Comparative Effects of Adapted Taekwondo Versus Tai Chi on Health Status in Independent Older Women: A Randomized Controlled Trial
Abstract
1. Introduction
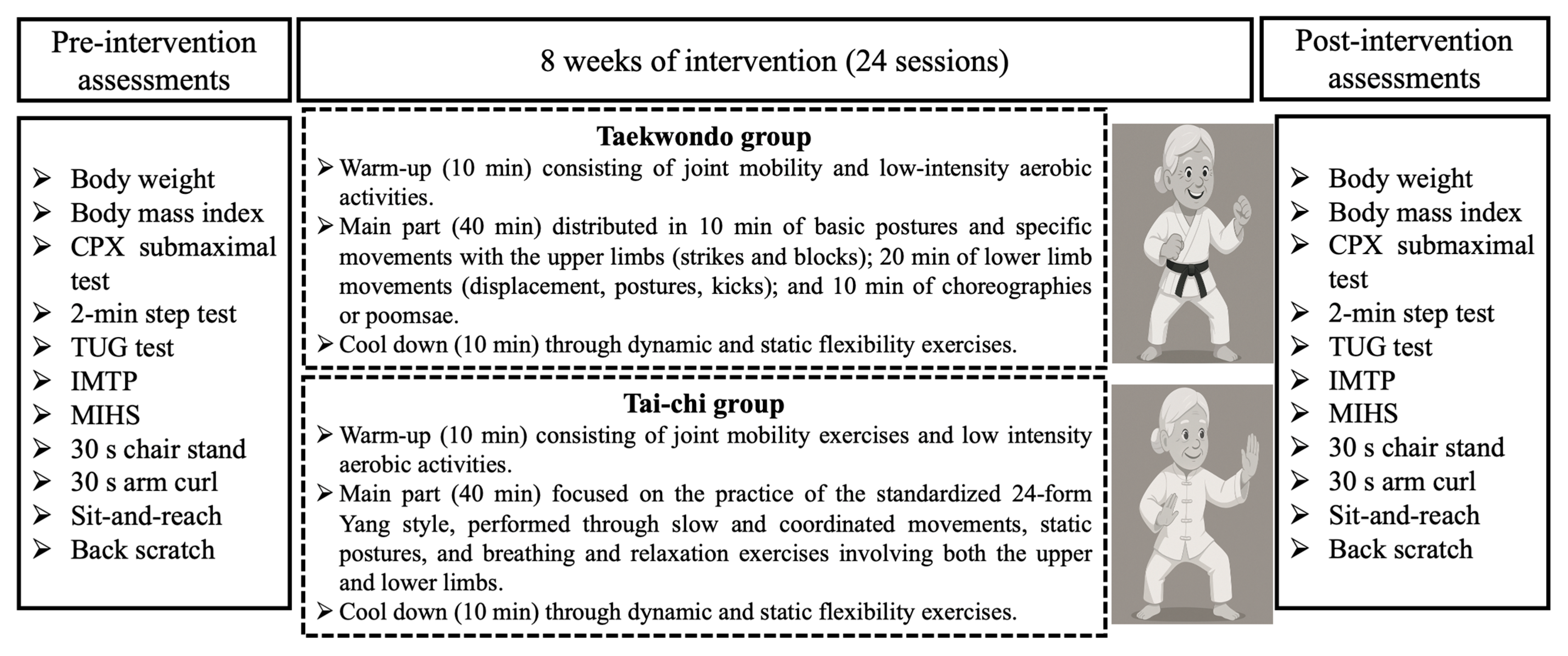
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Measurements
2.3.1. Anthropometric Variables
2.3.2. Cardiorespiratory Fitness
2.3.3. Balance Performance
2.3.4. Muscle Strength Performance
2.3.5. Flexibility Performance
2.4. Interventions
2.5. Statistical Analysis
3. Results
3.1. Anthropometric Variables
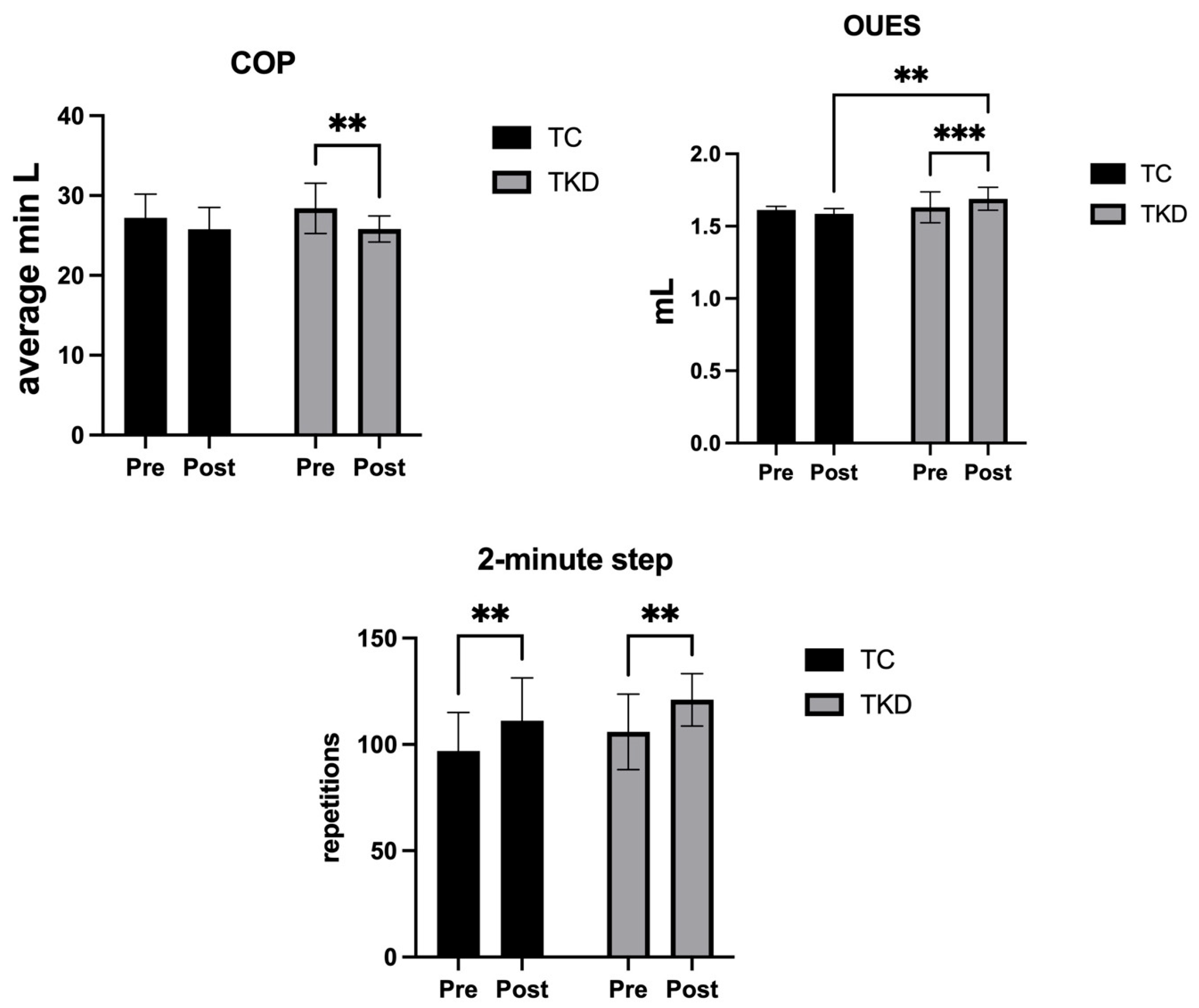
3.2. Cardiorespiratory Fitness
3.3. Balance Performance
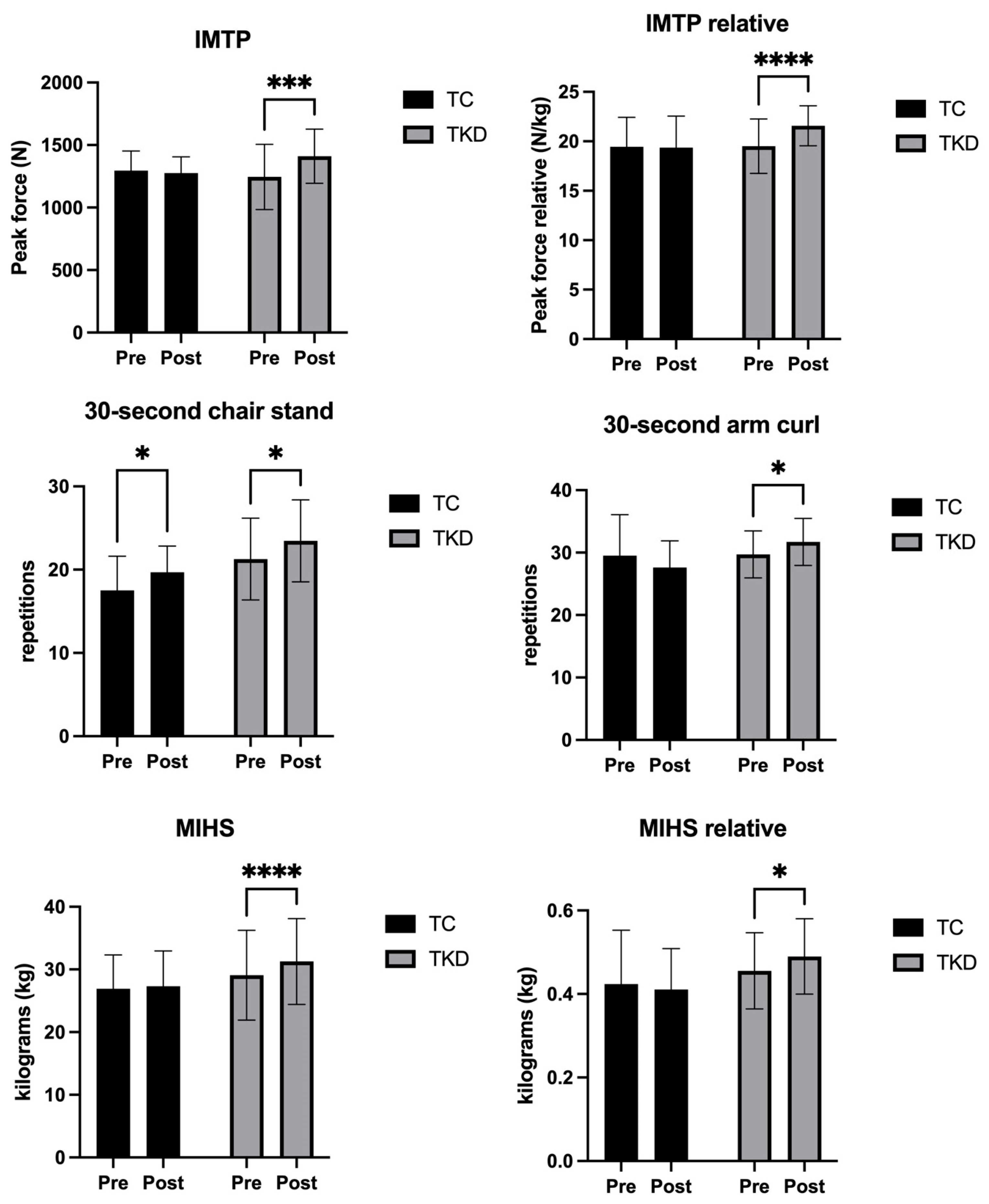
3.4. Muscle Strength Performance
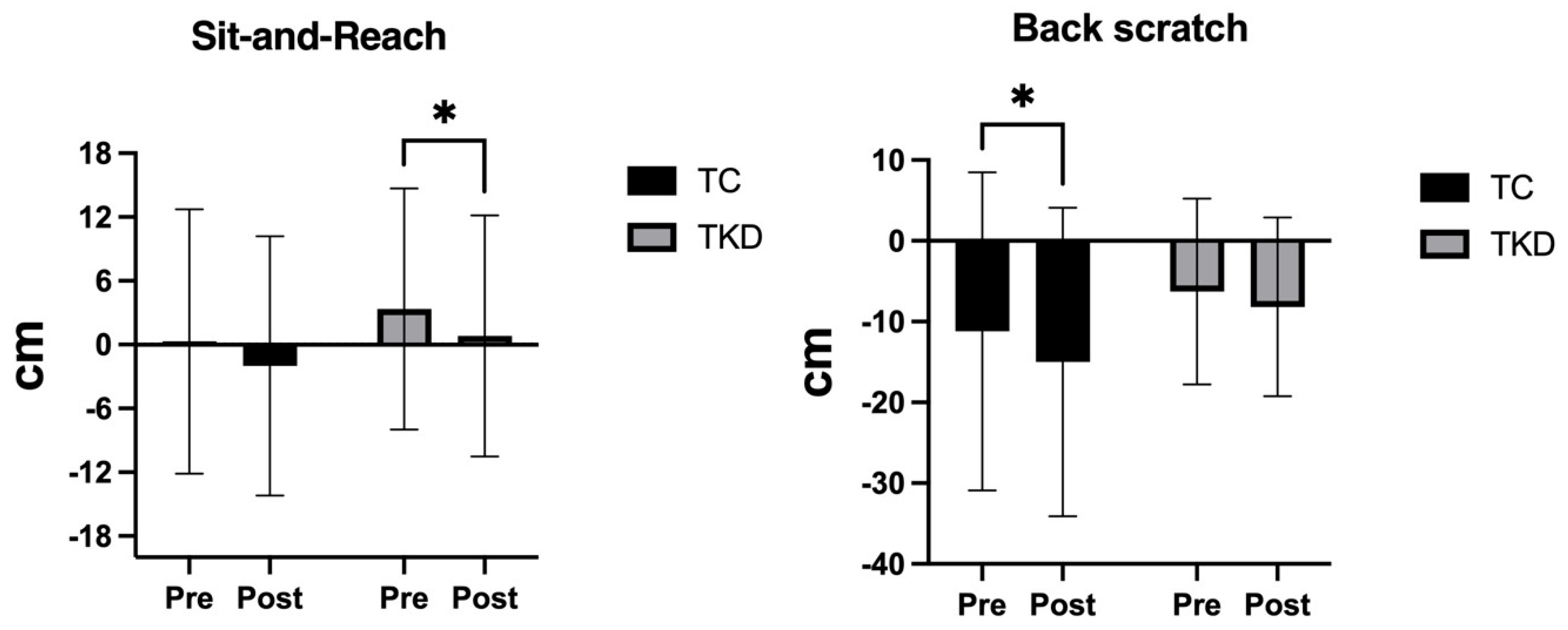
3.5. Flexibility Performance
4. Discussion
4.1. Anthropometric Variables
4.2. Cardiorespiratory Fitness
4.3. Balance Performance
4.4. Muscle Strength Performance
4.5. Flexibility Performance
4.6. Strengths and Limitations of the Study
4.7. Practical Applications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gutiérrez, P.; Carla, M.; Ortega, F. Políticas Públicas Del Cuidado Dirigidas a Personas Con Discapacidad y Dependencia En Chile. In Proceedings of the XXI Congreso Internacional del CLAD sobre la Reforma del Estado y de la Administración Pública, Santiago, Chile, 8–11 November 2016. [Google Scholar]
- Reis Júnior, W.M.; Ferreira, L.N.; Molina-Bastos, C.G.; Bispo Júnior, J.P.; Reis, H.F.T.; Goulart, B.N.G. Prevalence of Functional Dependence and Chronic Diseases in the Community-Dwelling Brazilian Older Adults: An Analysis by Dependence Severity and Multimorbidity Pattern. BMC Public Health 2024, 24, 140. [Google Scholar] [CrossRef]
- Meucci, R.D.; de Oliveira, A.S.L.A.; Araújo, G.C.; Gonzalez, T.N.; Pagliaro, G.; Hoffmann, T.; Marmitt, L.P. Functional Dependence among Adults: A Cross-Sectional Study with a Rural Population of Southern Brazil. Rural Remote Health 2020, 20, 5985. [Google Scholar] [CrossRef] [PubMed]
- Gomes, M.; Figueiredo, D.; Teixeira, L.; Poveda, V.; Paúl, C.; Santos-Silva, A.; Costa, E. Physical Inactivity among Older Adults across Europe Based on the SHARE Database. Age Ageing 2017, 46, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Martinez, J.; González-Castillo, C.; Herrera-Valenzuela, T.; Muñoz-Vásquez, C.; Magnani Branco, B.H.; Valdés-Badilla, P. Association between Physical Activity Habits with Cardiometabolic Variables, Body Composition, and Physical Performance in Chilean Older Women. Int. J. Environ. Res. Public Health 2023, 20, 6688. [Google Scholar] [CrossRef]
- Schlenk, E.A.; Fitzgerald, G.K.; Rogers, J.C.; Kwoh, C.K.; Sereika, S.M. Promoting Physical Activity in Older Adults with Knee Osteoarthritis and Hypertension: A Randomized Controlled Trial. J. Aging Phys. Act. 2021, 29, 207–218. [Google Scholar] [CrossRef]
- Miri, S.; Farhadi, B.; Takasi, P.; Ghorbani Vajargah, P.; Karkhah, S. Physical Independence and Related Factors among Older Adults: A Systematic Review and Meta-Analysis. Ann. Med. Surg. 2024, 86, 3400–3408. [Google Scholar] [CrossRef]
- Länsitie, M.; Kangas, M.; Jokelainen, J.; Venojärvi, M.; Timonen, M.; Keinänen-Kiukaanniemi, S.; Korpelainen, R. Cardiovascular Disease Risk and All-Cause Mortality Associated with Accelerometer-Measured Physical Activity and Sedentary Time—A Prospective Population-Based Study in Older Adults. BMC Geriatr. 2022, 22, 729. [Google Scholar] [CrossRef]
- Chopp-Hurley, J.N.; Wiebenga, E.G.; Keller, H.H.; Maly, M.R. Nutrition Risk, Physical Activity and Fibre Intake Are Associated with Body Composition in OA: Analysis of the Canadian Longitudinal Study on Aging. BMJ Nutr. Prev. Health 2022, 5, 191–200. [Google Scholar] [CrossRef]
- Martínez-Hernández, B.M.; Rosas-Carrasco, O.; López-Teros, M.; González-Rocha, A.; Muñoz-Aguirre, P.; Palazuelos-González, R.; Ortíz-Rodríguez, A.; Luna-López, A.; Denova-Gutiérrez, E. Association between Physical Activity and Physical and Functional Performance in Non-Institutionalized Mexican Older Adults: A Cohort Study. BMC Geriatr. 2022, 22, 388. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.; Alarcón-Rivera, M.; Hernandez-Martinez, J.; Herrera-Valenzuela, T.; Branco, B.H.M.; Núñez-Espinosa, C.; Guzmán-Muñoz, E. Factors Associated with Poor Health-Related Quality of Life in Physically Active Older People. Int. J. Environ. Res. Public Health 2022, 19, 13799. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Valdés-Badilla, P.; Herrera-Valenzuela, T.; Guzmán-Muñoz, E.; Delgado-Floody, P.; Núñez-Espinosa, C.; Monsalves-Álvarez, M.; Andrade, D.C. Effects of Olympic Combat Sports on Health-Related Quality of Life in Middle-Aged and Older People: A Systematic Review. Front. Psychol. 2022, 12, 797537. [Google Scholar] [CrossRef]
- Miller, I.; Climstein, M.; Del Vecchio, L. Functional benefits of hard martial arts for older adults: A scoping review. Int. J. Exerc. Sci. 2022, 15, 1430–1443. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.; Ramirez-Campillo, R.; Herrera-Valenzuela, T.; Branco, B.H.M.; Guzmán-Muñoz, E.; Mendez-Rebolledo, G.; Concha-Cisternas, Y.; Hernandez-Martínez, J. Effectiveness of Olympic Combat Sports on Balance, Fall Risk or Falls in Older Adults: A Systematic Review. Biology 2022, 11, 74. [Google Scholar] [CrossRef]
- Yang, F.C.; Desai, A.B.; Esfahani, P.; Sokolovskaya, T.V.; Bartlett, D.J. Effectiveness of Tai Chi for Health Promotion of Older Adults: A Scoping Review of Meta-Analyses. Am. J. Lifestyle Med. 2022, 16, 700–716. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.; Guzmán-Muñoz, E.; Herrera-Valenzuela, T.; Branco, B.H.M.; Hernandez-Martinez, J.; Nobari, H. Impact of Adapted Taekwondo vs. Multicomponent Training on Health Status in Independent Older Women: A Randomized Controlled Trial. Front. Public Health 2023, 11, 74. [Google Scholar] [CrossRef]
- Elhamrawy, M.Y.; Sherbini AehIes, M.E.; Mokhtar, M.M.; Mashaal, A.; Elkady, S.M.; Elsadany, S.M.; Said, M.T. Effect of Tai Chi versus Aerobic Training on Improving Hand Grip Strength, Fatigue, and Functional Performance in Older Adults Post-COVID-19: A Randomized Controlled Trial. J. Popul. Ther. Clin. Pharmacol. 2023, 30, E190–E198. [Google Scholar] [CrossRef]
- Cui, Z.; Xiong, J.; Li, Z.; Yang, C. Tai Chi Improves Balance Performance in Healthy Older Adults: A Systematic Review and Meta-Analysis. Front. Public Health 2024, 12, 1443168. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.; Guzmán-Muñoz, E.; Ramírez-Campillo, R.; Godoy-Cumillaf, A.; Concha-Cisternas, Y.; Ortega-Spuler, J.; Herrera-Valenzuela, T.; Durán-Agüero, S.; Vargas-Vitoria, R.; Magnani-Branco, B.H. Changes in Anthropometric Parameters and Physical Fitness in Older Adults after Participating in a 16-Week Physical Activity Program. Rev. Fac. De Med. 2020, 68, 375–382. [Google Scholar] [CrossRef]
- Ministerio de Salud de Chile. Manual de Aplicación del Examen de Medicina Preventiva del Adulto Mayor. Programa de Salud del Adulto Mayor; División de Prevención y Control de Enfermedades; Subsecretaría de Salud Pública; Santiago, Chile. 2013. Available online: https://diprece.minsal.cl/wrdprss_minsal/wp-content/uploads/2015/05/instructivo-de-control-de-salud-empam.pdf (accessed on 23 September 2025).
- Marfell-Jones, M.J.; Stewart, A.; de Ridder, J. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Wellington, New Zealand, 2012. [Google Scholar]
- Cofre-Bolados, C.; Ferrari, G.; Valdivia-Moral, P.; Vidal-Díaz, F.; Ramírez-Vélez, R.; Izquierdo-Redin, M. Sub Maximal Ergospirometry Parameters in Untrained Non-Frail Octogenarian Subjects. Medicina 2022, 58, 378. [Google Scholar] [CrossRef]
- Wasserman, K.; Hansen, J.E.; Sue, D.Y.; Whipp, B.J.; Froelicher, V.F. Principles of Exercise Testing and Interpretation. J. Cardiopulm. Rehabil. 1987, 7, 189. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and Validation of Criterion-Referenced Clinically Relevant Fitness Standards for Maintaining Physical Independence in Later Years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Comfort, P.; Dos, T.; Beckham, G.K.; Stone, M.H.; Guppy, S.N.; Gregory Haff, G. Standardization and Methodological Considerations for the Isometric Midthigh Pull. J. Strength. Cond. Res. 2019, 41, 57–79. [Google Scholar] [CrossRef]
- Dos’santos, T.; Jones, P.A.; Comfort, P.; Thomas, C. Effect of Different Onset Thresholds on Isometric Midthigh Pull Force-Time Variables. J. Strength. Cond. Res. 2017, 31, 3463–3473. [Google Scholar] [CrossRef]
- Hernandez-Martinez, J.; Castillo-Cerda, M.; Vera-Assaoka, T.; Carter-Truillier, B.; Herrera-Valenzuela, T.; Guzmán-Muñoz, E.; Branco, B.H.M.; Jofré-Saldía, E.; Valdés-Badilla, P. Warm-Up and Handgrip Strength in Physically Inactive Chilean Older Females According to Baseline Nutritional Status. Int. J. Environ. Res. Public Health 2022, 19, 13335. [Google Scholar] [CrossRef]
- Jones, C.J.; Rikli, R.E.; Beam, W.C. A 30-s Chair-Stand Test as a Measure of Lower Body Strength in Community-Residing Older Adults. Res. Q. Exerc. Sport. 1999, 70, 113–119. [Google Scholar] [CrossRef]
- Bruun, I.H.; Mogensen, C.B.; Nørgaard, B.; Schiøttz-Christensen, B.; Maribo, T. Validity and Responsiveness to Change of the 30-Second Chair-Stand Test in Older Adults Admitted to an Emergency Department. J. Geriatr. Phys. Ther. 2019, 42, 265–274. [Google Scholar] [CrossRef]
- Ayala, F.; Sainz de Baranda, P.; de Ste Croix, M.; Santonja, F. Fiabilidad y Validez de Las Pruebas Sit-and-Reach: Revisión Sistemática. Revisa Andal. Med. Deporte 2012, 5, 57–66. [Google Scholar] [CrossRef]
- Bhattacharya, P.K.; Deka, K.; Roy, A. Assessment of Inter-Rater Variability of the Senior Fitness Test in the Geriatric Population: A Community Based Study. Int. J. Biomed. Adv. Res. 2016, 7, 208. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.; Herrera-Valenzuela, T.; Guzmán-Muñoz, E.; Hernandez-Martinez, J.; Cid-Calfucura, I.; Vásquez-Carrasco, E.; Aristegui-Mondaca, J.; Aravena-Sagardia, P.; Mota, J.; Zapata-Bastias, J.; et al. Adapted Taekwondo Improves Postural Balance and Health-Related Quality of Life Concerning Multicomponent Training and Walking Exercise in Older Females: A Randomized Controlled Trial (TKD and Aging Project). J. Clin. Med. 2024, 13, 7250. [Google Scholar] [CrossRef] [PubMed]
- Mao, M.; Mercer, V.S.; Li, F.; Gross, M.T.; Blackburn, T.; Yu, B. The Effect of Tai Chi Lower Extremity Exercise on the Balance Control of Older Adults in Assistant Living Communities. BMC Complement. Med. Ther. 2024, 24, 112. [Google Scholar] [CrossRef] [PubMed]
- Haddad, M.; Stylianides, G.; Djaoui, L.; Dellal, A.; Chamari, K. Session-RPE Method for Training Load Monitoring: Validity, Ecological Usefulness, and Influencing Factors. Front. Neurosci. 2017, 11, 612. [Google Scholar] [CrossRef]
- Reddy, A.K.; Jogendra, M.R.D.; Rosendorff, C. Blood Pressure Measurement in the Geriatric Population. Blood Press. Monit. 2014, 19, 59–63. [Google Scholar] [CrossRef]
- Rendón-Macías, M.E.; Zarco-Villavicencio, I.S.; Villasís-Keever, M.Á. Statistical Methods for Effect Size Analysis. Rev. Alerg. Mex. 2021, 68, 128–136. [Google Scholar] [CrossRef]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Richardson, J.T.E. Eta Squared and Partial Eta Squared as Measures of Effect Size in Educational Research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Siu, P.M.; Yu, A.P.; Chin, E.C.; Yu, D.S.; Hui, S.S.; Woo, J.; Fong, D.Y.; Wei, G.X.; Irwin, M.R. Effects of Tai Chi or Conventional Exercise on Central Obesity in Middle-Aged and Older Adults a Three-Group Randomized Controlled Trial. Ann. Intern. Med. 2021, 174, 1050–1057. [Google Scholar] [CrossRef] [PubMed]
- Valdés-Badilla, P.; Herrera-Valenzuela, T.; Ramirez-Campillo, R.; Aedo-Muñoz, E.; Báez-San Martín, E.; Ojeda-Aravena, A.; Branco, B.H.M. Effects of Olympic combat sports on older adults’ health status: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 7381. [Google Scholar] [CrossRef] [PubMed]
- Vásquez-Carrasco, E.; Hernandez-Martinez, J.; Cid-Calfucura, I.; Guzmán-Muñoz, E.; Ruiz, C.; Baeza, C.; Márquez, M.J.; Herrera-Valenzuela, T.; Branco, B.H.M.; Carmine-Peña, E.; et al. Effects of Different Interventions Using Taekwondo, Boxing, and Elastic Band Training on Body Composition and Physical Function in Chilean Older Women: A Randomized Controlled Trial. Life 2025, 15, 1049. [Google Scholar] [CrossRef]
- Deutz, N.E.; Bauer, J.M.; Barazzoni, R.; Biolo, G.; Boirie, Y.; Bosy-Westphal, A.; Cederholm, T.; Cruz-Jentoft, A.; Krznariç, Z.; Nair, K.S.; et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the ESPEN Expert Group. Clin. Nutr. 2014, 33, 929–936. [Google Scholar] [CrossRef]
- Wang, C.; Collet, J.P.; Lau, J. The effect of Tai Chi on health outcomes in patients with chronic conditions: A systematic review. Arch. Intern. Med. 2004, 164, 493–501. [Google Scholar] [CrossRef]
- Cofre-Bolados, C.; Vidal, F.; Gutiérrez Espinoza, H.; Betancourt-Peters, I.; Orihuela, P.A.; Izquierdo, M. Periodized Aerobic Training between Thresholds Improves Submaximal Cardiorespiratory Parameters in Octogenarians. Sports 2023, 11, 219. [Google Scholar] [CrossRef] [PubMed]
- Sloth, M.; Sloth, D.; Overgaard, K.; Dalgas, U. Effects of Sprint Interval Training on VO2max and Aerobic Exercise Performance: A Systematic Review and Meta-Analysis. Scand. J. Med. Sci. Sports 2013, 23, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Franchini, E. Energy System Contributions during Olympic Combat Sports: A Narrative Review. Metabolites 2023, 13, 297. [Google Scholar] [CrossRef] [PubMed]
- Bartel, C.; Coswig, V.S.; Protzen, G.V.; Del Vecchio, F.B. Energy Demands in High-Intensity Intermittent Taekwondo Specific Exercises. PeerJ 2022, 10, e13654. [Google Scholar] [CrossRef]
- Milanović, Z.; Sporiš, G.; Weston, M. Effectiveness of High-Intensity Interval Training (HIT) and Continuous Endurance Training for VO2max Improvements: A Systematic Review and Meta-Analysis of Controlled Trials. Sports Med. 2015, 45, 1469–1481. [Google Scholar] [CrossRef]
- Sert, H.; Eren, M.G.; Gurcay, B.; Koc, F. The effectiveness of a high-intensity interval exercise on cardiometabolic health and quality of life in older adults: A systematic review and meta-analysis. BMC Sports Sci. Med. Rehabil. 2025, 17, 128. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Lee, E.N.; Ernst, E. Is Tai Chi Beneficial for Improving Aerobic Capacity? A Systematic Review. Br. J. Sports Med. 2009, 43, 569–573. [Google Scholar] [CrossRef]
- Taylor-Piliae, R.E.; Hoke, T.M.; Hepworth, J.T.; Latt, L.D.; Najafi, B.; Coull, B.M. Effect of Tai Chi on Physical Function, Fall Rates and Quality of Life among Older Stroke Survivors. In Proceedings of the Archives of Physical Medicine and Rehabilitation; W.B. Saunders: Philadelphia, PA, USA, 2014; Volume 95, pp. 816–824. [Google Scholar]
- Smart, T.F.F.; Doleman, B.; Hatt, J.; Paul, M.; Toft, S.; Lund, J.N.; Phillips, B.E. The Role of Resistance Exercise Training for Improving Cardiorespiratory Fitness in Healthy Older Adults: A Systematic Review and Meta-Analysis. Age Ageing 2022, 51, afac143. [Google Scholar]
- Rubenstein, L.Z.; Josephson, K.R. The epidemiology of falls and syncope. Clin. Geriatr. Med. 2002, 18, 141–158. [Google Scholar] [CrossRef]
- Kujach, S.; Chroboczek, M.; Jaworska, J.; Sawicka, A.; Smaruj, M.; Winklewski, P.; Laskowski, R. Judo Training Program Improves Brain and Muscle Function and Elevates the Peripheral BDNF Concentration among the Elderly. Sci. Rep. 2022, 12, 13900. [Google Scholar] [CrossRef]
- Penn, I.W.; Sung, W.H.; Lin, C.H.; Chuang, E.; Chuang, T.Y.; Lin, P.H. Effects of Individualized Tai-Chi on Balance and Lower-Limb Strength in Older Adults. BMC Geriatr. 2019, 19, 235. [Google Scholar] [CrossRef]
- Cormie, P.; McGuigan, M.R.; Newton, R.U. Developing Maximal Neuromuscular Power: Part 1—Biological Basis of Maximal Power Production. Sports Med. 2011, 41, 17–38. [Google Scholar] [CrossRef]
- Lee, S.S.; Scott, S.D.; Pekas, E.J.; Park, S.Y. Taekwondo training reduces blood catecholamine levels and arterial stiffness in postmenopausal women with stage-2 hypertension: Randomized clinical trial. Clin. Exp. Hypertens. 2019, 41, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Gamble, P. Implications and Applications of Training Specificity for Coaches and Athletes. Strength. Cond. J. 2006, 28, 54–58. [Google Scholar] [CrossRef]
- Wehner, C.; Blank, C.; Arvandi, M.; Wehner, C.; Schobersberger, W. Effect of Tai Chi on Muscle Strength, Physical Endurance, Postural Balance and Flexibility: A Systematic Review and Meta-Analysis. BMJ Open Sport. Exerc. Med. 2021, 7, e000817. [Google Scholar] [CrossRef]
- Bohannon, R.W. Minimal Clinically Important Difference for Grip Strength: A Systematic Review. J. Phys. Ther. Sci. 2017, 31, 75–78. [Google Scholar] [CrossRef]
- Kim, Y.H.; Jeong, M.K.; Park, H.; Park, S.K. Effects of Regular Taekwondo Intervention on Health-Related Physical Fitness, Cardiovascular Disease Risk Factors and Epicardial Adipose Tissue in Elderly Women with Hypertension. Int. J. Environ. Res. Public Health 2021, 18, 2935. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.Y.; Mayer, P.K.; Wu, M.Y.; Liu, D.H.; Wu, P.C.; Yen, H.R. The Effect of Tai Chi in Elderly Individuals with Sarcopenia and Frailty: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ageing Res. Rev. 2022, 82, 101747. [Google Scholar] [CrossRef]
- Mailapalli, D.R.; Benton, J.; Woodward, T.W. Biomechanics of the Taekwondo Axe Kick: A Review. J. Hum. Sport Exerc. 2015, 10, 141–149. [Google Scholar] [CrossRef]
- Franchini, E.; Herrera-Valenzuela, T. Developing Flexibility for Combat Sports Athletes. Rev. De Artes Marciales Asiat. 2021, 16, 192–203. [Google Scholar] [CrossRef]
- Niño, A.; Villa-Vicente, J.G.; Collado, P.S. Functional Capacity of Tai Chi-Practicing Elderly People. Int. J. Environ. Res. Public Health 2022, 19, 2178. [Google Scholar] [CrossRef] [PubMed]



| Variables | TKD Group (n = 11) | TC Group (n = 10) | p-Value |
|---|---|---|---|
| Age (years) | 70.7 ± 7.0 | 74.8 ± 6.6 | 0.18 |
| Height (m) | 1.58 ± 0.08 | 1.59 ± 0.06 | 0.88 |
| Body mass (kg) | 64.1 ± 11.6 | 67.4 ± 8.5 | 0.47 |
| BMI (kg/m2) | 25.4 ± 3.9 | 26.6 ± 3.2 | 0.44 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrera-Valenzuela, T.; Cid-Calfucura, I.; Hernandez-Martinez, J.; Valdés-Badilla, P.; García-García, J.M.; Calvo-Rico, B.; Cofre-Bolados, C.; Pavez-Lizarraga, A.; Flandes-Vargas, V.; Segueida-Lorca, Á.; et al. Comparative Effects of Adapted Taekwondo Versus Tai Chi on Health Status in Independent Older Women: A Randomized Controlled Trial. Life 2025, 15, 1511. https://doi.org/10.3390/life15101511
Herrera-Valenzuela T, Cid-Calfucura I, Hernandez-Martinez J, Valdés-Badilla P, García-García JM, Calvo-Rico B, Cofre-Bolados C, Pavez-Lizarraga A, Flandes-Vargas V, Segueida-Lorca Á, et al. Comparative Effects of Adapted Taekwondo Versus Tai Chi on Health Status in Independent Older Women: A Randomized Controlled Trial. Life. 2025; 15(10):1511. https://doi.org/10.3390/life15101511
Chicago/Turabian StyleHerrera-Valenzuela, Tomás, Izham Cid-Calfucura, Jordan Hernandez-Martinez, Pablo Valdés-Badilla, José Manuel García-García, Bibiana Calvo-Rico, Cristián Cofre-Bolados, Amaya Pavez-Lizarraga, Verónica Flandes-Vargas, Álvaro Segueida-Lorca, and et al. 2025. "Comparative Effects of Adapted Taekwondo Versus Tai Chi on Health Status in Independent Older Women: A Randomized Controlled Trial" Life 15, no. 10: 1511. https://doi.org/10.3390/life15101511
APA StyleHerrera-Valenzuela, T., Cid-Calfucura, I., Hernandez-Martinez, J., Valdés-Badilla, P., García-García, J. M., Calvo-Rico, B., Cofre-Bolados, C., Pavez-Lizarraga, A., Flandes-Vargas, V., Segueida-Lorca, Á., & Sánchez-Ramírez, C. (2025). Comparative Effects of Adapted Taekwondo Versus Tai Chi on Health Status in Independent Older Women: A Randomized Controlled Trial. Life, 15(10), 1511. https://doi.org/10.3390/life15101511











