High-Intensity Focused Ultrasound Ablation for Primary or Salvage Prostate Cancer Therapy: Initial Outcomes in the Veteran Healthcare Setting
Abstract
1. Introduction
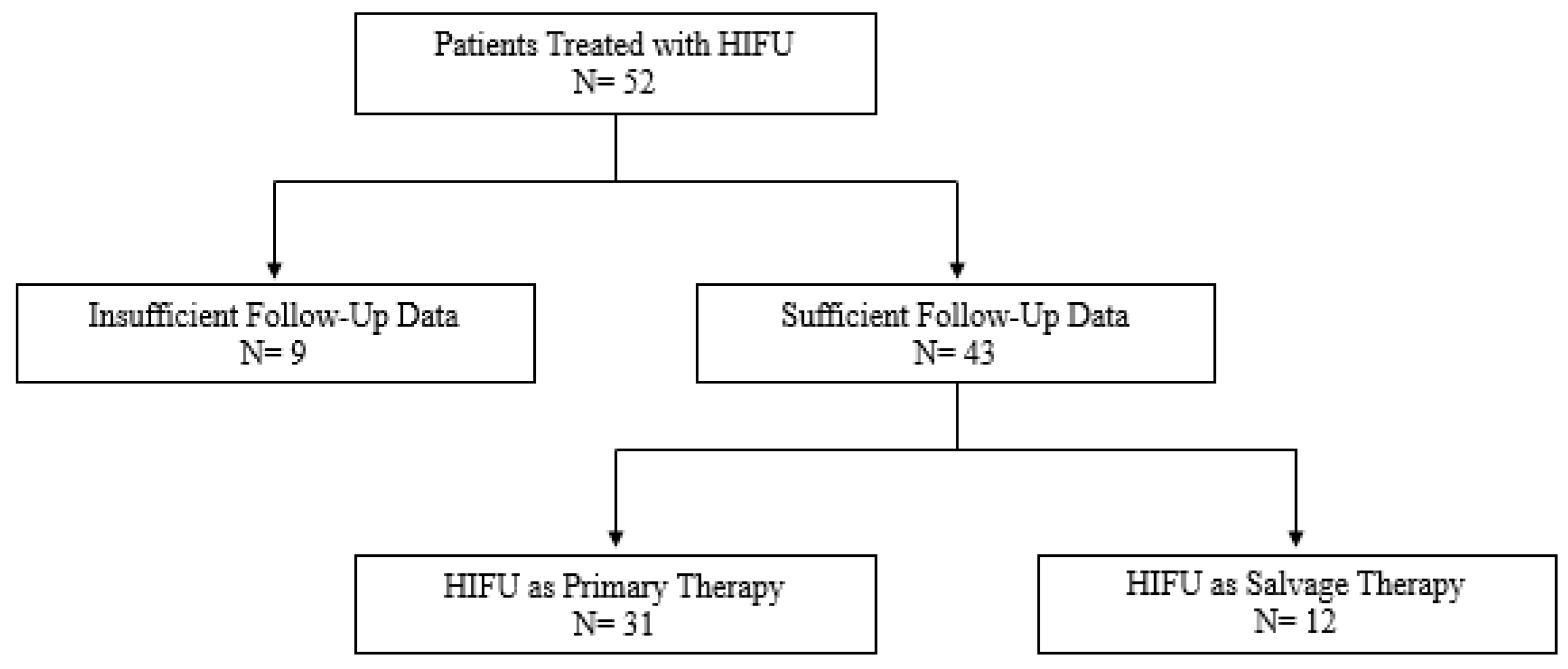
2. Materials and Methods
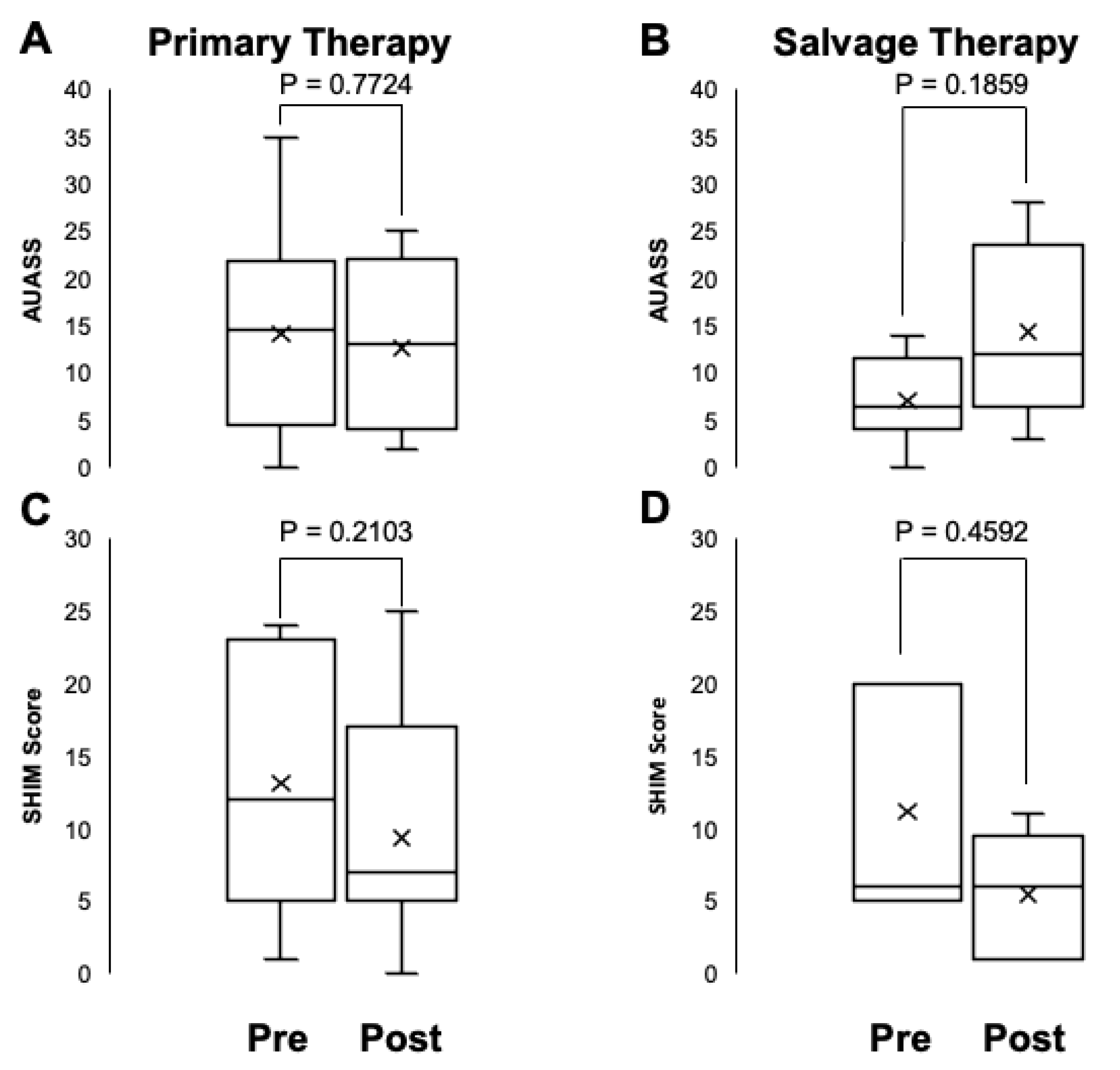
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef]
- National Cancer Institute. Cancer Stat Facts: Prostate Cancer. 2024. Available online: https://seer.cancer.gov/statfacts/html/prost.html (accessed on 18 December 2024).
- Cooperberg, M.R.; Carroll, P.R. Trends in Management for Patients with Localized Prostate Cancer, 1990–2013. JAMA 2015, 314, 80. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.R.; Benjamin, T.G.; Schwartz, M.J.; Rastinehad, A.R. Narrative review—Focal therapy: Are we ready to change the prostate cancer treatment paradigm? Ann. Transl. Med. 2023, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.; Leonardo, M.; Chengodu, T.; Bagguley, D.; Lawrentschuk, N. Irreversible Electroporation for Prostate Cancer. Life 2021, 11, 490. [Google Scholar] [CrossRef]
- Baskaran, R.; Lee, J.; Yang, S.G. Clinical Development of Photodynamic Agents and Therapeutic Applications. Biomater. Res. 2018, 22, 25. [Google Scholar] [CrossRef]
- Jung, J.H.; Risk, M.C.; Goldfarb, R.; Reddy, B.; Coles, B.; Dahm, P. Primary cryotherapy for localised or locally advanced prostate cancer. Cochrane Database Syst. Rev. 2018, 5, CD005010. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Van Luijtelaar, A.; Greenwood, B.M.; Ahmed, H.U.; Barqawi, A.B.; Barret, E.; Bomers, J.G.; Brausi, M.A.; Choyke, P.L.; Cooperberg, M.R.; Eggener, S.; et al. Focal laser ablation as clinical treatment of prostate cancer: Report from a Delphi consensus project. World J. Urol. 2019, 37, 2147–2153. [Google Scholar] [CrossRef] [PubMed]
- European Association of Urology. EAU Prostate Cancer Guidelines. In Proceedings of the EAU Annual Congress, Milan, Italy, 10–13 March 2023. [Google Scholar]
- Nyk, Ł.; Michalak, W.; Szempliński, S.; Woźniak, R.; Zagożdżon, B.; Krajewski, W.; Kryst, P.; Kamecki, H.; Poletajew, S. High-Intensity Focused-Ultrasound Focal Therapy Versus Laparoscopic Radical Prostatectomy: A Comparison of Oncological and Functional Outcomes in Low- and Intermediate-Risk Prostate Cancer Patients. J. Pers. Med. 2022, 12, 251. [Google Scholar] [CrossRef]
- Al Awamlh, B.A.H.; Wallis, C.J.; Penson, D.F.; Huang, L.C.; Zhao, Z.; Conwill, R.; Talwar, R.; Morgans, A.K.; Goodman, M.; Hamilton, A.S.; et al. Functional Outcomes After Localized Prostate Cancer Treatment. JAMA 2024, 331, 302–317. [Google Scholar] [CrossRef]
- Ong, S.; Chen, K.; Grummet, J.; Yaxley, J.; Scheltema, M.J.; Stricker, P.; Tay, K.J.; Lawrentschuk, N. Guidelines of guidelines: Focal therapy for prostate cancer, is it time for consensus? BJU Int. 2023, 131, 20–31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Philippou, Y.; Parker, R.A.; Volanis, D.; Gnanapragasam, V.J. Comparative Oncologic and Toxicity Outcomes of Salvage Radical Prostatectomy Versus Nonsurgical Therapies for Radiorecurrent Prostate Cancer: A Meta-Regression Analysis. Eur. Urol. Focus 2016, 2, 158–171. [Google Scholar] [CrossRef] [PubMed]
- Valle, L.F.; Lehrer, E.J.; Markovic, D.; Elashoff, D.; Levin-Epstein, R.; Karnes, R.J.; Reiter, R.E.; Rettig, M.; Calais, J.; Nickols, N.G.; et al. A Systematic Review and Meta-analysis of Local Salvage Therapies After Radiotherapy for Prostate Cancer (MASTER). Eur. Urol. 2021, 80, 280–292. [Google Scholar] [CrossRef]
- Hopstaken, J.S.; Bomers, J.G.R.; Sedelaar, M.J.P.; Valerio, M.; Fütterer, J.J.; Rovers, M.M. An Updated Systematic Review on Focal Therapy in Localized Prostate Cancer: What Has Changed over the Past 5 Years? Eur. Urol. 2022, 81, 5–33. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, L.; Arya, M.; Afzal, N.; Cathcart, P.; Charman, S.C.; Cornaby, A.; Hindley, R.G.; Lewi, H.; McCartan, N.; Moore, C.M.; et al. Medium-term Outcomes after Whole-gland High-intensity Focused Ultrasound for the Treatment of Nonmetastatic Prostate Cancer from a Multicentre Registry Cohort. Eur. Urol. 2016, 70, 668–674. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, B.; Raess, E.; Schmid, F.A.; Bieri, U.; Scherer, T.P.; Elleisy, M.; Donati, O.F.; Rupp, N.J.; Moch, H.; Gorin, M.A.; et al. Focal therapy with high-intensity focused ultrasound for prostate cancer: 3-year outcomes from a prospective trial. BJU Int. 2024, 133, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Ghai, S.; Finelli, A.; Corr, K.; Lajkosz, K.; McCluskey, S.; Chan, R.; Gertner, M.; van der Kwast, T.H.; Incze, P.F.; Zlotta, A.R.; et al. MRI-Guided Focused Ultrasound Focal Therapy for Intermediate-Risk Prostate Cancer: Final Results from a 2-Year Phase II Clinical Trial. Radiology 2024, 310, e231473. [Google Scholar] [CrossRef]
- Nagaraj, Y.; Falkenbach, F.; Veleva, V.; Pose, R.M.; Ekrutt, J.; Abrams-Pompe, R.; Ratkal, J.; Tennstedt, P.; Tilki, D.; Heinzer, H.; et al. MP73-02 Focal Therapy—7 Years Experience with Focal High Intensity Focused Ultrasound in 164 Patients with Prostate Cancer: Single Center Results. J. Urol. 2023, 209 (Suppl. S4), e1034. [Google Scholar] [CrossRef]
- Hill, C.R.; Ter Haar, G.R. High intensity focused ultrasound—Potential for cancer treatment. Br. J. Radiol. 1995, 68, 1296–1303. [Google Scholar] [CrossRef]
- Sundaram, K.; Chang, S.; Penson, D.; Arora, S. Therapeutic Ultrasound and Prostate Cancer. Semin. Interv. Radiol. 2017, 34, 187–200. [Google Scholar] [CrossRef]
- Taylor, J.; Patel, S.; Gaitonde, K.; Greene, K.; Liao, J.C.; McWilliams, G.; Sawyer, M.; Schroeck, F.; Alrabaa, A.; Saffati, G.; et al. The Management of Non-Muscle-Invasive Bladder Cancer in a Veteran Patient Population: Issues and Recommendations. Curr. Oncol. 2024, 31, 6686–6698. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, A.V.; Whittington, R.; Malkowicz, S.B.; Schultz, D.; Blank, K.; Broderick, G.A.; Tomaszewski, J.E.; Renshaw, A.A.; Kaplan, I.; Beard, C.J.; et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 1998, 280, 969–974. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network (NCCN). Practice Guidelines in Oncology: Prostate Cancer. Version 3.2023. Available online: https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf (accessed on 12 August 2023).
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- JMP. JMP Pro 15: Predictive Analytics Software. Available online: https://www.jmp.com/en_us/software/predictive-analytics-software.html (accessed on 9 January 2024).
- Schmid, F.A.; Schindele, D.; Mortezavi, A.; Spitznagel, T.; Sulser, T.; Schostak, M.; Eberli, D. Prospective multicentre study using high intensity focused ultrasound (HIFU) for the focal treatment of prostate cancer: Safety outcomes and complications. Urol. Oncol. 2020, 38, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Basseri, S.; Perlis, N.; Ghai, S. Focal therapy for prostate cancer. In Abdominal Radiology; Springer: Berlin/Heidelberg, Germany, 2024. [Google Scholar] [CrossRef]
- Crouzet, S.; Blana, A.; Murat, F.J.; Pasticier, G.; Brown, S.C.; Conti, G.N.; Ganzer, R.; Chapet, O.; Gelet, A.; Chaussy, C.G.; et al. Salvage high-intensity focused ultrasound (HIFU) for locally recurrent prostate cancer after failed radiation therapy: Multi-institutional analysis of 418 patients. BJU Int. 2017, 119, 896–904. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Tan, P.; He, M.; Hu, L.; Ai, J.; Yang, L.; Wei, Q. The primary treatment of prostate cancer with high-intensity focused ultrasound: A systematic review and meta-analysis. Medicine 2020, 99, e22610. [Google Scholar] [CrossRef]
- Autran-Gomez, A.M.; Scarpa, R.M.; Chin, J. High-Intensity Focused Ultrasound and Cryotherapy as Salvage Treatment in Local Radio-Recurrent Prostate Cancer. Urol. Int. 2012, 89, 373–379. [Google Scholar] [CrossRef]
- Hernandez, K.M.; Venkat, A.; Elbers, D.C.; Bihn, J.R.; Brophy, M.T.; Do, N.V.; La, J.; Liu, Q.; Prokhorenkov, A.; Metoki-Shlubsky, N.; et al. Prostate cancer patient stratification by molecular signatures in the Veterans Precision Oncology Data Commons. Mol. Case Stud. 2023, 9, a006298. [Google Scholar] [CrossRef] [PubMed]
- Pepe, P.; D’Urso, D.; Garufi, A.; Priolo, G.; Pennisi, M.; Russo, G.; Sabini, M.G.; Valastro, L.M.; Galia, A.; Fraggetta, F. Multiparametric MRI Apparent Diffusion Coefficient (ADC) Accuracy in Diagnosing Clinically Significant Prostate Cancer. In Vivo 2017, 31, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Pepe, P.; Pennisi, M. Targeted Biopsy in Men High Risk for Prostate Cancer: 68Ga-PSMA PET/CT Versus mpMRI. Clin. Genitourin. Cancer 2023, 21, 639–642. [Google Scholar] [CrossRef]
| Primary Therapy | Salvage Therapy | |
|---|---|---|
| No. of patients (N) | 31 | 12 |
| Median age (IQR) | 70 (64–74) | 71 (67–73) |
| Median cc prostate volume (IQR) | 33 (24–50) | 22 (16–32) |
| Median ng/mL PSA (IQR) | 6.2 (4.3–9.0) | 4.9 (4.8–8.8) |
| Median ng/mL/cc PSA density (IQR) | 0.19 (0.09–0.29) | 0.22 (0.15–0.51) |
| Clinical stage (%) | ||
| T1c | 23 (74.2) | 10 (83.3) |
| T2a | 1 (3.2) | 0 (0.0) |
| T2b | 2 (6.5) | 1 (8.3) |
| T2c | 5 (16.1) | 1 (9.3) |
| ISUP grade group (%) | ||
| 1 | 2 (6.5) | 2 (16.6) |
| 2 | 11 (35.5) | 2 (16.6) |
| 3 | 7 (22.6) | 2 (16.6) |
| 4 | 6 (19.4) | 0 (0.0) |
| 5 | 5 (16.1) | 6 (50.0) |
| Entry biopsy | ||
| Median no. of cores taken (IQR) | 12 (12–12) | 12 (12–12) |
| Median pos cores (any Ca) (IQR) | 4 (2–6) | 4 (2–7) |
| Median max Ca core % (IQR) | 50 (20–65) | 43 (24–65) |
| Amount of bilateral Ca on biopsy (%) | 11 (35.5) | 5 (41.7) |
| NCCN risk group (%) | ||
| Low | 2 (6.5) | 2 (16.6) |
| Intermediate favorable | 8 (25.8) | 2 (16.6) |
| Intermediate unfavorable | 10 (32.2) | 1 (8.3) |
| High | 11 (35.5) | 7 (58.3) |
| Prior therapy (%) | ||
| Radiation | 0 (0.0) | 12 (100.0) |
| Hormonal therapy | 0 (0.0) | 1 (8.3) |
| Median CCI (IQR) | 7 (5–8) | 5 (4–6) |
| Median BMI (IQR) | 27 (22–31) | 33 (30–34) |
| Prior abdominal surgery (%) | 9 (29.0) | 2 (16.6) |
| Primary Therapy | Salvage Therapy | |
|---|---|---|
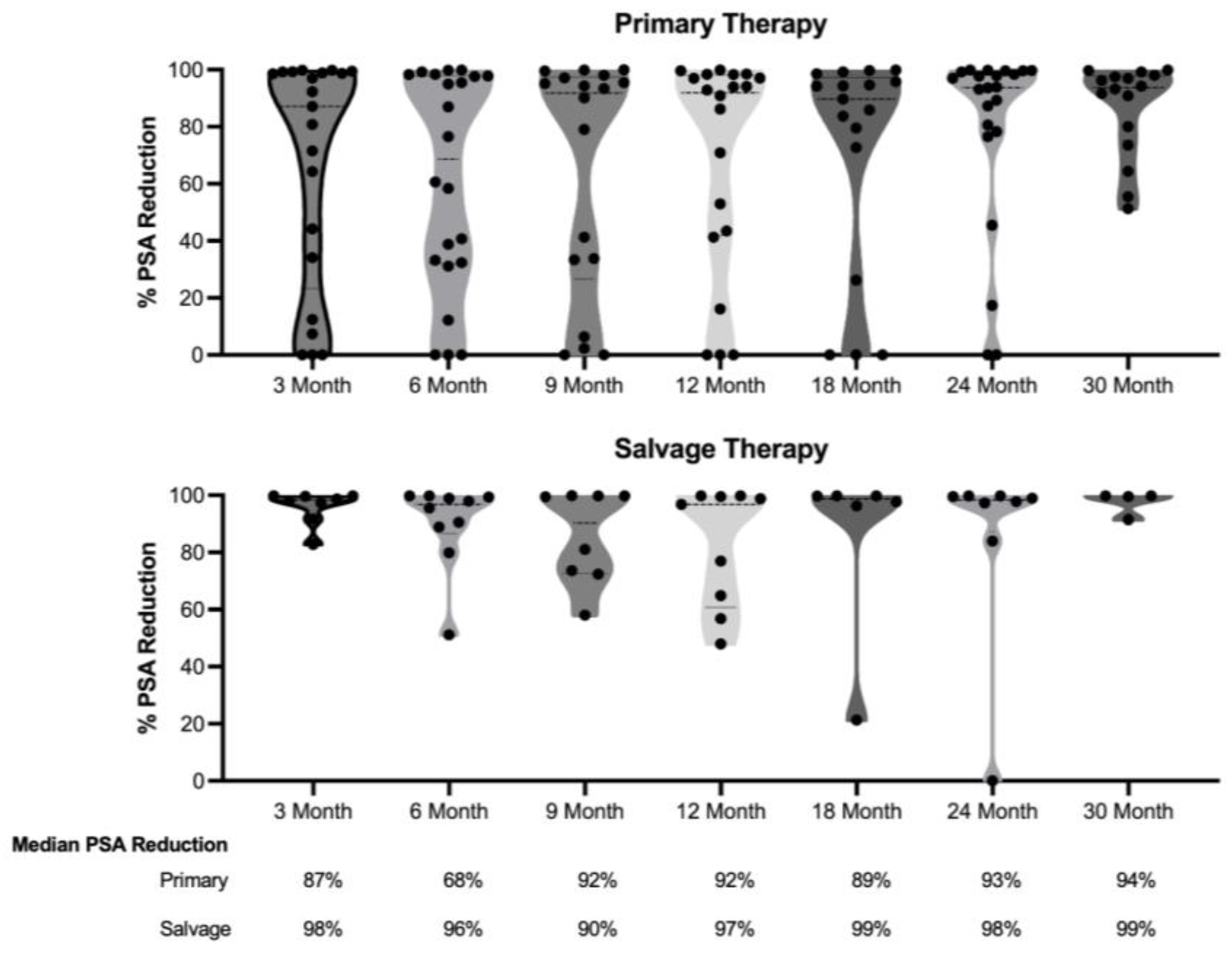
| Median follow-up period, in months (IQR) | 23 (15–34) | 25 (9–39) |
| Median PSA nadir (IQR) | 0.16 (0.06–2.96) | 0.12 (0.01–0.71) |
| Median time to PSA nadir, in months (IQR) | 6 (3–9) | 3 (3–9) |
| Median % PSA decrease (IQR) | 96 (55–99) | 98 (93–99) |
| Local recurrence (%) | 5 (16.1) | 2 (16.6) |
| Post-HIFU treatment (%) | ||
| Radiation | 2 (6.5) | 0 (0) |
| Hormonal | 1 (3.2) | 2 (16.6) |
| HIFU | 1 (3.2) | 0 (0) |
| Radical prostatectomy | 1 (3.2) | 0 (0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, S.; Antar, A.; Alrabaa, A.; Saffati, G.; Fleming, B.; Srikishen, N.; Slawin, J.; Taylor, J.; Jones, J. High-Intensity Focused Ultrasound Ablation for Primary or Salvage Prostate Cancer Therapy: Initial Outcomes in the Veteran Healthcare Setting. Life 2025, 15, 17. https://doi.org/10.3390/life15010017
Patel S, Antar A, Alrabaa A, Saffati G, Fleming B, Srikishen N, Slawin J, Taylor J, Jones J. High-Intensity Focused Ultrasound Ablation for Primary or Salvage Prostate Cancer Therapy: Initial Outcomes in the Veteran Healthcare Setting. Life. 2025; 15(1):17. https://doi.org/10.3390/life15010017
Chicago/Turabian StylePatel, Sagar, Ali Antar, Aly Alrabaa, Gal Saffati, Broderick Fleming, Neel Srikishen, Jeremy Slawin, Jennifer Taylor, and Jeffrey Jones. 2025. "High-Intensity Focused Ultrasound Ablation for Primary or Salvage Prostate Cancer Therapy: Initial Outcomes in the Veteran Healthcare Setting" Life 15, no. 1: 17. https://doi.org/10.3390/life15010017
APA StylePatel, S., Antar, A., Alrabaa, A., Saffati, G., Fleming, B., Srikishen, N., Slawin, J., Taylor, J., & Jones, J. (2025). High-Intensity Focused Ultrasound Ablation for Primary or Salvage Prostate Cancer Therapy: Initial Outcomes in the Veteran Healthcare Setting. Life, 15(1), 17. https://doi.org/10.3390/life15010017







