The Level of Adherence to Organic Food Consumption and Risk of Cancer: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Study Selection & Data Extraction
2.4. Dietary Data Extraction
2.5. Quality Assessment
2.6. Data Synthesis
2.7. Quality of the Evidence
3. Results
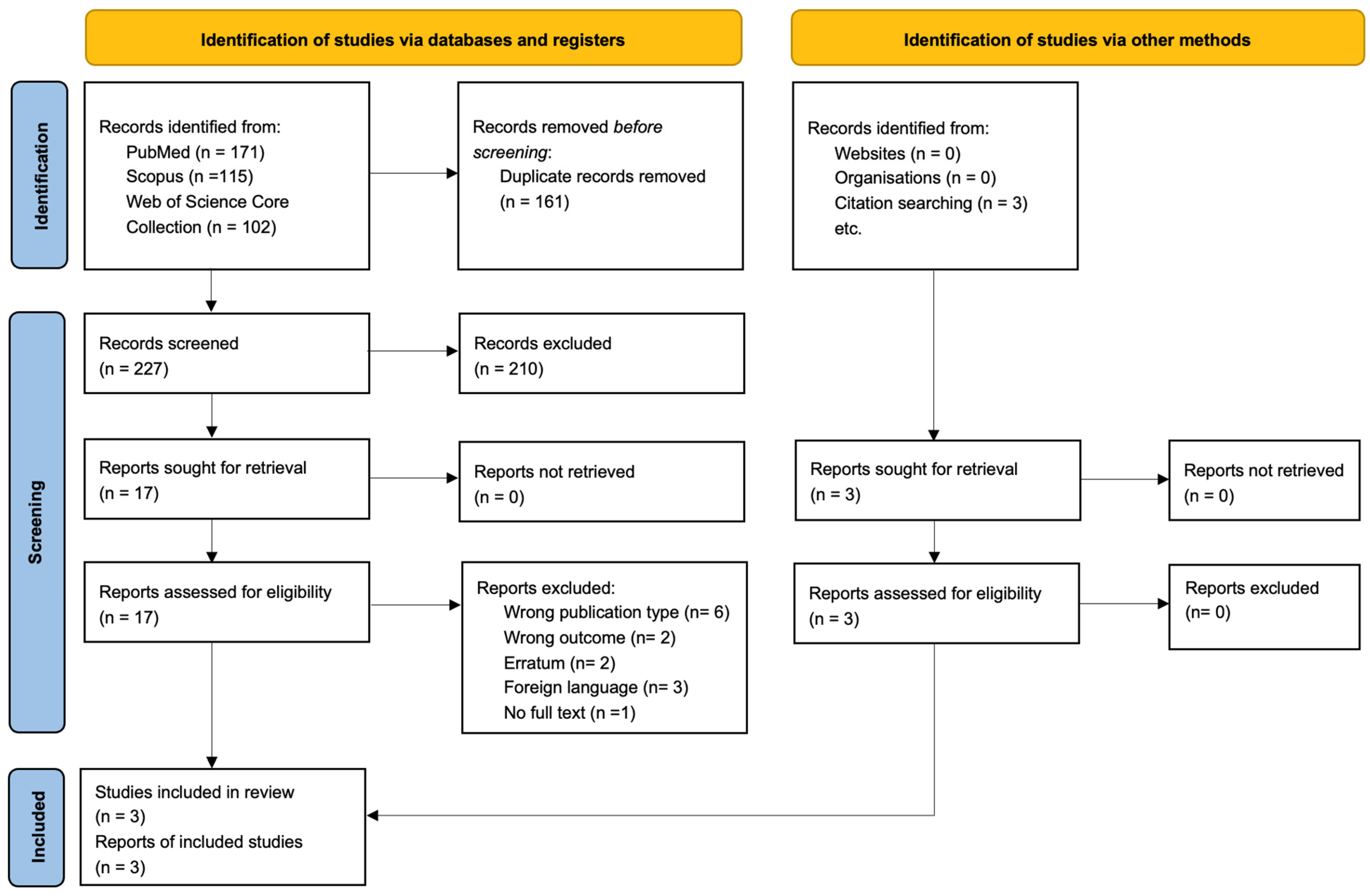
3.1. Literature Search and Study Characteristics
3.2. Outcomes of Interest
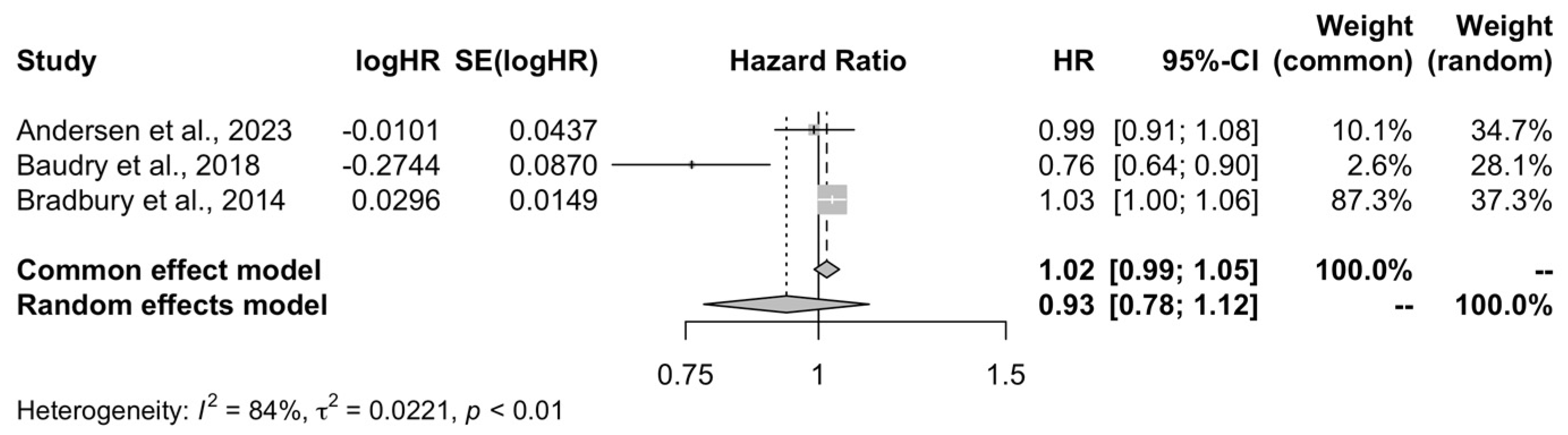
3.2.1. Overall Cancer
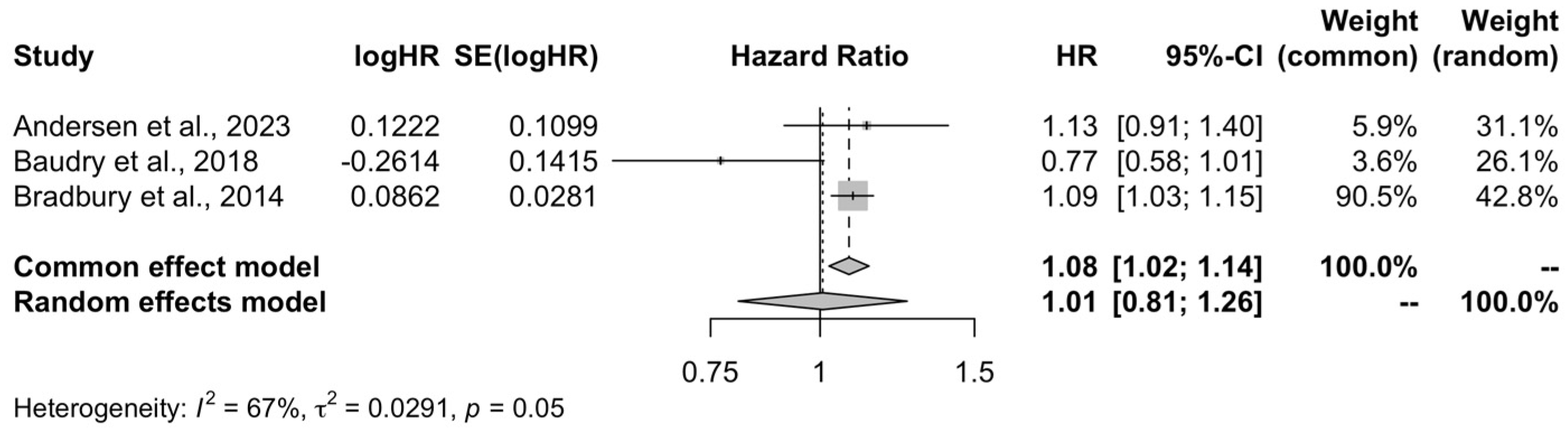
3.2.2. Breast Cancer
3.2.3. Colorectal Cancer
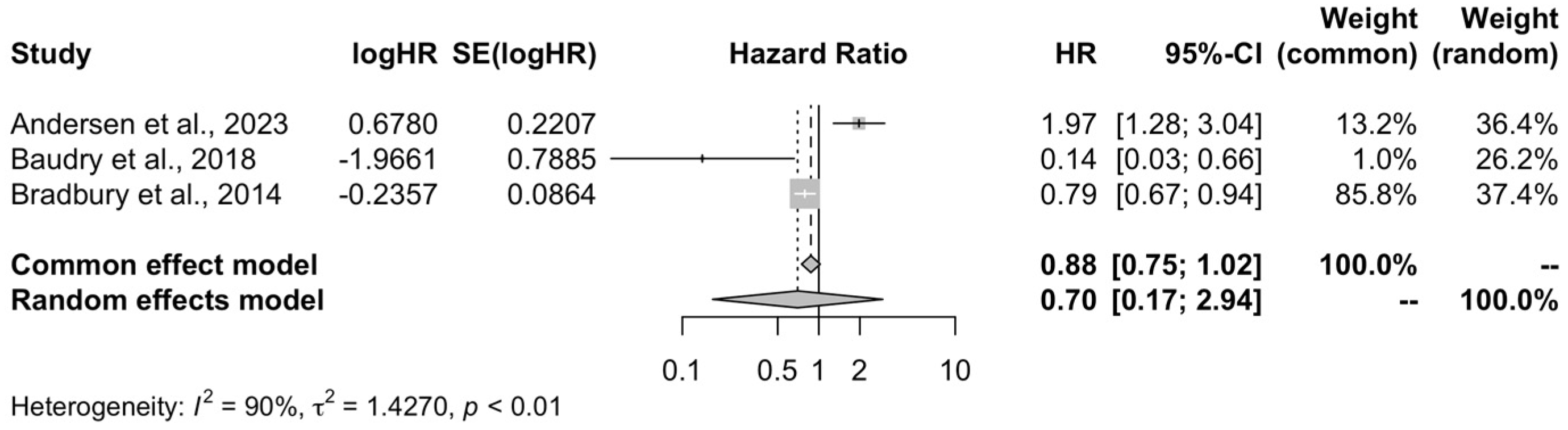
3.2.4. Non-Hodgkin Lymphoma
3.2.5. Site-Specific Cancer
3.3. Risk of Bias Assessment
3.4. Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization: Regional Office For Europe. World Cancer Report: Cancer Research for Cancer Development; IARC: Lyon, France, 2020; ISBN 9789283204473. [Google Scholar]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease 2019 Cancer Collaboration. Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life Years for 29 Cancer Groups from 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022, 8, 420–444. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- Donaldson, M.S. Nutrition and Cancer: A Review of the Evidence for an Anti-Cancer Diet. Nutr. J. 2004, 3, 19. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund; American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. Continuous Update Project Expert Report; World Cancer Research Fund International: London, UK, 2018. [Google Scholar]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean Diet: A Review. Nutrients 2019, 11, 2059. [Google Scholar] [CrossRef]
- Bishop, B. Organic Food in Cancer Therapy. Nutr. Health 1988, 6, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Vigar, V.; Myers, S.; Oliver, C.; Arellano, J.; Robinson, S.; Leifert, C. A Systematic Review of Organic versus Conventional Food Consumption: Is There a Measurable Benefit on Human Health? Nutrients 2020, 12, 7. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations Organic Agriculture. Available online: https://openknowledge.fao.org/server/api/core/bitstreams/b5377c27-d4b1-4cf1-9186-3eb7e702a18b/content (accessed on 26 January 2023).
- Kesse-Guyot, E.; Baudry, J.; Assmann, K.E.; Galan, P.; Hercberg, S.; Lairon, D. Prospective Association between Consumption Frequency of Organic Food and Body Weight Change, Risk of Overweight or Obesity: Results from the NutriNet-Santé Study. Br. J. Nutr. 2017, 117, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Bhagavathula, A.S.; Vidyasagar, K.; Khubchandani, J. Organic Food Consumption and Risk of Obesity: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 231. [Google Scholar] [CrossRef]
- Torjusen, H.; Brantsæter, A.L.; Haugen, M.; Alexander, J.; Bakketeig, L.S.; Lieblein, G.; Stigum, H.; Næs, T.; Swartz, J.; Holmboe-Ottesen, G.; et al. Reduced Risk of Pre-Eclampsia with Organic Vegetable Consumption: Results from the Prospective Norwegian Mother and Child Cohort Study. BMJ Open 2014, 4, e006143. [Google Scholar] [CrossRef]
- Simões-Wüst, A.P.; Moltó-Puigmartí, C.; Jansen, E.H.J.M.; Van Dongen, M.C.J.M.; Dagnelie, P.C.; Thijs, C. Organic Food Consumption during Pregnancy and Its Association with Health-Related Characteristics: The KOALA Birth Cohort Study. Public Health Nutr. 2017, 20, 2145–2156. [Google Scholar] [CrossRef]
- Petersen, S.B.; Rasmussen, M.A.; Strom, M.; Halldorsson, T.I.; Olsen, S.F. Sociodemographic Characteristics and Food Habits of Organic Consumers—A Study from the Danish National Birth Cohort. Public Health Nutr. 2013, 16, 1810–1819. [Google Scholar] [CrossRef] [PubMed]
- Karavasiloglou, N.; Pannen, S.T.; Jochem, C.; Kuhn, T.; Rohrmann, S. Sustainable Diets and Cancer: A Systematic Review. Curr. Nutr. Rep. 2022, 11, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Brooke, B.S.; Schwartz, T.A.; Pawlik, T.M. MOOSE Reporting Guidelines for Meta-Analyses of Observational Studies. JAMA Surg. 2021, 156, 787–788. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.L.M.; Frederiksen, K.; Hansen, J.; Kyrø, C.; Overvad, K.; Tjønneland, A.; Olsen, A.; Raaschou-Nielsen, O. Organic Food Consumption and the Incidence of Cancer in the Danish Diet, Cancer and Health Cohort. Eur. J. Epidemiol. 2023, 38, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Baudry, J.; Assmann, K.E.; Touvier, M.; Allès, B.; Seconda, L.; Latino-Martel, P.; Ezzedine, K.; Galan, P.; Hercberg, S.; Lairon, D.; et al. Association of Frequency of Organic Food Consumption With Cancer Risk: Findings From the NutriNet-Santé Prospective Cohort Study. JAMA Intern. Med. 2018, 178, 1597–1606. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, K.E.; Balkwill, A.; Spencer, E.A.; Roddam, A.W.; Reeves, G.K.; Green, J.; Key, T.J.; Pirie, K.; Banks, E.; Beral, V.; et al. Organic Food Consumption and the Incidence of Cancer in a Large Prospective Study of Women in the United Kingdom. Br. J. Cancer 2014, 110, 2321–2326. [Google Scholar] [CrossRef] [PubMed]
- ROBINS-E Development Group Risk of Bias in Non-Randomized Studies—Of Exposure (ROBINS-E). Available online: https://pubmed.ncbi.nlm.nih.gov/38555664/ (accessed on 13 November 2024).
- Veroniki, A.A.; Jackson, D.; Viechtbauer, W.; Bender, R.; Bowden, J.; Knapp, G.; Kuss, O.; Higgins, J.P.; Langan, D.; Salanti, G. Methods to Estimate the Between-Study Variance and Its Uncertainty in Meta-Analysis. Res. Synth. Methods 2016, 7, 55–79. [Google Scholar] [CrossRef]
- Ramachandran, K.M.; Tsokos, C.P. Chapter 14—Some Issues in Statistical Applications: An Overview. In Mathematical Statistics with Applications in R, 3rd ed.; Ramachandran, K.M., Tsokos, C.P., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 569–613. ISBN 978-0-12-817815-7. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019; ISBN 9781119536604. [Google Scholar]
- Katzke, V.A.; Kaaks, R.; Kühn, T. Lifestyle and Cancer Risk. Cancer J. 2015, 21, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.L.; Thomson, C.; Gansler, T.; Gapstur, S.M.; McCullough, M.L.; Patel, A.V.; Andrews, K.S.; Bandera, E.V.; Spees, C.K.; Robien, K.; et al. American Cancer Society Guideline for Diet and Physical Activity for Cancer Prevention. CA Cancer J. Clin. 2020, 70, 245–271. [Google Scholar] [CrossRef]
- Hemler, E.C.; Chavarro, J.E.; Hu, F.B. Organic Foods for Cancer Prevention-Worth the Investment? JAMA Intern. Med. 2018, 178, 1606–1607. [Google Scholar] [CrossRef]
- Guyton, K.Z.; Loomis, D.; Grosse, Y.; el Ghissassi, F.; Benbrahim-Tallaa, L.; Guha, N.; Scoccianti, C.; Mattock, H.; Straif, K.; Blair, A.; et al. Carcinogenicity of Tetrachlorvinphos, Parathion, Malathion, Diazinon, and Glyphosate. Lancet Oncol. 2015, 16, 490–491. [Google Scholar] [CrossRef]
- Alavanja, M.C.R.; Ross, M.K.; Bonner, M.R. Increased Cancer Burden among Pesticide Applicators and Others Due to Pesticide Exposure. CA Cancer J. Clin. 2013, 63, 120–142. [Google Scholar] [CrossRef] [PubMed]
- Maele-Fabry, G.V.; Willems, J.L. Occupation Related Pesticide Exposure and Cancer of the Prostate: A Meta-Analysis. Occup. Environ. Med. 2003, 60, 634. [Google Scholar] [CrossRef] [PubMed]
- Pardo, L.A.; Beane Freeman, L.E.; Lerro, C.C.; Andreotti, G.; Hofmann, J.N.; Parks, C.G.; Sandler, D.P.; Lubin, J.H.; Blair, A.; Koutros, S. Pesticide Exposure and Risk of Aggressive Prostate Cancer among Private Pesticide Applicators. Environ. Health 2020, 19, 30. [Google Scholar] [CrossRef]
- Panis, C.; Candiotto, L.Z.P.; Gaboardi, S.C.; Gurzenda, S.; Cruz, J.; Castro, M.; Lemos, B. Widespread Pesticide Contamination of Drinking Water and Impact on Cancer Risk in Brazil. Environ. Int. 2022, 165, 107321. [Google Scholar] [CrossRef] [PubMed]
- Schinasi, L.; Leon, M.E. Non-Hodgkin Lymphoma and Occupational Exposure to Agricultural Pesticide Chemical Groups and Active Ingredients: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2014, 11, 4449–4527. [Google Scholar] [CrossRef]
- Gatto, N.M.; Ogata, P.; Lytle, B. Farming, Pesticides, and Brain Cancer: A 20-Year Updated Systematic Literature Review and Meta-Analysis. Cancers 2021, 13, 4477. [Google Scholar] [CrossRef] [PubMed]
- International Agency for Research on Cancer (IARC). Some Organophosphate Insecticides and Herbicides Volume 112 Iarc Monographs on the Evaluation of Carcinogenic Risks to Humans; IARC: Lyon, France, 2017. [Google Scholar]
- Zhang, L.; Rana, I.; Shaffer, R.M.; Taioli, E.; Sheppard, L. Exposure to glyphosate-based herbicides and risk for non-Hodgkin lymphoma: A meta-analysis and supporting evidence. Mutat. Res. Rev. Mutat. Res. 2019, 781, 186–206. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.F.S.; Mattos, I.E.; Luz, L.L.; Carmo, C.N.; Aydos, R.D. Exposure to pesticides and prostate cancer: Systematic review of the literature. Rev. Environ. Health 2016, 31, 311–327. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.C.; Wigle, D.T.; Krewski, D. Residential Pesticides and Childhood Leukemia: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2010, 118, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Mie, A.; Andersen, H.R.; Gunnarsson, S.; Kahl, J.; Kesse-Guyot, E.; Rembiałkowska, E.; Quaglio, G.; Grandjean, P. Human Health Implications of Organic Food and Organic Agriculture: A Comprehensive Review. Environ. Health 2017, 16, 111. [Google Scholar] [CrossRef] [PubMed]
- Smith-Spangler, C.; Brandeau, M.L.; Hunter, G.E.; Clay Bavinger, J.; Pearson, M.; Eschbach, P.J.; Sundaram, V.; Liu, H.; Schirmer, P.; Stave, C.; et al. Are Organic Foods Safer or Healthier than Conventional Alternatives?: A Systematic Review. Ann. Intern. Med. 2012, 157, 348–366. [Google Scholar] [CrossRef] [PubMed]
- Dangour, A.D.; Lock, K.; Hayter, A.; Aikenhead, A.; Allen, E.; Uauy, R. Nutrition-Related Health Effects of Organic Foods: A Systematic Review. Am. J. Clin. Nutr. 2010, 92, 203–210. [Google Scholar] [CrossRef]
- Brantsæter, A.L.; Ydersbond, T.A.; Hoppin, J.A.; Haugen, M.; Meltzer, H.M. Organic Food in the Diet: Exposure and Health Implications. Annu. Rev. Public Health 2017, 38, 295–313. [Google Scholar] [CrossRef] [PubMed]
- Kesse-Guyot, E.; Péneau, S.; Méjean, C.; Szabo de Edelenyi, F.; Galan, P.; Hercberg, S.; Lairon, D. Profiles of Organic Food Consumers in a Large Sample of French Adults: Results from the Nutrinet-Santé Cohort Study. PLoS ONE 2013, 8, e76998. [Google Scholar] [CrossRef]
- Baudry, J.; Méjean, C.; Péneau, S.; Galan, P.; Hercberg, S.; Lairon, D.; Kesse-Guyot, E. Health and Dietary Traits of Organic Food Consumers: Results from the NutriNet-Santé Study. Br. J. Nutr. 2015, 114, 2064–2073. [Google Scholar] [CrossRef]
- Mctiernan, A.; Friedenreich, C.M.; Katzmarzyk, P.T.; Powell, K.E.; Macko, R.; Buchner, D.; Pescatello, L.S.; Bloodgood, B.; Tennant, B.; Vaux-Bjerke, A.; et al. Physical Activity in Cancer Prevention and Survival: A Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1252–1261. [Google Scholar] [CrossRef] [PubMed]
- Freisling, H.; Arnold, M.; Soerjomataram, I.; O’Doherty, M.G.; Ordóñez-Mena, J.M.; Bamia, C.; Kampman, E.; Leitzmann, M.; Romieu, I.; Kee, F.; et al. Comparison of General Obesity and Measures of Body Fat Distribution in Older Adults in Relation to Cancer Risk: Meta-Analysis of Individual Participant Data of Seven Prospective Cohorts in Europe. Br. J. Cancer 2017, 116, 1486–1497. [Google Scholar] [CrossRef]
- Nussbaumer-Streit, B.; Klerings, I.; Dobrescu, A.I.; Persad, E.; Stevens, A.; Garritty, C.; Kamel, C.; Affengruber, L.; King, V.J.; Gartlehner, G. Excluding Non-English Publications from Evidence-Syntheses Did Not Change Conclusions: A Meta-Epidemiological Study. J. Clin. Epidemiol. 2020, 118, 42–54. [Google Scholar] [CrossRef] [PubMed]
- Dobrescu, A.I.; Nussbaumer-Streit, B.; Klerings, I.; Wagner, G.; Persad, E.; Sommer, I.; Herkner, H.; Gartlehner, G. Restricting Evidence Syntheses of Interventions to English-Language Publications Is a Viable Methodological Shortcut for Most Medical Topics: A Systematic Review. J. Clin. Epidemiol. 2021, 137, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.-S.; Oh, K.; Kim, H.C. Dietary Assessment Methods in Epidemiologic Studies. Epidemiol. Health 2014, 36, e2014009. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture, A.M.S. Labeling Organic Products. Available online: https://www.ams.usda.gov/rules-regulations/organic/labeling (accessed on 13 November 2024).
- Agriculture and Rural Development Organic Production and Products. Available online: https://agriculture.ec.europa.eu/farming/organic-farming/organic-production-and-products_en (accessed on 13 November 2024).
- Fewell, Z.; Davey Smith, G.; Sterne, J.A.C. The Impact of Residual and Unmeasured Confounding in Epidemiologic Studies: A Simulation Study. Am. J. Epidemiol. 2007, 166, 646–655. [Google Scholar] [CrossRef] [PubMed]
- Young, L.M.; Gauci, S.; Scholey, A.; White, D.J.; Pipingas, A. Self-Selection Bias: An Essential Design Consideration for Nutrition Trials in Healthy Populations. Front. Nutr. 2020, 7, 7983. [Google Scholar] [CrossRef]
- Heaney, R.P. Guidelines for Optimizing Design and Analysis of Clinical Studies of Nutrient Effects. Nutr. Rev. 2014, 72, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Hyland, C.; Bradman, A.; Gerona, R.; Patton, S.; Zakharevich, I.; Gunier, R.B.; Klein, K. Organic Diet Intervention Significantly Reduces Urinary Pesticide Levels in U.S. Children and Adults. Environ. Res. 2019, 171, 568–575. [Google Scholar] [CrossRef] [PubMed]

| PICO Acronym Criteria | PICO Items Relevant to Eligibility Criteria |
|---|---|
| P—Population | Adult population without a cancer diagnosis |
| I—Intervention | High consumption of organic foods |
| C—Control | Low or no consumption of organic foods |
| O—Outcome | Overall and site-specific cancer risk |
| S—Study Design | Observational studies |
| First Author, Year, Country | Sample Size 1 | Population | Exposure Assessment | Outcome Assessment | Follow-Up (Mean Years) | Covariates |
|---|---|---|---|---|---|---|
| Andersen et al., 2023 [19], Denmark | Total: 41,928 Never: 6184 Low: 16,246 Medium: 15,374 High: 4124 | Danish adults aged 50–65 years with no previous cancer diagnosis | Follow-up FFQ (questions about the consumption of or organically produced foods) and a follow-up lifestyle questionnaire. | Linkage with the Danish Cancer Registry | 15 | Educational level, BMI, PA, smoking habits |
| Baudry et al., 2018 [20], France | Total: 68,946 Q1: 16,831 Q2: 17,644 Q3: 17,240 Q4: 17,231 | French adult volunteers with access to the internet | Self-administrated questionnaires, 24 h records, and anthropometric questionnaires. | Self-reported health events through yearly health status questionnaire | 4.56 | Age, sex, month of inclusion, occupational status, educational level, marital status, monthly income per household unit, PA, smoking status, alcohol intake, family history of cancer, BMI, height, energy intake, mPNNS-GS, fiber intake, processed meat intake, red meat intake, ultra-processed food consumption, fruit and vegetable consumption, dietary patterns, and (for women) parity, postmenopausal status, use of hormonal treatment for menopause, and use of oral contraception |
| Bradbury et al., 2014 [21], United Kingdom | Total: 623,080 Never: 187,451 Sometimes: 390,040 Usually/Always: 45,589 | Middle-aged women who had been invited for breast cancer screening at screening centers | At the 3-year survey, women were asked ‘Do you eat organic food?’ with four possible categorical responses. Women were also asked if they had changed their diet because of illness in the previous 5 years. The same questions were asked in the 8-year survey. | Participants are flagged on the NHSCR, so that cancer registrations and deaths are routinely notified to the study investigators by the Office for National Statistics, England, and the Information Services Division, Scotland | 9.3 | Age, geographical region, socioeconomic status, BMI, height, smoking status, alcohol intake, strenuous PA, age at first birth, fiber intake, type of meat eaten |
| Andersen et al., 2023 1 [19] | Baudry et al., 2018 2 [20] | Bradbury et al., 2014 3 [21] | |
|---|---|---|---|
| Overall cancer | 0.99 (0.91–1.08) | 0.76 (0.64–0.90) | 1.03 (1.00–1.06) |
| Pancreas cancer | 1.00 (0.61–1.65) | 1.06 (0.87–1.29) | |
| Lung cancer | 0.79 (0.60–1.04) | 0.98 (0.88–1.10) | |
| Stomach cancer | 0.54 (0.27–1.07) | 0.92 (0.67–1.26) | |
| Colorectal cancer | 0.98 (0.77–1.24) | 0.87 (0.45–1.57) | 1.02 (0.93–1.12) |
| Urinary bladder cancer | 0.91 (0.62–1.31) | ||
| Non-Hodgkin lymphoma | 1.97 (1.28–3.04) | 0.14 (0.03–1.05) | 0.79 (0.67–0.94) |
| Breast cancer | 1.13 (0.91–1.40) | 0.77 (0.58–1.01) | 1.09 (1.03–1.15) |
| Premenopausal breast cancer | 0.89 (0.59–1.35) | ||
| Postmenopausal breast cancer | 0.66 (0.45–0.96) | ||
| Prostate cancer | 0.95 (0.78–1.15) | 1.00 (0.63–1.60) | |
| Skin cancer | 0.63 (0.38–1.05) | ||
| Kidney cancer | 0.83 (0.64–1.08) | ||
| Brain cancer | 1.16 (0.97–1.40) | ||
| Leukemia | 0.92 (0.72–1.18) | ||
| Malignant melanoma | 0.90 (0.78–1.05) | ||
| Esophagus | 0.83 (0.62–1.12) | ||
| Oral cavity | 1.04 (0.78–1.39) | ||
| Uterus | 1.14 (1.00–1.29) | ||
| Ovary | 0.96 (0.83–1.11) | ||
| Bladder cancer | 1.08 (0.82–1.41) | ||
| Multiple myeloma | 1.03 (0.81–1.32) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theodoridis, X.; Papaemmanouil, A.; Papageorgiou, N.; Georgakou, A.V.; Kalaitzopoulou, I.; Stamouli, M.; Chourdakis, M. The Level of Adherence to Organic Food Consumption and Risk of Cancer: A Systematic Review and Meta-Analysis. Life 2025, 15, 160. https://doi.org/10.3390/life15020160
Theodoridis X, Papaemmanouil A, Papageorgiou N, Georgakou AV, Kalaitzopoulou I, Stamouli M, Chourdakis M. The Level of Adherence to Organic Food Consumption and Risk of Cancer: A Systematic Review and Meta-Analysis. Life. 2025; 15(2):160. https://doi.org/10.3390/life15020160
Chicago/Turabian StyleTheodoridis, Xenophon, Androniki Papaemmanouil, Niki Papageorgiou, Athina Vasiliki Georgakou, Ioustini Kalaitzopoulou, Marilena Stamouli, and Michail Chourdakis. 2025. "The Level of Adherence to Organic Food Consumption and Risk of Cancer: A Systematic Review and Meta-Analysis" Life 15, no. 2: 160. https://doi.org/10.3390/life15020160
APA StyleTheodoridis, X., Papaemmanouil, A., Papageorgiou, N., Georgakou, A. V., Kalaitzopoulou, I., Stamouli, M., & Chourdakis, M. (2025). The Level of Adherence to Organic Food Consumption and Risk of Cancer: A Systematic Review and Meta-Analysis. Life, 15(2), 160. https://doi.org/10.3390/life15020160







