Neonatal and Birth Risk Factors for Type 1 Diabetes Mellitus: Prediction Using an Artificial Neural Network
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Data Processing
2.3. Artificial Neural Network Architecture
- TP = True Positives;
- TN = True Negatives;
- FP = False Positives;
- FN = False Negatives.
3. Results
3.1. Comparisons Between Groups
3.2. Relationships Between Variables
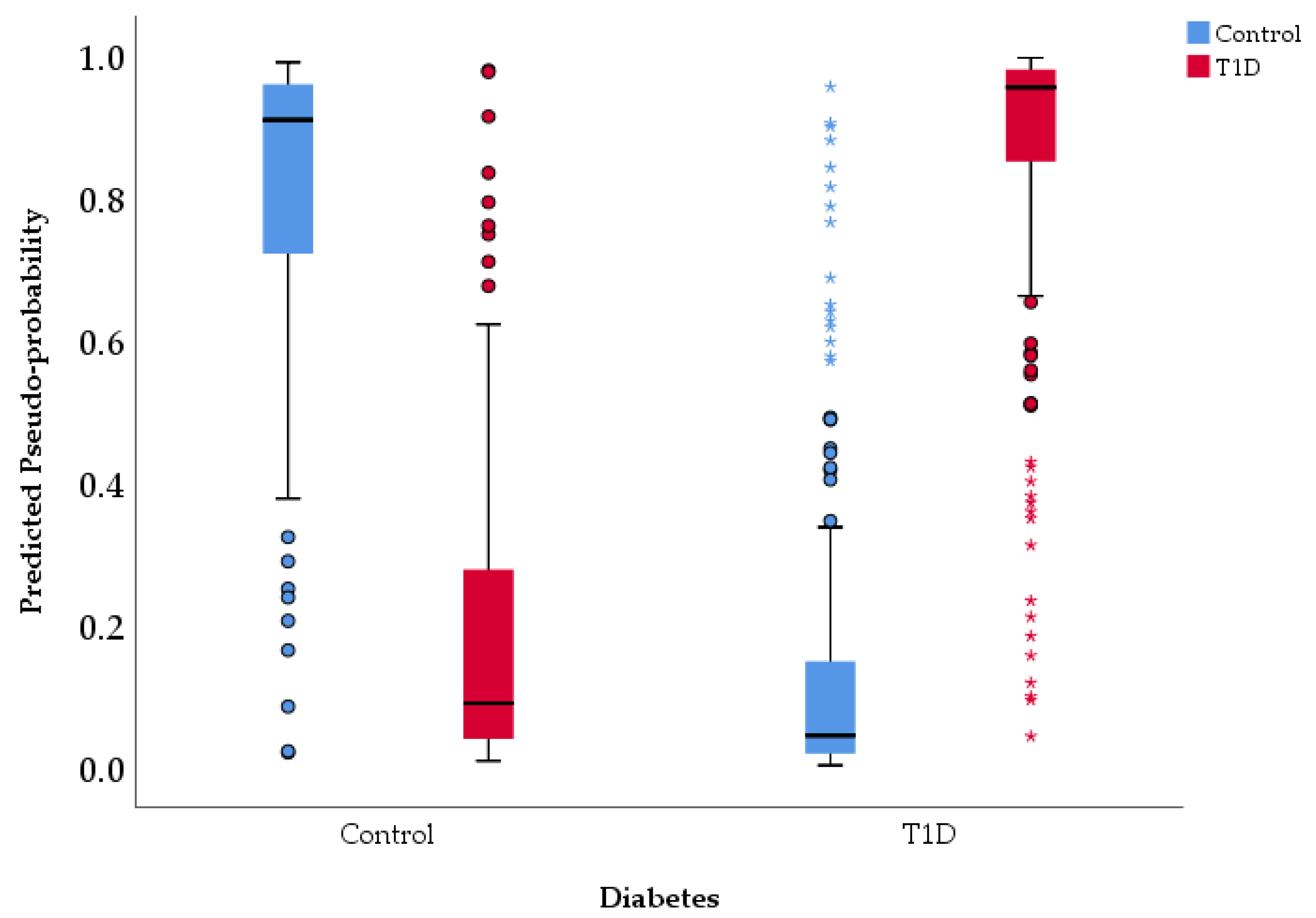
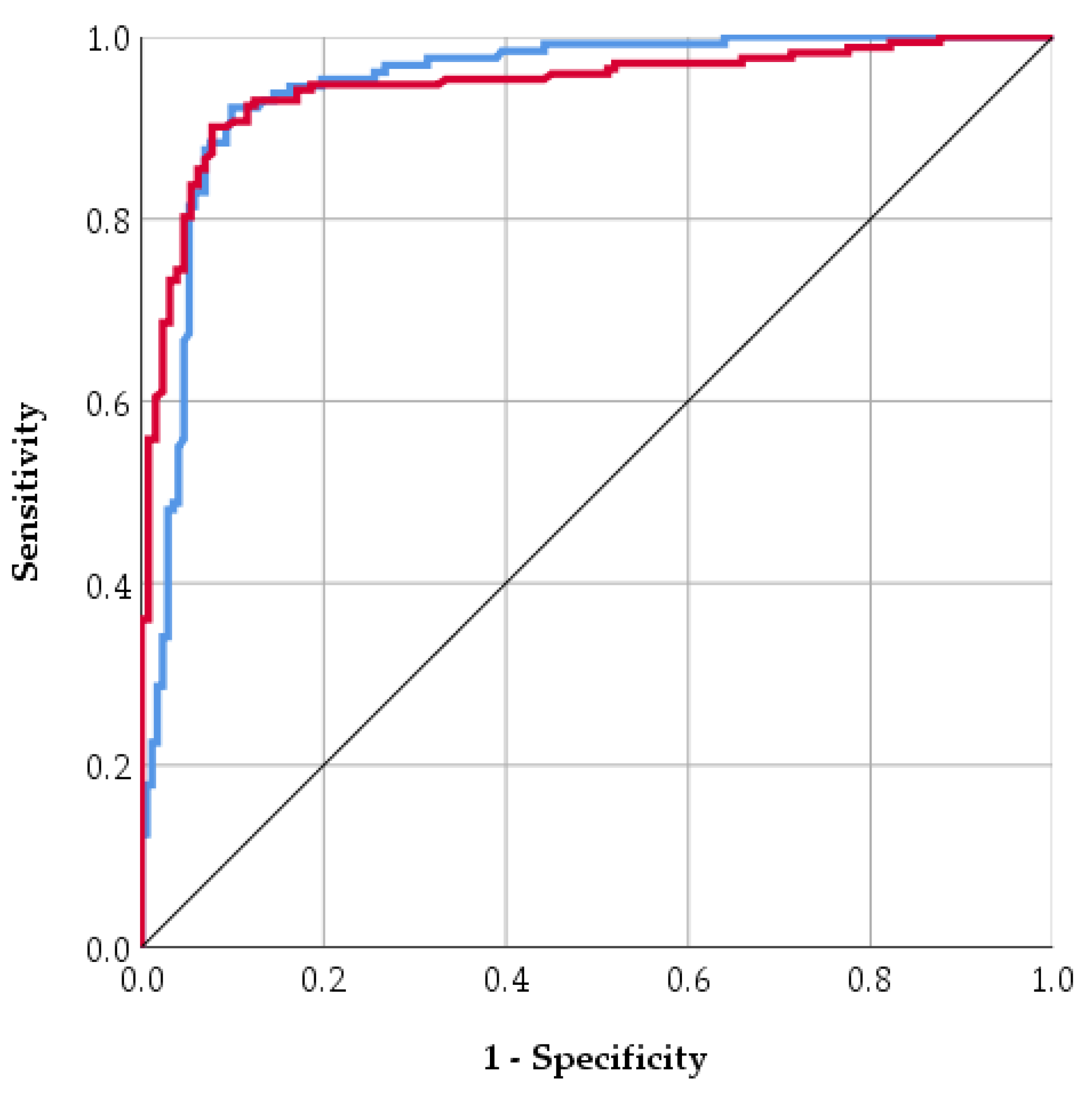
3.3. Multivariate Analysis and Artificial Neural Network for T1D
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lawlor, D.A. The society for social medicine John Pemberton Lecture 2011. Developmental overnutrition-an old hypothesis with new importance. Int. J. Epidemiol. 2013, 42, 7–29. [Google Scholar] [CrossRef] [PubMed]
- Metsälä, J.; Hakola, L.; Lundqvist, A.; Virta, L.J.; Gissler, M.; Virtanen, S.M. Perinatal factors and the risk of Type 1 Diabetes Mellitus in childhood and adolescence—A register-based case-cohort study in Finland, years 1987 to 2009. Pediatr. Diabetes 2020, 21, 586–596. [Google Scholar] [CrossRef] [PubMed]
- Censin, J.C.; Nowak, C.; Cooper, N.; Bergsten, P.; Todd, J.A.; Fall, T. Childhood adiposity and risk of Type 1 Diabetes Mellitus: A Mendelian randomization study. PLoS Med. 2017, 14, e1002362. [Google Scholar] [CrossRef]
- Anghel, L.; Cobuz, C.; Benchea, L.C.; Maciuc, V.; Cobuz, M.; Sascău, R.A.; Stătescu, C. Sudomotor Dysfunction as an Early Marker of Autonomic and Cardiovascular Risk in Diabetes: Insights from a Cross-Sectional Study Using SUDOSCAN. Biosensors 2025, 15, 372. [Google Scholar] [CrossRef]
- Lee, H.S.; Hwang, J.S. Genetic aspects of Type 1 Diabetes Mellitus. Ann. Pediatr. Endocrinol. Metab. 2019, 24, 143–148. [Google Scholar] [CrossRef]
- Robertson, L.; Harrild, K. Maternal and neonatal risk factors for childhood Type 1 Diabetes Mellitus: A matched case-control study. BMC Public Health 2010, 10, 281. [Google Scholar] [CrossRef]
- Ornoy, A.; Becker, M.; Weinstein-fudim, L.; Ergaz, Z. Diabetes during Pregnancy: A Maternal Disease Complicating the Course of Pregnancy with Long-Term Deleterious Effects on the Offspring. A Clinical Review. Int. J. Mol. Sci. 2021, 22, 2965. [Google Scholar] [CrossRef]
- Freinkel, N. Banting Lecture 1980 Of Pregnancy and Progeny. Diabetes 1980, 29, 1023–1035. [Google Scholar] [CrossRef]
- Lindell, N.; Bladh, M.; Carlsson, A.; Josefsson, A.; Aakesson, K.; Samuelsson, U. Size for gestational age affects the risk for Type 1 Diabetes Mellitus in children and adolescents: A Swedish national case–control study. Diabetologia 2021, 64, 1113–1120. [Google Scholar] [CrossRef]
- Zhang, Z.; Feng, Y.; Zhang, Y.; Li, X.; Li, Y.; Sun, L.; Li, X.; Du, H.; Zhang, J. Predicting Neonatal Hypoglycemia Using AI Neural Networks in Infants from Mothers with Gestational Diabetes Mellitus. Med. Sci. Monit. 2024, 30, e944513. [Google Scholar] [CrossRef]
- Haynes, A.; Bower, C.; Bulsara, M.K.; Finn, J.; Jones, T.W.; Davis, E.A. Perinatal risk factors for childhood Type 1 Diabetes Mellitus in Western Australia—A population-based study (1980–2002). Diabet. Med. 2007, 24, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Cardwell, C.R.; Stene, L.C.; Joner, G.; Davis, E.A.; Cinek, O.; Rosenbauer, J.; Ludvigsson, J.; Castell, C.; Svensson, J.; Goldacre, M.J.; et al. Birthweight and the risk of childhood-onset Type 1 Diabetes Mellitus: A meta-analysis of observational studies using individual patient data. Diabetologia 2010, 53, 641–651. [Google Scholar] [CrossRef] [PubMed]
- Güngör, D.; Nadaud, P.; Lapergola, C.C.; Dreibelbis, C.; Wong, Y.P.; Terry, N.; Abrams, S.A.; Beker, L.; Jacobovits, T.; Järvinen, K.M.; et al. Prácticas de alimentación con leche infantil y resultados de la diabetes en la descendencia: Una revisión sistemática. Am. J. Clin. Nutr. 2019, 109, 817S. [Google Scholar] [CrossRef]
- Lund-Blix, N.A.; Sander, S.D.; Størdal, K.; Nybo Andersen, A.M.; Rønningen, K.S.; Joner, G.; Skrivarhaug, T.; Njølstad, P.R.; Husby, S.; Stene, L.C. Infant feeding and risk of Type 1 Diabetes Mellitus in two large scandinavian birth cohorts. Diabetes Care 2017, 40, 920–927. [Google Scholar] [CrossRef]
- Cardwell, C.R.; Stene, L.C.; Joner, G.; Cinek, O.; Svensson, J.; Goldacre, M.J.; Parslow, R.C.; Pozzilli, P.; Brigis, G.; Stoyanov, D.; et al. Caesarean section is associated with an increased risk of childhood-onset Type 1 Diabetes Mellitus mellitus: A meta-analysis of observational studies. Diabetologia 2008, 51, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Yasmin, F.; Tun, H.M.; Konya, T.B.; Guttman, D.S.; Chari, R.S.; Field, C.J.; Becker, A.B.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; et al. Cesarean section, formula feeding, and infant antibiotic exposure: Separate and combined impacts on gut microbial changes in later infancy. Front. Pediatr. 2017, 5, 288753. [Google Scholar] [CrossRef]
- Cobuz, C.; Ungureanu-Iuga, M.; Anton-Paduraru, D.-T.; Cobuz, M. Possible Use of the SUDOSCAN Nephropathy Risk Score in Chronic Kidney Disease Diagnosis: Application in Patients with Type 2 Diabetes. Biosensors 2025, 15, 620. [Google Scholar] [CrossRef]
- Caicedo, R.A.; Li, N.; Robert, C.D.; Scumpia, P.O.; Hubsher, C.P.; Wasserfall, C.H.; Schatz, D.A.; Atkinson, M.A.; Neu, J. Neonatal formula feeding leads to immunological alterations in an animal model of Type 1 Diabetes Mellitus. Pediatr. Res. 2008, 63, 303–307. [Google Scholar] [CrossRef]
- Dahlquist, G.G.; Pundziūtė-Lyckå, A.; Nyström, L. Birthweight and risk of Type 1 Diabetes Mellitus in children and young adults: A population-based register study. Diabetologia 2005, 48, 1114–1117. [Google Scholar] [CrossRef]
- Harder, T.; Roepke, K.; Diller, N.; Stechling, Y.; Dudenhausen, J.W.; Plagemann, A. Birth weight, early weight gain, and subsequent risk of Type 1 Diabetes Mellitus: Systematic review and meta-analysis. Am. J. Epidemiol. 2009, 169, 1428–1436. [Google Scholar] [CrossRef]
- Meah, F.A.; DiMeglio, L.A.; Greenbaum, C.J.; Blum, J.S.; Sosenko, J.M.; Pugliese, A.; Geyer, S.; Xu, P.; Evans-Molina, C. The relationship between BMI and insulin resistance and progression from single to multiple autoantibody positivity and Type 1 Diabetes Mellitus among TrialNet Pathway to Prevention participants. Diabetologia 2016, 59, 1186–1195. [Google Scholar] [CrossRef]
- Yu, Z.B.; Han, S.P.; Zhu, G.Z.; Zhu, C.; Wang, X.J.; Cao, X.G.; Guo, X.R. Birth weight and subsequent risk of obesity: A systematic review and meta-analysis. Obes. Rev. 2011, 12, 525–542. [Google Scholar] [CrossRef]
- Dabelea, D.; Crume, T. Maternal environment and the transgenerational cycle of obesity and diabetes. Diabetes 2011, 60, 1849–1855. [Google Scholar] [CrossRef]
- Getaneh, T.; Negesse, A.; Dessie, G.; Desta, M.; Temesgen, H.; Getu, T.; Gelaye, K. Impact of cesarean section on timely initiation of breastfeeding in Ethiopia: A systematic review and meta-analysis. Int. Breastfeed. J. 2021, 16, 51. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, J.; Liu, Y.; Li, Y.; Li, Z. The association between cesarean delivery on maternal request and method of newborn feeding in china. PLoS ONE 2012, 7, e37336. [Google Scholar] [CrossRef] [PubMed]
- Anton-Paduraru, D.; Mindru, D.E.; Stefania, R.; Trofin, F.; Cobuz, C.; Cobuz, M.; Sur, L.M.; Petroaie, A.; Maria, A.; Manole, M.; et al. Unraveling Metabolic Syndrome in Youth: The Obesity Epidemic’ s Hidden Complication. Children 2025, 12, 482. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Frequency | Percent (%) |
|---|---|---|
| Birth weight class | ||
| Aga | 226 | 69.1 |
| Lga | 82 | 25.1 |
| Sga | 19 | 5.8 |
| Nutrition type | ||
| Breast milk | 154 | 47.1 |
| Formula | 173 | 52.9 |
| Sex | ||
| Men | 169 | 51.7 |
| Women | 158 | 48.3 |
| Delivery type | ||
| Vaginal | 125 | 38.2 |
| Cesarean section | 202 | 61.8 |
| Diabetes risk | ||
| Control | 149 | 45.6 |
| T1D | 178 | 54.4 |
| Input Layer | Factors | 1 | Nutrition type |
| 2 | Birth weight | ||
| 3 | Apgar score | ||
| Covariates | 1 | Sex | |
| 2 | Delivery type | ||
| Number of Units | 99 | ||
| Rescaling Method for Covariates | Standardized | ||
| Hidden Layer(s) | Number of Hidden Layers | 1 | |
| Number of Units in Hidden Layer 1 | 3 | ||
| Activation Function | Hyperbolic tangent | ||
| Output Layer | Dependent Variable | Diabetes risk | |
| Number of Units | 2 | ||
| Activation Function | Softmax | ||
| Error Function | Cross-entropy | ||
| Training time | 0.15 s | ||
| Inference time | 0.003 s | ||
| Diabetes Type | Birth Weight Class | Nutrition Type | Birth Weight | Sex | Apgar Score | Delivery Type | |
|---|---|---|---|---|---|---|---|
| Mean | Control | 1.14 | 1.30 | 3313.76 | 1.49 | 8.80 | 1.52 |
| T1D | 1.56 | 1.72 | 3828.31 | 1.48 | 8.04 | 1.70 | |
| Std. Deviation | Control | 0.44 | 0.46 | 473.84 | 0.50 | 0.89 | 0.50 |
| T1D | 0.64 | 0.45 | 912.14 | 0.50 | 1.07 | 0.46 | |
| Median | Control | 1.00 | 1.00 | 3280.00 | 1.00 | 9.00 | 2.00 |
| T1D | 1.00 | 2.00 | 3800.00 | 1.00 | 8.00 | 2.00 | |
| Std. Error of Mean | Control | 0.04 | 0.04 | 38.82 | 0.04 | 0.07 | 0.04 |
| T1D | 0.05 | 0.03 | 68.37 | 0.04 | 0.08 | 0.03 | |
| Mann–Whitney U test (p-value) | 0.00 | 0.00 | 0.00 | 0.91 | 0.00 | 0.00 | |
| Birth Weight Class | Nutrition Type | Birth Weight | Sex | Apgar Score | Delivery Type | Diabetes Risk | |
|---|---|---|---|---|---|---|---|
| Birth weight class | 1.00 | ||||||
| Nutrition type | 0.34 ** | 1.00 | |||||
| Birth weight | 0.42 ** | 0.36 ** | 1.00 | ||||
| Sex | 0.01 | −0.02 | −0.06 | 1.00 | |||
| Apgar score | −0.27 ** | −0.19 ** | −0.12 * | 0.01 | 1.00 | ||
| Delivery type | 0.30 ** | 0.39 ** | 0.32 ** | 0.02 | −0.08 | 1.00 | |
| Diabetes risk | 0.40 ** | 0.43 ** | 0.34 ** | −0.01 | −0.37 ** | 0.19 ** | 1.00 |
| Component | Initial Eigenvalues | % of Variance | Cumulative % |
|---|---|---|---|
| PC1 | 2.38 | 33.93 | 33.93 |
| PC2 | 1.09 | 15.60 | 49.54 |
| PC3 | 1.01 | 14.41 | 63.94 |
| Kaiser–Meyer–Olkin Measure of Sampling Adequacy | 0.73 | ||
| Bartlett’s Test of Sphericity | Approx. χ2 | 303.23 | |
| df | 21 | ||
| p-value | 0.00 | ||
| Source | Type III SS | df | MS | F | p-Value | ηp2 |
|---|---|---|---|---|---|---|
| Corrected Model | 71.36 | 201.00 | 0.36 | 4.55 | 0.00 | 0.88 |
| Intercept | 11.33 | 1.00 | 11.33 | 145.27 | 0.00 | 0.54 |
| Nutrition type | 0.32 | 1.00 | 0.32 | 4.04 | 0.05 | 0.03 |
| Birth weight | 31.03 | 109.00 | 0.28 | 3.65 | 0.00 | 0.76 |
| Apgar score | 1.86 | 6.00 | 0.31 | 3.98 | 0.00 | 0.16 |
| Nutrition type × Birth weight | 4.34 | 19.00 | 0.23 | 2.93 | 0.00 | 0.31 |
| Nutrition type × Apgar score | 0.55 | 2.00 | 0.28 | 3.55 | 0.03 | 0.05 |
| Birth weight × Apgar score | 4.74 | 46.00 | 0.10 | 1.32 | 0.12 | 0.33 |
| Nutrition type × Birth weight × Apgar score | 0.19 | 3.00 | 0.06 | 0.80 | 0.49 | 0.02 |
| Training | Cross-Entropy Error | 58.01 |
| Percent Incorrect Predictions | 7.10% | |
| Stopping Rule Used | 1 consecutive step(s) with no decrease in error a | |
| Testing | Cross-Entropy Error | 29.15 |
| Percent Incorrect Predictions | 15.8% |
| Metric | Value |
|---|---|
| True Positive (TP) | 41 |
| True Negative (TN) | 23 |
| False Positive (FP) | 7 |
| False Negative (FN) | 5 |
| Accuracy | 84.2% |
| Sensitivity (Recall/True Positive Rate) | 89.1% |
| Specificity (True Negative Rate) | 76.7% |
| Positive Predictive Value (PPV/Precision) | 85.4% |
| Negative Predictive Value (NPV) | 82.1% |
| Area Under the Curve (AUC) | 0.95 |
| Kappa | 0.81 |
| Mean Absolute Error (MAE) | 0.09 |
| Root Mean Squared Error (RMSE) | 0.31 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cobuz, C.; Ungureanu-Iuga, M.; Cobuz, M. Neonatal and Birth Risk Factors for Type 1 Diabetes Mellitus: Prediction Using an Artificial Neural Network. Life 2025, 15, 1800. https://doi.org/10.3390/life15121800
Cobuz C, Ungureanu-Iuga M, Cobuz M. Neonatal and Birth Risk Factors for Type 1 Diabetes Mellitus: Prediction Using an Artificial Neural Network. Life. 2025; 15(12):1800. https://doi.org/10.3390/life15121800
Chicago/Turabian StyleCobuz, Claudiu, Mădălina Ungureanu-Iuga, and Maricela Cobuz. 2025. "Neonatal and Birth Risk Factors for Type 1 Diabetes Mellitus: Prediction Using an Artificial Neural Network" Life 15, no. 12: 1800. https://doi.org/10.3390/life15121800
APA StyleCobuz, C., Ungureanu-Iuga, M., & Cobuz, M. (2025). Neonatal and Birth Risk Factors for Type 1 Diabetes Mellitus: Prediction Using an Artificial Neural Network. Life, 15(12), 1800. https://doi.org/10.3390/life15121800








