Conservative Treatment in Stress Urinary Incontinence—Narrative Literature Review
Simple Summary
Abstract
1. Introduction
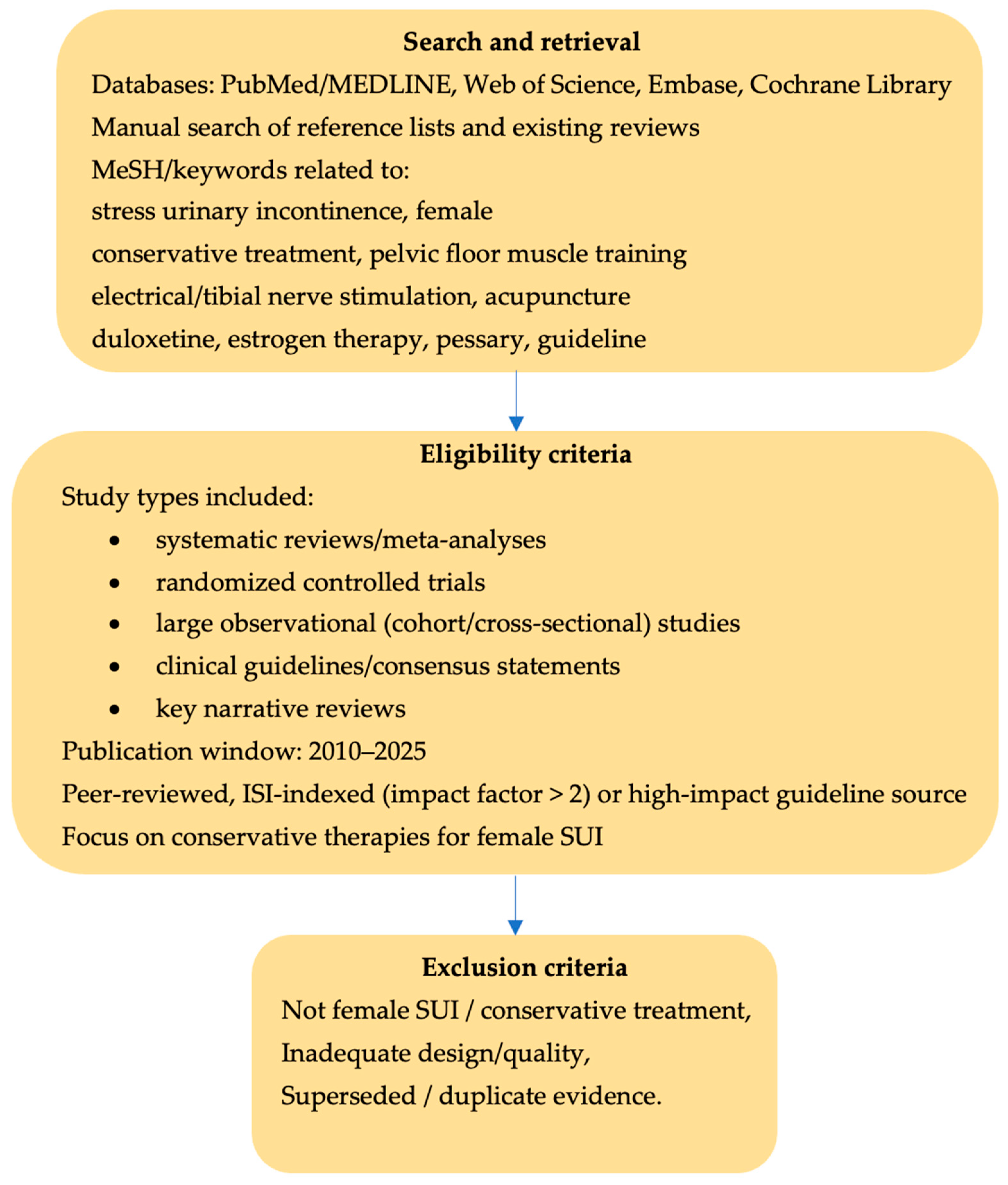
2. Materials and Methods
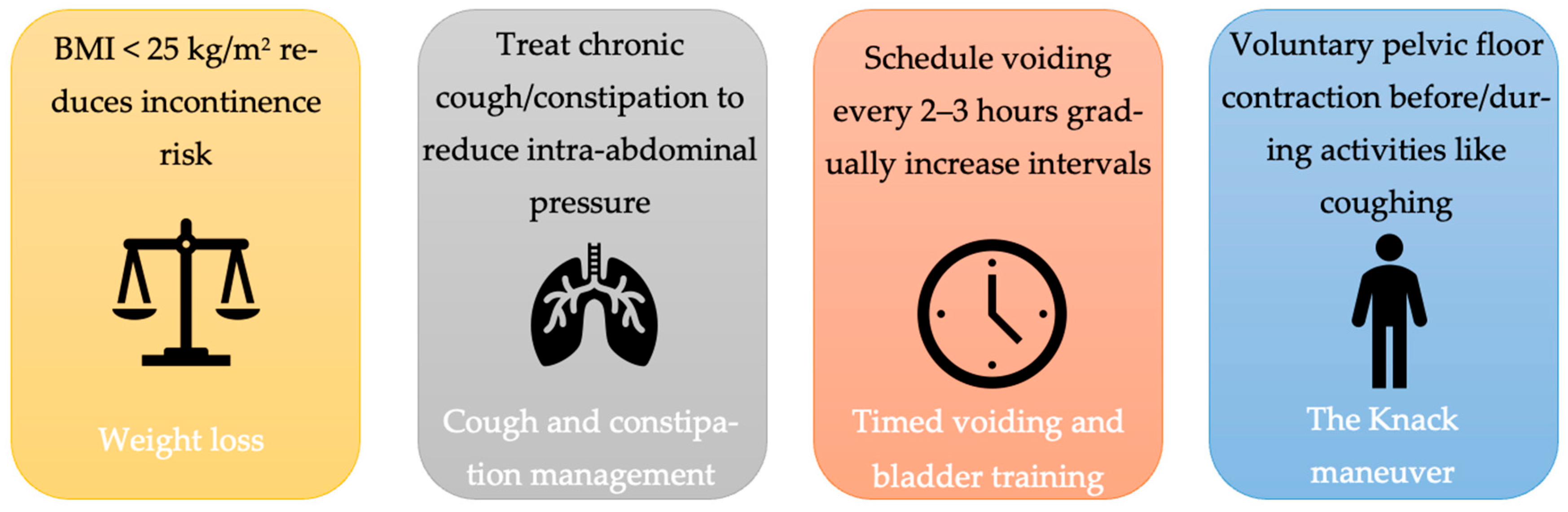
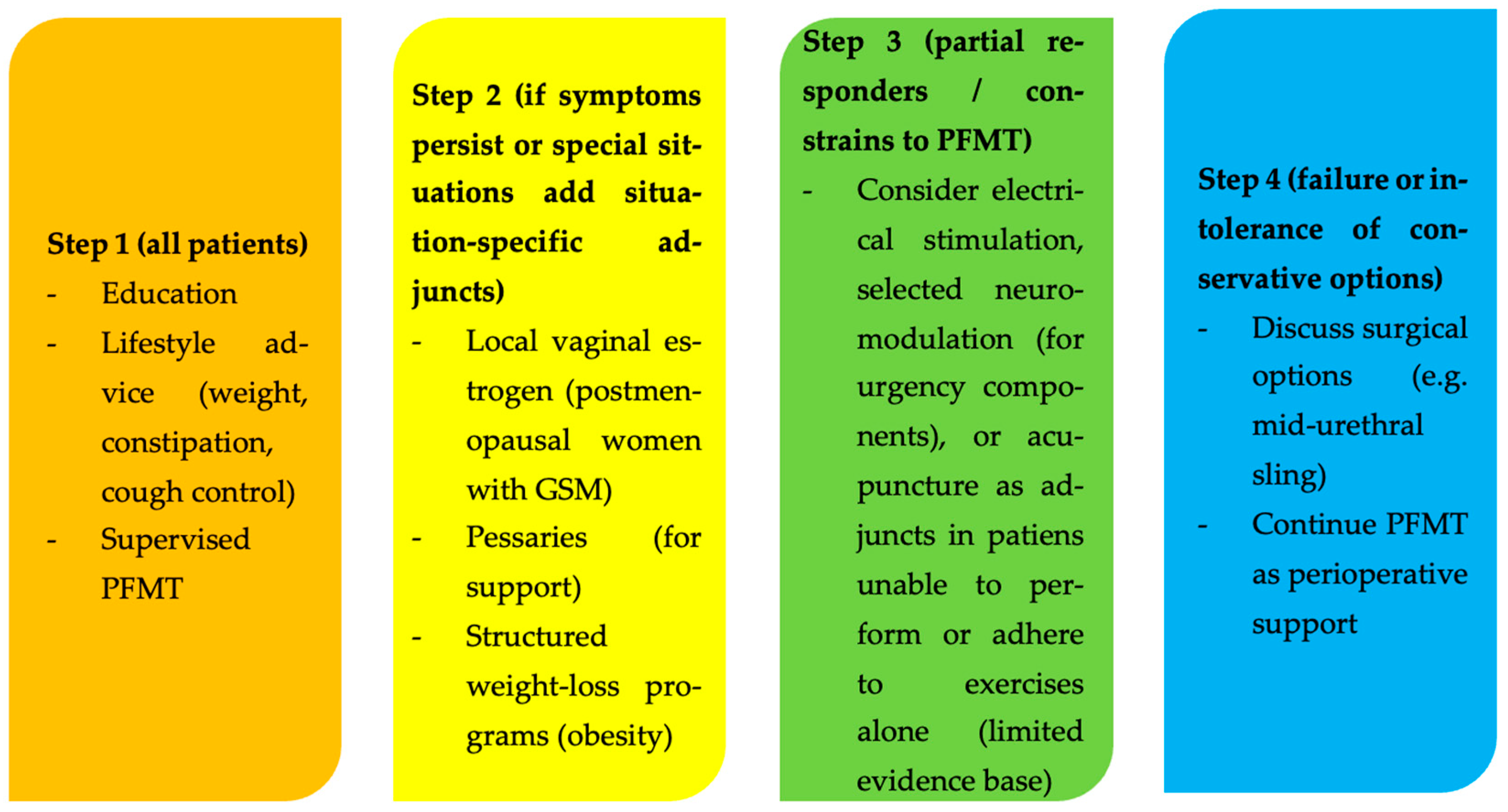
3. Results and Discussion
3.1. Pelvic Floor Muscle Training
- Symptom resolution: women with stress urinary incontinence (SUI) undergoing PFMT were eight times more likely to achieve symptom relief compared to those receiving no treatment or inactive interventions (56% vs. 6%; RR 8.38, 95% CI 3.68 −19.07; 4 trials, 165 women; high-quality evidence).
- Improvement in symptoms and quality of life (QoL): PFMT significantly improved UI symptoms (7 trials, 376 women; moderate-quality evidence) and QoL (6 trials, 348 women; low-quality evidence) compared to controls.
- Reduction in leakage episodes: PFMT reduced daily urine leakage by an average of one episode (MD −1.23; 95% CI −1.78 to −0.68; 7 trials, 432 women; moderate-quality evidence).
- Less urine loss on pad tests: Women in PFMT groups exhibited significantly reduced urine loss in short-duration (up to one hour) pad tests.
- These results highlight PFMT as a cost-effective conservative treatment for SUI [14].
3.2. Surface and Intravaginal Electrical Stimulation
- Intravaginal electrical stimulation: A probe electrode is inserted into the vagina to directly stimulate the pelvic floor musculature and periurethral tissue. Typically, intermittent, low-frequency (~20–50 Hz) pulses cause muscle contractions. Sessions last ~15–30 min and are carried out a few times per week for 6–12 weeks.
- Transcutaneous electrical nerve stimulation (TENS): Surface pad electrodes on the skin (e.g., over sacral nerves or pudendal nerve regions) deliver current through the skin to target pelvic floor nerves. This is less focal than vaginal ES but noninvasive.
- Extracorporeal magnetic innervation (ExMI): Although not electrical current per se, ExMI uses a magnetic field (usually via a chair device) to induce pelvic floor muscle contractions. It is often classed alongside electrical therapies and will be discussed here for convenience.
3.3. Acupuncture
3.4. Pharmacological Treatment of Stress Urinary Incontinence
3.5. Local Estrogen Therapy
3.6. Conservative Aids and Devices
3.7. Areas of Limited Evidence
3.8. Surgical Treatment
3.9. Guideline Convergence
3.10. Patient-Centered Care
3.11. Limitations of Evidence and Future Research
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUS | Artificial urinary sphincter |
| AUA | American Urological Association |
| BMI | Body mass index |
| CUA | Canadian Urological Association |
| EAU | European Association of Urology |
| ExMI | Extracorporeal magnetic innervation |
| FDA | Food and Drug Administration |
| GSM | Genitourinary syndrome of menopause |
| ICS | International Continence Society |
| ICIQ-SF | International Consultation on Incontinence Questionnaire—Short Form |
| ISD | Intrinsic sphincter deficiency |
| LUTS | Lower urinary tract symptoms |
| MeSH | Medical Subject Headings |
| MUS | Mid-urethral sling |
| NICE | National Institute for Health and Care Excellence |
| OAB | Overactive bladder |
| PFMT | Pelvic floor muscle training |
| PTNS | Posterior tibial nerve stimulation |
| QoL | Quality of life |
| RCT | Randomized controlled trial |
| RF | Radiofrequency |
| SNM | Sacral neuromodulation |
| SNRIs | Serotonin and norepinephrine reuptake inhibitors |
| SUI | Stress urinary incontinence |
| TAS-303 | Selective norepinephrine reuptake inhibitor TAS-303 |
| TENS | Transcutaneous electrical nerve stimulation |
| TTNS | Transcutaneous tibial nerve stimulation |
| UUI | Urgency urinary incontinence |
| UI | Urinary incontinence |
| US | United States (in context of FDA approval) |
References
- Moossdorff-Steinhauser, H.F.A.; Berghmans, B.C.M.; Spaanderman, M.E.A.; Bols, E.M.J. Urinary incontinence 6 weeks to 1 year post-partum: Prevalence, experience of bother, beliefs, and help-seeking behavior. Int. Urogynecol. J. 2021, 32, 1817–1824. [Google Scholar] [CrossRef] [PubMed]
- Legendre, G.; Fritel, X.; Panjo, H.; Zins, M.; Ringa, V. Incidence and remission of stress, urge, and mixed urinary incontinence in midlife and older women: A longitudinal cohort study. Neurourol. Urodyn. 2020, 39, 650–657. [Google Scholar] [CrossRef]
- Milsom, I.; Gyhagen, M. The prevalence of urinary incontinence. Climacteric 2019, 22, 217–222. [Google Scholar] [CrossRef]
- Lopes, F.D.; Henriques, C.; Lopes, M.S.; Mendes, I.M. Quality of life of women with urinary incontinence in the postpartum period: An integrative literature review. Front. Glob. Womens Health 2025, 6, 1562572. [Google Scholar] [CrossRef]
- Abrams, P.; Andersson, K.E.; Birder, L.; Bliss, D.; Brubaker, L.; Cardozo, L.; Castro-Diaz, D.; O’COnnell, P.; Cottenden, A.; Cotterill, N.; et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and Treatment of Urinary Incontinence, Pelvic Organ Prolapse, and Fecal Incontinence. Neurourol. Urodyn. 2018, 37, 2271–2292. [Google Scholar] [CrossRef]
- Bo, K.; Frawley, H.C.; Haylen, B.T.; Abramov, Y.; Almeida, F.G.; Berghmans, B.; Bortolini, M.; Dumoulin, C.; Gomes, M.; McClurg, D.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and non-pharmacological management of female pelvic floor dysfunction. Int. Urogynecol. J. 2017, 28, 191–213. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.N.; Anger, J.T. Urinary incontinence in women. BMJ 2014, 349, g4531. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.; Hu, Y.; Cai, W. Association between urinary incontinence and mortality risk among US adults: A prospective cohort study. BMC Public Health 2024, 24, 2753. [Google Scholar] [CrossRef]
- Paiva, L.L.; Ferla, L.; Darski, C.; Catarino, B.M.; Ramos, J.G.L. Pelvic floor muscle training in groups versus individual or home treatment of women with urinary incontinence: Systematic review and meta-analysis. Int. Urogynecol. J. 2017, 28, 351–359. [Google Scholar] [CrossRef]
- Denisenko, A.A.; Clark, C.B.; D’Amico, M.; Murphy, A.M. Evaluation and management of female urinary incontinence. Can. J. Urol. 2021, 28, 27–32. [Google Scholar]
- Mørkved, S.; Bø, K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: A systematic review. Br. J. Sports Med. 2014, 48, 299–310. [Google Scholar] [CrossRef]
- Ko, P.C.; Liang, C.C.; Chang, S.D.; Lee, J.T.; Chao, A.S.; Cheng, P.J. A randomized controlled trial of antenatal pelvic floor exercises to prevent and treat urinary incontinence. Int. Urogynecol. J. 2011, 22, 17–22. [Google Scholar] [CrossRef]
- Nambiar, A.K.; Arlandis, S.; Bø, K.; Cobussen-Boekhorst, H.; Costantini, E.; de Heide, M.; Farag, F.; Groen, J.; Karavitakis, M.; Lapitan, M.C.; et al. European Association of Urology Guidelines on the Diagnosis and Management of Female Non-neurogenic Lower Urinary Tract Symptoms. Part 1: Diagnostics, Overactive Bladder, Stress Urinary Incontinence, and Mixed Urinary Incontinence. Eur. Urol. 2022, 82, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Dumoulin, C.; Cacciari, L.P.; Hay-Smith, E.J.C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst. Rev. 2018, 10, CD005654. [Google Scholar] [CrossRef] [PubMed]
- Borello-France, D.F.; Zyczynski, H.M.; Downey, P.A.; Rause, C.R.; Wister, J.A. Effect of pelvic-floor muscle exercise position on continence and quality-of-life outcomes in women with stress urinary incontinence. Phys. Ther. 2006, 86, 974–986. [Google Scholar] [CrossRef] [PubMed]
- Radzimińska, A.; Strączyńska, A.; Weber-Rajek, M.; Styczyńska, H.; Strojek, K.; Piekorz, Z. The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: A systematic literature review. Clin. Interv. Aging 2018, 13, 957–965. [Google Scholar] [CrossRef]
- Abrams, P.; Linda, C.; Adrian, W.; Alan, W. 6th International Consultation on Incontinence. Tokyo 2016. Available online: https://www.ics.org/publications/ici6/Incontinence6thEdition2017eBookv2.pdf (accessed on 28 October 2025).
- Snooks, S.J.; Swash, M.; Henry, M.M.; Setchell, M. Risk factors in childbirth causing damage to the pelvic floor innervation. Int. J. Color. Dis. 1986, 1, 20–24. [Google Scholar] [CrossRef]
- Ptak, M.; Ciećwież, S.; Brodowska, A.; Nawrocka-Rutkowska, J.; Diaz-Mohedo, E.; Rotter, I. The Effect of Pelvic Floor Muscles Exercise on Quality of Life in Women with Stress Urinary Incontinence and Its Relationship with Vaginal Deliveries: A Randomized Trial. Biomed. Res. Int. 2019, 2019, 5321864. [Google Scholar] [CrossRef]
- Herbison, G.P.; Dean, N. Weighted vaginal cones for urinary incontinence. Cochrane Database Syst. Rev. 2013, 2013, CD002114. [Google Scholar] [CrossRef]
- Kim, H.; Suzuki, T.; Yoshida, Y.; Yoshida, H. Effectiveness of multidimensional exercises for the treatment of stress urinary incontinence in elderly community-dwelling Japanese women: A randomized, controlled, crossover trial. J. Am. Geriatr. Soc. 2007, 55, 1932–1939. [Google Scholar] [CrossRef]
- Lunardi, A.C.; Foltran, G.C.; Carro, D.F.; Silveira, L.T.; Haddad, J.M.; Ferreira, E.A. Efficacy of electrical stimulation vs pelvic floor muscle training on stress urinary incontinence: A systematic review and meta-analysis. Disabil. Rehabil. 2025, 47, 3256–3267. [Google Scholar] [CrossRef] [PubMed]
- Hagen, S.; Elders, A.; Stratton, S.; Sergenson, N.; Bugge, C.; Dean, S.; Hay-Smith, J.; Kilonzo, M.; Dimitrova, M.; Abdel-Fattah, M.; et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: Multicentre randomised controlled trial. BMJ 2020, 371, m3719. [Google Scholar] [CrossRef]
- Alouini, S.; Memic, S.; Couillandre, A. Pelvic Floor Muscle Training for Urinary Incontinence with or without Biofeedback or Electrostimulation in Women: A Systematic Review. Int. J. Environ. Res. Public. Health 2022, 19, 2789. [Google Scholar] [CrossRef] [PubMed]
- Al-Shaikh, G.; Syed, S.; Osman, S.; Bogis, A.; Al-Badr, A. Pessary use in stress urinary incontinence: A review of advantages, complications, patient satisfaction, and quality of life. Int. J. Womens Health 2018, 10, 195–201. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Urinary incontinence and pelvic organ prolapse in women: Management. In NICE Guideline NG123; NICE: London, UK, 2019. [Google Scholar]
- Kobashi, K.C.; Vasavada, S.; Bloschichak, A.; Hermanson, L.; Kaczmarek, J.; Kim, S.K.; Kirkby, E.; Malik, R. Updates to Surgical Treatment of Female Stress Urinary Incontinence (SUI): AUA/SUFU Guideline (2023). J. Urol. 2023, 209, 1091–1098. [Google Scholar] [CrossRef]
- Pelvic Floor Muscle Training for Urinary Incontinence in Women. Cochrane Library. Available online: https://www.cochrane.org/evidence/CD005654_pelvic-floor-muscle-training-urinary-incontinence-women (accessed on 28 October 2025).
- Strojek, K.; Strączyńska, A.; Radzimińska, A.; Weber-Rajek, M. The Effects of Extracorporeal Magnetic Innervation in the Treatment of Women with Urinary Incontinence: A Systematic Review. J. Clin. Med. 2023, 12, 5455. [Google Scholar] [CrossRef] [PubMed]
- Stewart, F.; Berghmans, B.; Bø, K.; Glazener, C.M.A. Electrical stimulation with non-implanted devices for stress urinary incontinence in women. Cochrane Database Syst. Rev. 2017, 12, CD012390. [Google Scholar] [CrossRef]
- Castro, R.A.; Arruda, R.M.; Zanetti, M.R.D.; Santos, P.D.; Sartori, M.G.F.; Girão, M.J.B.C. Single-Blind, Randomized, Controlled Trial of Pelvic Floor Muscle Training, Electrical Stimulation, Vaginal Cones, and No Active Treatment in the Management of Stress Urinary Incontinence. Clinics 2008, 63, 465–472. [Google Scholar] [CrossRef]
- Astasio-Picado, Á.; García-Cano, M. Neuromodulation of the Posterior Tibial Nerve for the Control of Urinary Incontinence. Medicina 2022, 58, 442. [Google Scholar] [CrossRef]
- Marchal, C.; Herrera, B.; Antuña, F.; Saez, F.; Perez, J.; Castillo, E.; Cantero, J.; Milla, F.; Machuca, J.; Redondo, M.; et al. Percutaneous tibial nerve stimulation in treatment of overactive bladder: When should retreatment be started? Urology 2011, 78, 1046–1050. [Google Scholar] [CrossRef]
- Sonmez, R.; Yildiz, N.; Alkan, H. Efficacy of percutaneous and transcutaneous tibial nerve stimulation in women with idiopathic overactive bladder: A prospective randomised controlled trial. Ann. Phys. Rehabil. Med. 2022, 65, 101486. [Google Scholar] [CrossRef]
- Yang, N.; Ge, X.; Ye, J.; Liu, Q.; Wu, Y.; Yan, H.; Han, X. Efficacy of acupuncture for urinary incontinence in middle-aged and elderly women: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 257, 138–143. [Google Scholar] [CrossRef]
- Kannan, P.; Bello, U.M. Efficacy of various forms of acupuncture for the treatment of urinary incontinence in women: A systematic review and meta-analysis. Explore 2023, 19, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Chen, B.; Si, X.; Hou, W.; Fan, Q.; Li, X.; Li, J.; Ming, S.; Yin, P.; Chen, Y. Optimized electroacupuncture treatment for female stress urinary incontinence: Study protocol for a multi-center randomized controlled trial. Front. Psychiatry 2023, 14, 1228131. [Google Scholar] [CrossRef]
- Xu, H.; Liu, B.; Wu, J.; Du, R.; Liu, X.; Yu, J.; Liu, Z. A Pilot Randomized Placebo Controlled Trial of Electroacupuncture for Women with Pure Stress Urinary Incontinence. PLoS ONE 2016, 11, e0150821. [Google Scholar] [CrossRef]
- Jiang, T.; Dong, Z.-Y.; Shi, Y.; Zhou, Y.-Q.; Zhang, H.-B.; Gong, Y. Efficacy and safety of acupuncture monotherapy or combined with pelvic floor muscle training for female stress urinary incontinence: A systematic review and meta-analysis. Front. Med. 2025, 11, 1499905. [Google Scholar] [CrossRef] [PubMed]
- Dmochowski, R.R. Duloxetine: A summary of published clinical experience. Rev. Urol. 2004, 6, S56–S63. [Google Scholar] [PubMed]
- Li, J.; Yang, L.; Pu, C.; Tang, Y.; Yun, H.; Han, P. The role of duloxetine in stress urinary incontinence: A systematic review and meta-analysis. Int. Urol. Nephrol. 2013, 45, 679–686. [Google Scholar] [CrossRef]
- Mangır, N.; Uçar, M.; Gülpınar, Ö.; Özkürkçügil, C.; Demirkesen, O.; Tarcan, T. Duloxetine in the Treatment of Women with Urinary Incontinence: A Systematic Review and Meta-analysis of Efficacy Data from Randomized Controlled Clinical Trials. J. Urol. Surg. 2023, 10, 1–8. [Google Scholar] [CrossRef]
- Viktrup, L.; Pangallo, B.A.; Detke, M.J.; Zinner, N.R. Urinary Side Effects of Duloxetine in the Treatment of Depression and Stress Urinary Incontinence. Prim. Care Companion J. Clin. Psychiatry 2004, 6, 65–73. [Google Scholar] [CrossRef]
- Lorzadeh, N.; Jahanshahi, M. The effect of duloxetine on stress urinary incontinence. Health Sci. Rep. 2024, 7, e2091. [Google Scholar] [CrossRef]
- Harland, N.; Walz, S.; Eberli, D.; Schmid, F.A.; Aicher, W.K.; Stenzl, A.; Amend, B. Stress Urinary Incontinence: An Unsolved Clinical Challenge. Biomedicines 2023, 11, 2486. [Google Scholar] [CrossRef]
- Kermode-Scott, B. Risks of duloxetine for stress incontinence outweigh benefits, say researchers. BMJ 2016, 355, i6103. [Google Scholar] [CrossRef]
- Takahashi, S.; Kato, K.; Yokoyama, O.; Takei, M.; Gotoh, M. Efficacy and Safety of TAS-303 in Female Patients With Stress Urinary Incontinence: A Phase 2, Randomized, Double-Blind, Placebo-Controlled Trial. J. Urol. 2024, 212, 267–279. [Google Scholar] [CrossRef]
- Hirschberg, A.L. Enhancing quality of life: Addressing vulvovaginal atrophy and urinary tract symptoms. Climacteric 2025, 28, 400–407. [Google Scholar] [CrossRef]
- Porcari, I.; Uccella, S.; Casprini, C.; Bosco, M.; Zorzato, P.C.; Garzon, S. Vulvovaginal estrogen therapy for urinary symptoms in postmenopausal women: A review and meta-analysis. Climacteric 2025, 26, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Cody, J.D.; Jacobs, M.L.; Richardson, K.; Moehrer, B.; Hextall, A. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst. Rev. 2012, 10, CD001405. [Google Scholar] [CrossRef] [PubMed]
- Richter, H.E.; Burgio, K.L.; Goode, P.S.; Borello-France, D.; Bradley, C.S.; Brubaker, L.; Handa, V.L.; Fine, P.M.; Visco, A.G.; Zyczynski, H.M.; et al. Non-surgical management of stress urinary incontinence: Ambulatory treatments for leakage associated with stress (ATLAS) trial. Clin. Trials 2007, 4, 92–101. [Google Scholar] [CrossRef]
- Nekkanti, S.; Wu, J.M.; Hundley, A.F.; Hudson, C.; Pandya, L.K.; Dieter, A.A. A randomized trial comparing continence pessary to continence device (Poise Impressa®) for stress incontinence. Int. Urogynecol. J. 2022, 33, 861–868. [Google Scholar] [CrossRef]
- Cameron, A.P.; Jimbo, M.; Heidelbaugh, J.J. Diagnosis and office-based treatment of urinary incontinence in adults. Part two: Treatment. Ther. Adv. Urol. 2013, 5, 189–200. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ranjbar, A.; Mehrnoush, V.; Darsareh, F.; Kotb, A.; Zakaria, A.; Shekari, M.; Jahromi, M.S. Vaginal Laser Therapy for Stress Urinary Incontinence: A Systematic Review of Prospective Randomized Clinical Trials. J. Menopausal Med. 2022, 28, 103–111. [Google Scholar] [CrossRef]
- Lee, P.; Perruzza, D.; Edell, H.; Jarvi, S.; Kim, K.; Sultana, R.; Alavi, N.; Kiss, A.; Cao, X.; Gagnon, L.-H.; et al. Double-blind randomized controlled trial of Er:YAG vaginal laser to treat female stress urinary incontinence. Am. J. Obstet. Gynecol. 2025, 232, 541.e1–541.e12. [Google Scholar] [CrossRef]
- Ippolito, G.M.; Crescenze, I.; Sitto, H.; Palanjian, R.R.; Raza, D.; Barboglio-Romo, P.; Wallace, S.A.; Leal, G.O.; Clemens, J.Q.; Dahm, P.; et al. Vaginal Lasers for Treating Stress Urinary Incontinence in Women: An Abridged Cochrane Systematic Review and Meta-Analysis. J. Urol. 2025, 214, 474–486. [Google Scholar] [CrossRef] [PubMed]
- Carlson, K.; Andrews, M.; Bascom, A.; Baverstock, R.; Campeau, L.; Dumoulin, C.; Labossiere, J.; Locke, J.; Nadeau, G.; Welk, B. 2024 Canadian Urological Association guideline: Female stress urinary incontinence. Can. Urol. Assoc. J. 2024, 18, 83–102. [Google Scholar] [CrossRef] [PubMed]
- Richter, H.E.; Albo, M.E.; Zyczynski, H.M.; Kenton, K.; Norton, P.A.; Sirls, L.T.; Kraus, S.R.; Chai, T.C.; Lemack, G.E.; Dandreo, K.J.; et al. Retropubic versus transobturator midurethral slings for stress incontinence. N. Engl. J. Med. 2010, 362, 2066–2076. [Google Scholar] [CrossRef] [PubMed]
- Goldman, H.B.; Zimmern, P.E. Artificial urinary sphincter for female stress incontinence: A review of the literature and current recommendations. Int. Urogynecol. J. 2015, 26, 175–182. [Google Scholar]
- Rehman, H.; Bezerra, C.A.; Bruschini, H.; Cody, J.D.; Aluko, P. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database Syst. Rev. 2011, 2011, CD001754. [Google Scholar]
- European Association of Urology. 2017 Edition—Urology Guidelines. Available online: https://www.urology.wiki/HandBooks/EAU/2017/Guidelines_WebVersion_Complete.pdf (accessed on 28 October 2025).
- Woodley, S.J.; Lawrenson, P.; Boyle, R.; Cody, J.D.; Mørkved, S.; Kernohan, A.; Hay-Smith, E.J. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2020, 5, CD007471. [Google Scholar] [CrossRef]
| Factor | Description |
|---|---|
| Advancing Age | Weakened pelvic floor muscles and decreased bladder elasticity with aging |
| Genetic Predisposition | Hereditary component in some cases |
| Obstetric History | Multiple pregnancies, vaginal deliveries, complicated childbirth leading to pelvic floor dysfunction |
| Surgical History | Gynecological and pelvic surgeries (e.g., hysterectomy) altering bladder and urethra support |
| Smoking | Chronic coughing stresses pelvic floor muscles |
| Chronic Constipation | Persistent straining weakens pelvic support structures |
| Menopause | Estrogen deficiency reduces elasticity and strength of urogenital tissues |
| High Impact Sports | Activities increasing intra-abdominal pressure strain pelvic floor muscles |
| Therapy/Method | Effectiveness | Evidence Strength | Key Benefits | Safety/Tolerability | Notes/Limitations |
|---|---|---|---|---|---|
| Pelvic floor muscle training (PFMT) | Highly effective; 50–70% symptom reduction or cure | Strong evidence; front-line recommended by NICE, AUA | Improves symptoms significantly; improves postoperative outcomes | Excellent safety profile | Requires proper instruction, training duration/intensity, long-term compliance |
| Electrical stimulation (ES) | Some benefit over no treatment; similar or no significant advantage vs. PFMT | Moderate evidence; no superiority to PFMT | Provides symptom improvement | Generally safe; some discomfort and contraindications (e.g., pacemakers, pregnancy) | Not justified as first-line over PFMT |
| PTNS/TTNS (neuromodulation) | Neuromodulation for overactive bladder/urgency component in mixed UI; not indicated for isolated SUI | Moderate evidence | Reversible, safe option for refractory OAB symptoms | Good patient comfort and ease of application | TTNS preferred over PTNS for comfort |
| Acupuncture | Some improvement; low evidence strength | Low evidence level | Relatively low risk | Safe if performed by qualified practitioners | Not a first-line or standalone therapy; better with PFMT |
| Pharmacological (e.g., duloxetine) | Effective in some; side effects limit use | Evidence level 1 for efficacy but limited by tolerability | Optional adjunct | Side effects common; caution advised | Not routinely recommended due to safety concerns |
| Local estrogen therapy | Recommended for menopausal women with UI and vaginal atrophy | Moderate evidence, Recommendation Grade B | Safe; improves symptoms related to atrophy | Minor side effects (discharge, irritation) | Systemic estrogen contraindicated |
| Conservative aids/devices (pessary, Impressa) | Useful for management, not cure | Moderate evidence | Minimally invasive; device choice may improve symptoms | Minimal risks, some vaginal discharge/ulceration | Trial reasonable before surgery; good for those unable or unwilling to do PFMT |
| Bulking agents | Less invasive, reserved for intrinsic sphincter deficiency | Moderate evidence | Useful for patients unsuitable for surgery | Minimal complications (urinary retention, UTI) | Benefits may gradually decrease |
| Laser therapy | No significant benefit over placebo | Low evidence, warnings against routine use | None established | Not recommended outside research settings | FDA and international societies warn against routine use |
| Magnetic stimulation (EXMI) | Mixed evidence; no routine recommendation | Insufficient evidence (Level C) | Noninvasive, patient-friendly | Unknown benefit, safety profile adequate | Evidence from small, heterogeneous RCTs shows short-term improvement, but long-term and comparative benefit versus PFMT remain unclear (low-quality evidence) |
| Clinical Profile/Key Factors | Preferred First-Line Options | Possible Adjuncts or Alternatives |
|---|---|---|
| Young postpartum woman, mild–moderate SUI | Supervised PFMT; lifestyle measures (weight, constipation) | Short-term pessary; postpartum continuation of PFMT programs |
| Overweight/obese woman with SUI | PFMT plus structured weight-loss and activity program | Pessary; consider duloxetine only if surgery unsuitable and counseled |
| Postmenopausal SUI with GSM/vaginal atrophy | PFMT plus local vaginal estrogen | Pessary; bulking agents if surgery declined or contraindicated |
| SUI with mixed UI (urgency/OAB component) | PFMT for stress component; bladder training ± OAB drugs | PTNS/TTNS or SNM for refractory urgency; sling only for stress part |
| SUI in woman unfit or unwilling for surgery | Intensive supervised PFMT ± ES; pessary | Bulking agents; selected acupuncture or magnetic stimulation (adjunct only) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Poenaru, M.-O.; Ples, L.; Toma, C.-V.; Augustin, F.-E.; Sima, R.-M.; Amza, M.; Pacu, I.; Zampieri, G.; Diaconescu, A.S.; Poenaru, D. Conservative Treatment in Stress Urinary Incontinence—Narrative Literature Review. Life 2026, 16, 69. https://doi.org/10.3390/life16010069
Poenaru M-O, Ples L, Toma C-V, Augustin F-E, Sima R-M, Amza M, Pacu I, Zampieri G, Diaconescu AS, Poenaru D. Conservative Treatment in Stress Urinary Incontinence—Narrative Literature Review. Life. 2026; 16(1):69. https://doi.org/10.3390/life16010069
Chicago/Turabian StylePoenaru, Mircea-Octavian, Liana Ples, Cristian-Valentin Toma, Fernanda-Ecaterina Augustin, Romina-Marina Sima, Mihaela Amza, Irina Pacu, Giorgia Zampieri, Andrei Sebastian Diaconescu, and Daniela Poenaru. 2026. "Conservative Treatment in Stress Urinary Incontinence—Narrative Literature Review" Life 16, no. 1: 69. https://doi.org/10.3390/life16010069
APA StylePoenaru, M.-O., Ples, L., Toma, C.-V., Augustin, F.-E., Sima, R.-M., Amza, M., Pacu, I., Zampieri, G., Diaconescu, A. S., & Poenaru, D. (2026). Conservative Treatment in Stress Urinary Incontinence—Narrative Literature Review. Life, 16(1), 69. https://doi.org/10.3390/life16010069








