Surgical Management of Lower Back Pain: Is Optimizing Spinopelvic Alignment Beneficial for Patient Outcomes?
Abstract
1. Introduction
1.1. Spinopelvic Parameters
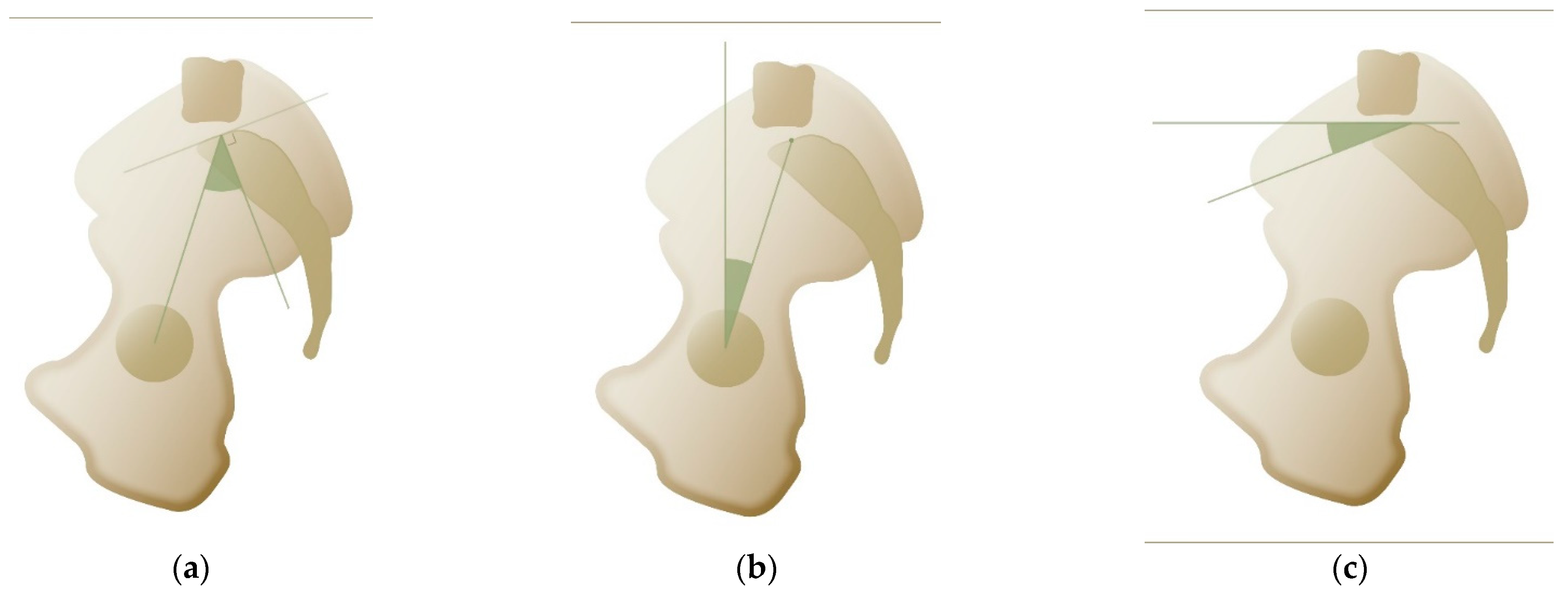
1.2. Pelvic Incidence
- 1.
- Pelvic tilt
- 2.
- Sacral slope
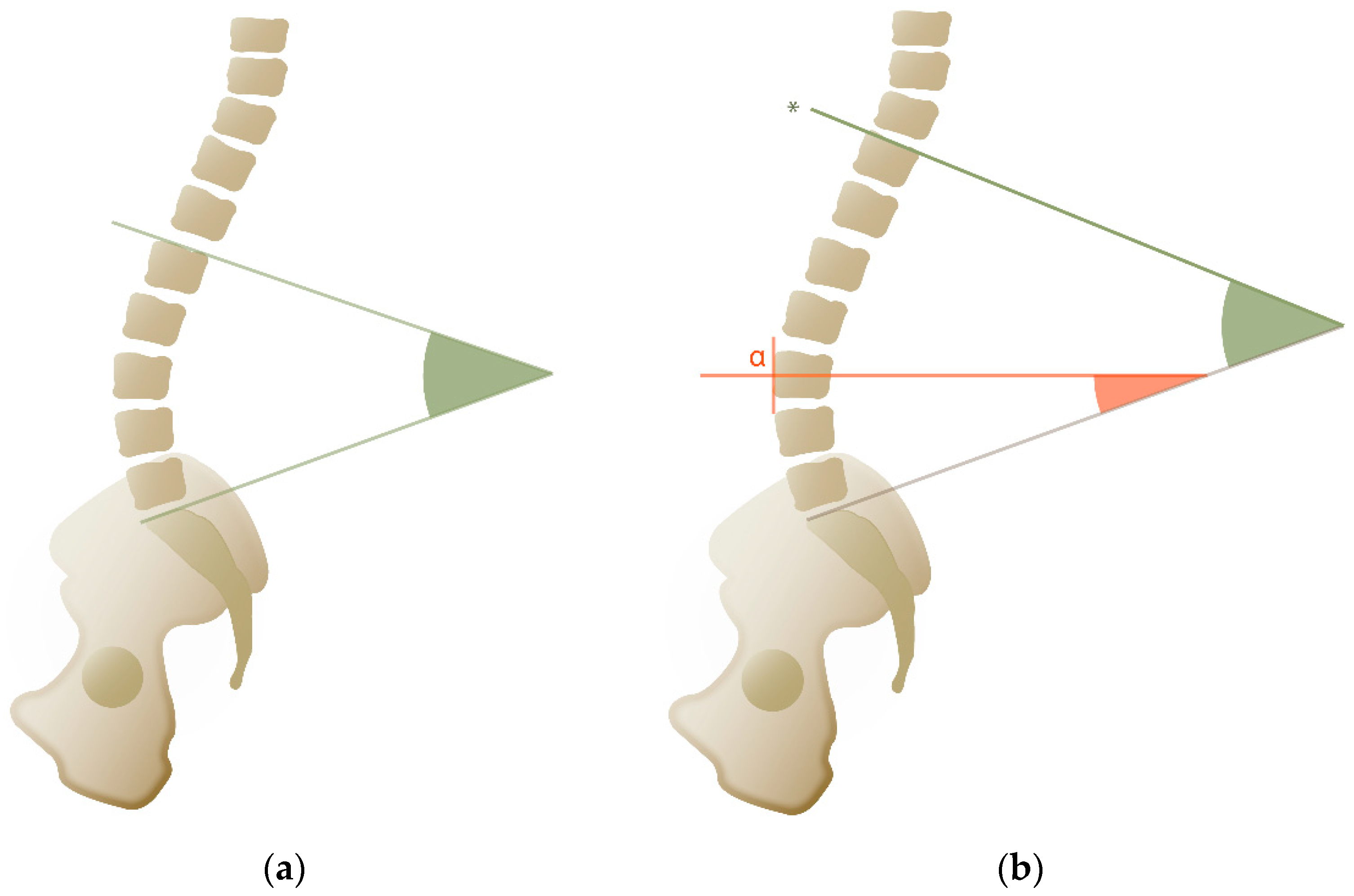
1.3. Lumbar Lordosis
1.4. Spinal Lordosis
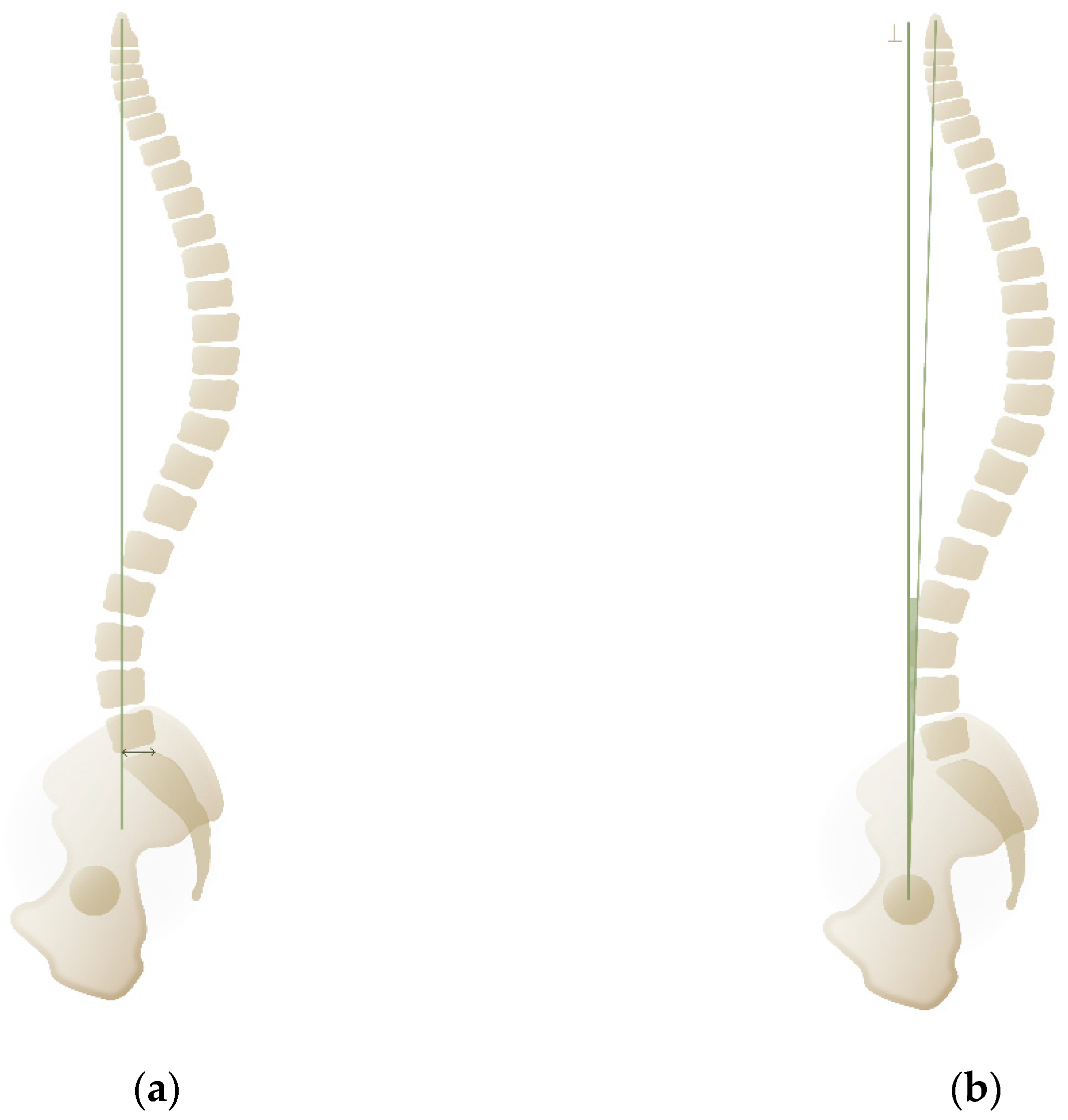
1.5. Sagittal Vertical Axis
1.6. Odontoid-Hip Axis
1.7. T1 Pelvic Angle
1.8. Other Measurements
2. Materials and Methods
3. Results
3.1. Global Disorders of Coronal/Sagittal Balance
3.2. Regional Disorders of Spinal Balance/Alignment
3.3. Evidence Table
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Katz, J.N. Lumbar disc disorders and low-back pain: Socioeconomic factors and consequences. J. Bone Jt. Surg. Am. 2006, 88 (Suppl. 2), 21–24. [Google Scholar] [CrossRef]
- Barrey, C.Y.; Le Huec, J.C.; French Society for Spine Surgery. Chronic low back pain: Relevance of a new classification based on the injury pattern. Orthop. Traumatol. Surg. Res. 2019, 105, 339–346. [Google Scholar] [CrossRef]
- Groen, G.J.; Beese, U.H.; Van de Kelft, E.; Groen, R.J.M. A Practical Approach to the Diagnosis and Understanding of Chronic Low Back Pain, Based on Its Pathophysiology. In Surgery of the Spine and Spinal Cord: A Neurosurgical Approach; van de Kelft, E., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 359–381. [Google Scholar]
- Taher, F.; Essig, D.; Lebl, D.R.; Hughes, A.P.; Sama, A.A.; Cammisa, F.P.; Girardi, F.P. Lumbar degenerative disc disease: Current and future concepts of diagnosis and management. Adv. Orthop. 2012, 2012, 970752. [Google Scholar] [CrossRef] [PubMed]
- Barrey, C.; Darnis, A. Current strategies for the restoration of adequate lordosis during lumbar fusion. World J. Orthop. 2015, 6, 117–126. [Google Scholar] [CrossRef]
- Jackson, R.P.; McManus, A.C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine 1994, 19, 1611–1618. [Google Scholar] [CrossRef] [PubMed]
- Legaye, J.; Duval-Beaupère, G.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef]
- Mikula, A.L.; Fogelson, J.L.; Oushy, S.; Pinter, Z.W.; Peters, P.A.; Abode-Iyamah, K.; Sebastian, A.S.; Freedman, B.; Currier, B.L.; Polly, D.W.; et al. Change in pelvic incidence between the supine and standing positions in patients with bilateral sacroiliac joint vacuum signs. J. Neurosurg. Spine 2021, 34, 617–622. [Google Scholar] [CrossRef]
- Boulay, C.; Tardieu, C.; Hecquet, J.; Benaim, C.; Mouilleseaux, B.; Marty, C.; Prat-Pradal, D.; Legaye, J.; Duval-Beaupère, G.; Pélissier, J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: Standard values and prediction of lordosis. Eur. Spine J. 2006, 15, 415–422. [Google Scholar] [CrossRef]
- Savarese, L.G.; Menezes-Reis, R.; Bonugli, G.P.; Herrero, C.; Defino, H.L.A.; Nogueira-Barbosa, M.H. Spinopelvic sagittal balance: What does the radiologist need to know? Radiol. Bras. 2020, 53, 175–184. [Google Scholar] [CrossRef]
- Barrey, C.; Jund, J.; Perrin, G.; Roussouly, P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery 2007, 61, 981–986; discussion 6. [Google Scholar] [CrossRef]
- Labelle, H.; Roussouly, P.; Chopin, D.; Berthonnaud, E.; Hresko, T.; O’Brien, M. Spino-pelvic alignment after surgical correction for developmental spondylolisthesis. Eur. Spine J. 2008, 17, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- Greimel, F.; Wolkerstorfer, S.; Spörrer, J.F.; Zeman, F.; Hoffstetter, P.; Grifka, J.; Benditz, A. Radiological outcome of postoperative sagittal balance on standing radiographs in comparison to intraoperative radiographs in prone position when performing lumbar spinal fusion. Arch. Orthop. Trauma Surg. 2017, 137, 1319–1325. [Google Scholar] [CrossRef] [PubMed]
- Le Huec, J.C.; Faundez, A.; Dominguez, D.; Hoffmeyer, P.; Aunoble, S. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: A literature review. Int. Orthop. 2015, 39, 87–95. [Google Scholar] [CrossRef]
- Le Huec, J.C.; Thompson, W.; Mohsinaly, Y.; Barrey, C.; Faundez, A. Sagittal balance of the spine. Eur. Spine J. 2019, 28, 1889–1905. [Google Scholar] [CrossRef]
- Van Royen, B.J.; Toussaint, H.M.; Kingma, I.; Bot, S.D.; Caspers, M.; Harlaar, J.; Wuisman, P.I. Accuracy of the sagittal vertical axis in a standing lateral radiograph as a measurement of balance in spinal deformities. Eur. Spine J. 1998, 7, 408–412. [Google Scholar] [CrossRef]
- Zhou, Q.; Zhang, J.X.; Zheng, Y.F.; Teng, Y.; Yang, H.L.; Liu, H.; Liu, T. Effects of different pedicle screw insertion depths on sagittal balance of lumbar degenerative spondylolisthesis, a retrospective comparative study. BMC Musculoskelet. Disord. 2021, 22, 850. [Google Scholar] [CrossRef]
- Laouissat, F.; Sebaaly, A.; Gehrchen, M.; Roussouly, P. Classification of normal sagittal spine alignment: Refounding the Roussouly classification. Eur. Spine J. 2018, 27, 2002–2011. [Google Scholar] [CrossRef]
- Chaléat-Valayer, E.; Mac-Thiong, J.M.; Paquet, J.; Berthonnaud, E.; Siani, F.; Roussouly, P. Sagittal spino-pelvic alignment in chronic low back pain. Eur. Spine J. 2011, 20 (Suppl. 5), 634–640. [Google Scholar] [CrossRef] [PubMed]
- Roussouly, P.; Gollogly, S.; Berthonnaud, E.; Dimnet, J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 2005, 30, 346–353. [Google Scholar] [CrossRef]
- Berthonnaud, E.; Dimnet, J.; Roussouly, P.; Labelle, H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J. Spinal Disord. Tech. 2005, 18, 40–47. [Google Scholar] [CrossRef]
- Chevillotte, T.; Chan, S.-K.; Grobost, P.; Laouissat, F.; Darnis, A.; Silvestre, C.; Roussouly, P. Quantifying the Spinal Lordosis Ratio Unique to the Type of Spinal Sagittal Alignment in a Normal Population. Glob. Spine J. 2024, 14, 1110–1115. [Google Scholar] [CrossRef] [PubMed]
- Swank, S.M.; Mauri, T.M.; Brown, J.C. The lumbar lordosis below Harrington instrumentation for scoliosis. Spine 1990, 15, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.P.; Kanemura, T.; Kawakami, N.; Hales, C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine 2000, 25, 575–586. [Google Scholar] [CrossRef]
- Gelb, D.E.; Lenke, L.G.; Bridwell, K.H.; Blanke, K.; McEnery, K.W. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine 1995, 20, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Patel, A.; Ungar, B.; Farcy, J.P.; Lafage, V. Adult spinal deformity-postoperative standing imbalance: How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 2010, 35, 2224–2231. [Google Scholar] [CrossRef]
- Ferrero, E.; Guigui, P.; Khalife, M.; Carlier, R.; Feydy, A.; Felter, A.; Lafage, V.; Skalli, W. Global alignment taking into account the cervical spine with odontoid hip axis angle (OD-HA). Eur. Spine J. 2021, 30, 3647–3655. [Google Scholar] [CrossRef]
- Protopsaltis, T.; Schwab, F.; Bronsard, N.; Smith, J.S.; Klineberg, E.; Mundis, G.; Ryan, D.J.; Hostin, R.; Hart, R.; Burton, D.; et al. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J. Bone Jt. Surg. Am. 2014, 96, 1631–1640. [Google Scholar] [CrossRef]
- Yilgor, C.; Sogunmez, N.; Boissiere, L.; Yavuz, Y.; Obeid, I.; Kleinstuck, F.; Perez-Grueso, F.J.S.; Acaroglu, E.; Haddad, S.; Mannion, A.F.; et al. Global Alignment and Proportion (GAP) Score: Development and Validation of a New Method of Analyzing Spinopelvic Alignment to Predict Mechanical Complications After Adult Spinal Deformity Surgery. J. Bone Jt. Surg. Am. 2017, 99, 1661–1672. [Google Scholar] [CrossRef]
- Roussouly, P.; Gollogly, S.; Noseda, O.; Berthonnaud, E.; Dimnet, J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: A radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine 2006, 31, E320–E325. [Google Scholar] [CrossRef]
- Le Huec, J.C.; Richards, J.; Tsoupras, A.; Price, R.; Leglise, A.; Faundez, A.A. The mechanism in junctional failure of thoraco-lumbar fusions. Part I: Biomechanical analysis of mechanisms responsible of vertebral overstress and description of the cervical inclination angle (CIA). Eur. Spine J. 2018, 27, 129–138. [Google Scholar] [CrossRef]
- Barrey, C.; Roussouly, P.; Le Huec, J.C.; D’Acunzi, G.; Perrin, G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur. Spine J. 2013, 22 (Suppl. 6), S834–S841. [Google Scholar] [CrossRef] [PubMed]
- Boissiere, L.; Takemoto, M.; Bourghli, A.; Vital, J.M.; Pellise, F.; Alanay, A.; Yilgor, C.; Acaroglu, E.; Perez-Grueso, F.J.; Kleinstuck, F.; et al. Global tilt and lumbar lordosis index: Two parameters correlating with health-related quality of life scores-but how do they truly impact disability? Spine J. 2017, 17, 480–488. [Google Scholar] [CrossRef]
- Lafage, V.; Schwab, F.; Patel, A.; Hawkinson, N.; Farcy, J.P. Pelvic tilt and truncal inclination: Two key radiographic parameters in the setting of adults with spinal deformity. Spine 2009, 34, E599–E606. [Google Scholar] [CrossRef]
- Park, S.J.; Lee, C.S.; Park, J.S.; Kang, D.H. Are Surgical Outcomes Different According to Baseline Balance Status in Elderly Patients with Degenerative Sagittal Imbalance? Spine 2024, 50, 395–404. [Google Scholar] [CrossRef]
- Zhou, H.; Liang, Z.; Li, P.; Shi, H.; Liang, A.; Gao, W.; Huang, D.; Peng, Y. Correlation analysis of surgical outcomes and spino-pelvic parameters in patients with degenerative lumbar scoliosis. Front. Surg. 2023, 10, 1319884. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.-Y.; Zhang, X.-N.; Hai, Y. Optimum pelvic incidence minus lumbar lordosis value after operation for patients with adult degenerative scoliosis. Spine J. 2017, 17, 983–989. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Li, W.; Su, T.; Du, C.; Wang, W.; Xu, F.; Sun, Z.; Li, W. Does lumbar lordosis minus thoracic kyphosis predict the clinical outcome of patients with adult degenerative scoliosis? J. Orthop. Surg. Res. 2019, 14, 290. [Google Scholar] [CrossRef]
- Zhang, H.C.; Zhang, Z.F.; Wang, Z.H.; Cheng, J.Y.; Wu, Y.C.; Fan, Y.M.; Wang, T.H.; Wang, Z. Optimal Pelvic Incidence Minus Lumbar Lordosis Mismatch after Long Posterior Instrumentation and Fusion for Adult Degenerative Scoliosis. Orthop. Surg. 2017, 9, 304–310. [Google Scholar] [CrossRef]
- Bourghli, A.; Aunoble, S.; Reebye, O.; Le Huec, J.C. Correlation of clinical outcome and spinopelvic sagittal alignment after surgical treatment of low-grade isthmic spondylolisthesis. Eur. Spine J. 2011, 20 (Suppl. 5), 663–668. [Google Scholar] [CrossRef]
- Simon, J.; Longis, P.M.; Passuti, N. Correlation between radiographic parameters and functional scores in degenerative lumbar and thoracolumbar scoliosis. Orthop. Traumatol. Surg. Res. 2017, 103, 285–290. [Google Scholar] [CrossRef]
- Tan, L.X.; Du, X.K.; Tang, R.M.; Rong, L.M.; Zhang, L.M. Effect of spinal-pelvic sagittal balance on the clinical outcomes after lumbar fusion surgery. BMC Surg. 2023, 23, 334. [Google Scholar] [CrossRef] [PubMed]
- Lenz, M.; Oikonomidis, S.; Hartwig, R.; Gramse, R.; Meyer, C.; Scheyerer, M.J.; Hofstetter, C.; Eysel, P.; Bredow, J. Clinical outcome after lumbar spinal fusion surgery in degenerative spondylolisthesis: A 3-year follow-up. Arch. Orthop. Trauma Surg. 2022, 142, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Thornley, P.; Meade, M.H.; Oitment, C.; Fernandes, R.R.; Urquhart, J.C.; Singh, S.; Siddiqi, F.; Rasoulinejad, P.; Bailey, C.S. Sagittal alignment in operative degenerative lumbar spondylolisthesis: A scoping review. J. Spine Surg. 2023, 9, 314–322. [Google Scholar] [CrossRef]
- He, S.; Zhang, Y.; Ji, W.; Liu, H.; He, F.; Chen, A.; Yang, H.; Pi, B. Analysis of Spinopelvic Sagittal Balance and Persistent Low Back Pain (PLBP) for Degenerative Spondylolisthesis (DS) following Posterior Lumbar Interbody Fusion (PLIF). Pain Res. Manag. 2020, 2020, 5971937. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, D.; Shen, Y.; Qi, X. Lumbar degenerative disease after oblique lateral interbody fusion: Sagittal spinopelvic alignment and its impact on low back pain. J. Orthop. Surg. Res. 2020, 15, 326. [Google Scholar] [CrossRef] [PubMed]
- Liow, M.H.L.; Goh, G.S.; Chua, J.L.; Ling, Z.M.; Soh, R.C.C.; Guo, C.M.; Tan, S.B.; Chen, J.L. Sagittally Balanced Degenerative Spondylolisthesis Patients With Increased Sacral Slope and Greater Lumbar Lordosis Experience Less Back Pain After Short-Segment Lumbar Fusion Surgery. Clin. Spine Surg. 2020, 33, E231–E235. [Google Scholar] [CrossRef]
- Sun, J.; Wang, J.J.; Zhang, L.W.; Huang, H.; Fu, N.X. Sagittal Alignment as Predictor of Adjacent Segment Disease After Lumbar Transforaminal Interbody Fusion. World Neurosurg. 2018, 110, e567–e571. [Google Scholar] [CrossRef]
- Aoki, Y.; Nakajima, A.; Takahashi, H.; Sonobe, M.; Terajima, F.; Saito, M.; Takahashi, K.; Ohtori, S.; Watanabe, A.; Nakajima, T.; et al. Influence of pelvic incidence-lumbar lordosis mismatch on surgical outcomes of short-segment transforaminal lumbar interbody fusion. BMC Musculoskelet. Disord. 2015, 16, 213. [Google Scholar] [CrossRef]
- Kim, M.K.; Lee, S.H.; Kim, E.S.; Eoh, W.; Chung, S.S.; Lee, C.S. The impact of sagittal balance on clinical results after posterior interbody fusion for patients with degenerative spondylolisthesis: A pilot study. BMC Musculoskelet. Disord. 2011, 12, 69. [Google Scholar] [CrossRef]
- Kumar, M.N.; Baklanov, A.; Chopin, D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur. Spine J. 2001, 10, 314–319. [Google Scholar] [CrossRef]
- Lazennec, J.Y.; Ramaré, S.; Arafati, N.; Laudet, C.G.; Gorin, M.; Roger, B.; Hansen, S.; Saillant, G.; Maurs, L.; Trabelsi, R. Sagittal alignment in lumbosacral fusion: Relations between radiological parameters and pain. Eur. Spine J. 2000, 9, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Turk, D.C.; Swanson, K.S.; Tunks, E.R. Psychological approaches in the treatment of chronic pain patients--when pills, scalpels, and needles are not enough. Can. J. Psychiatry 2008, 53, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Khalil, N.; Bizdikian, A.J.; Bakouny, Z.; Salameh, M.; Bou Zeid, N.; Yared, F.; Otayek, J.; Kharrat, K.; Kreichati, G.; Ghanem, I.; et al. Cervical and postural strategies for maintaining horizontal gaze in asymptomatic adults. Eur. Spine J. 2018, 27, 2700–2709. [Google Scholar] [CrossRef] [PubMed]
- Perna, A.; Proietti, L.; Smakaj, A.; Velluto, C.; Meluzio, M.C.; Rovere, G.; Florio, D.; Zirio, G.; Tamburrelli, F.C. The role of femoral obliquity angle and T1 pelvic angle in predicting quality of life after spinal surgery in adult spinal deformities. BMC Musculoskelet. Disord. 2021, 22, 999. [Google Scholar] [CrossRef]
- Azimi, P.; Yazdanian, T.; Benzel, E.C.; Montazeri, A. Global Sagittal Balance of Spine in Asymptomatic Controls: A Systematic Review and Meta-Analysis. World Neurosurg. 2021, 154, 93–108. [Google Scholar] [CrossRef]
- Roussouly, P.; Berthonnaud, E.; Dimnet, J. Geometrical and mechanical analysis of lumbar lordosis in an asymptomatic population: Proposed classification. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2003, 89, 632–639. [Google Scholar]
- Stagnara, P.; De Mauroy, J.C.; Dran, G.; Gonon, G.P.; Costanzo, G.; Dimnet, J.; Pasquet, A. Reciprocal angulation of vertebral bodies in a sagittal plane: Approach to references for the evaluation of kyphosis and lordosis. Spine 1982, 7, 335–342. [Google Scholar] [CrossRef]
| Study | Population | Intervention | Follow-Up | Outcome | Method | Spinopelvic Parameters | Conclusion | Level of Evidence |
|---|---|---|---|---|---|---|---|---|
| Prospective observational studies | ||||||||
| Lenz, 2022 [43] | Spondylolisthesis n = 32 | PLIA 1 or 2 levels | 3 years | ODI EQ-5D | Multivariate analysis | SS Sagittal rotation Sacral inclination | Restoration of sagittal parameters showed significant correlation with improvement in clinical outcomes. | Level III |
| Bourghli, 2011 [40] | Spondylolisthesis n = 30 | PLIA | Mean 36 months | ODI | Multivariate analysis | SVA | All patients with poor clinical outcomes had the same or increased SVA. | Level III |
| Lafage, 2009 [34] | Spinal stenosis n = 33 | Posterior spinal instrumentation | Unknown | ODI SF-12 SRS | Multivariate analysis | PT | High PT is a compensatory mechanism for sagittal imbalance and was correlated with poor clinical outcomes and quality of life. | Level III |
| Retrospective cohort studies | ||||||||
| Park, 2024 [35] | Scoliosis/sagittal imbalance n = 156 | Posterior spinal instrumentation 5 levels or greater | Mean 50 months | ODI SRS-22 | Retrospective SVA < 5 cm SVA ≥ 5 cm | SVA | The group with suboptimal correction of SVA had significantly inferior clinical outcomes compared to the compensatory balance group. | Level IV |
| Zhou, 2023 [36] | Scoliosis/sagittal imbalance n = 71 | Posterior spinal instrumentation | 2 years or more | ODI SRS-22 HRQOL | Retrospective PI-LL < 10° PI-LL = 10–20° PI-LL > 20° | PI-LL LL SVA | PI-LL is an important spinopelvic parameter that affects the postoperative HRQOL. LL should be restored during surgery with the aim of achieving LL ≥ PI-14°. As age increases, lower LL goals are necessary for age-adjusted correction. | Level IV |
| Tan, 2023 [42] | Spondylolisthesis Spinal stenosis Disc herniation n = 303 patients | PLIA | 2 years or more | ODI VAS | Retrospective PI-LL 10° or less PI-LL > 10 | PI-LL | Postoperative PI-LL has an effect of patient’s quality of life and degree of lower back pain. | Level IV |
| Thornley, 2023 [44] |
Spondylolisthesis n = 243 | Decompression +/− interbody arthrodesis | 1 year |
ODI VAS |
Retrospective Multivariate analysis | PI-LL LL SVA | Global postoperative spinopelvic parameters are correlated with functional outcomes. | Level IV |
| He, 2020 [45] | Spondylolisthesis n = 107 | PLIA 1 or 2 level | 6 months | ODI VAS | Retrospective PLBP Non-PLBP | PT SL | SL, height of disc, and PT were significantly less improved in the PLBP group compared to non-PLBP. | Level IV |
| Li, 2020 [46] | Spondylolisthesis Spinal stenosis n = 120 | OLIA 1 level | 2 years or more | ODI VAS | Retrospective PLBP Non-PLBP | PI-LL PT SVA | High PT, PI-LL mismatch, and high SVA were identified as significant risk factors for PLBP. Decreased PT, improved SVA, and improved PI-LL were associated with better functional outcomes. | Level IV |
| Liow, 2020 [47] | Spondylolisthesis n = 63 | PLIA L4/L5 | 2 years | ODI Short-form 36 | Retrospective SS ≥ 30° SS < 30° | PT PI LL SS | Patients with increased SS (≥30 degrees) experienced less back pain after short-segment lumbar arthrodesis surgery. This was associated with increased LL postoperatively, indicating better sagittal balance. | Level IV |
| Zhou, 2019 [38] | Scoliosis/sagittal imbalance n = 130 | Posterior spinal instrumentation | 2 years or more | ODI VAS JOA | Retrospective LL–TK ≥ 10° LL–TK < 10° | LL-TK SVA | Postoperative LL-TK was strongly associated with patient HRQOL. Postoperative SVA is suitable for predicting the surgical outcomes for patients after correction surgery. Based on ROC curve, the cutoff value of LL-TK is ≥10° to achieve good clinical outcomes and sagittal balance. | Level IV |
| Sun, 2018 [48] | Spondylolisthesis Spinal stenosis Disc herniation n = 163 | PLIA | Mean 40.6 months | Adjacent segment disease | Retrospective Multivariate analysis | PT TK | A PT of more than 24.3° and TK of more than 23.3° could be regarded as predictors for adjacent segment disease. | Level IV |
| Zhang, 2017 [48] | Scoliosis/sagittal imbalance n = 44 | Posterior spinal instrumentation | Mean 2.6 years | ODI VAS JOA | Retrospective PI-LL< 10° 10° ≤ PI-LL ≤ 20° PI-LL >20° | PI-LL | The optimal PI-LL value may be achieved between 10° and 20° with good clinical outcomes. | Level IV |
| Sun, 2017 [37] | Scoliosis/sagittal imbalance n = 74 | Posterior spinal instrumentation | 2 years or more | Adjacent segment disease ODI VAS JOA | Retrospective PI-LL< 10° 10° ≤ PI-LL ≤ 20° PI-LL > 20° | PI-LL | The optimal PI-LL value may be achieved between 10° and 20° with excellent clinical outcomes and a lower adjacent-level disease occurrence. | Level IV |
| Simon, 2017 [41] | Scoliosis/sagittal imbalance n = 47 | Posterolateral arthrodesis | Mean 6.4 years | ODI SF-36 | Retrospective Univariate analysis | LL SS | Significant correlation between the SF-36 and postoperative SS and LL. | Level IV |
| Aoki, 2015 [49] | Spinal stenosis n = 52 | PLIA 1 or 2 level | Mean 16.9 months | VAS Nakai scores | Retrospective PI-LL 10° or less PI-LL > 10 | PI-LL | Greater PI-LL was significantly associated with worse postoperative clinical outcomes. | Level IV |
| Kim, 2011 [50] | Spondylolisthesis n = 18 | Posterior interbody arthrodesis | Mean 43.1 months | ODI VAS | Retrospective Univariate analysis | PT | In patients with improved postoperative PT after arthrodesis, clinical outcomes were good regarding VAS and ODI improvement. | Level IV |
| Kumar, 2001 [51] | Disc herniation n = 83 | Posterior spinal instrumentation | Mean 5 years | Adjacent segment disease | Retrospective Univariate analysis | SVA SS | Higher incidence of adjacent segment disease in patients with abnormal postoperative SS and SVA values. | Level IV |
| Lazennec, 2000 [52] | Spondylolisthesis Disc herniation n = 81 | Posterior spinal instrumentation | Mean 2.8 years | Pain | Retrospective PLBP No-PLBP | PT SS | Decreased SS and PT were associated with postoperative PLBP. | Level IV |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thijs, D.; Kashtiara, A.; Beldé, S.; Van de Kelft, E. Surgical Management of Lower Back Pain: Is Optimizing Spinopelvic Alignment Beneficial for Patient Outcomes? Life 2025, 15, 833. https://doi.org/10.3390/life15060833
Thijs D, Kashtiara A, Beldé S, Van de Kelft E. Surgical Management of Lower Back Pain: Is Optimizing Spinopelvic Alignment Beneficial for Patient Outcomes? Life. 2025; 15(6):833. https://doi.org/10.3390/life15060833
Chicago/Turabian StyleThijs, Dieter, Ardavan Kashtiara, Sarah Beldé, and Erik Van de Kelft. 2025. "Surgical Management of Lower Back Pain: Is Optimizing Spinopelvic Alignment Beneficial for Patient Outcomes?" Life 15, no. 6: 833. https://doi.org/10.3390/life15060833
APA StyleThijs, D., Kashtiara, A., Beldé, S., & Van de Kelft, E. (2025). Surgical Management of Lower Back Pain: Is Optimizing Spinopelvic Alignment Beneficial for Patient Outcomes? Life, 15(6), 833. https://doi.org/10.3390/life15060833






