Lipid Metabolism and Breast Cancer: A Narrative Review of the Prognostic Implications and Chemotherapy-Induced Dyslipidemia
Abstract
1. Introduction
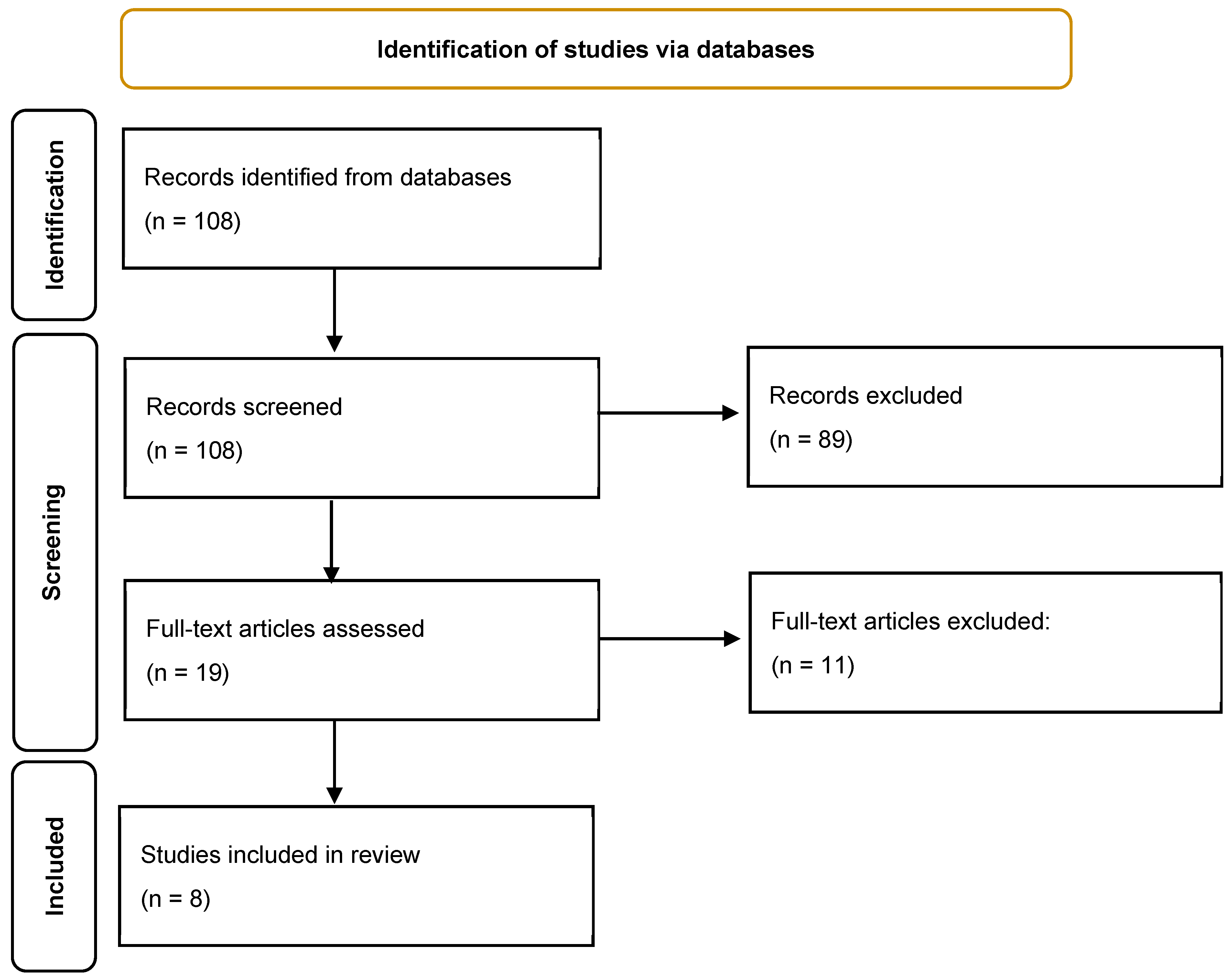
2. Materials and Methods
3. Results
3.1. Chemotherapy-Induced Dyslipidemia: Evidence from Clinical Cohorts
3.2. Predictive Role of Lipid Alterations in Chemotherapy Response
3.3. Long-Term Implications of Dyslipidemia in Breast Cancer’s Prognosis
3.4. Key Findings
3.5. Chemotherapy-Induced Dyslipidemia
3.6. Transient vs. Persistent Dyslipidemia Post-Chemotherapy
3.7. Lipid Profiles as Prognostic Indicators
3.8. Impact of Lipid-Lowering Therapies
4. Discussion
4.1. Integration of Findings and Mechanistic Interpretations
4.2. Prognostic Role of Dyslipidemia in Breast Cancer
4.3. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gradishar, W.; Moran, M.S.; Abraham, J.; Abramson, V.; Aft, R.; Agnese, D.; Allison, K.H.; Anderson, B.; Bailey, J.; Burstein, H.; et al. Breast Cancer, Version 3.2024, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2024, 22, 331–357. [Google Scholar] [CrossRef]
- Fu, J.; Wu, L.; Jiang, M.; Li, D.; Jiang, T.; Fu, W.; Wang, L.; Du, J. Real-world impact of non-breast cancer-specific death on overall survival in resectable breast cancer. Cancer 2017, 123, 2432–2443. [Google Scholar] [CrossRef]
- Barzaman, K.; Karami, J.; Zarei, Z.; Hosseinzadeh, A.; Kazemi, M.H.; Moradi-Kalbolandi, S.; Safari, E.; Farahmand, L. Breast cancer: Biology, biomarkers, and treatments. Int. Immunopharmacol. 2020, 84, 106535. [Google Scholar] [CrossRef] [PubMed]
- Santana, M.; Sawada, M.I.; Junior, D.R.S.; Giacaglia, M.B.; Reis, M.; Xavier, J.; Côrrea-Giannella, M.; Soriano, F.G.; Gebrim, L.; Ronsein, G.E.; et al. Proteomic Profiling of HDL in Newly Diagnosed Breast Cancer Based on Tumor Molecular Classification and Clinical Stage of Disease. Cells 2024, 13, 1327. [Google Scholar] [CrossRef]
- Goto, W.; Kashiwagi, S.; Takada, K.; Asano, Y.; Takahashi, K.; Fujita, H.; Takashima, T.; Tomita, S.; Hirakawa, K.; Ohira, M. Significance of intrinsic breast cancer subtypes on the long-term prognosis after neoadjuvant chemotherapy. J. Transl. Med. 2018, 16, 307. [Google Scholar] [CrossRef]
- von Minckwitz, G.; Untch, M.; Blohmer, J.-U.; Costa, S.D.; Eidtmann, H.; Fasching, P.A.; Gerber, B.; Eiermann, W.; Hilfrich, J.; Huober, J.; et al. Definition and Impact of Pathologic Complete Response on Prognosis After Neoadjuvant Chemotherapy in Various Intrinsic Breast Cancer Subtypes. J. Clin. Oncol. 2012, 30, 1796–1804. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Daniels, G.; Lee, P.; Monaco, M.E. Lipid metabolism in prostate cancer. Am. J. Clin. Exp. Urol. 2014, 2, 111. [Google Scholar] [PubMed]
- de Guia, R.M.; Herzig, S. How Do Glucocorticoids Regulate Lipid Metabolism. Adv. Exp. Med. Biol. 2015, 872, 127–144. [Google Scholar] [CrossRef]
- Tan, W.; Zhong, Z.; Wang, S.; Suo, Z.; Yang, X.; Hu, X.; Wang, Y. Berberine Regulated Lipid Metabolism in the Presence of C75, Compound C, and TOFA in Breast Cancer Cell Line MCF-7. Evid. Based Complement. Altern. Med. 2015, 2015, 396035. [Google Scholar] [CrossRef]
- Arpino, G.; De Angelis, C.; Buono, G.; Colao, A.; Giuliano, M.; Malgieri, S.; Cicala, S.; De Laurentiis, M.; Accurso, A.; Crispo, A.; et al. Metabolic and anthropometric changes in early breast cancer patients receiving adjuvant therapy. Breast Cancer Res. Treat. 2015, 154, 127–132. [Google Scholar] [CrossRef]
- Berglund, A.; Wigertz, A.; Adolfsson, J.; Ahlgren, J.; Fornander, T.; Wärnberg, F.; Lambe, M. Impact of comorbidity on management and mortality in women diagnosed with breast cancer. Breast Cancer Res. Treat. 2012, 135, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Llanos, A.A.M.; Makambi, K.H.; Tucker, C.A.; Wallington, S.F.; Shields, P.G.; Adams-Campbell, L.L. Cholesterol, lipoproteins, and breast cancer risk in African-American women. Ethn. Dis. 2012, 22, 281. [Google Scholar]
- Wei, S.; Liu, L.; Zhang, J.; Bowers, J.; Gowda, G.A.N.; Seeger, H.; Fehm, T.; Neubauer, H.J.; Vogel, U.; Clare, S.E.; et al. Metabolomics approach for predicting response to neoadjuvant chemotherapy for breast cancer. Mol. Oncol. 2013, 7, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Furberg, A.; Veierød, M.B.; Wilsgaard, T.; Bernstein, L.; Thune, I. Serum High-Density Lipoprotein Cholesterol, Metabolic Profile, and Breast Cancer Risk. J. Natl. Cancer Inst. 2004, 96, 1152–1160. [Google Scholar] [CrossRef]
- Eliassen, A.H.; Colditz, G.A.; Rosner, B.; Willett, W.C.; Hankinson, S.E. Serum lipids, lipid-lowering drugs, and the risk of breast cancer. JAMA Intern. Med. 2005, 165, 2264–2271. [Google Scholar] [CrossRef] [PubMed]
- Menendez, J.A.; Lupu, R. Fatty acid synthase regulates estrogen receptor-α signaling in breast cancer cells. Oncogenesis 2017, 6, e299. [Google Scholar] [CrossRef]
- Luo, D.-X.; Cao, D.-L.; Xiong, Y.; Peng, X.-H.; Liao, D.-F. A novel model of cholesterol efflux from lipid-loaded cells. Acta Pharmacol. Sin. 2010, 31, 1243–1257. [Google Scholar] [CrossRef]
- Yan, G.; Li, L.; Zhu, B.; Li, Y. Lipidome in colorectal cancer. Oncotarget 2016, 7, 33429–33439. [Google Scholar] [CrossRef]
- Li, X.; Liu, Z.-L.; Wu, Y.; Wu, H.; Dai, W.; Arshad, B.; Xu, Z.; Li, H.; Wu, K.; Kong, L.-Q. Status of lipid and lipoprotein in female breast cancer patients at initial diagnosis and during chemotherapy. Lipids Health Dis. 2018, 17, 91. [Google Scholar] [CrossRef]
- Tian, W.; Yao, Y.; Fan, G.; Zhou, Y.; Wu, M.; Xu, D.; Deng, Y. Changes in lipid profiles during and after (neo)adjuvant chemotherapy in women with early-stage breast cancer: A retrospective study. PLoS ONE 2019, 14, e0221866. [Google Scholar] [CrossRef]
- Qu, F.; Chen, R.; Peng, Y.; Ye, Y.; Tang, Z.; Wang, Y.; Zong, B.; Yu, H.; Liu, S. Assessment of the Predictive Role of Serum Lipid Profiles in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy. J. Breast Cancer 2020, 23, 246–258. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Wang, C.; Tan, Q.; Wang, Z.; Li, J.; Chen, T.; Cui, K.; Wu, Y.; Sun, J.; Zheng, D.; et al. Adjuvant chemotherapy-associated lipid changes in breast cancer patients: A real-word retrospective analysis. Medicine 2020, 99, e21498. [Google Scholar] [CrossRef]
- Xu, L.; Dong, Q.; Long, Y.; Tang, X.; Zhang, N.; Lu, K. Dynamic Changes of Blood Lipids in Breast Cancer Patients After (Neo)adjuvant Chemotherapy: A Retrospective Observational Study. Int. J. Gen. Med. 2020, 13, 817–823. [Google Scholar] [CrossRef] [PubMed]
- Goto, W.; Kashiwagi, S.; Takada, K.; Asano, Y.; Ogisawa, K.; Morisaki, T.; Shibutani, M.; Tanaka, H.; Maeda, K. Clinical verification of the relationship between serum lipid metabolism and immune activity in breast cancer patients treated with neoadjuvant chemotherapy. Eur. J. Med Res. 2023, 28, 2. [Google Scholar] [CrossRef]
- Ma, Y.; Lv, M.; Yuan, P.; Chen, X.; Liu, Z. Dyslipidemia is associated with a poor prognosis of breast cancer in patients receiving neoadjuvant chemotherapy. BMC Cancer 2023, 23, 208. [Google Scholar] [CrossRef] [PubMed]
- Bicakli, D.H.; Varol, U.; Degirmenci, M.; Tunali, D.; Cakar, B.; Durusoy, R.; Karaca, B.; Sanli, U.A.; Uslu, R. Adjuvant chemotherapy may contribute to an increased risk for metabolic syndrome in patients with breast cancer. J. Oncol. Pharm. Pract. 2016, 22, 46–53. [Google Scholar] [CrossRef]
- Beckwitt, C.H.; Clark, A.M.; Ma, B.; Whaley, D.; Oltvai, Z.N.; Wells, A. Statins attenuate outgrowth of breast cancer metastases. Br. J. Cancer 2018, 119, 1094–1105. [Google Scholar] [CrossRef]
- Ahern, T.P.; Lash, T.L.; Damkier, P.; Christiansen, P.; Cronin-Fenton, D. Statins and breast cancer prognosis: Evidence and opportunities. Lancet Oncol. 2014, 15, e461–e468. [Google Scholar] [CrossRef]
- Weis, M.; Heeschen, C.; Glassford, A.; Cooke, J.P. Statins Have Biphasic Effects on Angiogenesis. Circulation 2002, 105, 739–745. [Google Scholar] [CrossRef]
- Manthravadi, S.; Shrestha, A.; Madhusudhana, S. Impact of statin use on cancer recurrence and mortality in breast cancer: A systematic review and meta-analysis. Int. J. Cancer 2016, 139, 1281–1288. [Google Scholar] [CrossRef]
- Alexopoulos, C.; Pournaras, S.; Vaslamatzis, M.; Avgerinos, A.; Raptis, S. Changes in serum lipids and lipoproteins in cancer patients during chemotherapy. Cancer Chemother. Pharmacol. 1992, 30, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Neuhouser, M.L.; Aragaki, A.K.; Prentice, R.L.; Manson, J.A.E.; Chlebowski, R.T.; Carty, C.L.; Ochs-Balcom, H.M.; Thomson, C.A.; Caan, B.J.; Tinker, L.F.; et al. Overweight, Obesity, and Postmenopausal Invasive Breast Cancer Risk: A Secondary Analysis of the Women’s Health Initiative Randomized Clinical Trials. JAMA Oncol. 2015, 1, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Sheth, J.; Shah, A.; Sheth, F.; Trivedi, S.; Nabar, N.; Shah, N.; Thakor, P.; Vaidya, R. The association of dyslipidemia and obesity with glycated hemoglobin. Clin. Diabetes Endocrinol. 2015, 1, 6. [Google Scholar] [CrossRef]
- Picon-Ruiz, M.; Morata-Tarifa, C.; Valle-Goffin, J.J.; Friedman, E.R.; Slingerland, J.M. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA Cancer J. Clin. 2017, 67, 378–397. [Google Scholar] [CrossRef] [PubMed]
- Bjørge, T.; Lukanova, A.; Jonsson, H.; Tretli, S.; Ulmer, H.; Manjer, J.; Stocks, T.; Selmer, R.; Nagel, G.; Almquist, M.; et al. Metabolic syndrome and breast cancer in the Me-Can (metabolic syndrome and cancer) project. Cancer Epidemiol. Biomark. Prev. 2010, 19, 1737–1745. [Google Scholar] [CrossRef]
- Finkelman, B.S.; Putt, M.E.; Wang, T.; Wang, L.; Narayan, H.K.; Domchek, S.M.; DeMichele, A.; Fox, K.; Matro, J.M.; Shah, P.D.; et al. Arginine-Nitric Oxide Metabolites and Cardiac Dysfunction in Patients With Breast Cancer. J. Am. Coll. Cardiol. 2017, 70, 152–162. [Google Scholar] [CrossRef]
- Li, X.; Wenes, M.; Romero, P.; Huang, S.C.-C.; Fendt, S.-M.; Ho, P.-C. Navigating metabolic pathways to enhance antitumour immunity and immunotherapy. Nat. Rev. Clin. Oncol. 2019, 16, 425–441. [Google Scholar] [CrossRef] [PubMed]
- Furberg, A.-S.; Jasienska, G.; Bjurstam, N.; Torjesen, P.A.; Emaus, A.; Lipson, S.F.; Ellison, P.T.; Thune, I. Metabolic and Hormonal Profiles: HDL Cholesterol as a Plausible Biomarker of Breast Cancer Risk. The Norwegian EBBA Study. Cancer Epidemiol. Biomark. Prev. 2005, 14, 33–40. [Google Scholar] [CrossRef]
- Shi, Y.; Yan, S. Identifying Biomarkers for Prognostic Treatment in Breast Cancer through Bioinformatics Analysis. Res. Sq. 2023. [Google Scholar] [CrossRef]
- Baroni, S.; Scribano, D.; Zuppi, C.; Pagano, L.; Leone, G.; Giardina, B. Prognostic Relevance of Lipoprotein Cholesterol Levels in Acute Lymphocytic and Nonlymphocytic Leukemia. Acta Haematol. 1996, 96, 24–28. [Google Scholar] [CrossRef]
- Fichtali, K.; Bititi, A.; Elghanmi, A.; Ghazi, B. Serum Lipidomic Profiling in Breast Cancer to Identify Screening, Diagnostic, and Prognostic Biomarkers. Biores. Open Access 2020, 9, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Zhan, J.; Fang, W.; Zhao, Y.; Yang, Y.; Hou, X.; Zhang, Z.; He, X.; Zhang, Y.; Huang, Y.; et al. Serum low-density lipoprotein and low-density lipoprotein expression level at diagnosis are favorable prognostic factors in patients with small-cell lung cancer (SCLC). BMC Cancer 2017, 17, 269. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, C.; Fonseca, I.; Dias, S.; de Almeida, J.C.M. Plasma level of LDL-cholesterol at diagnosis is a predictor factor of breast tumor progression. BMC Cancer 2014, 14, 132. [Google Scholar] [CrossRef]
- Santos, C.; Domingues, G.; Matias, I.; Matos, J.; Fonseca, I.; de Almeida, J.C.M.; Dias, S. LDL-cholesterol signaling induces breast cancer proliferation and invasion. Lipids Health Dis. 2014, 13, 16. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Park, S.K.; Han, W.; Kim, D.-H.; Hong, Y.-C.; Ha, E.H.; Ahn, S.-H.; Noh, D.-Y.; Kang, D.; Yoo, K.-Y. Serum High-Density Lipoprotein Cholesterol and Breast Cancer Risk by Menopausal Status, Body Mass Index, and Hormonal Receptor in Korea. Cancer Epidemiol. Biomark. Prev. 2009, 18, 508–515. [Google Scholar] [CrossRef]
- Alimperti, A.; Alikari, V.; Tsironi, M.; Gil, A.P.; Papageorgiou, D.; Kolovos, P.; Panagiotou, A.; Panoutsopoulos, G.I.; Lavdaniti, M.; Zyga, S. Lipid Disturbances in Breast Cancer Patients during Chemotherapy. Nurs. Rep. 2023, 13, 1500–1510. [Google Scholar] [CrossRef]
- Tőkés, A.M.; Vári-Kakas, S.; Kulka, J.; Törőcsik, B. Tumor Glucose and Fatty Acid Metabolism in the Context of Anthracycline and Taxane-Based (Neo)Adjuvant Chemotherapy in Breast Carcinomas. Front. Oncol. 2022, 12, 850401. [Google Scholar] [CrossRef]
- Zagar, T.M.; Cardinale, D.; Marks, L.B. Breast cancer therapy-associated cardiovascular disease. Nat. Rev. Clin. Oncol. 2015, 13, 172–184. [Google Scholar] [CrossRef]
- Gernaat, S.A.M.; Ho, P.J.; Rijnberg, N.; Lee, S.C.; Lim, S.H.; Yap, Y.S.; Grobbee, D.E.; Hartman, M.; Verkooijen, H.M. Risk of death from cardiovascular disease following breast cancer in Southeast Asia: A prospective cohort study. Sci. Rep. 2017, 7, 1365. [Google Scholar] [CrossRef]
- Gao, S.; Zhao, D.; Wang, M.; Zhao, F.; Han, X.; Qi, Y.; Liu, J. Association Between Circulating Oxidized LDL and Atherosclerotic Cardiovascular Disease: A Meta-analysis of Observational Studies. Can. J. Cardiol. 2017, 33, 1624–1632. [Google Scholar] [CrossRef]
- Patnaik, J.L.; Byers, T.; DiGuiseppi, C.; Dabelea, D.; Denberg, T.D. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: A retrospective cohort study. Breast Cancer Res. 2011, 13, R64. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, R.; Dixit, N.M.; Yang, E.H.; Sallam, T. Cancer therapy’s impact on lipid metabolism: Mechanisms and future avenues. Front. Cardiovasc. Med. 2022, 9, 925816. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Tuaine, J.M.; McLaren, B.; Waters, D.L.; Black, K.E.; Jones, L.M.; McCormick, S.P.A. Chemotherapy Agents Alter Plasma Lipids in Breast Cancer Patients and Show Differential Effects on Lipid Metabolism Genes in Liver Cells. PLoS ONE 2016, 11, e0148049. [Google Scholar] [CrossRef] [PubMed]
- Kaye, J.A.; Meier, C.R.; Walker, A.M.; Jick, H. Statin use, hyperlipidaemia, and the risk of breast cancer. Br. J. Cancer 2002, 86, 1436–1439. [Google Scholar] [CrossRef][Green Version]
- White, A.J.; Nichols, H.B.; Bradshaw, P.T.; Sandler, D.P. Overall and central adiposity and breast cancer risk in the sister study. Cancer 2015, 121, 3700–3708. [Google Scholar] [CrossRef]
| Article (Year) | Study Design | Sample Size | Breast Cancer Subtype | Lipid Parameters Assessed | Main Findings | Chemotherapy Regimen | Follow-Up Duration | Key Outcome |
|---|---|---|---|---|---|---|---|---|
| Li et al. (2018) [19] | Retrospective cohort | 1054 BC patients, 2483 controls | Mixed | TC, TGs, LDL-C, HDL-C | BC patient had significantly lower TC, TGs, LDL-C, and HDC-c than controls (p < 0.05). Dyslipidemia worsened post-chemotherapy, with TGs and LDL-C increasing while HDL-C decreased. | Various | Not specified | Dyslipidemia incidence increased from 42.98% to 58.28% after chemotherapy. |
| Tian et al. (2019) [20] | Prospective cohort | 805 | Mixed | TC, TGs, LDL-C, HDL-C | Chemotherapy-induced lipid alterations were transient, with TC and LDL-C increasing during treatment but returning to baseline after 6 months. Younger patients showed greater lipid fluctuations. | Various | 6 months | Chemotherapy-induced dyslipidemia is temporary in most patients. |
| Qu et al. (2020) [21] | Retrospective | 533 | ER+ | TGs, HDL-C | High pre-NAC HDL-C (≥1.305 mmol/L) was an independent predictor of better chemotherapy response (p = 0.007). Low TGs (<1.155 mmol/L) also predicted improved NAC response. | NAC | Not specified | Lipid profiles may serve as biomarkers for NAC response. |
| He et al. (2020) [22] | Retrospective | 1934 | Mixed | TC, TGs, LDL-C, HDL-C | TGs increased by 38%, HDL-C decreased by 23% after chemotherapy. FEC had milder lipid changes than taxane-based regimens. Postmenopausal women had less severe lipid alterations. | AC-T, EC-T, TC, FEC | Not specified | Chemotherapy significantly alters lipid profiles, with taxane-based regimens showing more pronounced effects. |
| Xu et al. (2020) [23] | Longitudinal | 159 | Mixed | TC, TGs, LDL-C, HDL-C | TGs increased from 1.3 to 1.6 mmol/L post-chemotherapy and remained elevated at 12 months (p < 0.05). LDL-C also remained high, while HDL-C was stable. | Various | 12 months | Persistent dyslipidemia post-chemotherapy, requiring long-term lipid management. |
| Goto et al. (2023) [24] | Prospective | 327 | TNBC | TGs, HDL-C, TC | Post-NAC TG increase correlated with improved survival (5-year OS: 78% vs. 65%, p = 0.014). High TC post-NAC was linked to better survival in TNBC patients (p = 0.014). | NAC | 5 years | Lipid metabolism influences immune activity and survival in TNBC. |
| Ma et al. (2023) [25] | Retrospective | 312 | Mixed | TC, TGs, LDL-C | Pre-treatment dyslipidemia was associated with lower pCR rates and higher relapse (30% vs. 18%, p < 0.05). Full-course lipid levels correlated with DFS (HR = 1.896, p = 0.029). | NAC | Not specified | High TG levels independently predicted poor DFS. |
| Santana et al. (2024) [4] | Cross-sectional | 141 BC patients, 103 controls | Mixed | HDL-C, ApoA-1, ApoA-2, ApoC-2, Apo C-4 | TNBC patients had lower ApoA-1 and ApoA-2 levels than other subtypes, suggesting altered HDL proteomics. Higher HDL-associated proteins correlated with tumor stage. | Not applicable | Not applicable | HDL composition differs by BC subtype and may serve as a biomarker. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faur, I.F.; Dobrescu, A.; Clim, I.A.; Pasca, P.; Burta, C.; Marian, M.; Brebu, D.; Neamtu, A.-A.; Braicu, V.; Tamas, T.; et al. Lipid Metabolism and Breast Cancer: A Narrative Review of the Prognostic Implications and Chemotherapy-Induced Dyslipidemia. Life 2025, 15, 689. https://doi.org/10.3390/life15050689
Faur IF, Dobrescu A, Clim IA, Pasca P, Burta C, Marian M, Brebu D, Neamtu A-A, Braicu V, Tamas T, et al. Lipid Metabolism and Breast Cancer: A Narrative Review of the Prognostic Implications and Chemotherapy-Induced Dyslipidemia. Life. 2025; 15(5):689. https://doi.org/10.3390/life15050689
Chicago/Turabian StyleFaur, Ionut Flaviu, Amadeus Dobrescu, Ioana Adelina Clim, Paul Pasca, Cosmin Burta, Marco Marian, Dan Brebu, Andreea-Adriana Neamtu, Vlad Braicu, Talpai Tamas, and et al. 2025. "Lipid Metabolism and Breast Cancer: A Narrative Review of the Prognostic Implications and Chemotherapy-Induced Dyslipidemia" Life 15, no. 5: 689. https://doi.org/10.3390/life15050689
APA StyleFaur, I. F., Dobrescu, A., Clim, I. A., Pasca, P., Burta, C., Marian, M., Brebu, D., Neamtu, A.-A., Braicu, V., Tamas, T., Duta, C., & Totolici, B. (2025). Lipid Metabolism and Breast Cancer: A Narrative Review of the Prognostic Implications and Chemotherapy-Induced Dyslipidemia. Life, 15(5), 689. https://doi.org/10.3390/life15050689






