NT-proBNP in Acute De Novo Heart Failure: A Key Biomarker for Predicting Myocardial Recovery—COMFE Registry
Abstract
1. Introduction
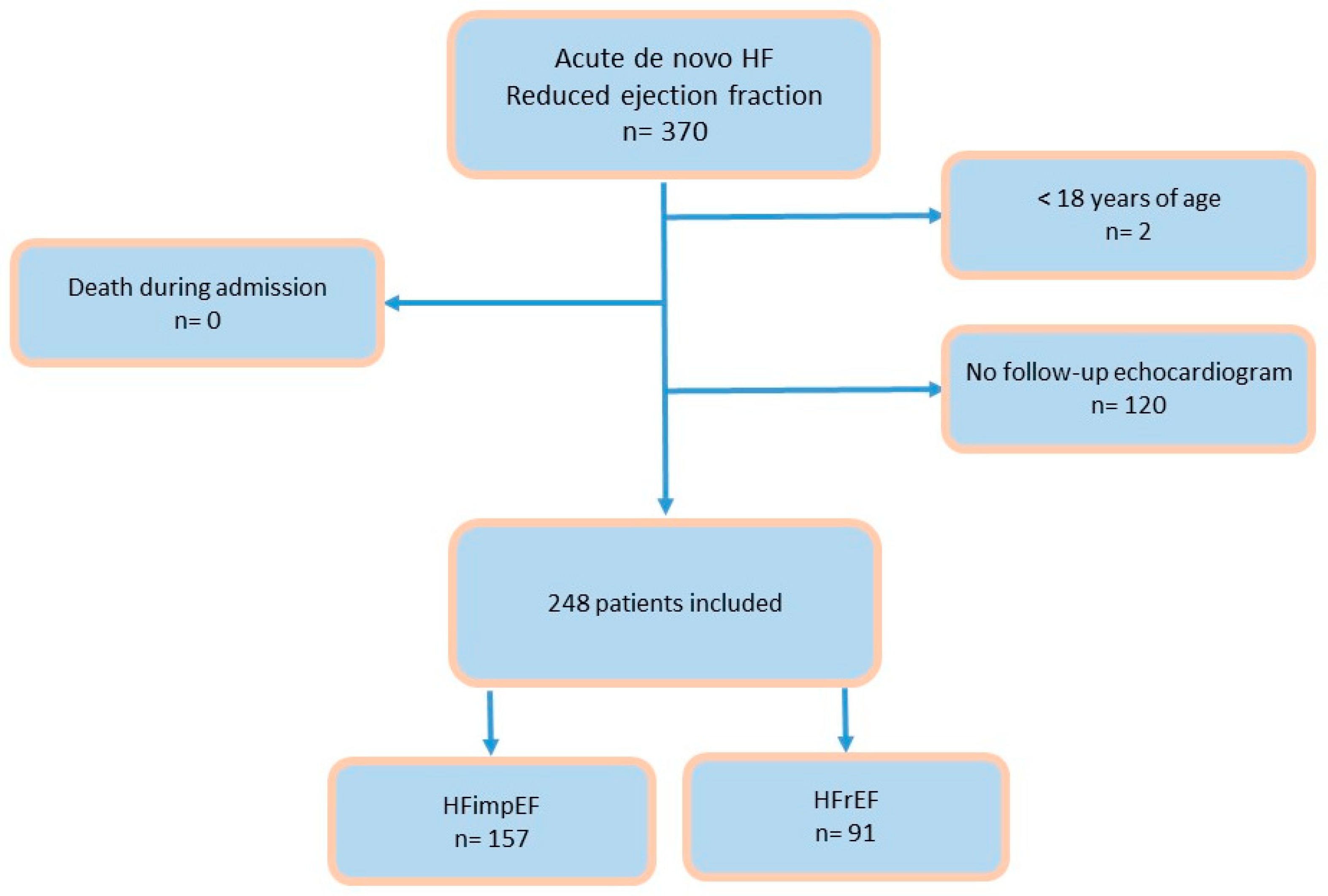
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Baseline Characteristics
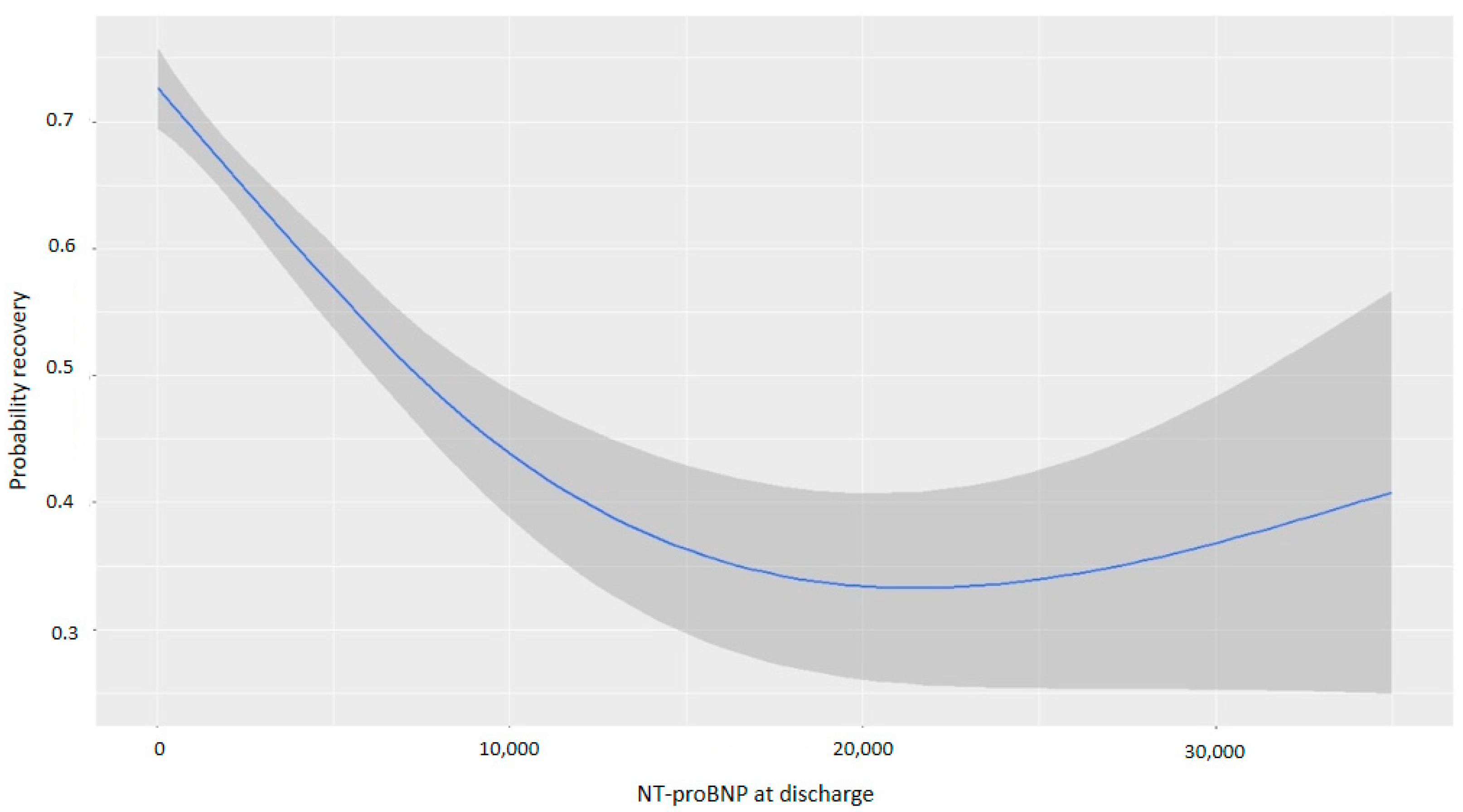
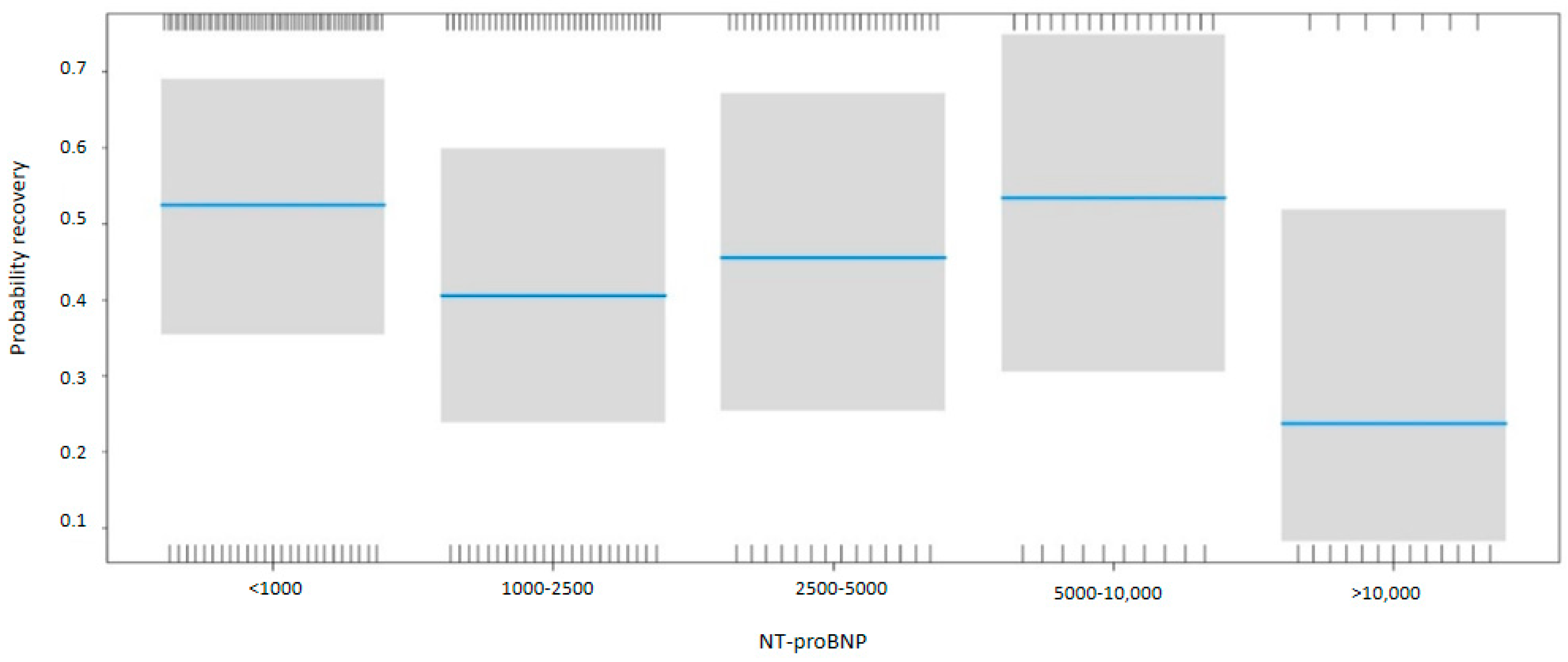
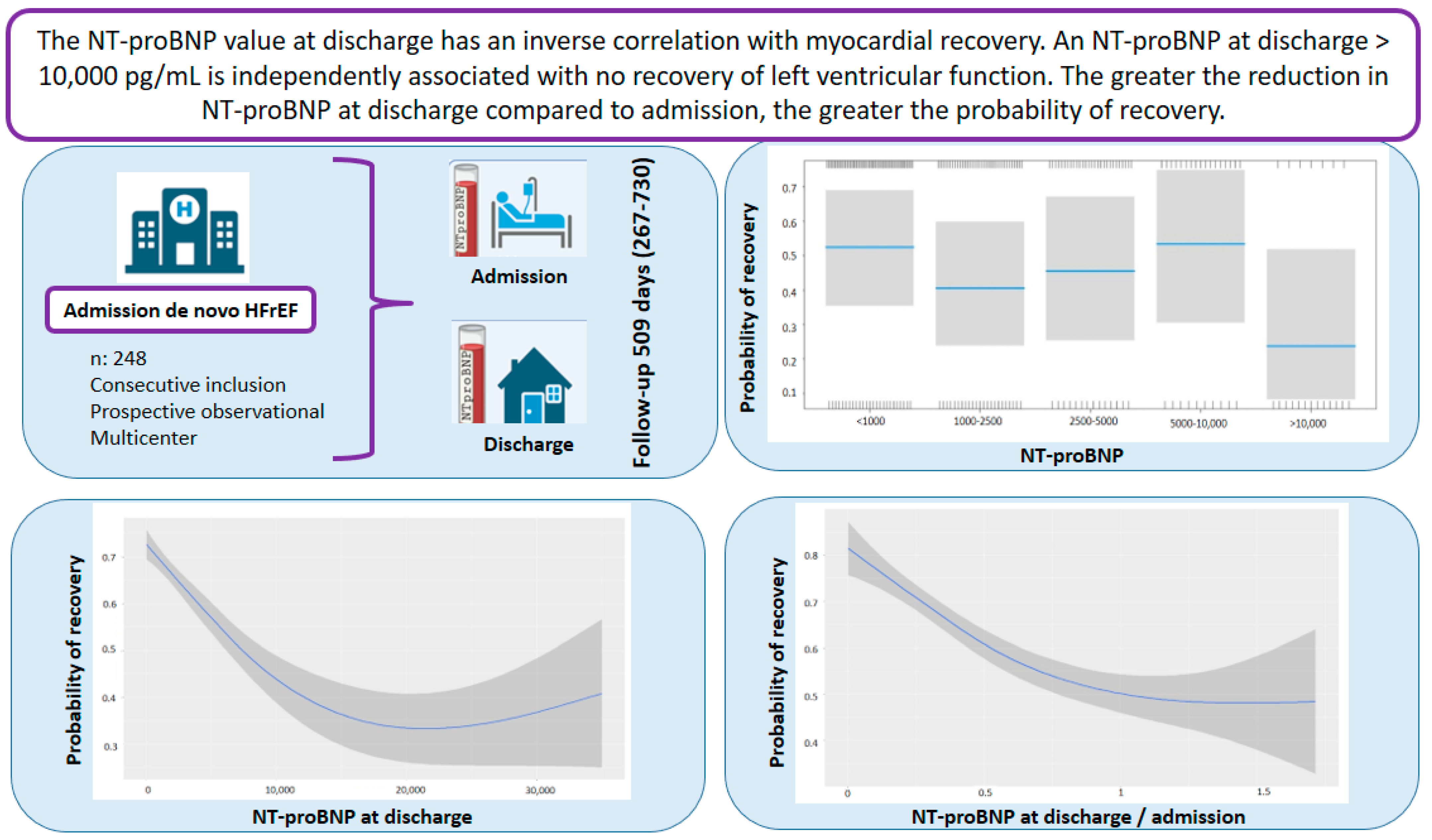
3.2. Relationship Between NT-proBNP at Discharge and Myocardial Recovery
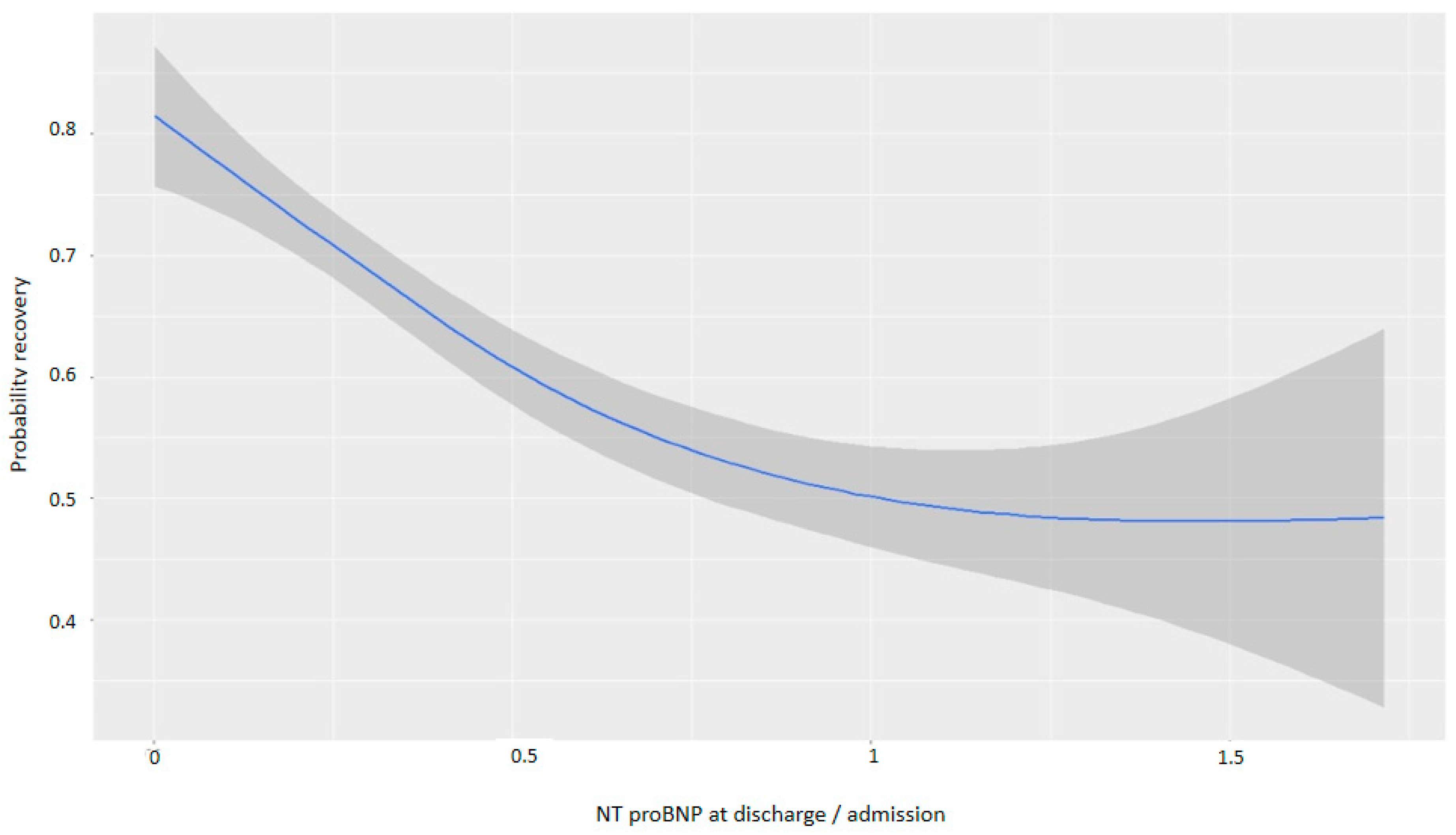
3.3. Impact of NT-proBNP Reduction During Hospitalization
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021, 42, 3599–3726, Erratum in Eur. Heart J. 2021, 42, 4901. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.W.; Lyass, A.; Enserro, D.; Larson, M.G.; Ho, J.E.; Kizer, J.R.; Gottdiener, J.S.; Psaty, B.M.; Vasan, R.S. Temporal Trends in the Incidence of and Mortality Associated with Heart Failure with Preserved and Reduced Ejection Fraction. JACC Heart Fail. 2018, 6, 678–685. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- López-Vilella, R.; Pastor, P.J.; Trenado, V.D.; Sánchez-Lázaro, I.; Caballero, E.B.; Crespo-Leiro, M.G.; Dolz, L.M.; Bonet, L.A. Mortality After the First Hospital Admission for Acute Heart Failure, De Novo Versus Acutely Decompensated Heart Failure With Reduced Ejection Fraction. Am. J. Cardiol. 2023, 196, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-E.; Cho, D.-H.; Son, J.-W.; Kim, J.Y.; Kang, S.-M.; Cho, M.-C.; Lee, H.-Y.; Jeon, E.-S.; Yoo, B.-S. Impact of NT-proBNP on prognosis of acute decompensated chronic heart failure versus de novo heart failure. Int. J. Cardiol. 2022, 363, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Savarese, G.; Becher, P.M.; Lund, L.H.; Seferovic, P.; Rosano, G.M.C.; Coats, A.J.S. Global burden of heart failure: A comprehensive and updated review of epidemiology. Cardiovasc. Res. 2023, 118, 3272–3287. [Google Scholar] [CrossRef] [PubMed]
- Oommen, S.G.; Man, R.K.; Talluri, K.; Nizam, M.; Kohir, T.; Aviles, M.A.; Nino, M.; Jaisankar, L.G.; Jaura, J.; Wannakuwatte, R.A.; et al. Heart Failure With Improved Ejection Fraction: Prevalence, Predictors, and Guideline-Directed Medical Therapy. Cureus 2024, 16, e61790. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vaduganathan, M.; Claggett, B.L.; Jhund, P.S.; Cunningham, J.W.; Ferreira, J.P.; Zannad, F.; Packer, M.; Fonarow, G.C.; McMurray, J.J.V.; Solomon, S.D. Estimating lifetime benefits of comprehensive disease-modifying pharmacological therapies in patients with heart failure with reduced ejection fraction: A comparative analysis of three randomised controlled trials. Lancet 2020, 396, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, P.; Pluchinotta, F.R.; Salvioni, E.; Mapelli, M.; Galotta, A.; Bonomi, A.; Magrì, D.; Perna, E.; Paolillo, S.; Corrà, U.; et al. Heart failure patients with improved ejection fraction: Insights from the MECKI score database. Eur. J. Heart Fail. 2023, 25, 1976–1984. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.P.; Ibrahim, N.E.; Januzzi, J.L., Jr. Heart Failure With Reduced Ejection Fraction: A Review. JAMA 2020, 324, 488–504, Erratum in JAMA 2020, 324, 2107. [Google Scholar] [CrossRef] [PubMed]
- Basuray, A.; French, B.; Ky, B.; Vorovich, E.; Olt, C.; Sweitzer, N.K.; Cappola, T.P.; Fang, J.C. Heart failure with recovered ejection fraction clinical description, biomarkers, and outcomes. Circulation 2014, 129, 2380–2387. [Google Scholar] [CrossRef]
- Senni, M.; D’Elia, E.; Emdin, M.; Vergaro, G. Biomarkers of Heart Failure with Preserved and Reduced Ejection Fraction. Handb. Exp. Pharmacol. 2017, 243, 79–108. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Fernández, A.; Gómez-Otero, I.; López-Fernández, S.; Santamarta, M.R.; Pastor-Pérez, F.J.; Fluvià-Brugués, P.; Pérez-Rivera, J.; López, A.L.; García-Pinilla, J.M.; Palomas, J.L.B.; et al. Influence of the medical treatment schedule in new diagnoses patients with heart failure and reduced ejection fraction. Clin. Res. Cardiol. 2024, 113, 1171–1182. [Google Scholar] [CrossRef] [PubMed]
- Mebazaa, A.; Davison, B.; Chioncel, O.; Cohen-Solal, A.; Diaz, R.; Filippatos, G.; Metra, M.; Ponikowski, P.; Sliwa, K.; Voors, A.A.; et al. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): A multinational, open-label, randomised, trial. Lancet 2022, 400, 1938–1952. [Google Scholar] [CrossRef] [PubMed]
- Nawrocka-Millward, S.; Biegus, J.; Hurkacz, M.; Guzik, M.; Rosiek-Biegus, M.; Jankowska, E.A.; Ponikowski, P.; Zymliński, R. Differences in the Biomarker Profile of De Novo Acute Heart Failure versus Decompensation of Chronic Heart Failure. Biomolecules 2021, 11, 1701. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kalogeropoulos, A.P.; Fonarow, G.C.; Georgiopoulou, V.; Burkman, G.; Siwamogsatham, S.; Patel, A.; Li, S.; Papadimitriou, L.; Butler, J. Characteristics and outcomes of adult outpatients with heart failure and improved or recovered ejection fraction. JAMA Cardiol. 2016, 1, 510–518. [Google Scholar]
- Florea, V.G.; Rector, T.S.; Anand, I.S.; Cohn, J.N. Heart failure with improved ejection fraction: Clinical characteristics, correlates of recovery, and survival. Circ. Heart Fail. 2016, 9, e003123. [Google Scholar] [PubMed]
- Ghimire, A.; Fine, N.; Ezekowitz, J.A.; Howlett, J.; Youngson, E.; McAlister, F.A. Frequency, predictors, and prognosis of ejection fraction improvement in heart failure: An echocardiogram-based registry study. Eur. Heart J. 2019, 40, 2110–2117. [Google Scholar] [CrossRef] [PubMed]
- Lupón, J.; Gaggin, H.K.; de Antonio, M.; Domingo, M.; Galán, A.; Zamora, E.; Vila, J.; Peñafiel, J.; Urrutia, A.; Ferrer, E.; et al. Biomarker-assist score for reverse remodeling prediction in heart failure: The ST2-R2 score. Int. J. Cardiol. 2015, 184, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, J.E.; Fang, J.C.; Margulies, K.B.; Mann, D.L. Heart Failure With Recovered Left Ventricular Ejection Fraction: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 2020, 76, 719–734. [Google Scholar] [CrossRef] [PubMed]
- Gulati, G.; Udelson, J.E. Heart Failure With Improved Ejection Fraction: Is it Possible to Escape One’s Past? JACC Heart Fail. 2018, 6, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Aimo, A.; Gaggin, H.K.; Barison, A.; Emdin, M.; Januzzi, J.L., Jr. Imaging, biomarker, and clinical predictors of cardiac remodeling in heart failure with reduced ejection fraction. J. Am. Coll. Cardiol. HF 2019, 7, 782–794. [Google Scholar]
- Segev, A.; Avrahamy, B.; Fardman, A.; Matetzky, S.; Freimark, D.; Regev, O.; Kuperstein, R.; Grupper, A. Heart failure with improved ejection fraction: Patient characteristics, clinical outcomes and predictors for improvement. Front. Cardiovasc. Med. 2024, 11, 1378955. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Daubert, M.A.; Adams, K.; Yow, E.; Barnhart, H.X.; Douglas, P.S.; Rimmer, S.; Norris, C.; Cooper, L.; Leifer, E.; Desvigne-Nickens, P.; et al. NT-proBNP goal achievement is associated with significant reverse remodeling and improved clinical outcomes in HFrEF. J. Am. Coll. Cardiol. HF 2019, 7, 158–168. [Google Scholar]
- López-Vilella, R.; Marqués-Sulé, E.; Sánchez-Lázaro, I.; Laymito Quispe, R.; Martínez Dolz, L.; Almenar Bonet, L. Creatinine and NT-proBNP levels could predict the length of hospital stay of patients with decompensated heart failure. Acta Cardiol. 2021, 76, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- Stawiarski, K.; Ramakrishna, H. Guideline-Directed Medical Management of Heart Failure with Reduced Ejection Fraction: Improved Outcomes With Quadruple Therapy. J. Cardiothorac. Vasc. Anesth. 2022, 36, 1820–1822. [Google Scholar] [CrossRef] [PubMed]
- Bettencourt, P.; Ferreira, S.; Azevedo, A.; Ferreira, A. Preliminary data on the potential usefulness of B-type natriuretic peptide levels in predicting outcome after hospital discharge in patients with heart failure. Am. J. Med. 2002, 113, 215–219. [Google Scholar] [CrossRef]
- Paredes-Paucar, C.; Medina, L.V.; Araiza-Garaygordobil, D.; Gopar-Nieto, R.; Martínez-Amezcua, P.; Cabello-Lopez, A.; Sierra-Lara, D.; De La Cruz, J.L.B.; Pacheco, H.G.; Mendoza, A.A. Prognostic value of the absolute decrease of the N-terminal portion of B-type natriuretic propeptide in decompensated heart failure: Secondary analysis of the CLUSTER-HF study. Arch. Peru. Cardiol. Cir. Cardiovasc. 2022, 3, 8–15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]


| Variables | HFimpEF YES n: 157 | HFimpEF NO n: 91 | p |
|---|---|---|---|
| Age (years) | 69 (58–76) | 71 (61–78) | 0.353 |
| Male (n,%) | 120 (76.43) | 68 (74.73) | 0.882 |
| Hypertension (n,%) | 92 (58.60) | 63 (69.23) | 0.126 |
| Dyslipidemia (n,%) | 73 (46.50) | 48 (52.74) | 0.414 |
| Diabetes (n,%) | 43 (27.39) | 34 (37.36) | 0.135 |
| CKD (n,%) | 28 (17.83) | 29 (31.87) | 0.018 |
| Stroke (n,%) | 8 (5.12) | 8 (8.79%) | 0.390 |
| CPOD (n,%) | 11 (7.00) | 10 (10.99) | 0.396 |
| SAHS (n,%) | 7 (4.49) | 7 (7.69) | 0.444 |
| PAD (n,%) | 9 (5.7) | 12 (13.33) | 0.068 |
| Alcohol (n,%) | 44 (28.03) | 21 (23.08) | 0.481 |
| Smoking (n/%) | 64 (40.76) | 26 (28.57) | 0.074 |
| Time to titration/optimization (days) | 117 (38.25–186.25) | 110 (44.50–172.00) | 0.837 |
| Etiology of HF (n, %) | |||
| Hypertension | 10 (6.37) | 3 (3.30) | 0.453 |
| Tachycardiomyopathy | 46 (29.30) | 12 (13.19) | 0.006 |
| Ischemic | 27 (17.20) | 40 (43.96) | <0.0001 |
| Idiopathic | 32 (20.38) | 20 (21.98) | 0.892 |
| Valvular | 12 (7.64) | 1 (1.10) | 0.050 |
| Other | 26 (19.11) | 15 (16.48) | 0.729 |
| Creatinine at discharge (mg/dL) | 1.10 (0.89–1.37) | 1.14 (0.87–1.51) | 0.361 |
| GFR at discharge (mL/min/1.73 m2) | 65.93 (21.63) | 62.00 (24.44) | 0.217 |
| NT-proBNP at admission (ng/mL) | 4695 (2280–8623.0) | 5069 (2166–11,324.5) | 0.439 |
| NT-proBNP at discharge (ng/mL) | 1464 (607.5–3316.5) | 2349 (917.0–5943.0) | 0.006 |
| LVEF at admission | 28.90 (6.44) | 28.78 (7.38) | 0.90 |
| LVEF after titration | 51.58 (7.249) | 32.916 (6.60) | <0.0001 |
| SBP at admission (mmHg) | 149 ± 24 | 154 ± 14 | 0.067 |
| DBP at admission (mmHg) | 76 ± 11 | 78 ± 13 | 0.195 |
| SBP at discharge (mmHg) | 121 ± 15 | 124 ± 17 | 0.458 |
| DBP at discharge (mmHg) | 65 ± 12 | 66 ± 13 | 0.452 |
| 4 Pillars at discharge (n, %) | 103 (66.03) | 53 (58.24) | 0.277 |
| 4 Pillars after optimization (n, %) | 110 (72.37) | 57 (64.04) | 0.227 |
| RAASi at discharge (n, %) | 142 (90.45) | 76 (83.52) | 0.158 |
| Beta-blockers at discharge (n, %) | 142 (91.03) | 88 (96.70) | 0.150 |
| Mineralocorticoid receptor antagonists at discharge (n, %) | 130 (82.80) | 69 (75.82) | 0.244 |
| SGLT2i at discharge (n, %) | 131 (83.39) | 76 (83.52) | 0.126 |
| RAASi after optimization (n, %) | 139 (90.26) | 74 (81.32) | 0.070 |
| Beta-blockers after optimization (n, %) | 147 (93.63) | 88 (97.78) | 0.250 |
| Mineralocorticoid receptor antagonists after optimization (n, %) | 128 (82.58) | 74 (81.32) | 0.939 |
| SGLT2i after optimization (n, %) | 144 (91.72) | 80 (88.89) | 0.611 |
| Duration of admission in days | 7.00 (5.00–11.00) | 7.00 (5.00–10.50) | 0.636 |
| Weight at discharge (kg) | 72.00 (61.85–86.00) | 74.50 (63.62–90.00) | 0.547 |
| NYHA first consultation (I-IV) | 2.00 (1.00–2.00) | 2.00 (2.00–2.00) | 0.782 |
| Time to titration (days) | 115.00 (38.5–185.5) | 110.0 (44.5–166.0) | <0.001 |
| Variable | OR | Low | High | p-Value |
|---|---|---|---|---|
| √NT-proBNP at discharge | 0.990 | 0.980 | 0.999 | 0.048 |
| √Age | 0.923 | 0.646 | 1.300 | 0.652 |
| Sex (female) | 0.911 | 0.458 | 1.835 | 0.792 |
| Peripheral artery disease | 0.484 | 0.167 | 1.366 | 0.171 |
| Hypertensive etiology | 3.888 | 1.043 | 18.941 | 0.058 |
| Tachycardiomyopathy | 4.256 | 1.893 | 10.051 | <0.001 |
| Idiopathic etiology | 2.325 | 1.025 | 5.428 | 0.046 |
| Valvular etiology | 24.399 | 4.074 | 475.593 | 0.004 |
| Other etiology | 2.064 | 0.910 | 4.796 | 0.086 |
| Titrated medical therapy | 1.153 | 0.594 | 2.218 | 0.670 |
| OR | Low | High | p-Value | |
|---|---|---|---|---|
| (Intercept) | 1.618 | 0.285 | 9515 | 0.588 |
| NT-proBNP at discharge (1000–2500) | 0.617 | 0.289 | 1.317 | 0.211 |
| NT-proBNP at discharge (2500–5000) | 0.755 | 0.327 | 1.773 | 0.512 |
| NT-proBNP at discharge (5000–10,000) | 1.038 | 0.378 | 2.949 | 0.942 |
| NT-proBNP at discharge (>10,000) | 0.28 | 0.077 | 0.939 | 0.043 |
| Age | 0.992 | 0.969 | 1.015 | 0.486 |
| Sex (female) | 0.86 | 0.431 | 1.737 | 0.670 |
| Peripheral artery disease | 0.52 | 0.174 | 1.532 | 0.233 |
| Hypertensive etiology | 4.829 | 1.245 | 24.46 | 0.033 |
| Tachycardiomyopathy | 4.601 | 2.023 | 11.018 | <0.001 |
| Idiopathic etiology | 2.423 | 1.054 | 5.756 | 0.040 |
| Valvular etiology | 25.709 | 4.299 | 499.231 | 0.003 |
| Other etiology | 2.353 | 1.018 | 5.606 | 0.048 |
| Titrated medical therapy | 1.204 | 0.617 | 2.33 | 0.583 |
| Variable | OR | Low | High | p-Value |
|---|---|---|---|---|
| √ Reduction in NT-proBNP | 0.133 | 0.027 | 0.611 | 0.010 |
| Age | 0.990 | 0.967 | 1.013 | 0.400 |
| Sex (female) | 0.879 | 0.440 | 1.775 | 0.716 |
| Peripheral artery disease | 0.387 | 0.127 | 1.110 | 0.083 |
| Hypertensive etiology | 3.884 | 1.020 | 19.228 | 0.0621 |
| Tachycardiomyopathy | 4.398 | 1.951 | 10.429 | <0.001 |
| Idiopathic etiology | 2.375 | 1.038 | 5.597 | 0.043 |
| Valvular etiology | 24.415 | 4.050 | 478.916 | 0.004 |
| Other etiology | 1.924 | 0.838 | 4.520 | 0.126 |
| Titrated medical therapy | 1.121 | 0.577 | 2.160 | 0.733 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Vilella, R.; Gómez-Otero, I.; Donoso Trenado, V.; García-Vega, D.; Otero-García, Ó.; Martínez Dolz, L.; González-Juanatey, J.R.; Almenar Bonet, L. NT-proBNP in Acute De Novo Heart Failure: A Key Biomarker for Predicting Myocardial Recovery—COMFE Registry. Life 2025, 15, 526. https://doi.org/10.3390/life15040526
López-Vilella R, Gómez-Otero I, Donoso Trenado V, García-Vega D, Otero-García Ó, Martínez Dolz L, González-Juanatey JR, Almenar Bonet L. NT-proBNP in Acute De Novo Heart Failure: A Key Biomarker for Predicting Myocardial Recovery—COMFE Registry. Life. 2025; 15(4):526. https://doi.org/10.3390/life15040526
Chicago/Turabian StyleLópez-Vilella, Raquel, Inés Gómez-Otero, Víctor Donoso Trenado, David García-Vega, Óscar Otero-García, Luis Martínez Dolz, José Ramón González-Juanatey, and Luis Almenar Bonet. 2025. "NT-proBNP in Acute De Novo Heart Failure: A Key Biomarker for Predicting Myocardial Recovery—COMFE Registry" Life 15, no. 4: 526. https://doi.org/10.3390/life15040526
APA StyleLópez-Vilella, R., Gómez-Otero, I., Donoso Trenado, V., García-Vega, D., Otero-García, Ó., Martínez Dolz, L., González-Juanatey, J. R., & Almenar Bonet, L. (2025). NT-proBNP in Acute De Novo Heart Failure: A Key Biomarker for Predicting Myocardial Recovery—COMFE Registry. Life, 15(4), 526. https://doi.org/10.3390/life15040526










