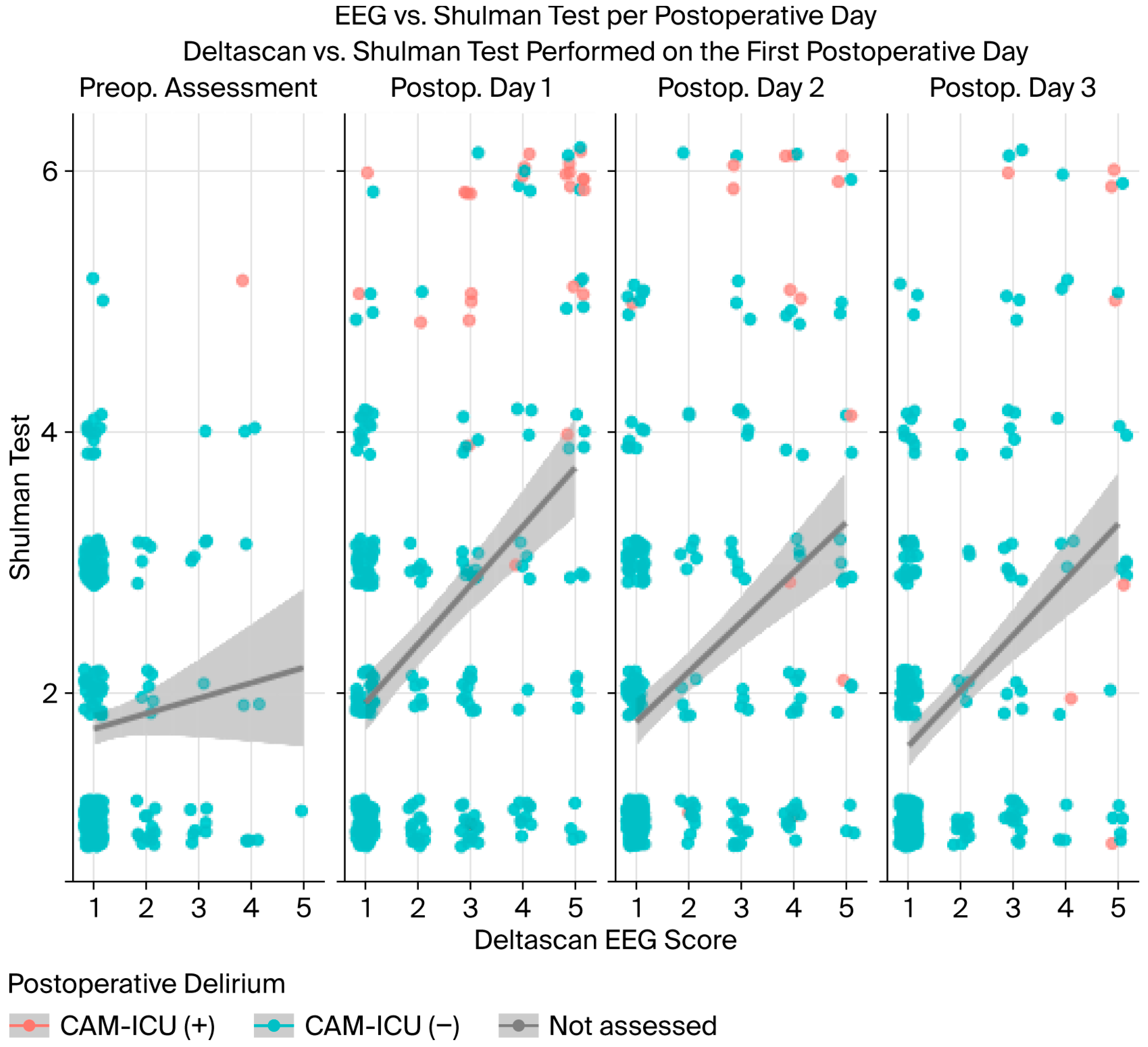
Comparison of DeltaScan® and CAM-ICU for the Assessment of Postoperative Delirium in Patients Undergoing Cardiac Surgery and Cardiac Interventions: A Prospective Observational Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CAM-ICU | Confusion Assessment Method for Intermediate Care Medicine |
| DSM-5 | Diagnostic and Statistical Manual of Mental Disorders |
| DRS-R-98 | Delirium Rating Scale Revised 1998 Edition |
| EEG | Electroencephalography |
| fMRI | Functional Magnetic Resonance Imaging |
| POD-QV | Postopeatives Delirium-Qualitätsvertrag |
| G-BA | Gemeinsamer Bundesausschuss |
| IQTIG | Institut für Qualität und Transparenz im Gesundheitswesenelectroencephalography |
| DRKS | Deutsches Register Klinischer Studien |
References
- Wilson, J.E.; Mart, M.; Cunningham, C.; Shehabi, Y.; Girard, T.D.; MacLullich, A.M.J.; Slooter, A.J.C.; Ely, E.W. Delirium. Nat. Rev. Dis. Primers 2020, 6, 90. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, S.; Bode, L.; Ernst, J.; Marquetand, J.; Von Känel, R.; Böttger, S. Delirium in Elderly Patients: Prospective Prevalence across Hospital Services. Gen. Hosp. Psychiatry 2020, 67, 19–25. [Google Scholar] [CrossRef]
- Urban, M.K.; Sasaki, M.; Schmucker, A.M.; Magid, S.K. Postoperative Delirium after Major Orthopedic Surgery. World J. Orthop. 2020, 11, 90–106. [Google Scholar] [CrossRef]
- Marcantonio, E.R. Delirium in Hospitalized Older Adults. N. Engl. J. Med. 2017, 377, 1456–1466. [Google Scholar] [CrossRef]
- Ely, E.W.; Shintani, A.; Truman, B.; Speroff, T.; Gordon, S.M.; Harrell, F.E.; Inouye, S.K.; Bernard, G.R.; Dittus, R.S. Delirium as a Predictor of Mortality in Mechanically Ventilated Patients in the Intensive Care Unit. JAMA 2004, 291, 1753–1762. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Cook, D.; Devlin, J.W.; Skrobik, Y.; Meade, M.; Fergusson, D.; Herridge, M.; Steinberg, M.; Granton, J.; Ferguson, N.; et al. Prevalence, Risk Factors, and Outcomes of Delirium in Mechanically Ventilated Adults. Crit. Care Med. 2015, 43, 557. [Google Scholar] [CrossRef]
- De La Varga-Martínez, O.; Gutiérrez-Bustillo, R.; Muñoz-Moreno, M.F.; López-Herrero, R.; Gómez-Sánchez, E.; Tamayo, E. Postoperative Delirium: An Independent Risk Factor for Poorer Quality of Life with Long-Term Cognitive and Functional Decline after Cardiac Surgery. J. Clin. Anesth. 2023, 85, 111030. [Google Scholar] [CrossRef]
- Gleason, L.J.; Schmitt, E.M.; Kosar, C.M.; Tabloski, P.; Saczynski, J.S.; Robinson, T.; Cooper, Z.; Rogers, S.O.; Jones, R.N.; Marcantonio, E.R.; et al. Effect of Delirium and Other Major Complications After Elective Surgery in Older Adults. JAMA Surg. 2015, 150, 1134–1140. [Google Scholar] [CrossRef]
- Zywiel, M.G.; Hurley, R.T.; Perruccio, A.V.; Hancock-Howard, R.L.; Coyte, P.C.; Rampersaud, Y.R. Health Economic Implications of Perioperative Delirium in Older Patients After Surgery for a Fragility Hip Fracture. J. Bone Jt. Surg. 2015, 97, 829–836. [Google Scholar] [CrossRef]
- Van Lieshout, C.; Schuit, E.; Hermes, C.; Kerrigan, M.; Frederix, G.W.J. Hospitalisation Costs and Health Related Quality of Life in Delirious Patients: A Scoping Review. Z. Evidenz Fortbild. Qual. Gesundheitswes. 2022, 169, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Ely, E.W.; Margolin, R.; Francis, J.; May, L.; Truman, B.; Dittus, R.; Speroff, T.; Gautam, S.; Bernard, G.R.; Inouye, S.K. Evaluation of Delirium in Critically Ill Patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit. Care Med. 2001, 29, 1370. [Google Scholar] [CrossRef] [PubMed]
- Gusmao-Flores, D.; Salluh, J.I.F.; Chalhub, R.Á.; Quarantini, L.C. The Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) and Intensive Care Delirium Screening Checklist (ICDSC) for the Diagnosis of Delirium: A Systematic Review and Meta-Analysis of Clinical Studies. Crit. Care 2012, 16, R115. [Google Scholar] [CrossRef]
- Guenther, U.; Wolke, M.; Hansen, H.-C.; Feldmann, N.; Diers, A.; Dewald, O.; Ely, E.W.; Weyland, A. Bedeutung Der Desorientierung Bei Der Delireinschätzung. Med. Klin. Intensivmed. Notfmed 2022, 117, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Numan, T.; van den Boogaard, M.; Kamper, A.M.; Rood, P.J.T.; Peelen, L.M.; Slooter, A.J.C.; the Dutch Delirium Detection Study Group. Recognition of Delirium in Postoperative Elderly Patients: A Multicenter Study. J. Am. Geriatr. Soc. 2017, 65, 1932–1938. [Google Scholar] [CrossRef]
- Khan, B.A.; Perkins, A.J.; Prasad, N.K.; Shekhar, A.; Campbell, N.L.; Gao, S.; Wang, S.; Khan, S.H.; Marcantonio, E.R.; Twigg, H.L.; et al. Biomarkers of Delirium Duration and Delirium Severity in the ICU. Crit. Care Med. 2020, 48, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.H.; Lindroth, H.; Jawed, Y.; Wang, S.; Nasser, J.; Seyffert, S.; Naqvi, K.; Perkins, A.J.; Gao, S.; Kesler, K.; et al. Serum Biomarkers in Postoperative Delirium after Esophagectomy. Ann. Thorac. Surg. 2022, 113, 1000–1007. [Google Scholar] [CrossRef]
- Hochleitner, M.; Pickert, L.; Nolting, N.A.; Affeldt, A.M.; Becker, I.; Benzing, T.; Kochanek, M.; Polidori, M.C. Patient- vs. Organ-Based Prognostic Tools for Older Patients in Critical Care Units: An Observational Study with a 3-Month Follow-Up. Med. Klin.-Intensivmed. Notfallmedizin 2024, 120, 322–328. [Google Scholar] [CrossRef]
- Ditzel, F.L.; Hut, S.C.; Dijkstra-Kersten, S.M.; Numan, T.; Leijten, F.S.; van den Boogaard, M.; Slooter, A.J. An Automated Electroencephalography Algorithm to Detect Polymorphic Delta Activity in Acute Encephalopathy Presenting as Postoperative Delirium. Psychiatry Clin. Neurosci. 2022, 76, 676–678. [Google Scholar] [CrossRef]
- Van Der Kooi, A.W.; Zaal, I.J.; Klijn, F.A.; Koek, H.L.; Meijer, R.C.; Leijten, F.S.; Slooter, A.J. Delirium Detection Using EEG. Chest 2015, 147, 94–101. [Google Scholar] [CrossRef]
- Numan, T.; Van Den Boogaard, M.; Kamper, A.M.; Rood, P.J.T.; Peelen, L.M.; Slooter, A.J.C.; Abawi, M.; Van Den Boogaard, M.; Claassen, J.A.; Coesmans, M.; et al. Delirium Detection Using Relative Delta Power Based on 1-Minute Single-Channel EEG: A Multicentre Study. Br. J. Anaesth. 2019, 122, 60–68. [Google Scholar] [CrossRef]
- van der A, J.; Ottens, T.H.; Lodema, D.Y.; de Haan, W.; Tendolkar, I.; Emmelot-Vonk, M.H.; Schutter, D.J.L.G.; van Dellen, E.; Slooter, A.J.C. Electroencephalography and connectivity in delirium. Tijdschr. Psychiatr. 2023, 65, 633–636. [Google Scholar]
- Ditzel, F.L.; Van Montfort, S.J.T.; Vernooij, L.M.; Kant, I.M.J.; Aarts, E.; Spies, C.D.; Hendrikse, J.; Slooter, A.J.C.; Van Dellen, E. Functional Brain Network and Trail Making Test Changes Following Major Surgery and Postoperative Delirium: A Prospective, Multicentre, Observational Cohort Study. Br. J. Anaesth. 2023, 130, e281–e288. [Google Scholar] [CrossRef]
- Prolira DeltaScan Handbücher. Available online: https://www.manualslib.de/products/Prolira-Deltascan-1755541.html (accessed on 6 February 2025).
- Adamis, D.; Meagher, D.; O’Neill, D.; McCarthy, G. The Utility of the Clock Drawing Test in Detection of Delirium in Elderly Hospitalised Patients. Aging Ment. Health 2016, 20, 981–986. [Google Scholar] [CrossRef]
- Fliegenschmidt, J.; Middeke, C.; Ruggeri, S.; Bunge, C.; Schütte, E.; Hulde, N.; von Dossow, V. Delirprävention im Co-Management mit Qualitätsvertrag: Die OP-Paten. Eine narrative Zusammenfassung einer Co-Management-Strategie in der Prävention des postoperativen Delirs in der Herzchirurgie als Umsetzung eines Qualitätsvertrages. Anaesthesiol. Intensivmed. 2024, 65, 389–394. [Google Scholar] [CrossRef]
- Boettger, S.; Nuñez, D.G.; Meyer, R.; Richter, A.; Fernandez, S.F.; Rudiger, A.; Schubert, M.; Jenewein, J. Delirium in the Intensive Care Setting: A Reevaluation of the Validity of the CAM–ICU and ICDSC versus the DSM–IV–TR in Determining a Diagnosis of Delirium as Part of the Daily Clinical Routine. Palliat. Support. Care 2017, 15, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying Confusion: The Confusion Assessment Method. Ann. Intern. Med. 1990, 113, 941–948. [Google Scholar] [CrossRef]
- Shulman, K.I.; Pushkar Gold, D.; Cohen, C.A.; Zucchero, C.A. Clock-Drawing and Dementia in the Community: A Longitudinal Study. Int. J. Geriatr. Psychiatry 1993, 8, 487–496. [Google Scholar] [CrossRef]
- Shulman, K.I. Clock-Drawing: Is It the Ideal Cognitive Screening Test? Int. J. Geriatr. Psychiatry 2000, 15, 548–561. [Google Scholar] [CrossRef]
- Shulman, K.I.; Shedletsky, R.; Silver, I.L. The Challenge of Time: Clock-Drawing and Cognitive Function in the Elderly. Int. J. Geriatr. Psychiatry 1986, 1, 135–140. [Google Scholar] [CrossRef]
- Home—DeltaScan® Brain State Monitor. Available online: https://hollandcapital.nl/en/project/prolira/ (accessed on 6 February 2025).
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2021. [Google Scholar]
- Wickham, H. Ggplot2; Use R! Springer International Publishing: Cham, Switzerland, 2016; ISBN 978-3-319-24275-0. [Google Scholar]
- Aben, J.; Pouwels, S.; Oldenbeuving, A. Comparison Between Deltascan Single Channel Electroencephalography (EEG), Confusion Assessment Method-Intensive Care Unit (CAM-ICU) Score and Clinical Assessment in Diagnosing Delirium in Intubated Patients in the Intensive Care Unit. Cureus 2022, 14, e26449. [Google Scholar] [CrossRef] [PubMed]
- Hut, S.C.A.; Dijkstra-Kersten, S.M.A.; Numan, T.; Henriquez, N.R.V.R.; Teunissen, N.W.; van den Boogaard, M.; Leijten, F.S.; Slooter, A.J.C. EEG and Clinical Assessment in Delirium and Acute Encephalopathy. Psychiatry Clin. Neurosci. 2021, 75, 265–266. [Google Scholar] [CrossRef]
- de Fraiture, E.J.; Schuijt, H.J.; Menninga, M.; Koevoets, I.A.I.; Verheul, T.F.M.; van Goor, C.W.; Nijdam, T.M.P.; van Dartel, D.; Hegeman, J.H.; van der Velde, D. Automated EEG-Based Brainwave Analysis for the Detection of Postoperative Delirium Does Not Result in a Shorter Length of Stay in Geriatric Hip Fracture Patients: A Multicentre Randomized Controlled Trial. J. Clin. Med. 2024, 13, 6987. [Google Scholar] [CrossRef] [PubMed]
- Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Audisio, R.; Borozdina, A.; Cherubini, A.; Jones, C.; Kehlet, H.; MacLullich, A.; et al. European Society of Anaesthesiology Evidence-Based and Consensus-Based Guideline on Postoperative Delirium. Eur. J. Anaesthesiol. 2017, 34, 192–214. [Google Scholar] [CrossRef] [PubMed]
- AWMF Leitlinienregister. Available online: https://register.awmf.org/de/leitlinien/detail/001-012 (accessed on 25 September 2025).
- Jones, R.N.; Cizginer, S.; Pavlech, L.; Albuquerque, A.; Daiello, L.A.; Dharmarajan, K.; Gleason, L.J.; Helfand, B.; Massimo, L.; Oh, E.; et al. Assessment of Instruments for Measurement of Delirium Severity: A Systematic Review. JAMA Intern. Med. 2019, 179, 231. [Google Scholar] [CrossRef] [PubMed]


| Variable | Overall N = 335 | POD − N = 285 | POD + N = 50 |
|---|---|---|---|
| Age | 77 (7) | 77 (7) | 78 (6) |
| Sex | |||
| M | 179/335 (53%) | 154/285 (54%) | 25/50 (50%) |
| F | 156/335 (47%) | 131/285 (46%) | 25/50 (50%) |
| Intervention | |||
| Surg | 183/335 (55%) | 141/285 (49%) | 42/50 (84%) |
| Cath | 152/335 (45%) | 144/285 (51%) | 8/50 (16%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bergmann, A.; Fliegenschmidt, J.; Ruggeri, S.; Hulde, N.; Middeke, C.; Bunge, C.; Preising, M.; Hermes, C.; von Dossow, V. Comparison of DeltaScan® and CAM-ICU for the Assessment of Postoperative Delirium in Patients Undergoing Cardiac Surgery and Cardiac Interventions: A Prospective Observational Pilot Study. Life 2025, 15, 1640. https://doi.org/10.3390/life15101640
Bergmann A, Fliegenschmidt J, Ruggeri S, Hulde N, Middeke C, Bunge C, Preising M, Hermes C, von Dossow V. Comparison of DeltaScan® and CAM-ICU for the Assessment of Postoperative Delirium in Patients Undergoing Cardiac Surgery and Cardiac Interventions: A Prospective Observational Pilot Study. Life. 2025; 15(10):1640. https://doi.org/10.3390/life15101640
Chicago/Turabian StyleBergmann, Astrid, Janis Fliegenschmidt, Silvia Ruggeri, Nikolai Hulde, Catharina Middeke, Claudia Bunge, Maria Preising, Carsten Hermes, and Vera von Dossow. 2025. "Comparison of DeltaScan® and CAM-ICU for the Assessment of Postoperative Delirium in Patients Undergoing Cardiac Surgery and Cardiac Interventions: A Prospective Observational Pilot Study" Life 15, no. 10: 1640. https://doi.org/10.3390/life15101640
APA StyleBergmann, A., Fliegenschmidt, J., Ruggeri, S., Hulde, N., Middeke, C., Bunge, C., Preising, M., Hermes, C., & von Dossow, V. (2025). Comparison of DeltaScan® and CAM-ICU for the Assessment of Postoperative Delirium in Patients Undergoing Cardiac Surgery and Cardiac Interventions: A Prospective Observational Pilot Study. Life, 15(10), 1640. https://doi.org/10.3390/life15101640





