Predicting ICU Delirium in Critically Ill COVID-19 Patients Using Demographic, Clinical, and Laboratory Admission Data: A Machine Learning Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
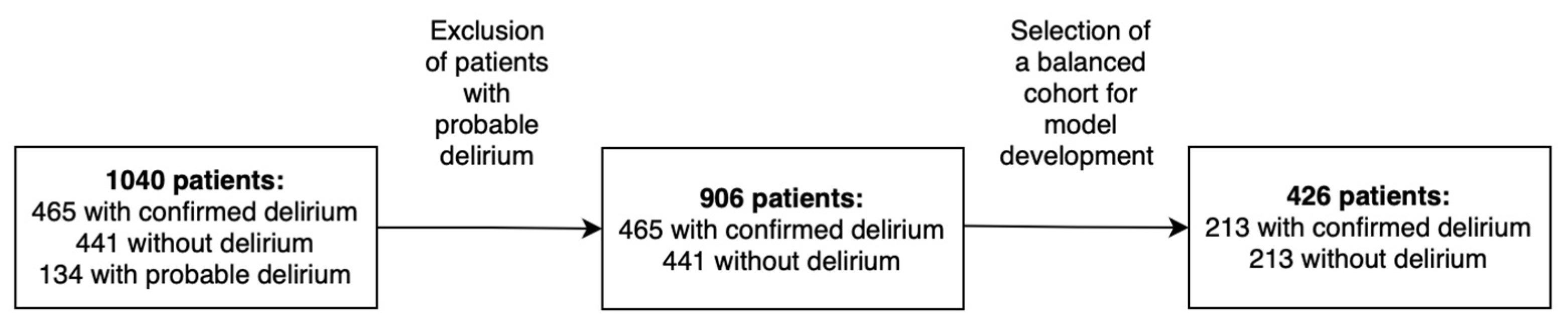
2.2. Population
2.3. Demographic, Clinical, and Laboratory Features
2.4. Collection of Biological Samples
2.5. Statistical Analysis
2.6. ML and Data Analysis
Feature Selection
- Low variability in the categorical variables:
- a.
- Criteria: categorical variables in which a single category (0 or 1) dominated more than 95% of the cases in both groups were excluded.
- b.
- Objective: to ensure that the variables exhibited sufficient variability to distinguish between the analyzed groups (delirium vs. non-delirium).
- Low frequency and absence of categorical variables:
- a.
- Criteria: variables for which one category (0 or 1) had fewer than 2 absolute occurrences in either group were removed; variables for which one category was entirely absent in one group were also excluded.
- b.
- Objective: to ensure minimal representativeness of all categorical variables in both groups to avoid statistical bias.
- High frequency of missing values in the continuous variables:
- a.
- Criteria: continuous variables with more than 30% missing values were excluded.
- b.
- Objective: to retain only variables with at least 70% valid values and to minimize the impact of missing data on modeling.
- Low variance in the continuous variables:
- a.
- Criteria: continuous variables with a variance of less than 0.01 were removed.
- b.
- Objective: to eliminate features with low dispersion, which have limited predictive value for classification between groups.
3. Results
3.1. General Characteristics of the Population at ICU Admission
3.2. Demographic, Clinical, and Laboratory ML Models
4. Discussion
4.1. Clinical and Demographic Characteristics of the Population
4.2. Performance of the Developed ML Models
4.3. Comparison with ML-Based Models
4.4. Comparison with Traditional Regression-Based Models
4.5. Factors Influencing Model Performance
4.6. Identification of Key Predictors of Delirium
4.7. Clinical Relevance
4.8. Limitations
4.9. Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Girard, T.D.; Pandharipande, P.P.; Ely, E.W. Delirium in the intensive care unit. Crit. Care 2008, 12, S3. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Cui, W.; Ding, S.; Li, X.; Zhang, X.W.; Wu, Y. A cluster-randomized controlled trial of a nurse-led artificial intelligence assisted prevention and management for delirium (AI-AntiDelirium) on delirium in intensive care unit: Study protocol. PLoS One 2024, 19, e0298793. [Google Scholar] [CrossRef] [PubMed]
- Al Huraizi, A.R.; Al-Maqbali, J.S.; Al Farsi, R.S.; Al Zeedy, K.; Al-Saadi, T.; Al-Hamadani, N.; Al Alawi, A.M. Delirium and Its Association with Short- and Long-Term Health Outcomes in Medically Admitted Patients: A Prospective Study. J. Clin. Med. 2023, 12, 5346. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Dziegielewski, C.; Skead, C.; Canturk, T.; Webber, C.; Fernando, S.M.; Thompson, L.H.; Foster, M.; Ristovic, V.; Lawlor, P.G.; Chaudhuri, D.; et al. Delirium and Associated Length of Stay and Costs in Critically Ill Patients. Crit. Care Res. Pract. 2021, 2021, 6612187. [Google Scholar] [CrossRef]
- Leslie, D.L.; Inouye, S.K. The Importance of Delirium: Economic and Societal Costs. J. Am. Geriatr. Soc. 2011, 59, S241–S243. [Google Scholar] [CrossRef]
- Abdelbaky, A.M.; Eldelpshany, M.S. Patient Outcomes and Management Strategies for Intensive Care Unit (ICU)-Associated Delirium: A Literature Review. Cureus 2024, 16, e61527. [Google Scholar] [CrossRef]
- Page, V.J.; Ely, E.W. Delirium in Critical Care, 1st ed.; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Ely, E.W.; Shintani, A.; Truman, B.; Speroff, T.; Gordon, S.M.; Harrell, F.E.; Inouye, S.K.; Bernard, G.R.; Dittus, R.S. Delirium as a Predictor of Mortality in Mechanically Ventilated Patients in the Intensive Care Unit. JAMA 2004, 291, 1753–1762. [Google Scholar] [CrossRef]
- Vasilevskis, E.E.; Chandrasekhar, R.; Holtze, C.H.; Graves, J.; Speroff, T.; Girard, T.D.; Patel, M.B.; Hughes, C.G.; Cao, A.; Pandharipande, P.P.; et al. The cost of ICU delirium and coma in the intensive care unit patient. Med. Care 2018, 56, 890–897. [Google Scholar] [CrossRef]
- Goldberg, T.E.; Chen, C.; Wang, Y.; Jung, E.; Swanson, A.; Ing, C.; Garcia, P.S.; Whittington, R.A.; Moitra, V. Association of Delirium With Long-term Cognitive Decline: A Meta-analysis. JAMA Neurol. 2020, 77, 1373–1381. [Google Scholar] [CrossRef]
- Inouye, S.K.; Westendorp, R.G.J.; Saczynski, J.S. Delirium in elderly people. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef]
- Girard, T.D.; Jackson, J.C.; Pandharipande, P.P.; Pun, B.T.; Thompson, J.L.; Shintani, A.K.; Gordon, S.M.; Canonico, A.E.; Dittus, R.S.; Bernard, G.R.; et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit. Care Med. 2010, 38, 1513–1520. [Google Scholar] [CrossRef] [PubMed]
- Devlin, J.W.; Needham, D.M. Long-term outcomes after Delirium in the ICU: Addressing gaps in our knowledge. Am. J. Respir. Crit. Care Med. 2021, 204, 383–385. [Google Scholar] [CrossRef] [PubMed]
- Pereira, J.V.B.; Aung Thein, M.Z.; Nitchingham, A.; Caplan, G.A. Delirium in older adults is associated with development of new dementia: A systematic review and meta-analysis. Int. J. Geriatr. Psychiatry 2021, 36, 993–1003. [Google Scholar] [CrossRef] [PubMed]
- Oh-Park, M.; Chen, P.; Romel-Nichols, V.; Hreha, K.; Boukrina, O.; Barrett, A.M. Delirium screening and management in inpatient rehabilitation facilities. Am. J. Phys. Med. Rehabil. 2018, 97, 754. [Google Scholar] [CrossRef]
- Cheng, H.; Huang, X.; Yuan, S.; Song, S.; Tang, Y.; Ling, Y.; Tan, S.; Wang, Z.; Zhou, F.; Lyu, J. Can admission Braden skin score predict delirium in older adults in the intensive care unit? Results from a multicenter study. J. Clin. Nurs. 2024, 33, 2209–2225. [Google Scholar] [CrossRef]
- Oosterhoff, J.H.F.; Karhade, A.V.; Oberai, T.; Franco-Garcia, E.; Doornberg, J.N.; Schwab, J.H. Prediction of Postoperative Delirium in Geriatric Hip Fracture Patients: A Clinical Prediction Model Using Machine Learning Algorithms. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 1–10. [Google Scholar] [CrossRef]
- Fick, D.M.; Auerbach, A.D.; Avidan, M.S.; Busby-Whitehead, J.; Ely, E.W.; Jones, R.N.; Marcantonio, E.R.; Needham, D.M.; Pandharipande, P.; Robinson, T.N.; et al. Network for Investigation of Delirium across the U.S.: Advancing the Field of Delirium with a New Interdisciplinary Research Network. J. Am. Geriatr. Soc. 2017, 65, 2158–2160. [Google Scholar] [CrossRef]
- Ospina, J.P.; King, F.; Madva, E.; Celano, C.M. Clinical Medicine and Therapeutics REVIEW Epidemiology, Mechanisms, Diagnosis, and Treatment of Delirium: A Narrative Review. Clin. Med. Ther. 2018, 1, 3. [Google Scholar] [CrossRef]
- Alexander, S.K.; Needham, E. Diagnosis of delirium: A practical approach. Pract. Neurol. 2023, 23, 192–199. [Google Scholar] [CrossRef]
- Fong, T.G.; Tulebaev, S.R.; Inouye, S.K. Delirium in elderly adults: Diagnosis, prevention and treatment. Nat. Rev. Neurol. 2009, 5, 210. [Google Scholar] [CrossRef]
- Guenther, U.; Weykam, J.; Andorfer, U.; Theuerkauf, N.; Popp, J.; Ely, E.W.; Putensen, C. Implications of Objective vs Subjective Delirium Assessment in Surgical Intensive Care Patients. Am. J. Crit. Care 2012, 21, e12–e20. [Google Scholar] [CrossRef] [PubMed]
- Moss, S.J.; Lee, C.H.; Doig, C.J.; Whalen-Browne, L.; Stelfox, H.T.; Fiest, K.M. Delirium diagnosis without a gold standard: Evaluating diagnostic accuracy of combined delirium assessment tools. PLoS One 2022, 17, e0267110. [Google Scholar] [CrossRef] [PubMed]
- Gusmao-Flores, D.; Figueira Salluh, J.I.; Chalhub, R.T.; Quarantini, L.C. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: A systematic review and meta-analysis of clinical studies. Crit. Care 2012, 16, R115. [Google Scholar] [CrossRef]
- Brummel, N.E.; Vasilevskis, E.E.; Han, J.H.; Boehm, L.; Pun, B.T.; Ely, E.W. Implementing Delirium Screening in the Intensive Care Unit: Secrets to Success. Crit. Care Med. 2013, 41, 2196. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, Z.; Li, Y.; Ge, N.; Yue, J. Detecting delirium: A systematic review of ultrabrief identification instruments for hospital patients. Front. Psychol. 2023, 14, 1166392. [Google Scholar] [CrossRef]
- Lian, F.; Li, F.; Tang, X.; Yuan, Y. Risk factors for hypoactive delirium in patients with non-traumatic ARDS: A prospective, observational study. Sci. Rep. 2024, 14, 6980. [Google Scholar] [CrossRef]
- Van Eijk, M.M.; Van Den Boogaard, M.; Van Marum, R.J.; Benner, P.; Eikelenboom, P.; Honing, M.L.; Van Der Hoven, B.; Horn, J.; Izaks, G.J.; Kalf, A.; et al. Routine Use of the Confusion Assessment Method for the Intensive Care Unit. Am. J. Respir. Crit. Care Med. 2012, 184, 340–344. [Google Scholar] [CrossRef]
- Bhattacharyya, A.; Sheikhalishahi, S.; Torbic, H.; Yeung, W.; Wang, T.; Birst, J.; Duggal, A.; Celi, L.A.; Osmani, V. Delirium prediction in the ICU: Designing a screening tool for preventive interventions. JAMIA Open 2022, 5, ooac048. [Google Scholar] [CrossRef]
- Strating, T.; Shafiee Hanjani, L.; Tornvall, I.; Hubbard, R.; Scott, I.A. Navigating the machine learning pipeline: A scoping review of inpatient delirium prediction models. BMJ Health Care Inform. 2023, 30, 100767. [Google Scholar] [CrossRef]
- Ruppert, M.M.; Lipori, J.; Patel, S.; Ingersent, E.; Cupka, J.; Ozrazgat-Baslanti, T.; Loftus, T.; Rashidi, P.; Bihorac, A. ICU Delirium Prediction Models: A Systematic Review. Crit. Care Explor. 2020, 2, e296. [Google Scholar] [CrossRef]
- Mattar, I.; Fai Chan, M.; Childs, C.; Llompart-Pou, A.; Stover, J.F. Risk Factors for Acute Delirium in Critically Ill Adult Patients: A Systematic Review. Int. Sch. Res. Notices 2013, 2013, 910125. [Google Scholar] [CrossRef]
- Hughes, C.G.; Pandharipande, P.P.; Ely, E.W. Acute Brain Dysfunction in the Critically Ill, 1st ed.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Rahimi-Bashar, F.; Abolhasani, G.; Manouchehrian, N.; Jiryaee, N.; Vahedian-Azimi, A.; Sahebkar, A. Incidence and Risk Factors of Delirium in the Intensive Care Unit: A Prospective Cohort. Biomed. Res. Int. 2021, 2021, 6219678. [Google Scholar] [CrossRef] [PubMed]
- Zhong, X.; Lin, J.Y.; Li, L.; Barrett, A.M.; Poeran, J.; Mazumdar, M. Derivation and validation of a novel comorbidity-based delirium risk index to predict postoperative delirium using national administrative healthcare database. Health Serv. Res. 2021, 56, 154–165. [Google Scholar] [CrossRef] [PubMed]
- Fong, T.G.; Inouye, S.K. The inter-relationship between delirium and dementia: The importance of delirium prevention. Nat. Rev. Neurol. 2022, 18, 579. [Google Scholar] [CrossRef] [PubMed]
- Erbay Dalli, Ö.; Kelebek Girgin, N.; Kahveci, F. Incidence, characteristics and risk factors of delirium in the intensive care unit: An observational study. J. Clin. Nurs. 2023, 32, 96–105. [Google Scholar] [CrossRef]
- Jin, T.; Jin, Y.; Lee, S.M. Medication Use and Risk of Delirium in Mechanically Ventilated Patients. Clin. Nurs. Res. 2019, 30, 474–481. [Google Scholar] [CrossRef]
- Khan, S.H.; Lindroth, H.; Perkins, A.J.; Jamil, Y.; Wang, S.; Roberts, S.; Farber, M.; Rahman, O.; Gao, S.; Marcantonio, E.R.; et al. Delirium Incidence, Duration, and Severity in Critically Ill Patients With Coronavirus Disease 2019. Crit. Care Explor. 2020, 2, E0290. [Google Scholar] [CrossRef]
- Van Den Boogaard, M.; Pickkers, P.; Slooter, A.J.C.; Kuiper, M.A.; Spronk, P.E.; Van Der Voort, P.H.J.; Van Der Hoeven, J.G.; Donders, R.; Van Achterberg, T.; Schoonhoven, L. Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for intensive care patients: Observational multicentre study. BMJ 2012, 344, 17. [Google Scholar] [CrossRef]
- Wassenaar, A.; van den Boogaard, M.; van Achterberg, T.; Slooter, A.J.C.; Kuiper, M.A.; Hoogendoorn, M.E.; Simons, K.S.; Maseda, E.; Pinto, N.; Jones, C.; et al. Multinational development and validation of an early prediction model for delirium in ICU patients. Intensive Care Med. 2015, 41, 1048–1056. [Google Scholar] [CrossRef]
- Lv, S.; Li, J.; He, H.; Zhao, Q.; Jiang, Y. Artificial Intelligence Applications in Delirium Prediction, Diagnosis, and Management: A Systematic Review. Artif. Intell. Rev. 2025, 58, 269. [Google Scholar] [CrossRef]
- Hur, S.; Ko, R.E.; Yoo, J.; Ha, J.; Cha, W.C.; Chung, C.R. A machine learning-based algorithm for the prediction of intensive care unit delirium (PRIDE): Retrospective study. JMIR Med. Inform. 2021, 9, e23401. [Google Scholar] [CrossRef]
- Esumi, R.; Funao, H.; Kawamoto, E.; Sakamoto, R.; Ito-Masui, A.; Okuno, F.; Shinkai, T.; Hane, A.; Ikejiri, K.; Akama, Y.; et al. Machine Learning–Based Prediction of Delirium and Risk Factor Identification in Intensive Care Unit Patients With Burns: Retrospective Observational Study. JMIR Form. Res. 2025, 9, e65190. [Google Scholar] [CrossRef]
- Park, W.R.; Kim, H.R.; Park, J.Y.; Kim, H.E.; Cho, J.; Oh, J. Potential Usefulness of Blood Urea Nitrogen to Creatinine Ratio in the Prediction and Early Detection of Delirium Motor Subtype in the Intensive Care Unit. J. Clin. Med. 2022, 11, 5073. [Google Scholar] [CrossRef] [PubMed]
- Davoudi, A.; Ozrazgat-Baslanti, T.; Ebadi, A.; Bursian, A.C.; Bihorac, A.; Rashidi, P. Delirium Prediction using Machine Learning Models on Preoperative Electronic Health Records Data. Proc. IEEE Int. Symp. Bioinformatics Bioeng. 2017, 568–573. [Google Scholar] [CrossRef]
- Oh, J.; Cho, D.; Park, J.; Na, S.H.; Kim, J.; Heo, J.; Shin, C.S.; Kim, J.J.; Park, J.Y.; Lee, B. Prediction and early detection of delirium in the intensive care unit by using heart rate variability and machine learning. Physiol. Meas. 2018, 39, 035004. [Google Scholar] [CrossRef] [PubMed]
- Rollo, E.; Marotta, J.; Callea, A.; Brunetti, V.; Vollono, C.; Scala, I.; Imperatori, C.; Frisullo, G.; Broccolini, A.; Della Marca, G. Heart rate variability and delirium in acute non-cardioembolic stroke: A prospective, cross-sectional, cohort study. Neurol. Sci. 2021, 43, 2423. [Google Scholar] [CrossRef] [PubMed]
- Jalali, A.; Alvarez-Iglesias, A.; Roshan, D.; Newell, J. Visualising statistical models using dynamic nomograms. PLoS ONE 2019, 14, e0225253. [Google Scholar] [CrossRef]
- Kim, H.; Kim, M.; Kim, D.Y.; Seo, D.G.; Hong, J.M.; Yoon, D. Prediction of delirium occurrence using machine learning in acute stroke patients in intensive care unit. Front. Neurosci. 2024, 18, 1425562. [Google Scholar] [CrossRef]
- Ren, Y.; Zhang, Y.; Zhan, J.; Sun, J.; Luo, J.; Liao, W.; Cheng, X. Machine learning for prediction of delirium in patients with extensive burns after surgery. CNS Neurosci. Ther. 2023, 29, 2986. [Google Scholar] [CrossRef]
- Fang, Y.; Tang, X.; Gao, Y.; Xie, H.; Shen, Y.; Peng, M.; Liu, J.; Zhang, Y.; Cui, Y.; Xie, K. Association Between Blood Urea Nitrogen and Delirium in Critically Ill Elderly Patients Without Kidney Diseases: A Retrospective Study and Mendelian Randomization Analysis. CNS Neurosci. Ther. 2025, 31, e70201. [Google Scholar] [CrossRef]
- Seo, C.L.; Park, J.Y.; Park, J.; Kim, H.E.; Cho, J.; Seok, J.H.; Kim, J.J.; Shin, C.S.; Oh, J. Neutrophil-Lymphocyte Ratio as a Potential Biomarker for Delirium in the Intensive Care Unit. Front. Psychiatry 2021, 12, 729421. [Google Scholar] [CrossRef] [PubMed]
- Park, H.Y.; Sohn, H.; Hong, A.; Han, S.W.; Jang, Y.; Yoon, E.k.K.; Kim, M.; Park, H.Y. Application of machine learning for delirium prediction and analysis of associated factors in hospitalized COVID-19 patients: A comparative study using the Korean Multidisciplinary cohort for delirium prevention (KoMCoDe). Int. J. Med. Inform. 2025, 195, 105747. [Google Scholar] [CrossRef] [PubMed]
- Denke, C.; Balzer, F.; Menk, M.; Szur, S.; Brosinsky, G.; Tafelski, S.; Wernecke, K.D.; Deja, M. Long-term sequelae of acute respiratory distress syndrome caused by severe community-acquired pneumonia: Delirium-associated cognitive impairment and post-traumatic stress disorder. J. Int. Med. Res. 2018, 46, 2265–2283. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Hur, H.J.; Kim, S.N.; Ahn, J.H.; Ro, D.H.; Hong, A.; Park, H.Y.; Choe, P.G.; Kim, B.; Park, H.Y. Predicting delirium and the effects of medications in hospitalized COVID-19 patients using machine learning: A retrospective study within the Korean Multidisciplinary Cohort for Delirium Prevention (KoMCoDe). Digit. Health 2024, 10, 20552076231223812. [Google Scholar] [CrossRef]
- Lindroth, H.; Liu, K.; Szalacha, L.; Ashkenazy, S.; Bellelli, G.; van den Boogaard, M.; Caplan, G.; Chung, C.R.; Elhadi, M.; Gurjar, M.; et al. World delirium awareness and quality survey in 2023—a worldwide point prevalence study. Age Ageing 2024, 53, 31. [Google Scholar] [CrossRef]
- Wong, A.; Young, A.T.; Liang, A.S.; Gonzales, R.; Douglas, V.C.; Hadley, D. Development and Validation of an Electronic Health Record–Based Machine Learning Model to Estimate Delirium Risk in Newly Hospitalized Patients Without Known Cognitive Impairment. JAMA Netw. Open 2018, 1, e181018. [Google Scholar] [CrossRef]
- Contreras, M.; Kapoor, S.; Zhang, J.; Davidson, A.; Ren, Y.; Guan, Z.; Ozrazgat-Baslanti, T.; Nerella, S.; Bihorac, A.; Rashidi, P. DeLLiriuM: A large language model for delirium prediction in the ICU using structured EHR. arXiv 2024, arXiv:2410.17363. [Google Scholar]
- Gong, K.D.; Lu, R.; Bergamaschi, T.S.; Sanyal, A.; Guo, J.; Kim, H.B.; Nguyen, H.T.; Greenstein, J.L.; Winslow, R.L.; Stevens, R.D. Predicting Intensive Care Delirium with Machine Learning: Model Development and External Validation. Anesthesiology 2023, 138, 299–311. [Google Scholar] [CrossRef]
- Li, H.; Zang, Q.; Li, Q.; Lin, Y.; Duan, J.; Huang, J.; Hu, H.; Zhang, Y.; Xia, D.; Zhou, M. Development of a machine learning-based predictive model for postoperative delirium in elderly intensive care unit patients: Retrospective Study. J. Med. Internet Res. 2025, 27, e67258. [Google Scholar] [CrossRef]
- Dylan, F.; Byrne, G.; Mudge, A.M. Delirium risk in non-surgical patients: Systematic review of predictive tools. Arch. Gerontol. Geriatr. 2019, 83, 292–302. [Google Scholar] [CrossRef]
- Wong, C.K.; Van Munster, B.C.; Hatseras, A.; Huis In ’TVeld, E.; Van Leeuwen, B.L.; De Rooij, S.E.; Pleijhuis, R.G. Head-to-head comparison of 14 prediction models for postoperative delirium in elderly non-ICU patients: An external validation study. BMJ Open 2022, 12, e054023. [Google Scholar] [CrossRef] [PubMed]
- Mi, J.X.; Li, A.D.; Zhou, L.F. Review study of interpretation methods for future interpretable machine learning. IEEE Access 2020, 8, 191969–191985. [Google Scholar] [CrossRef]
- Matumoto, K.; Nohara, Y.; Sakaguchi, M.; Takayama, Y.; Fukushige, S.; Soejima, H.; Nakashima, N. Delirium Prediction Using Machine Learning Interpretation Method and Its Incorporation into a Clinical Workflow. Appl. Sci. 2023, 13, 1564. [Google Scholar] [CrossRef]
- Demšar, J.; Curk, T.; Erjavec, A.; Črt Gorup; Hočevar, T.; Milutinovič, M.; Možina, M.; Polajnar, M.; Toplak, M.; Staric, A.; et al. Orange: Data Mining Toolbox in Python Tomaž Curk Matija Polajnar Laň Zagar. J. Mach. Learn. Res. 2013, 14, 2349–2353. [Google Scholar]
- Ely, E.W.; Inouye, S.K.; Bernard, G.R.; Gordon, S.; Francis, J.; May, L.; Truman, B.; Speroff, T.; Gautam, S.; Margolin, R.; et al. Delirium in Mechanically Ventilated Patients Validity and Reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). JAMA 2001, 286, 2703–2719. [Google Scholar] [CrossRef]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef]
- Taheri, S.; Mammadov, M. Learning the naive bayes classifier with optimization models. Int. J. Appl. Math. Comput. Sci. 2013, 23, 787–795. [Google Scholar] [CrossRef]
- Krishnan, S. Machine learning for biomedical signal analysis. In Biomedical Signal Analysis for Connected Healthcare; Academic Press: Cambridge, MA, USA, 2021; pp. 223–264. [Google Scholar] [CrossRef]
- Marneni, D.; Vemula, S. Analysis of COVID-19 using machine learning techniques. In Statistical Modeling in Machine Learning: Concepts and Applications; Academic Press: Cambridge, MA, USA, 2023; pp. 37–53. [Google Scholar] [CrossRef]
- Das, A. Logistic Regression. In Encyclopedia of Quality of Life and Well-Being Research; Springer: Cham, Switzerland, 2023; pp. 3985–3986. [Google Scholar] [CrossRef]
- Zollanvari, A. Decision Trees. In Machine Learning with Python; Springer: Cham, Switzerland, 2023; pp. 187–207. [Google Scholar] [CrossRef]
- Shmilovici, A. Support Vector Machines. In Machine Learning for Data Science Handbook: Data Mining and Knowledge Discovery Handbook, 3rd ed.; Springer: Cham, Switzerland, 2023; pp. 93–110. [Google Scholar] [CrossRef]
- Berk, R.A. Random Forests. In Statistical Learning from a Regression Perspective, 3rd ed.; Springer: Cham, Switzerland, 2020; pp. 233–295. [Google Scholar] [CrossRef]
- Sun, Z.; Wang, G.; Li, P.; Wang, H.; Zhang, M.; Liang, X. An improved random forest based on the classification accuracy and correlation measurement of decision trees. Expert. Syst. Appl. 2024, 237, 121549. [Google Scholar] [CrossRef]
- Salama, M.A.; Hassan, G. A Novel Feature Selection Measure Partnership-Gain. Int. J. Online Biomed. Eng. (IJOE) 2019, 15, 4–19. [Google Scholar] [CrossRef]
- Fahrudy, D.; Uyun, S. Classification of Student Graduation using Naïve Bayes by Comparing between Random Oversampling and Feature Selections of Information Gain and Forward Selection. JOIV Int. J. Inform. Vis. 2022, 6, 798–808. [Google Scholar] [CrossRef]
- Singh, P.; Singh, N.; Singh, K.K.; Singh, A. Diagnosing of disease using machine learning. In Machine Learning and the Internet of Medical Things in Healthcare; Academic Press: Cambridge, MA, USA, 2021; pp. 89–111. [Google Scholar] [CrossRef]
- Vellido, A. The importance of interpretability and visualization in machine learning for applications in medicine and health care. Neural Comput. Applic 2020, 32, 18069–18083. [Google Scholar] [CrossRef]
- Wang, J.W.D. Naïve Bayes is an interpretable and predictive machine learning algorithm in predicting osteoporotic hip fracture in-hospital mortality compared to other machine learning algorithms. PLoS Digit. Health 2025, 4, e0000529. [Google Scholar] [CrossRef] [PubMed]
- Van Gelder, T.G.; van Diem-Zaal, I.J.; Dijkstra-Kersten, S.M.A.; de Mul, N.; Lalmohamed, A.; Slooter, A.J.C. The risk of delirium after sedation with propofol or midazolam in intensive care unit patients. Br. J. Clin. Pharmacol. 2024, 90, 1471–1479. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhou, Y.; Kang, Y.; Xu, B.; Wang, P.; Lv, Y.; Wang, Z. Risk Factors of Delirium in Sequential Sedation Patients in Intensive Care Units. Biomed Res. Int. 2017, 2017, 3539872. [Google Scholar] [CrossRef] [PubMed]
- Viegas, A.; Araújo, R.; Ramalhete, L.; Von Rekowski, C.; Fonseca, T.A.H.; Bento, L.; Calado, C.R.C. Discovery of Delirium Biomarkers through Minimally Invasive Serum Molecular Fingerprinting. Metabolites 2024, 14, 301. [Google Scholar] [CrossRef]
- Kotfis, K.; Williams Roberson, S.; Wilson, J.E.; Dabrowski, W.; Pun, B.T.; Ely, E.W. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit. Care 2020, 24, 176. [Google Scholar] [CrossRef]
- Krupa, S.; Friganovic, A.; Mędrzycka-Dabrowska, W. Occurrence of delirium during ecmo therapy in a critical care unit in poland—A cross-sectional pilot study. Int. J. Environ. Res. Public Health 2021, 18, 4029. [Google Scholar] [CrossRef]
- Smonig, R.; Wallenhorst, T.; Bouju, P.; Letheulle, J.; Le Tulzo, Y.; Tadié, J.M.; Gacouin, A. Constipation is independently associated with delirium in critically ill ventilated patients. Intensive Care Med. 2016, 42, 126–127. [Google Scholar] [CrossRef]
- Ticinesi, A.; Parise, A.; Nouvenne, A.; Cerundolo, N.; Prati, B.; Meschi, T. The possible role of gut microbiota dysbiosis in the pathophysiology of delirium in older persons. Microbiome Res. Rep. 2023, 2, 19. [Google Scholar] [CrossRef]
- Ohl, I.C.B.; Chavaglia, S.R.R.; Ohl, R.I.B.; Lopes, M.C.B.T.; Campanharo, C.R.V.; Okuno, M.F.P.; Batista, R.E.A. Evaluation of delirium in aged patients assisted at emergency hospital service. Rev. Bras. Enferm. 2019, 72, 153–160. [Google Scholar] [CrossRef]
- Li, H.-R.; Guo, Y. High-risk factors for delirium in severely ill patients and the application of emotional nursing combined with pain nursing. World J. Psychiatry 2024, 14, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- Kotfis, K.; Szylińska, A.; Listewnik, M.; Brykczyński, M.; Ely, E.W.; Rotter, I. Diabetes and elevated preoperative HbA1c level as risk factors for postoperative delirium after cardiac surgery: An observational cohort study. Neuropsychiatr. Dis. Treat. 2019, 15, 511–521. [Google Scholar] [CrossRef] [PubMed]
- Kong, D.; Luo, W.; Zhu, Z.; Sun, S.; Zhu, J. Factors associated with post-operative delirium in hip fracture patients: What should we care. Eur. J. Med. Res. 2022, 27, 40. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.C.; Swisher, C.L.; Chung, C.; Jaffray, D.; Sidey-Gibbons, C. On the importance of interpretable machine learning predictions to inform clinical decision making in oncology. Front. Oncol. 2023, 13, 1129380. [Google Scholar] [CrossRef]
- Wallace, M.L.; Mentch, L.; Wheeler, B.J.; Tapia, A.L.; Richards, M.; Zhou, S.; Yi, L.; Redline, S.; Buysse, D.J. Use and misuse of random forest variable importance metrics in medicine: Demonstrations through incident stroke prediction. BMC Med. Res. Methodol. 2023, 23, 144. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Erion, G.; Chen, H.; DeGrave, A.; Prutkin, J.M.; Nair, B.; Katz, R.; Himmelfarb, J.; Bansal, N.; Lee, S.-I. Explainable AI for Trees: From Local Explanations to Global Understanding. Nat. Mach. Intell. 2020, 2, 56–67. [Google Scholar] [CrossRef]
- Petkovic, D.; Altman, R.; Wong, M.; Vigil, A. Improving the explainability of Random Forest classifier—User centered approach. Pac. Symp. Biocomput. 2018, 23, 204. [Google Scholar] [CrossRef]
- Gao, X.; Alam, S.; Shi, P.; Dexter, F.; Kong, N. Interpretable machine learning models for hospital readmission prediction: A two-step extracted regression tree approach. BMC Med. Inform. Decis. Mak. 2023, 23, 104. [Google Scholar] [CrossRef]
- Heinrich, M.; Woike, J.K.; Spies, C.D.; Wegwarth, O. Forecasting Postoperative Delirium in Older Adult Patients with Fast-and-Frugal Decision Trees. J. Clin. Med. 2022, 11, 5629. [Google Scholar] [CrossRef]
- Amerongen Hvan, N.; Stapel, S.; Spijkstra, J.J.; Ouweneel, D.; Schenk, J. Comparison of Prognostic Accuracy of 3 Delirium Prediction Models. Am. J. Crit. Care 2023, 32, 43–50. [Google Scholar] [CrossRef]
- Ko, R.-E.; Lee, J.; Kim, S.; Ahn, J.H.; Na, S.J.; Yang, J.H. Machine learning methods for developing a predictive model of the incidence of delirium in cardiac intensive care units. Rev. Española Cardiol. (Engl. Ed.) 2024, 77, 547–555. [Google Scholar] [CrossRef]
- Pudjihartono, N.; Fadason, T.; Kempa-Liehr, A.W.; O’Sullivan, J.M. A Review of Feature Selection Methods for Machine Learning-Based Disease Risk Prediction. Front. Bioinform. 2022, 2, 927312. [Google Scholar] [CrossRef] [PubMed]
- Rudin, C. Stop Explaining Black Box Machine Learning Models for High Stakes Decisions and Use Interpretable Models Instead. Nat. Mach. Intell. 2018, 1, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Tonekaboni, S.; Joshi, S.; McCradden, M.D.; Goldenberg, A. What Clinicians Want: Contextualizing Explainable Machine Learning for Clinical End Use. Proc. Mach. Learn. Res. 2019, 106, 359–380. [Google Scholar]
- Elshawi, R.; Al-Mallah, M.H.; Sakr, S. On the interpretability of machine learning-based model for predicting hypertension. BMC Med. Inform. Decis. Mak. 2019, 19, 146. [Google Scholar] [CrossRef]
- Liu, S.; Schlesinger, J.J.; McCoy, A.B.; Reese, T.J.; Steitz, B.; Russo, E.; Koh, B.; Wright, A. New onset delirium prediction using machine learning and long short-Term memory (LSTM) in electronic health record. J. Am. Med. Inform. Assoc. 2023, 30, 120–131. [Google Scholar] [CrossRef]
- Tang, D.; Ma, C.; Xu, Y. Interpretable machine learning model for early prediction of delirium in elderly patients following intensive care unit admission: A derivation and validation study. Front. Med. 2024, 11, 1399848. [Google Scholar] [CrossRef]
- Nagata, C.; Hata, M.; Miyazaki, Y.; Masuda, H.; Wada, T.; Kimura, T.; Fujii, M.; Sakurai, Y.; Matsubara, Y.; Yoshida, K.; et al. Development of postoperative delirium prediction models in patients undergoing cardiovascular surgery using machine learning algorithms. Sci. Rep. 2023, 13, 21090. [Google Scholar] [CrossRef]
- Cherak, S.J.; Soo, A.; Brown, K.N.; Wesley Ely, E.; Stelfox, H.T.; Fiest, K.M. Development and validation of delirium prediction model for critically ill adults parameterized to ICU admission acuity. PLoS ONE 2020, 15, e0237639. [Google Scholar] [CrossRef]
- Hassija, V.; Chamola, V.; Mahapatra, A.; Singal, A.; Goel, D.; Huang, K.; Scardapane, S.; Spinelli, I.; Mahmud, M.; Hussain, A. Interpreting Black-Box Models: A Review on Explainable Artificial Intelligence. Cognit. Comput. 2024, 16, 45–74. [Google Scholar] [CrossRef]
- Chen, Y.; Du, H.; Wei, B.H.; Chang, X.N.; Dong, C.M. Development and validation of risk-stratification delirium prediction model for critically ill patients. Medicine 2017, 96, e7543. [Google Scholar] [CrossRef] [PubMed]
- Alhamzawi, R.; Ali, H.T.M. The Bayesian adaptive lasso regression. Math. Biosci. 2018, 303, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.; Hastie, T.; Tibshirani, R. Regularization Paths for Generalized Linear Models via Coordinate Descent. J. Stat. Softw. 2010, 33, 1. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Wang, X. A Feature Selection Method Based on Competition Winners Mechanism. In Proceedings of the 2015 International Power, Electronics and Materials Engineering Conference, Dalian, China, 16–17 May 2015; Volume 17, pp. 638–643. [Google Scholar] [CrossRef]
- Fan, H.; Ji, M.; Huang, J.; Yue, P.; Yang, X.; Wang, C.; Ying, W. Development and validation of a dynamic delirium prediction rule in patients admitted to the Intensive Care Units (DYNAMIC-ICU): A prospective cohort study. Int. J. Nurs. Stud. 2019, 93, 64–73. [Google Scholar] [CrossRef]
- Kim, J.H.; Hua, M.; Whittington, R.A.; Lee, J.; Liu, C.; Ta, C.N.; Marcantonio, E.R.; Goldberg, T.E.; Weng, C. A machine learning approach to identifying delirium from electronic health records. JAMIA Open 2022, 5, ooac042. [Google Scholar] [CrossRef]
- Andrade, C. Sample Size and its Importance in Research. Indian J. Psychol. Med. 2020, 42, 102. [Google Scholar] [CrossRef]
- Li, Q.; Li, J.; Chen, J.; Zhao, X.; Zhuang, J.; Zhong, G.; Song, Y.; Lei, L. A machine learning-based prediction model for postoperative delirium in cardiac valve surgery using electronic health records. BMC Cardiovasc. Disord. 2024, 24, 66. [Google Scholar] [CrossRef]
- Ghasemzadeh, H.; Hillman, R.E.; Mehta, D.D. Toward Generalizable Machine Learning Models in Speech, Language, and Hearing Sciences: Estimating Sample Size and Reducing Overfitting. J. Speech Lang. Hear. Res. 2023, 67, 753–781. [Google Scholar] [CrossRef]
- Park, S.Y.; Lee, H.B. Prevention and management of delirium in critically ill adult patients in the intensive care unit: A review based on the 2018 PADIS guidelines. Acute Crit. Care 2019, 34, 117–125. [Google Scholar] [CrossRef]
- Liu, S.B.; Wu, H.Y.; Duan, M.L.; Yang, R.L.; Ji, C.H.; Liu, J.J.; Zhao, H. Delirium in the ICU: How much do we know? A narrative review. Ann. Med. 2024, 56, 2405072. [Google Scholar] [CrossRef]
- Pun, B.; Devlin, J. Delirium monitoring in the ICU: Strategies for initiating and sustaining screening efforts. Semin. Respir. Crit. Care Med. 2013, 34, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Eldean, T.N.N.; Bakri, M.H.; Aziz, M.A.A.; Khalaf, G.S. Effectiveness of the ABCDEF Bundle to Manage and Prevent Delirium Pre- and Postintervention Quasi-Experimental Study. Crit. Care Nurs. Q. 2024, 47, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.H.; Lee, J.J.; Lai, P.C.K.; Li, P.W.C. Prevalence of delirium among critically ill patients who received extracorporeal membrane oxygenation therapy: A systematic review and proportional meta-analysis. Intensive Crit. Care Nurs. 2023, 79, 103498. [Google Scholar] [CrossRef]
- Kalra, A.; Kang, J.K.; Khanduja, S.; Menta, A.K.; Ahmad, S.A.; Liu, O.; Rodriguez, E.; Spann, M.; Hernandez, A.V.; Brodie, D.; et al. Long-Term Neuropsychiatric, Neurocognitive and Functional Outcomes of Patients Receiving ECMO: A Systematic Review and Meta-Analysis. Neurology 2024, 102, e208081. [Google Scholar] [CrossRef] [PubMed]
- Fernando, S.M.; Scott, M.; Talarico, R.; Fan, E.; McIsaac, D.I.; Sood, M.M.; Myran, D.T.; Herridge, M.S.; Needham, D.M.; Hodgson, C.L.; et al. Association of Extracorporeal Membrane Oxygenation with New Mental Health Diagnoses in Adult Survivors of Critical Illness. JAMA 2022, 328, 1827–1836. [Google Scholar] [CrossRef]
- Al-Hoodar, R.K.; Lazarus, E.R.; Al Omari, O.; Al Zaabi, O. Incidence, Associated Factors, and Outcome of Delirium among Patients Admitted to ICUs in Oman. Crit. Care Res. Pract. 2022, 2022, 4692483. [Google Scholar] [CrossRef]
- Cui, Z.; Fritz, B.A.; King, C.R.; Avidan, M.S.; Chen, Y. A Factored Generalized Additive Model for Clinical Decision Support in the Operating Room. AMIA Annu. Symp. Proc. 2020, 2019, 343–352. [Google Scholar]
- Siragusa, L.; Angelico, R.; Angrisani, M.; Zampogna, B.; Materazzo, M.; Sorge, R.; Giordano, L.; Meniconi, R.; Coppola, A.; SPIGC Survey Collaborative Group. How future surgery will benefit from SARS-CoV-2-related measures: A SPIGC survey conveying the perspective of Italian surgeons. Updates Surg. 2023, 75, 1711–1727. [Google Scholar] [CrossRef]

| Patients with Confirmed Delirium (n = 213) | Patients Without Delirium (n = 213) | p-Value | Statistic Test | |
|---|---|---|---|---|
| Age (years) (median, IQR) | 62.00 (21.00) | 62.00 (25.00) | 0.377 | Mann–Whitney U test |
| Male sex (n, %) | 173 (81.2%) | 141 (66.2%) | <0.001 | Chi-square |
| Portuguese nationality (n, %) | 158 (74.2%) | 159 (74.6%) | 0.939 | Chi-square |
| Administration of the COVID-19 vaccine (n, %) | 48 (22.5%) | 60 (28.2%) | 0.181 | Chi-square |
| Comorbidities (n, %) | 103 (48.4%) | 86 (40.4%) | 0.097 | Chi-square |
| Hypertension (n, %) | 109 (51.2%) | 102 (47.9%) | 0.498 | Chi-square |
| Diabetes Mellitus (n, %) | 60 (28.2%) | 55 (25.8%) | 0.585 | Chi-square |
| Dyslipidemia (n, %) | 53 (24.9%) | 50 (23.5%) | 0.734 | Chi-square |
| Obesity (n, %) | 54 (25.4%) | 45 (21.1%) | 0.302 | Chi-square |
| Hospital death (n, %) | 50 (23.5%) | 50 (23.5%) | 1.000 | Chi-square |
| ICU death (n, %) | 32 (15.0%) | 41 (19.2%) | 0.247 | Chi-square |
| Days of ICU stay (median, IQR) | 16.00 (14.00) | 6.00 (6.00) | <0.001 | Mann–Whitney U test |
| Use of IMV (n, %) | 141 (66.2%) | 75 (35.2%) | <0.001 | Chi-square |
| Use of ECMO (n, %) | 18 (8.5%) | 5 (2.3%) | 0.005 | Chi-square |
| Deep sedation with benzodiazepine (n, %) | 39 (18.3%) | 10 (4.7%) | <0.001 | Chi-square |
| Deep sedation without benzodiazepine (n, %) | 64 (30.0%) | 46 (21.6%) | 0.046 | Chi-square |
| Constipation (n, %) | 37 (17.4%) | 16 (7.5%) | 0.002 | Chi-square |
| RANK (Order) | Model | AUC | Accuracy | Precision | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| SVM | 0.558 | 0.509 | 0.507 | 0.657 | 0.362 |
| Logistic Regression | 0.690 | 0.643 | 0.661 | 0.587 | 0.700 | |
| Decision Tree | 0.707 | 0.634 | 0.645 | 0.596 | 0.671 | |
| Random Forest | 0.714 | 0.655 | 0.660 | 0.638 | 0.671 | |
| Naïve Bayes | 0.717 | 0.653 | 0.662 | 0.624 | 0.681 |
| Predicted | ||||
|---|---|---|---|---|
| Real | Without delirium | With delirium | Σ | |
| Without delirium | 64.4% (145) | 33.8% (68) | 213 | |
| With delirium | 35.6% (80) | 66.2% (133) | 213 | |
| Σ | 225 | 201 | 426 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viegas, A.; Von Rekowski, C.P.; Araújo, R.; Viana-Baptista, M.; Macedo, M.P.; Bento, L. Predicting ICU Delirium in Critically Ill COVID-19 Patients Using Demographic, Clinical, and Laboratory Admission Data: A Machine Learning Approach. Life 2025, 15, 1045. https://doi.org/10.3390/life15071045
Viegas A, Von Rekowski CP, Araújo R, Viana-Baptista M, Macedo MP, Bento L. Predicting ICU Delirium in Critically Ill COVID-19 Patients Using Demographic, Clinical, and Laboratory Admission Data: A Machine Learning Approach. Life. 2025; 15(7):1045. https://doi.org/10.3390/life15071045
Chicago/Turabian StyleViegas, Ana, Cristiana P. Von Rekowski, Rúben Araújo, Miguel Viana-Baptista, Maria Paula Macedo, and Luís Bento. 2025. "Predicting ICU Delirium in Critically Ill COVID-19 Patients Using Demographic, Clinical, and Laboratory Admission Data: A Machine Learning Approach" Life 15, no. 7: 1045. https://doi.org/10.3390/life15071045
APA StyleViegas, A., Von Rekowski, C. P., Araújo, R., Viana-Baptista, M., Macedo, M. P., & Bento, L. (2025). Predicting ICU Delirium in Critically Ill COVID-19 Patients Using Demographic, Clinical, and Laboratory Admission Data: A Machine Learning Approach. Life, 15(7), 1045. https://doi.org/10.3390/life15071045






