Effectiveness of Mobile Exergaming with Sensor-Based Visual Feedback as an Adjunct Therapy for Home-Based Quadriceps Exercise Training in Knee Osteoarthritis: A Prospective Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
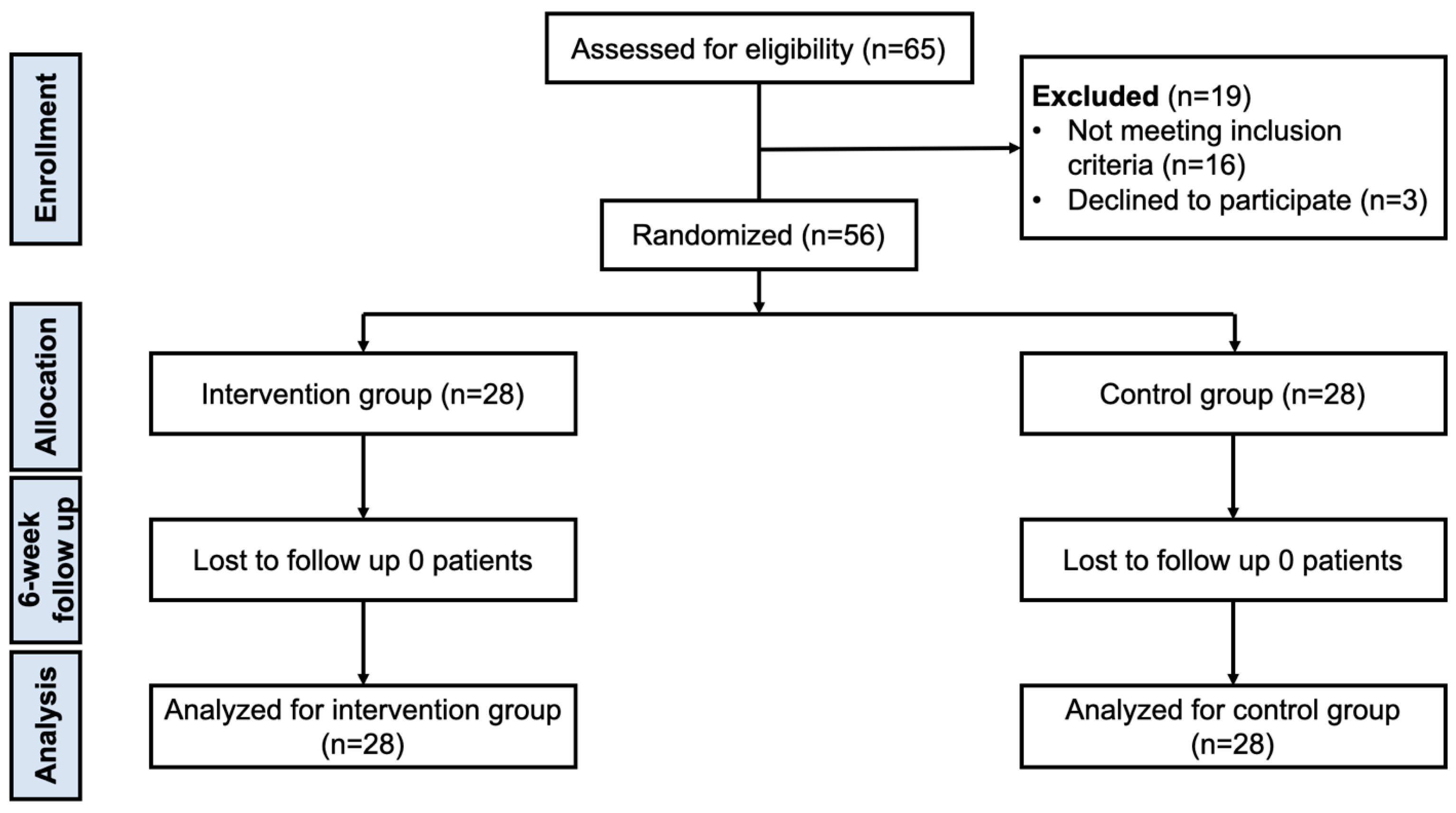
2.1. Study Design, Inclusion, and Exclusion Criteria
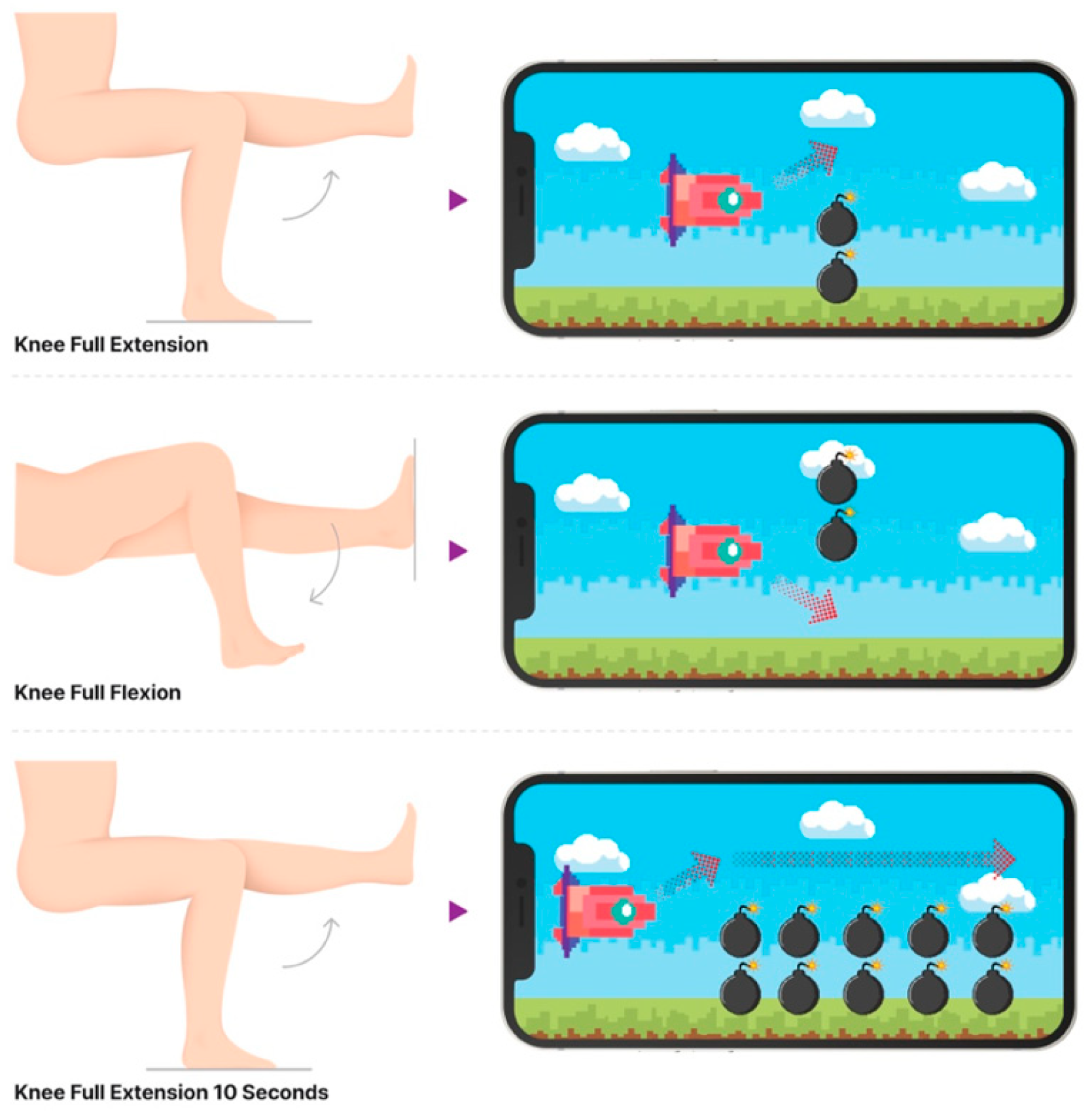
2.2. Information Related to Mobile Exergaming Device and Quadriceps Exercise Protocol
2.3. Data Collection
2.4. Statistical Analysis
2.5. Sample Size Calculation
3. Results
3.1. Patients’ Characteristic Data
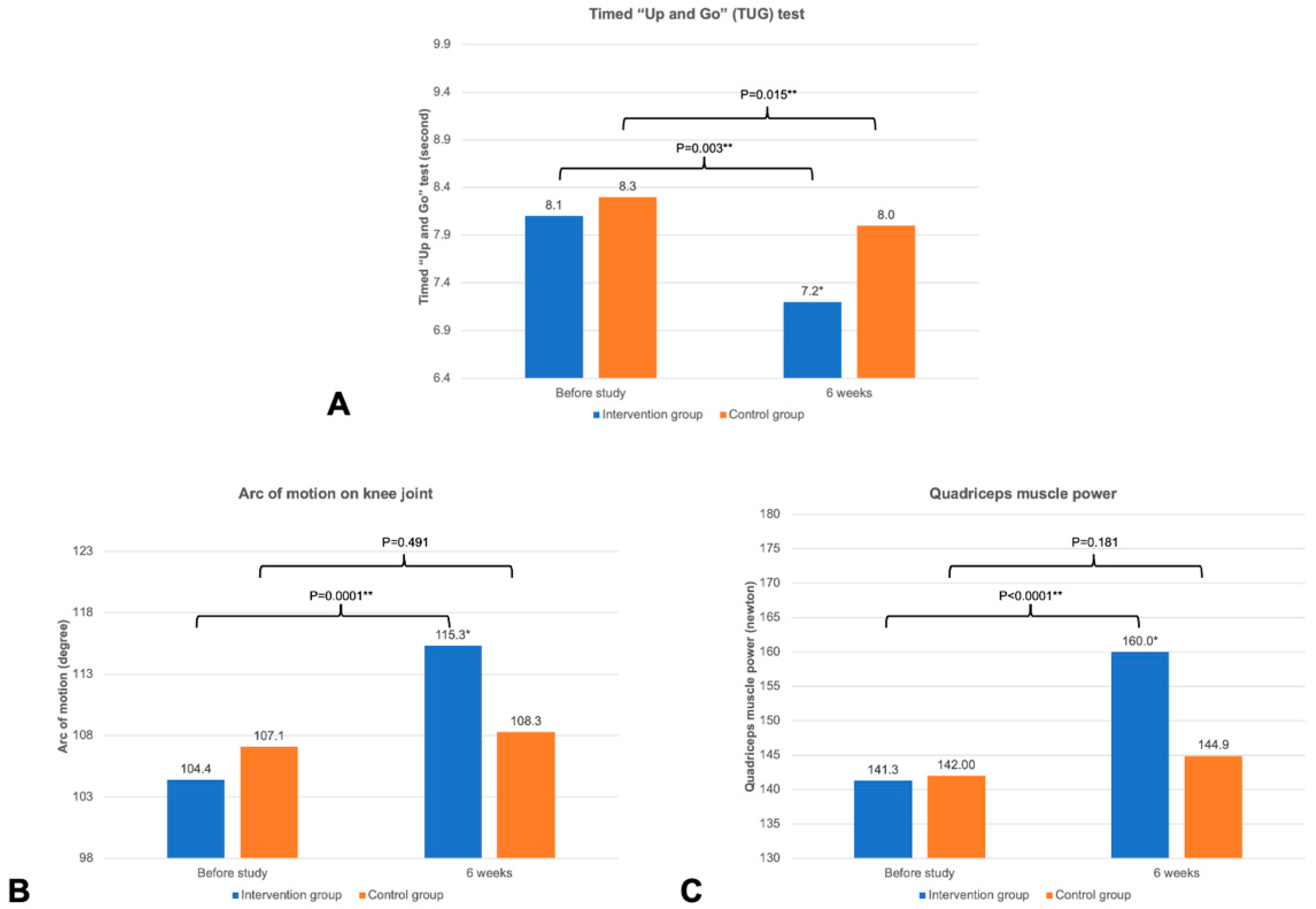
3.2. Outcomes of This Study
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| KOA | Knee osteoarthritis |
| VAS | Visual analog scale score |
| TUG | Timed “Up and Go” |
| KOOS | Knee Injury and Osteoarthritis Outcome Score |
| QSE | Quadriceps strengthening exercise |
| KL | Kellgren and Lawrence |
| HHD | Hand-held dynamometer |
References
- Felson, D.T. Developments in the clinical understanding of osteoarthritis. Arthritis Res. Ther. 2009, 11, 203. [Google Scholar] [CrossRef]
- Maurer, B.T.; Stern, A.G.; Kinossian, B.; Cook, K.D.; Schumacher, H.R., Jr. Osteoarthritis of the knee: Isokinetic quadriceps exercise versus an educational intervention. Arch. Phys. Med. Rehabil. 1999, 80, 1293–1299. [Google Scholar] [CrossRef]
- Brophy, R.H.; Fillingham, Y.A. AAOS clinical practice guideline summary: Management of osteoarthritis of the knee (nonarthroplasty). J. Am. Acad. Orthop. Surg. 2022, 30, e721–e729. [Google Scholar] [CrossRef]
- Aglamis, B.; Toraman, N.F.; Yaman, H. Change of quality of life due to exercise training in knee osteoarthritis: SF-36 and WOMAC. J. Back Musculoskelet. Rehabil. 2009, 22, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.; McConnell, S. Exercise for osteoarthritis of the knee. Cochrane Database Syst. Rev. 2008, 8, CD004376. [Google Scholar]
- Thomas, K.S.; Muir, K.R.; Doherty, M.; Jones, A.C.; O’Reilly, S.C.; Bassey, E.J. Home based exercise programme for knee pain and knee osteoarthritis: Randomised controlled trial. BMJ 2002, 325, 752. [Google Scholar] [CrossRef]
- Zeng, C.Y.; Zhang, Z.R.; Tang, Z.M.; Hua, F.Z. Benefits and Mechanisms of Exercise Training for Knee Osteoarthritis. Front. Physiol. 2021, 12, 794062. [Google Scholar] [CrossRef]
- Marks, R. Knee osteoarthritis and exercise adherence: A review. Curr. Aging Sci. 2012, 5, 72–83. [Google Scholar] [CrossRef]
- Pisters, M.F.; Veenhof, C.; Schellevis, F.G.; Twisk, J.W.; Dekker, J.; De Bakker, D.H. Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res. 2010, 62, 1087–1094. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Lavin-Perez, A.M.; Penacoba, C.; Del Coso, J.; Leyton-Roman, M.; Luque-Casado, A.; Gasque, P.; Fernandez-Del-Olmo, M.A.; Amado-Alonso, D. Key Factors Associated with Adherence to Physical Exercise in Patients with Chronic Diseases and Older Adults: An Umbrella Review. Int. J. Environ. Res. Public Health 2021, 18, 2023. [Google Scholar] [CrossRef] [PubMed]
- Al-Rayes, S.; Al Yaqoub, F.A.; Alfayez, A.; Alsalman, D.; Alanezi, F.; Alyousef, S.; AlNujaidi, H.; Al-Saif, A.K.; Attar, R.; Aljabri, D.; et al. Gaming elements, applications, and challenges of gamification in healthcare. Inform. Med. Unlocked 2022, 31, 100974. [Google Scholar] [CrossRef]
- Manser, P.; de Bruin, E.D.; Temprado, J.J.; Bherer, L.; Herold, F. Beyond “just” fun: The role of exergames in advancing health promotion and disease prevention. Neurosci. Biobehav. Rev. 2025, 176, 106260. [Google Scholar] [CrossRef]
- Lin, Y.T.; Lee, W.C.; Hsieh, R.L. Active video games for knee osteoarthritis improve mobility but not WOMAC score: A randomized controlled trial. Ann. Phys. Rehabil. Med. 2020, 63, 458–465. [Google Scholar] [CrossRef]
- Büyükyilmaz, G.; Menek, B.; Tarakçi, D. Closed Kinetic Chain Exercises Therapy Versus Wii-Based Exergame Therapy in the Treatment of Knee Osteoarthritis: Randomized Controlled Trial. Arch. Health Sci. Res. 2024, 11, 133–139. [Google Scholar] [CrossRef]
- Ardern, C.L.; Kvist, J.; on behalf of the BANG Trial Group; Fältström, A.; Stålman, A.; O’hAlloran, P.; Webster, K.; Taylor, N. BAck iN the Game (BANG)—A smartphone application to help athletes return to sport following anterior cruciate ligament reconstruction: Protocol for a multi-centre, randomised controlled trial. BMC Musculoskel. Disor. 2020, 21, 523. [Google Scholar] [CrossRef]
- Ozlu, A.; Unver, G.; Tuna, H.I.; Menekseoglu, A.K. The Effect of a Virtual Reality-Mediated Gamified Rehabilitation Program on Pain, Disability, Function, and Balance in Knee Osteoarthritis: A Prospective Randomized Controlled Study. Games Health J. 2023, 12, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Rose, M.J.; Costello, K.E.; Eigenbrot, S.; Torabian, K.; Kumar, D. Inertial Measurement Units and Application for Remote Health Care in Hip and Knee Osteoarthritis: Narrative Review. JMIR Rehabil. Assist. Technol. 2022, 9, e33521. [Google Scholar] [CrossRef] [PubMed]
- Riffitts, M.; Cook, H.; McClincy, M.; Bell, K. Evaluation of a Smart Knee Brace for Range of Motion and Velocity Monitoring during Rehabilitation Exercises and an Exergame. Sensors 2022, 22, 9965. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Zhu, B.; Fan, Y.; Wu, M.; Wang, X.; Zhang, H.; Yao, L.; Sun, Y.; Su, B.; Ma, Z. Design and evaluation of an exergame system to assist knee disorders patients’ rehabilitation based on gesture interaction. Health Inf. Sci. Syst. 2022, 10, 20. [Google Scholar] [CrossRef]
- Mete, E.; Sari, Z. The efficacy of exergaming in patients with knee osteoarthritis: A randomized controlled clinical trial. Physioth. Res. Int. 2022, 27, e1952. [Google Scholar] [CrossRef]
- Hopewell, S.; Chan, A.W.; Collins, G.S.; Hrobjartsson, A.; Moher, D.; Schulz, K.F.; Tunn, R.; Aggarwal, R.; Berkwits, M.; Berlin, J.A.; et al. CONSORT 2025 statement: Updated guideline for reporting randomized trials. Nat. Med. 2025, 31, 1776–1783. [Google Scholar] [CrossRef]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res. 2020, 72, 149–162. [Google Scholar] [CrossRef]
- Webster, K.E.; Klemm, H.J.; Whitehead, T.S.; Norsworthy, C.J.; Feller, J.A. Responsiveness of the Various Short-Form Versions of the Knee Injury and Osteoarthritis Outcome Score Between 2 and 5 Years After Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2024, 12, 23259671241236513. [Google Scholar] [CrossRef]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef]
- Schlenk, E.A.; Fitzgerald, G.K.; Rogers, J.C.; Kwoh, C.K.; Sereika, S.M. Promoting Physical Activity in Older Adults With Knee Osteoarthritis and Hypertension: A Randomized Controlled Trial. J. Aging Phys. Act. 2021, 29, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Vincent, K.R.; Vasilopoulos, T.; Montero, C.; Vincent, H.K. Eccentric and Concentric Resistance Exercise Comparison for Knee Osteoarthritis. Med. Sci. Sports Exerc. 2019, 51, 1977–1986. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.J.; Prinsen, C.A.; Christensen, R.; Bartels, E.M.; Terwee, C.B.; Roos, E.M. Knee Injury and Osteoarthritis Outcome Score (KOOS): Systematic review and meta-analysis of measurement properties. Osteoarthr. Cartil. 2016, 24, 1317–1329. [Google Scholar] [CrossRef]
- Gagnon, D.; Nadeau, S.; Gravel, D.; Robert, J.; Belanger, D.; Hilsenrath, M. Reliability and validity of static knee strength measurements obtained with a chair-fixed dynamometer in subjects with hip or knee arthroplasty. Arch. Phys. Med. Rehabil. 2005, 86, 1998–2008. [Google Scholar] [CrossRef] [PubMed]
- Guede-Rojas, F.; Mendoza, C.; Rodriguez-Lagos, L.; Soto-Martinez, A.; Ulloa-Diaz, D.; Jorquera-Aguilera, C.; Carvajal-Parodi, C. Effects of Non-Immersive Virtual Reality Exercise on Self-Reported Pain and Mechanical Hyperalgesia in Older Adults with Knee and Hip Osteoarthritis: A Secondary Analysis of a Randomized Controlled Trial. Medicina 2025, 61, 1122. [Google Scholar] [CrossRef]
- Gay, C.; Chabaud, A.; Guilley, E.; Coudeyre, E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Ann. Phys. Rehabil. Med. 2016, 59, 174–183. [Google Scholar] [CrossRef]
- Doi, T.; Akai, M.; Fujino, K.; Iwaya, T.; Kurosawa, H.; Hayashi, K.; Marui, E. Effect of home exercise of quadriceps on knee osteoarthritis compared with nonsteroidal antiinflammatory drugs: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2008, 87, 258–269. [Google Scholar] [CrossRef]
- Imoto, A.M.; Peccin, M.S.; Trevisani, V.F. Quadriceps strengthening exercises are effective in improving pain, function and quality of life in patients with osteoarthritis of the knee. Acta Ortopédica Bras. 2012, 20, 174–179. [Google Scholar] [CrossRef]
- Carvajal-Parodi, C.; Mendoza, C.; Alvarez, C.; Soto-Martínez, A.; Ulloa-Díaz, D.; Jorquera-Aguilera, C.; Guede-Rojas, F. Effectiveness of Exergames on Functional Physical Performance in Older Adults with Knee/Hip Osteoarthritis: A Randomized Controlled Trial. J. Clin. Med. 2025, 14, 2968. [Google Scholar] [CrossRef]
- Ishida, T.; Samukawa, M. Validity and Reliability of a Wearable Goniometer Sensor Controlled by a Mobile Application for Measuring Knee Flexion/Extension Angle during the Gait Cycle. Sensors 2023, 23, 3266. [Google Scholar] [CrossRef]
- Plavoukou, T.; Apostolakopoulou, K.; Papagiannis, G.; Stasinopoulos, D.; Georgoudis, G. Impact of Virtual Reality, Augmented Reality, and Sensor Technology in Knee Osteoarthritis Rehabilitation: A Systematic Review. Cureus 2025, 17, e79011. [Google Scholar] [CrossRef] [PubMed]
- Argent, R.; Daly, A.; Caulfield, B. Patient Involvement with Home-Based Exercise Programs: Can Connected Health Interventions Influence Adherence? JMIR Mhealth Uhealth 2018, 6, e47. [Google Scholar] [CrossRef]
- Schroeder, T.; Dodds, L.; Georgiou, A.; Gewald, H.; Siette, J. Older Adults and New Technology: Mapping Review of the Factors Associated with Older Adults’ Intention to Adopt Digital Technologies. JMIR Aging 2023, 6, e44564. [Google Scholar] [CrossRef] [PubMed]
- Franco, T.; Sestrem, L.; Henriques, P.R.; Alves, P.; Varanda Pereira, M.J.; Brandao, D.; Leitao, P.; Silva, A. Motion Sensors for Knee Angle Recognition in Muscle Rehabilitation Solutions. Sensors 2022, 22, 7605. [Google Scholar] [CrossRef] [PubMed]



| Intervention Group (n = 28) | Control Group (n = 28) | p-Value | |
|---|---|---|---|
| Age, year a | 59.9 (5.8) | 62.1 (5.6) | 0.158 |
| Male–female b | 5:23 | 6:22 | 1.000 |
| BMI, kg/m2 a | 26.1 (3.2) | 27.1 (3.6) | 0.268 |
| Extension, degree a | 10.9 (6.2) | 9.0 (4.5) | 0.205 |
| Flexion, degree a | 115.6 (12.2) | 116.4 (10.1) | 0.803 |
| Arc of motion, degree a | 104.8 (15.6) | 107.4 (10.2) | 0.463 |
| Quadriceps muscle power, N a | 141.3 (23.2) | 142.0 (19.2) | 0.911 |
| VAS score at rest c | 2 (0–6) | 2 (0–5) | 0.620 |
| VAS score on motion a | 5.5 (2.0) | 6.5 (2.4) | 0.125 |
| TUG test, second a | 8.1 (1.5) | 8.3 (2.6) | 0.753 |
| KOOS a | |||
| Symptoms | 68.1 (21.0) | 70.4 (16.4) | 0.652 |
| Pain | 68.2 (17.3) | 68.9 (19.9) | 0.887 |
| ADL | 69.9 (16.9) | 71.1 (18.0) | 0.790 |
| Sports activity | 40.5 (21.5) | 44.3 (24.0) | 0.541 |
| Quality of life | 41.0 (20.0) | 50.5 (19.4) | 0.081 |
| Total score | 63.0 (16.9) | 65.4 (17.2) | 0.604 |
| Intervention Group (n = 28) | Control Group (n = 28) | p-Value | |
|---|---|---|---|
| Extension, degree a | 7.8 (5.7) | 5.6 (3.6) | 0.94 |
| Flexion, degree a | 123.1 (8.4) | 114.4 (8.0) | 0.0002 * |
| Arc of motion, degree a | 115.3 (10.6) | 108.8 (7.9) | 0.011 * |
| Quadriceps muscle power, N a | 160.0 (24.1) | 144.9 (15.6) | 0.007 * |
| VAS score at rest b | 1 (0–5) | 2 (0–5) | 0.025 * |
| VAS score on motion a | 3.6 (2.1) | 5.9 (2.2) | 0.0002 * |
| TUG test, second a | 7.2 (1.4) | 8.0 (2.3) | 0.145 |
| KOOS a | |||
| Symptoms | 83.8 (10.4) | 67.0 (17.4) | <0.0001 * |
| Pain | 75.8 (21.0) | 71.2 (17.8) | 0.379 |
| ADL | 79.9 (15.5) | 79.7 (13.6) | 0.964 |
| Sports activity | 57.3 (27.8) | 53.4 (20.6) | 0.551 |
| Quality of life | 59.4 (28.6) | 51.7 (25.5) | 0.290 |
| Total score | 75.0 (16.5) | 69.9 (14.4) | 0.227 |
| Satisfaction score a | 4.6 (0.5) | 3.4 (0.6) | <0.0001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarungvittayakon, C.; Sa-ngasoongsong, P.; Chockchaisakul, D.; Bamrungchaowkasem, J.; Wongsak, S. Effectiveness of Mobile Exergaming with Sensor-Based Visual Feedback as an Adjunct Therapy for Home-Based Quadriceps Exercise Training in Knee Osteoarthritis: A Prospective Randomized Controlled Trial. Life 2025, 15, 1738. https://doi.org/10.3390/life15111738
Jarungvittayakon C, Sa-ngasoongsong P, Chockchaisakul D, Bamrungchaowkasem J, Wongsak S. Effectiveness of Mobile Exergaming with Sensor-Based Visual Feedback as an Adjunct Therapy for Home-Based Quadriceps Exercise Training in Knee Osteoarthritis: A Prospective Randomized Controlled Trial. Life. 2025; 15(11):1738. https://doi.org/10.3390/life15111738
Chicago/Turabian StyleJarungvittayakon, Chavarat, Paphon Sa-ngasoongsong, Danai Chockchaisakul, Jaturong Bamrungchaowkasem, and Siwadol Wongsak. 2025. "Effectiveness of Mobile Exergaming with Sensor-Based Visual Feedback as an Adjunct Therapy for Home-Based Quadriceps Exercise Training in Knee Osteoarthritis: A Prospective Randomized Controlled Trial" Life 15, no. 11: 1738. https://doi.org/10.3390/life15111738
APA StyleJarungvittayakon, C., Sa-ngasoongsong, P., Chockchaisakul, D., Bamrungchaowkasem, J., & Wongsak, S. (2025). Effectiveness of Mobile Exergaming with Sensor-Based Visual Feedback as an Adjunct Therapy for Home-Based Quadriceps Exercise Training in Knee Osteoarthritis: A Prospective Randomized Controlled Trial. Life, 15(11), 1738. https://doi.org/10.3390/life15111738






