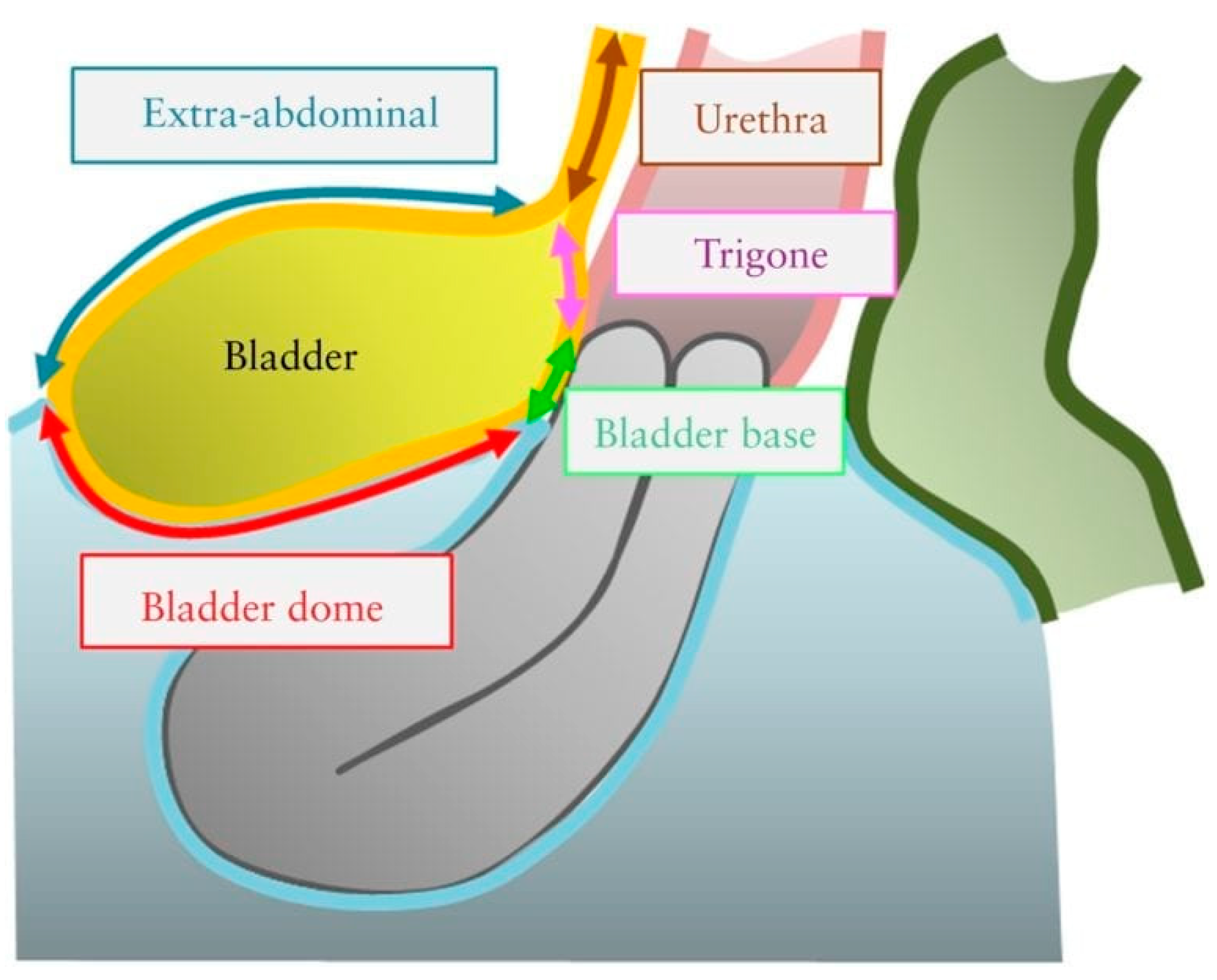
4.1. Definition of Bladder Endometriosis
4.2. Clinical Symptoms of Bladder DE
4.3. Diagnosis of Bladder DE
4.3.1. Medical History and Physical Examination
4.3.2. Laboratory Testing
4.3.3. Imaging Techniques
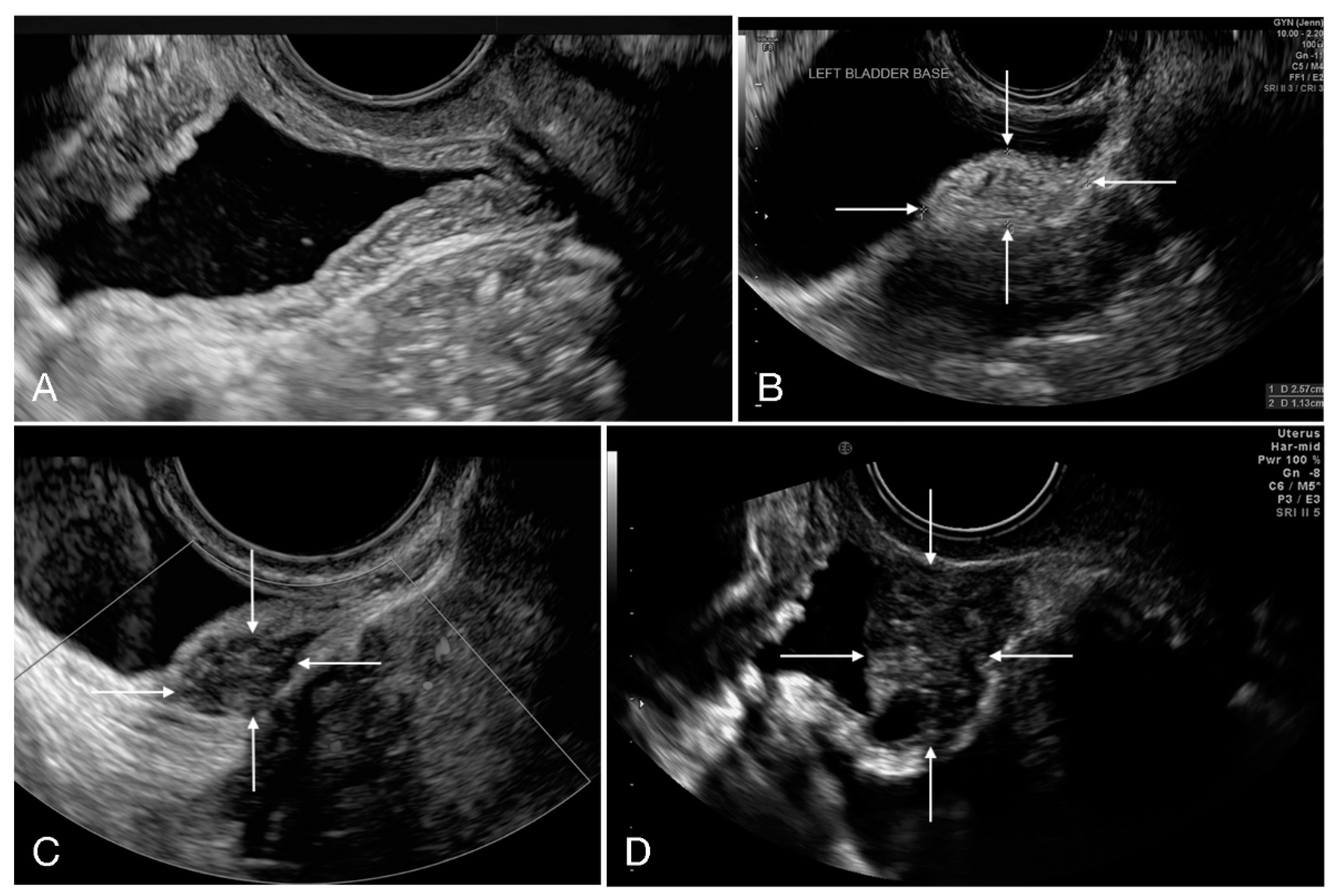
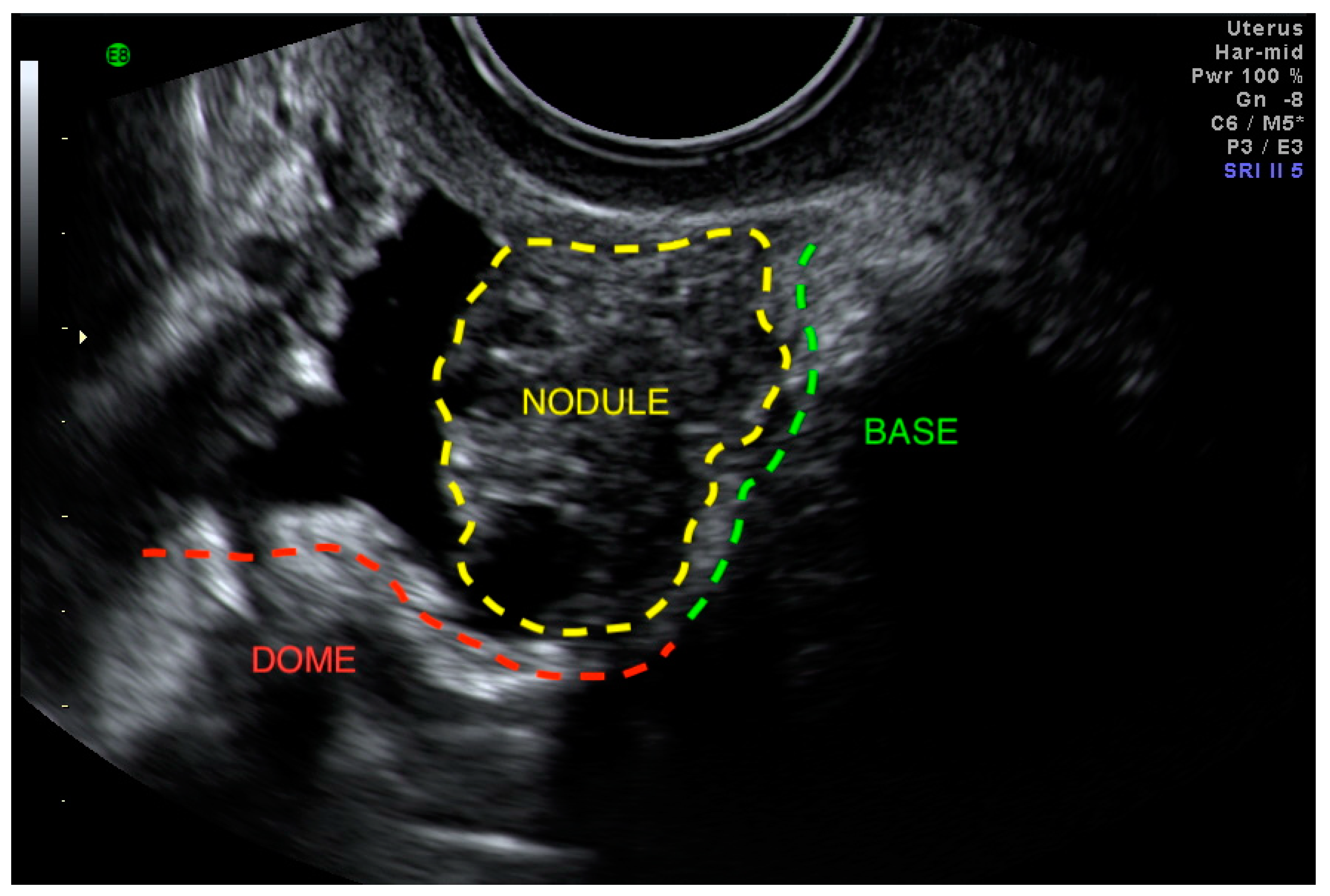
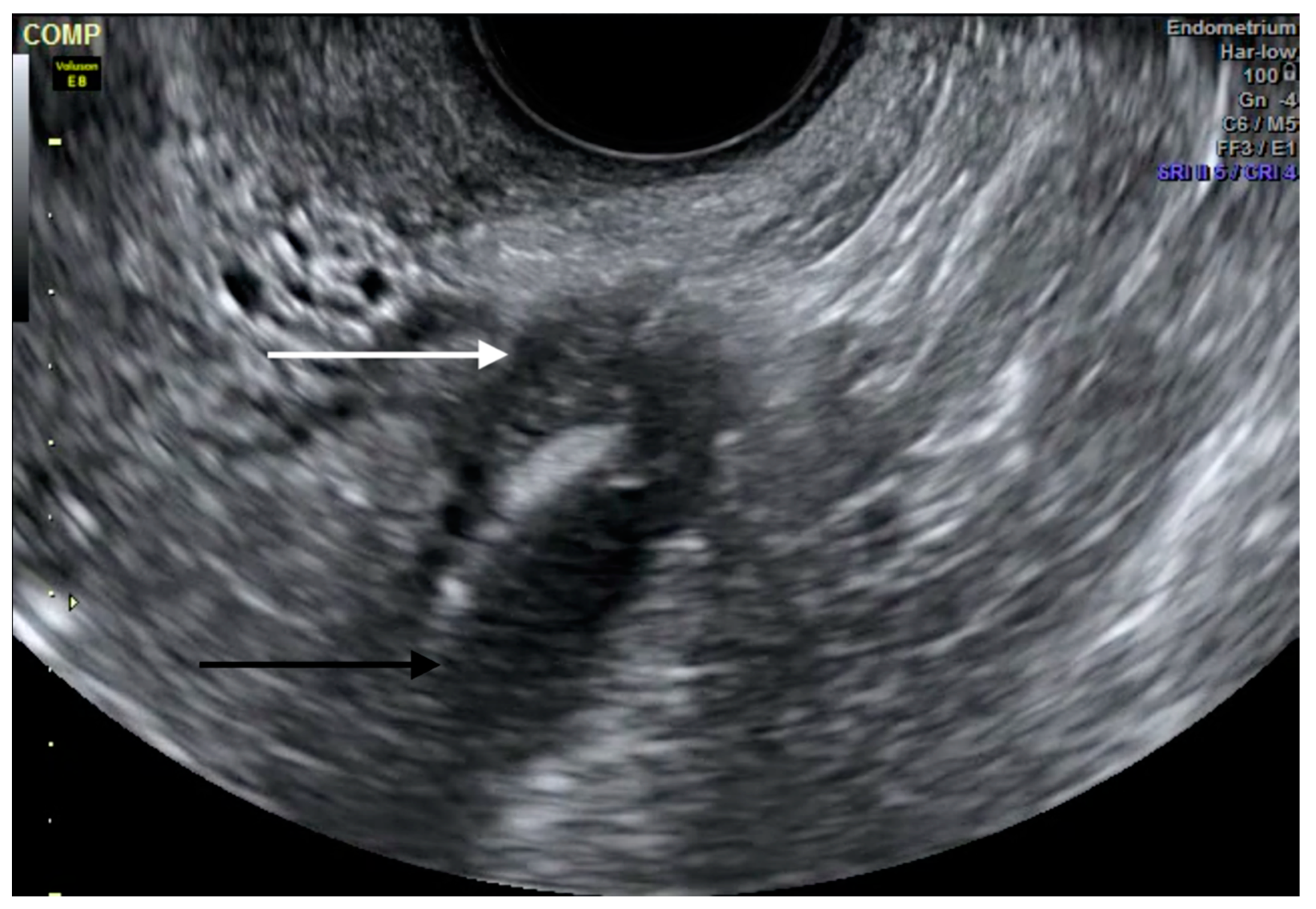
Ultrasound
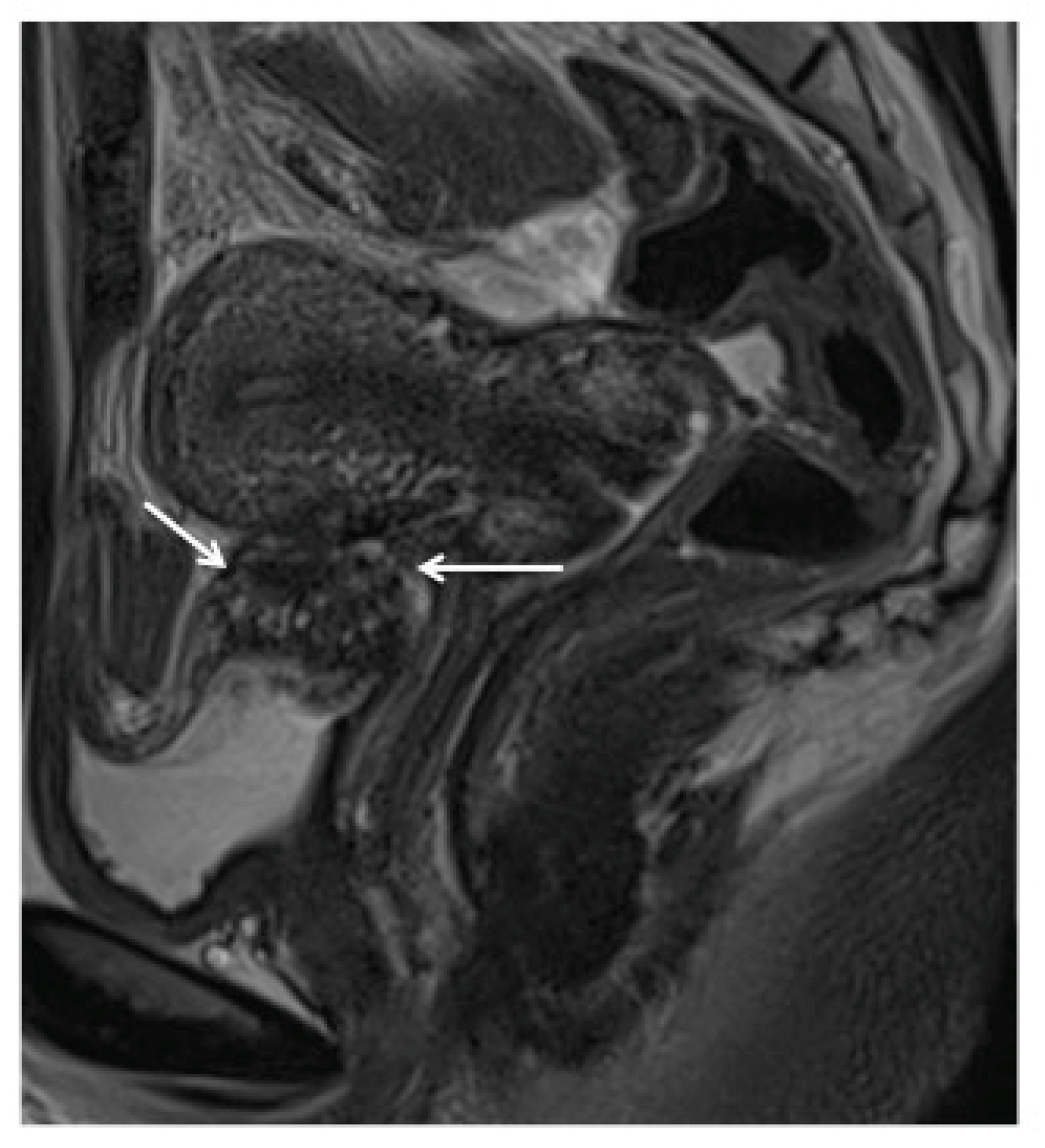
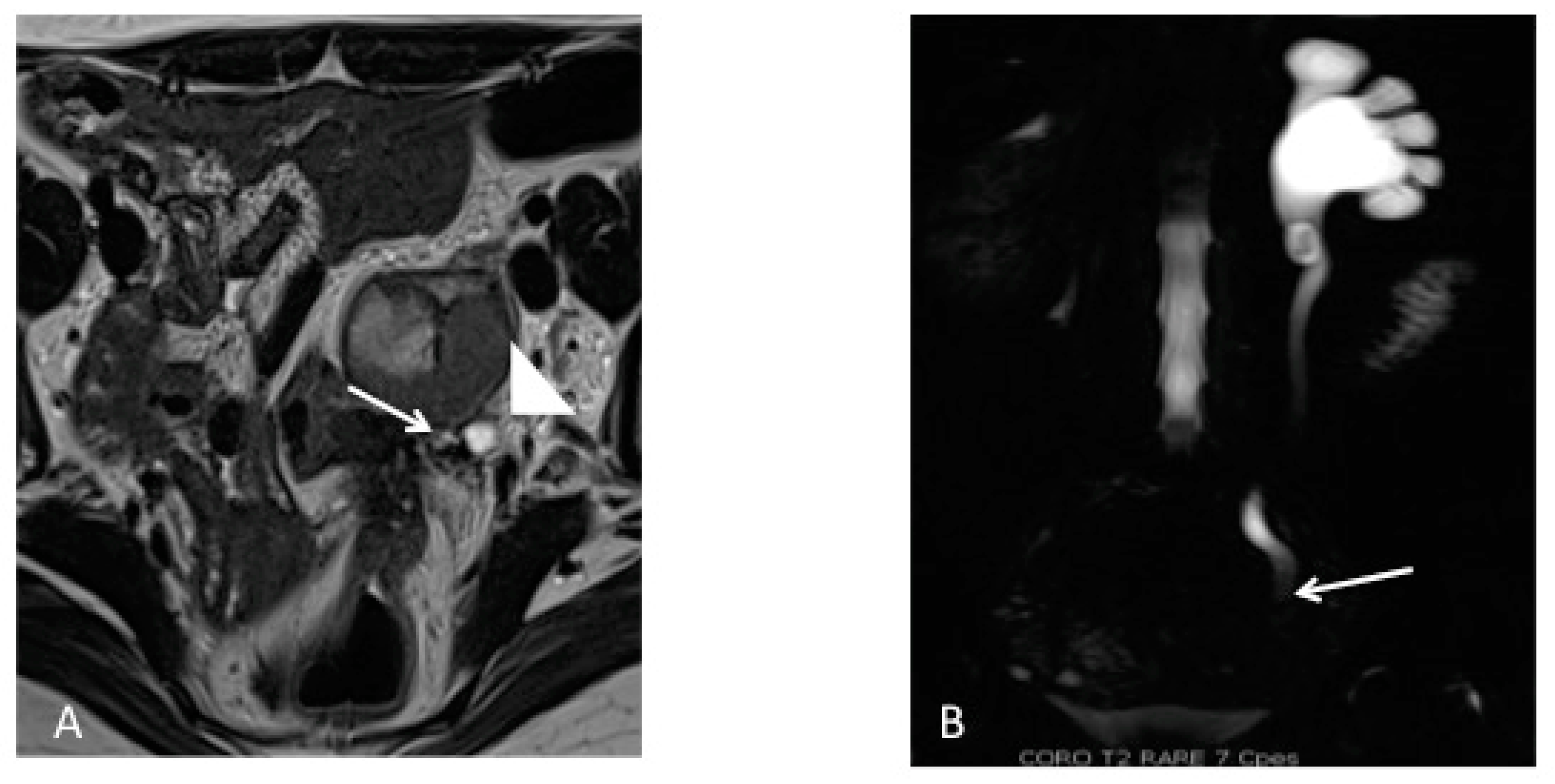
Magnetic Resonance Imaging
Supplementary Imaging
Cystourethroscopy
4.4. Differential Diagnosis of Bladder DE
4.4.1. Intraluminal Bladder Lesions
4.4.2. Urinary Tract Infection
4.4.3. Urinary Tract Calculus
4.4.4. Interstitial Cystitis
4.5. Treatment of Bladder DE
4.5.1. Medical Management
4.5.2. Surgical Management
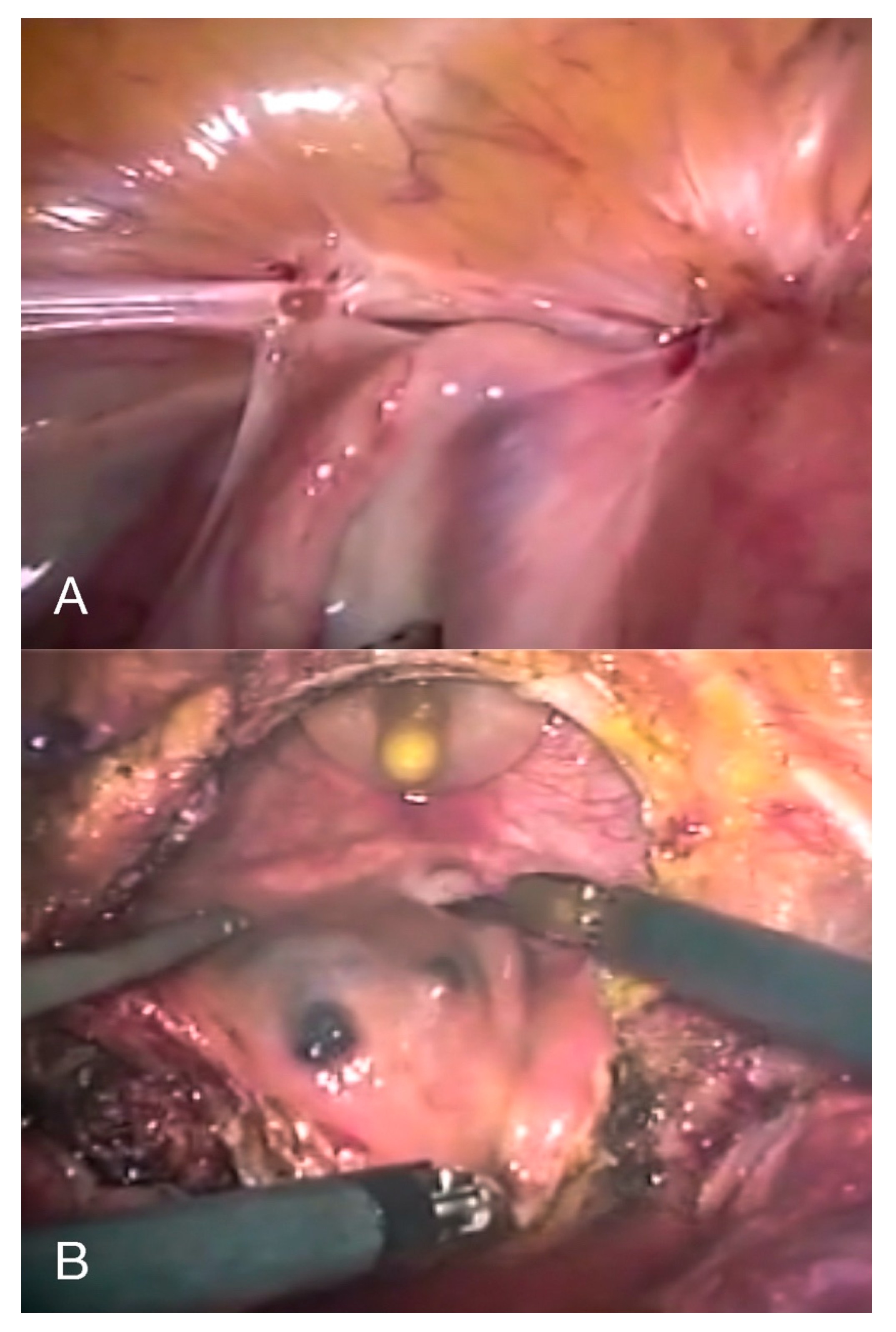
4.5.3. Surgical Approach
- (1)
- Cystourethroscopy: to evaluate the size of the lesion(s) and measure the distance between the lesion and the ureteral ridge. The use of ureteral catheters is not supported by strong evidence-based data; however, their use might be helpful when the distance between the lesion and the ureteral ridge is less than 2 cm or when the anatomy is distorted from previous surgeries or extensive disease, in order to reduce the risk of inadvertent ureteral damage at surgery.
- (2)
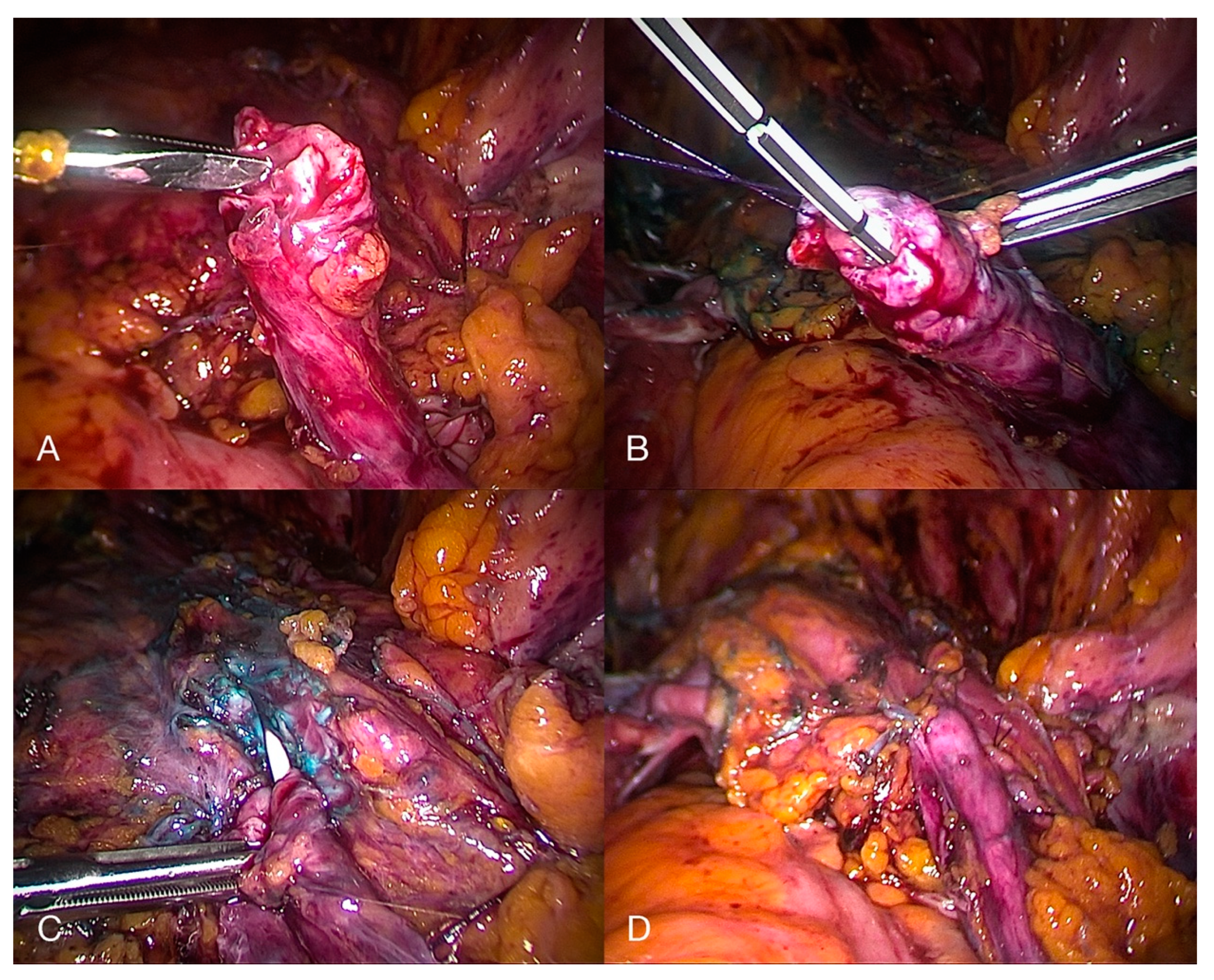
- Diagnostic laparoscopy, followed by the shaving of superficial serosal lesions off the bladder or partial cystectomy (Figure 7) when there is infiltration of the detrusor muscle, in order to restore a normal anatomy and prevent hydronephrosis and recurrence of the disease [6]. If the nodule affects the vesical base, it can either be approached laparoscopically (starting with the dissection of the vesicouterine pouch to facilitate a complete resection) or through an operative cystoscope, followed by reconstruction of the bladder either laparoscopically or robotically. Resecting the underlying myometrium has been proven to prevent a recurrence of the symptoms when it comes to bladder DE affecting the vesical base [46].
- (3)
- Bladder closure: We recommend closing the bladder with two layers of transverse sutures. At the end of the operation, the bladder is filled with methylene blue to confirm the integrity of the bladder, and a bladder catheter should be left in place for 10 days to prevent fistula formation.
4.5.4. Medical versus Surgical Treatment
5. Ureteral Endometriosis
5.1. Definition of Ureteral Endometriosis (UE)
5.2. Clinical Symptoms of UE
5.3. Diagnosis of UE
5.3.1. Medical History and Physical Examination
5.3.2. Laboratory Testing
5.3.3. Imaging Techniques
5.4. Differential Diagnosis of UE
5.5. Treatment of UE
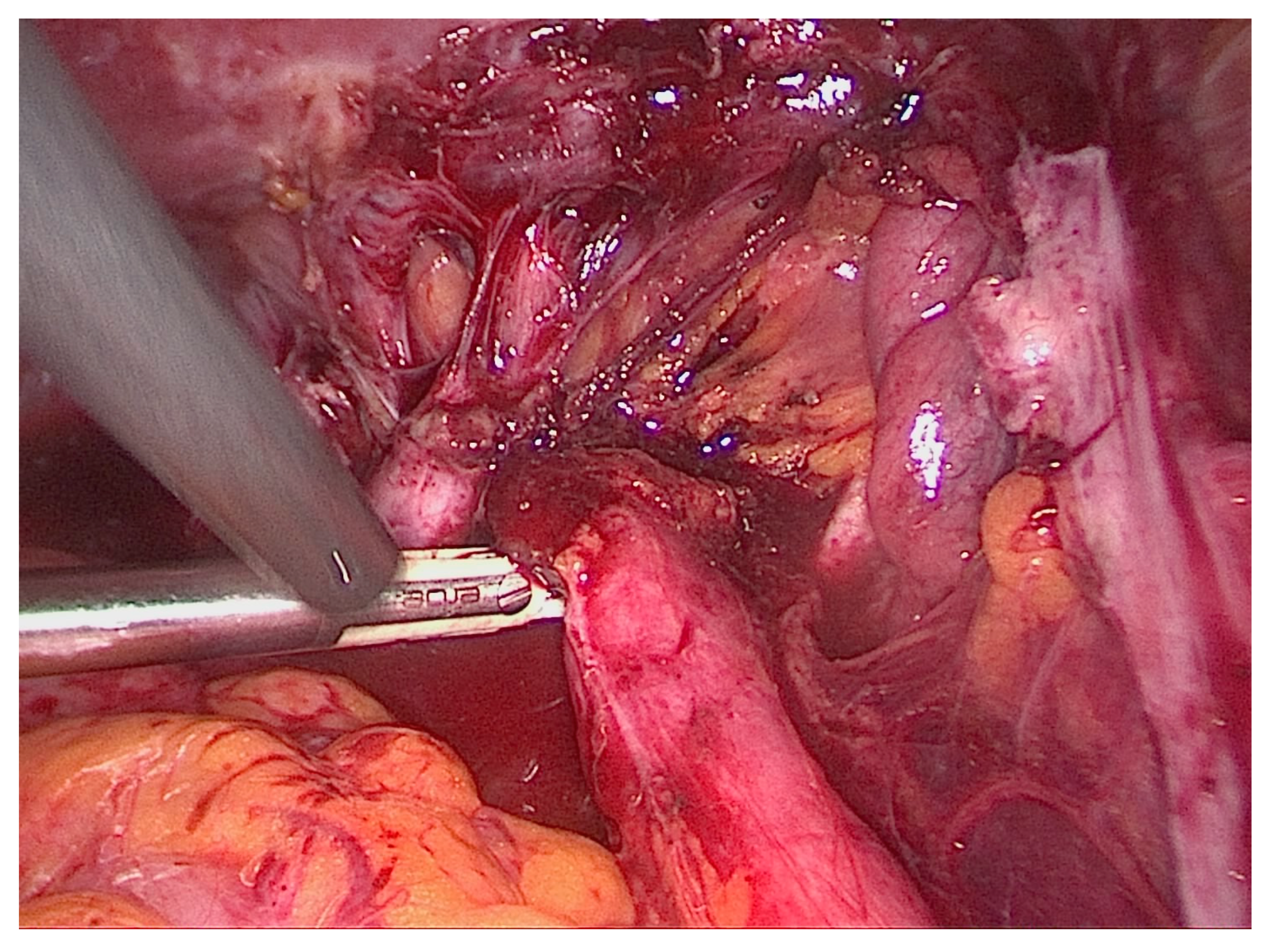
5.5.1. Ureterolysis
5.5.2. Ureterolysis, Ureterectomy with Ureteroureteral Anastomosis
5.5.3. Ureterolysis, Ureterectomy, and Ureteroneocystostomy
5.6. Postoperative Complications
6. Discussion
Supplementary Materials
Funding
Conflicts of Interest
References
- Berveiller, P.; Ropert, S.; Mir, O.; Becker, C.M.; Missmer, S.A.; Zondervan, K.T. Endometriosis. N. Engl. J. Med. 2020, 383, 193–194. [Google Scholar] [CrossRef]
- Johnson, N.P.; Hummelshoj, L.; Abrao, M.S.; Adamson, G.D.; Allaire, C.; Amelung, V.; Andersson, E.; Becker, C.; Ardal, K.B.B.; Bush, D.; et al. Consensus on current management of endometriosis. Hum. Reprod. 2013, 28, 1552–1568. [Google Scholar] [CrossRef]
- Leonardi, M.; Lam, A.; Abrão, M.S.; Johnson, N.P.; Condous, G. Ignored Because It Is Benign—It Is Time to Treat Endometriosis as if It Were Cancer. J. Obstet. Gynaecol. Can. 2020, 42, 507–509. [Google Scholar] [CrossRef]
- Johnson, N.P.; Hummelshoj, L.; Adamson, G.D.; Keckstein, J.; Taylor, H.S.; Abrao, M.S.; Bush, D.; Kiesel, L.; Tamimi, R.; Sharpe-Timms, K.L.; et al. World Endometriosis Society consensus on the classification of endometriosis. Hum. Reprod. 2016, 32, 315–324. [Google Scholar] [CrossRef]
- Berlanda, N.; Vercellini, P.; Carmignani, L.; Aimi, G.; Amicarelli, F.; Fedele, L. Ureteral and Vesical Endometriosis. Obstet. Gynecol. Surv. 2009, 64, 830–842. [Google Scholar] [CrossRef]
- Seracchioli, R.; Mabrouk, M.; Montanari, G.; Manuzzi, L.; Concetti, S.; Venturoli, S. Conservative laparoscopic management of urinary tract endometriosis (UTE): Surgical outcome and long-term follow-up. Fertil. Steril. 2010, 94, 856–861. [Google Scholar] [CrossRef]
- Maggiore, U.L.R.; Ferrero, S.; Candiani, M.; Somigliana, E.; Viganò, P.; Vercellini, P. Bladder Endometriosis: A Systematic Review of Pathogenesis, Diagnosis, Treatment, Impact on Fertility, and Risk of Malignant Transformation. Eur. Urol. 2017, 71, 790–807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knabben, L.; Imboden, S.; Fellmann, B.; Nirgianakis, K.; Kuhn, A.; Mueller, M.D. Urinary tract endometriosis in patients with deep infiltrating endometriosis: Prevalence, symptoms, management, and proposal for a new clinical classification. Fertil. Steril. 2015, 103, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, B.; Nassif, J.; Trompoukis, P.; Barata, S.; Wattiez, A. Prevalence and Management of Urinary Tract Endometriosis: A Clinical Case Series. Urology 2011, 78, 1269–1274. [Google Scholar] [CrossRef] [PubMed]
- Maccagnano, C.; Pellucchi, F.; Rocchini, L.; Ghezzi, M.; Scattoni, V.; Montorsi, F.; Rigatti, P.; Colombo, R. Ureteral Endometriosis: Proposal for a Diagnostic and Therapeutic Algorithm with a Review of the Literature. Urol. Int. 2013, 91, 1–9. [Google Scholar] [CrossRef]
- Espada, M.; Alvarez-Moreno, E.; De La Peña, M.J.; Capio, V.M.; Reid, S.; Condous, G. Imaging techniques in endometriosis. J. Endometr. Pelvic Pain Disord. 2018, 10, 136–150. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Wattiez, A.; Donnez, J. Deep endometriosis: Definition, diagnosis, and treatment. Fertil. Steril. 2012, 98, 564–571. [Google Scholar] [CrossRef]
- Horne, A.W.; Saunders, P.T. SnapShot: Endometriosis. Cell 2019, 179, 1677–1677.e1. [Google Scholar] [CrossRef] [PubMed]
- Somigliana, E.; Vercellini, P.; Gattei, U.; Chopin, N.; Chiodo, I.; Chapron, C. Bladder endometriosis: Getting closer and closer to the unifying metastatic hypothesis. Fertil. Steril. 2007, 87, 1287–1290. [Google Scholar] [CrossRef] [PubMed]
- Fedele, L. Bladder Endometriosis: Deep Infiltrating Endometriosis or Adenomyosis? Fertil. Steril. 1998, 69, 972–975. [Google Scholar] [CrossRef]
- Vercellini, P.; Pisacreta, A.; Pesole, A.; Vicentini, S.; Stellato, G.; Crosignani, P.G. Is ureteral endometriosis an asymmetric disease? BJOG: Int. J. Obstet. Gynaecol. 2000, 107, 559–561. [Google Scholar] [CrossRef] [Green Version]
- Guerriero, S.; Condous, G.; Bosch, T.V.D.; Valentin, L.; Leone, F.P.G.; Van Schoubroeck, D.; Exacoustos, C.; Installé, A.J.F.; Martins, W.P.; Abrao, M.S.; et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: A consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet. Gynecol. 2016, 48, 318–332. [Google Scholar] [CrossRef]
- Maggiore, U.L.R.; Ferrero, S.; Salvatore, S. Urinary incontinence and bladder endometriosis: Conservative management. Int. Urogynecol. J. 2014, 26, 159–162. [Google Scholar] [CrossRef]
- Guideline developed in collaboration with the American College of Radiology (ACR); the American College of Obstetricians and Gynecologists (ACOG); (Spr), T.S.F.P.R.; (Sru), T.S.O.R.I.U. AIUM Practice Guideline for the Performance of Ultrasound of the Female Pelvis. J. Ultrasound Med. 2014, 33, 1122–1130. [Google Scholar] [CrossRef] [Green Version]
- Arion, K.; Aksoy, T.; Allaire, C.; Noga, H.; Williams, C.; Bedaiwy, M.A.; Yong, P.J. Prediction of Pouch of Douglas Obliteration: Point-of-care Ultrasound Versus Pelvic Examination. J. Minim. Invasive Gynecol. 2019, 26, 928–934. [Google Scholar] [CrossRef]
- Reid, S.; Leonardi, M.; Lu, C.; Condous, G. The association between ultrasound-based ‘soft markers’ and endometriosis type/location: A prospective observational study. Eur. J. Obstet. Gynecol. Reprod. Boil. 2019, 234, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Savelli, L.; Manuzzi, L.; Pollastri, P.; Mabrouk, M.; Seracchioli, R.; Venturoli, S. Diagnostic accuracy and potential limitations of transvaginal sonography for bladder endometriosis. Ultrasound Obstet. Gynecol. 2009, 34, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Bean, E.; Naftalin, J.; Jurkovic, D. How to assess the ureters during pelvic ultrasound. Ultrasound Obstet. Gynecol. 2019, 53, 729–733. [Google Scholar] [CrossRef] [PubMed]
- Carfagna, P.; Nardone, C.D.C.; Nardone, A.D.C.; Scambia, G.; Marana, R.; Nardone, F.D.C.; Testa, A.C. Role of transvaginal ultrasound in evaluation of ureteral involvement in deep infiltrating endometriosis. Ultrasound Obstet. Gynecol. 2018, 51, 550–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leonardi, M.; Martins, W.P.; Espada, M.; Arianayagam, M.; Condous, G. Proposed technique to visualize and classify uterosacral ligament deep endometriosis with and without infiltration into parametrium or torus uterinus. Ultrasound Obstet. Gynecol. 2020, 55, 137–139. [Google Scholar] [CrossRef] [Green Version]
- Leonardi, M.; Condous, G. A pictorial guide to the ultrasound identification and assessment of uterosacral ligaments in women with potential endometriosis. Australas. J. Ultrasound Med. 2019, 22, 157–164. [Google Scholar] [CrossRef] [Green Version]
- Lima, R.; Abdalla-Ribeiro, H.; Nicola, A.L.; Eras, A.; Lobao, A.; Ribeiro, P.A. Endometriosis on the uterosacral ligament: A marker of ureteral involvement. Fertil. Steril. 2017, 107, 1348–1354. [Google Scholar] [CrossRef] [Green Version]
- Bretón, S.A.; Carrasco, A.L.; Gutierrez, A.H.; González, R.R.; García, J.D.S. Complete loss of unilateral renal function secondary to endometriosis: A report of three cases. Eur. J. Obstet. Gynecol. Reprod. Boil. 2013, 171, 132–137. [Google Scholar] [CrossRef]
- Nezhat, C.; Paka, C.; Gomaa, M.; Schipper, E. Silent Loss of Kidney Seconary to Ureteral Endometriosis. JSLS J. Soc. Laparoendosc. Surg. 2012, 16, 451–455. [Google Scholar] [CrossRef] [Green Version]
- Berger, J.P.; Rhemrev, J.; Smeets, M.; Henneman, O.; English, J.; Jansen, F.W. Limited Added Value of Magnetic Resonance Imaging After Dynamic Transvaginal Ultrasound for Preoperative Staging of Endometriosis in Daily Practice: A Prospective Cohort Study. J. Ultrasound Med. 2018, 38, 989–996. [Google Scholar] [CrossRef]
- Gutiérrez, A.H.; Spagnolo, E.; Hidalgo, P.; López, A.; Zapardiel, I.; Rodriguez, R.; Hernández, A. Magnetic resonance imaging versus transvaginal ultrasound for complete survey of the pelvic compartments among patients with deep infiltrating endometriosis. Int. J. Gynecol. Obstet. 2019, 146, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Bazot, M.; Darai, E.; Hourani, R.; Thomassin, I.; Cortez, A.; Uzan, S.; Buy, J.-N. Deep Pelvic Endometriosis: MR Imaging for Diagnosis and Prediction of Extension of Disease. Radiology 2004, 232, 379–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medeiros, L.R.F.; Da Rosa, M.I.; Silva, B.R.; Reis, M.E.; Simon, C.S.; Dondossola, E.R.; Cunha-Filho, J.S. Accuracy of magnetic resonance in deeply infiltrating endometriosis: A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2014, 291, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Nisenblat, V.; Farquhar, C.; Akoum, A.; Fraser, I.; Bossuyt, P.M. Non-invasive tests for the diagnosis of endometriosis. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef]
- Bazot, M.; Daraï, E. Diagnosis of deep endometriosis: Clinical examination, ultrasonography, magnetic resonance imaging, and other techniques. Fertil. Steril. 2017, 108, 886–894. [Google Scholar] [CrossRef] [Green Version]
- Sillou, S.; Poirée, S.; Millischer, A.; Chapron, C.; Helenon, O. Urinary endometriosis: MR Imaging appearance with surgical and histological correlations. Diagn. Interv. Imaging 2015, 96, 373–381. [Google Scholar] [CrossRef] [Green Version]
- Kinkel, K.; Frei, K.A.; Balleyguier, C.; Chapron, C. Diagnosis of endometriosis with imaging: A review. Eur. Radiol. 2005, 16, 285–298. [Google Scholar] [CrossRef] [Green Version]
- Barra, F.; Scala, C.; Biscaldi, E.; Vellone, V.G.; Ceccaroni, M.; Terrone, C.; Ferrero, S. Ureteral endometriosis: A systematic review of epidemiology, pathogenesis, diagnosis, treatment, risk of malignant transformation and fertility. Hum. Reprod. Updat. 2018, 24, 710–730. [Google Scholar] [CrossRef] [Green Version]
- Abreu-Gomez, J.; Udare, A.; Shanbhogue, K.P.; Schieda, N. Update on MR urography (MRU): Technique and clinical applications. Abdom. Radiol. 2019, 44, 3800–3810. [Google Scholar] [CrossRef]
- Geng, J.-H.; Lee, Y.-C. Bladder Endometriosis. N. Engl. J. Med. 2019, 381, e43. [Google Scholar] [CrossRef]
- Berlanda, N.; Somigliana, E.; Frattaruolo, M.P.; Buggio, L.; Dridi, D.; Vercellini, P. Surgery versus hormonal therapy for deep endometriosis: Is it a choice of the physician? Eur. J. Obstet. Gynecol. Reprod. Boil. 2017, 209, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Chapron, C.; Bourret, A.; Chopin, N.; Dousset, B.; Leconte, M.; Amsellem-Ouazana, D.; De Ziegler, D.; Borghese, B. Surgery for bladder endometriosis: Long-term results and concomitant management of associated posterior deep lesions. Hum. Reprod. 2010, 25, 884–889. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kołodziej, A.; Krajewski, W.; Dołowy, Ł.; Hirnle, L. Urinary Tract Endometriosis. Urol. J. 2015, 12, 2213–2217. [Google Scholar] [PubMed]
- Westney, O.L.; Amundsen, C.L.; McGuire, E.J. BLADDER ENDOMETRIOSIS: CONSERVATIVE MANAGEMENT. J. Urol. 2000, 163, 1814–1817. [Google Scholar] [CrossRef]
- Fedele, L.; Bianchi, S.; Montefusco, S.; Frontino, G.; Carmignani, L. A gonadotropin-releasing hormone agonist versus a continuous oral contraceptive pill in the treatment of bladder endometriosis. Fertil. Steril. 2008, 90, 183–184. [Google Scholar] [CrossRef]
- Fedele, L.; Bianchi, S.; Zanconato, G.; Bergamini, V.; Berlanda, N.; Carmignani, L. Long-term follow-up after conservative surgery for bladder endometriosis. Fertil. Steril. 2005, 83, 1729–1733. [Google Scholar] [CrossRef]
- Reisenauer, C. Vesicovaginal fistulas: A gynecological experience in 41 cases at a German pelvic floor center. Arch. Gynecol. Obstet. 2015, 292, 245–253. [Google Scholar] [CrossRef]
- Chapron, C.; Chiodo, I.; Leconte, M.; Amsellem-Ouazana, D.; Chopin, N.; Borghese, B.; Dousset, B. Severe ureteral endometriosis: The intrinsic type is not so rare after complete surgical exeresis of deep endometriotic lesions. Fertil. Steril. 2010, 93, 2115–2120. [Google Scholar] [CrossRef]
- Soriano, D.; Schonman, R.; Nadu, A.; Lebovitz, O.; Schiff, E.; Seidman, D.S.; Goldenberg, M. Multidisciplinary Team Approach to Management of Severe Endometriosis Affecting the Ureter: Long-term Outcome Data and Treatment Algorithm. J. Minim. Invasive Gynecol. 2011, 18, 483–488. [Google Scholar] [CrossRef]
- Frenna, V.; Santos, L.; Ohana, E.; Bailey, C.; Wattiez, A. Laparoscopic management of ureteral endometriosis: Our experience. J. Minim. Invasive Gynecol. 2007, 14, 169–171. [Google Scholar] [CrossRef]
- Comiter, C.V. Endometriosis of the urinary tract. Urol. Clin. N. Am. 2002, 29, 625–635. [Google Scholar] [CrossRef]
- Seracchioli, R.; Raimondo, D.; Di Donato, N.; Leonardi, D.; Spagnolo, E.; Paradisi, R.; Montanari, G.; Caprara, G.; Zannoni, L. Histological evaluation of ureteral involvement in women with deep infiltrating endometriosis: Analysis of a large series. Hum. Reprod. 2015, 30, 833–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freire, M.J.; Dinis, P.J.; Medeiros, R.; Sousa, L.; Águas, F.; Figueiredo, A. Deep Infiltrating Endometriosis—Urinary Tract Involvement and Predictive Factors for Major Surgery. Urology 2017, 108, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Fernbach, S.K.; Maizels, M.; Conway, J.J. Ultrasound grading of hydronephrosis: Introduction to the system used by the society for fetal urology. Pediatr. Radiol. 1993, 23, 478–480. [Google Scholar] [CrossRef]
- Gantt, P.A.; Hunt, J.B.; McDonough, P.G. Progestin reversal of ureteral endometriosis. Obstet. Gynecol. 1981, 57, 665–667. [Google Scholar]
- Leonardi, M.; Condous, G. Redefining ureterolysis to mirror the skills of modern gynecologists. J. Minim. Invasive Gynecol. 2020. [Google Scholar] [CrossRef]
- Ceccaroni, M.; Ceccarello, M.; Caleffi, G.; Clarizia, R.; Scarperi, S.; Pastorello, M.; Molinari, A.; Ruffo, G.; Cavalleri, S. Total Laparoscopic Ureteroneocystostomy for Ureteral Endometriosis: A Single-Center Experience of 160 Consecutive Patients. J. Minim. Invasive Gynecol. 2019, 26, 78–86. [Google Scholar] [CrossRef]
- Pérez, M.P.-U.; Bazán, A.A.; Dorrego, J.M.A.; Hernandez, A.; De Francisco, M.G.; Hernandez, M.M.; De Santiago, J.; Barthel, J.D.L.P. Urinary Tract Endometriosis: Clinical, Diagnostic, and Therapeutic Aspects. Urology 2009, 73, 47–51. [Google Scholar] [CrossRef]
- Dallas, K.B.; Rogo-Gupta, L.; Elliott, C.S. Urologic Injury and Fistula after Hysterectomy for Benign Indications. Obstet. Gynecol. 2019, 134, 241–249. [Google Scholar] [CrossRef] [Green Version]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leonardi, M.; Espada, M.; Kho, R.M.; Magrina, J.F.; Millischer, A.-E.; Savelli, L.; Condous, G. Endometriosis and the Urinary Tract: From Diagnosis to Surgical Treatment. Diagnostics 2020, 10, 771. https://doi.org/10.3390/diagnostics10100771
Leonardi M, Espada M, Kho RM, Magrina JF, Millischer A-E, Savelli L, Condous G. Endometriosis and the Urinary Tract: From Diagnosis to Surgical Treatment. Diagnostics. 2020; 10(10):771. https://doi.org/10.3390/diagnostics10100771
Chicago/Turabian StyleLeonardi, Mathew, Mercedes Espada, Rosanne M. Kho, Javier F. Magrina, Anne-Elodie Millischer, Luca Savelli, and George Condous. 2020. "Endometriosis and the Urinary Tract: From Diagnosis to Surgical Treatment" Diagnostics 10, no. 10: 771. https://doi.org/10.3390/diagnostics10100771
APA StyleLeonardi, M., Espada, M., Kho, R. M., Magrina, J. F., Millischer, A.-E., Savelli, L., & Condous, G. (2020). Endometriosis and the Urinary Tract: From Diagnosis to Surgical Treatment. Diagnostics, 10(10), 771. https://doi.org/10.3390/diagnostics10100771



