Ocular Manifestation in Systemic Sclerosis—A Literature Review
Abstract
1. Introduction
2. Methodology
3. Anterior Segment of the Eye
3.1. Eyelids
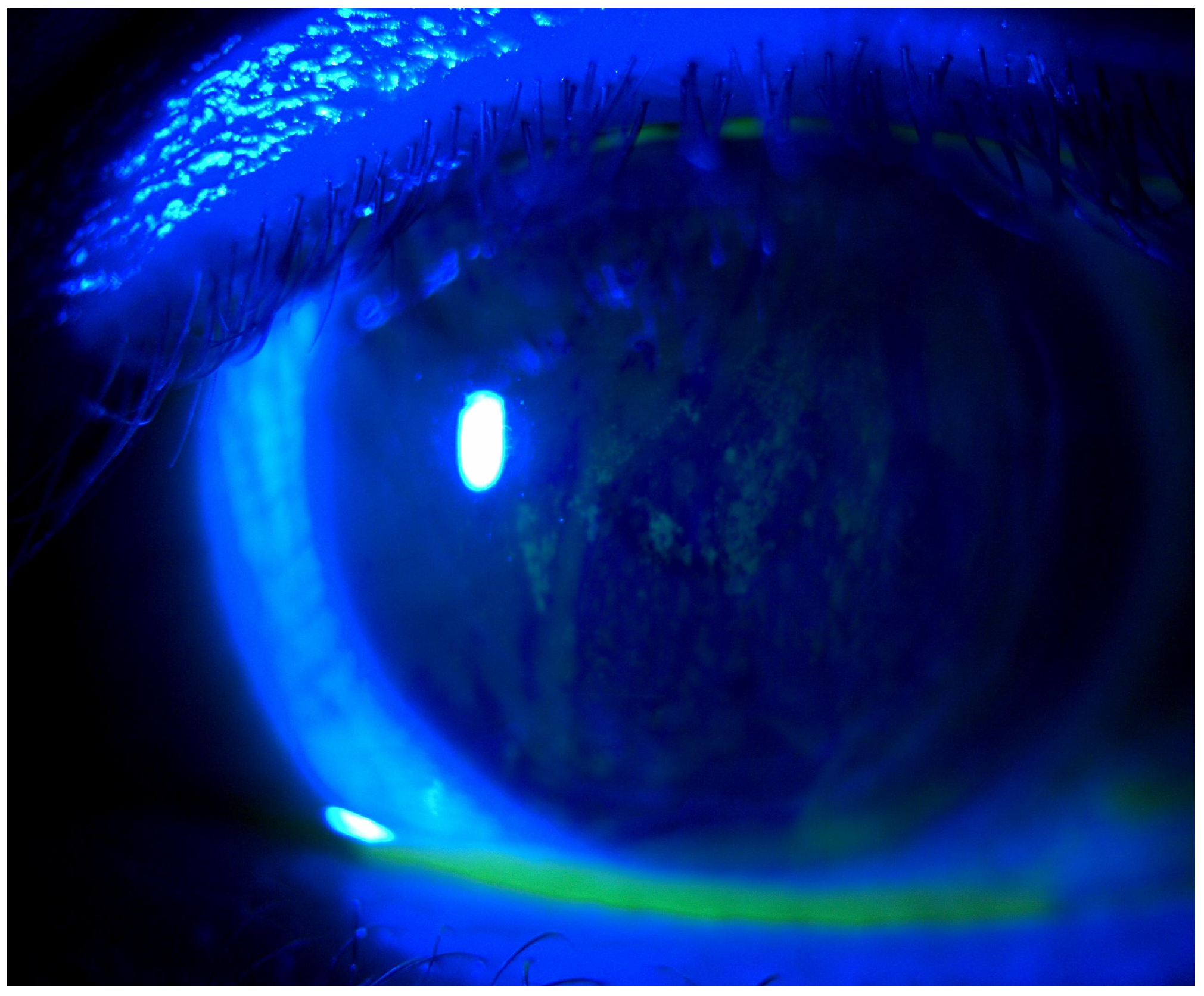
3.2. Dry Eye Disease
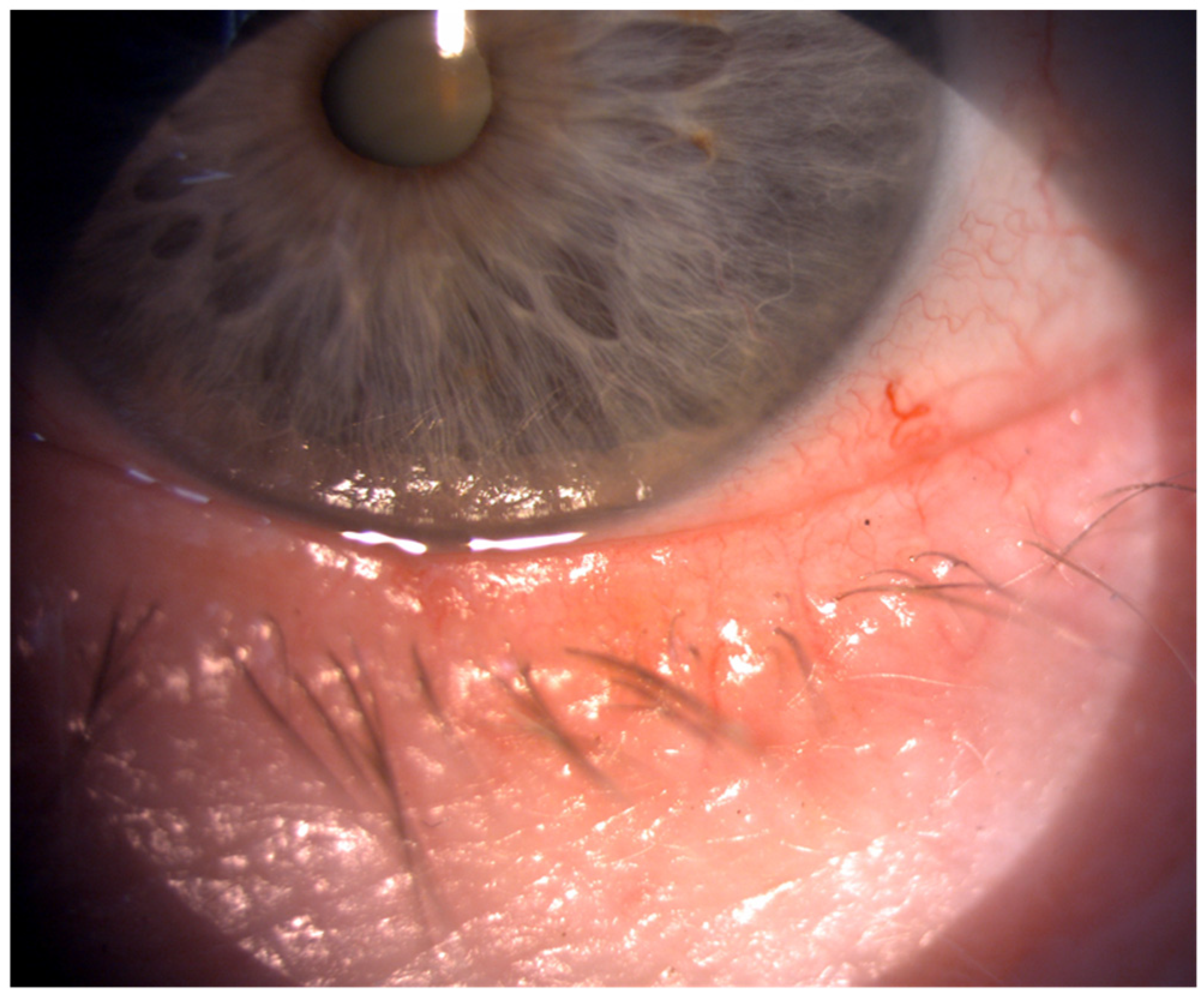
3.3. Conjunctiva
3.4. Cornea
3.5. Iris
3.6. Pupil Diameter
3.7. Cataract
4. Posterior Segment of the Eye
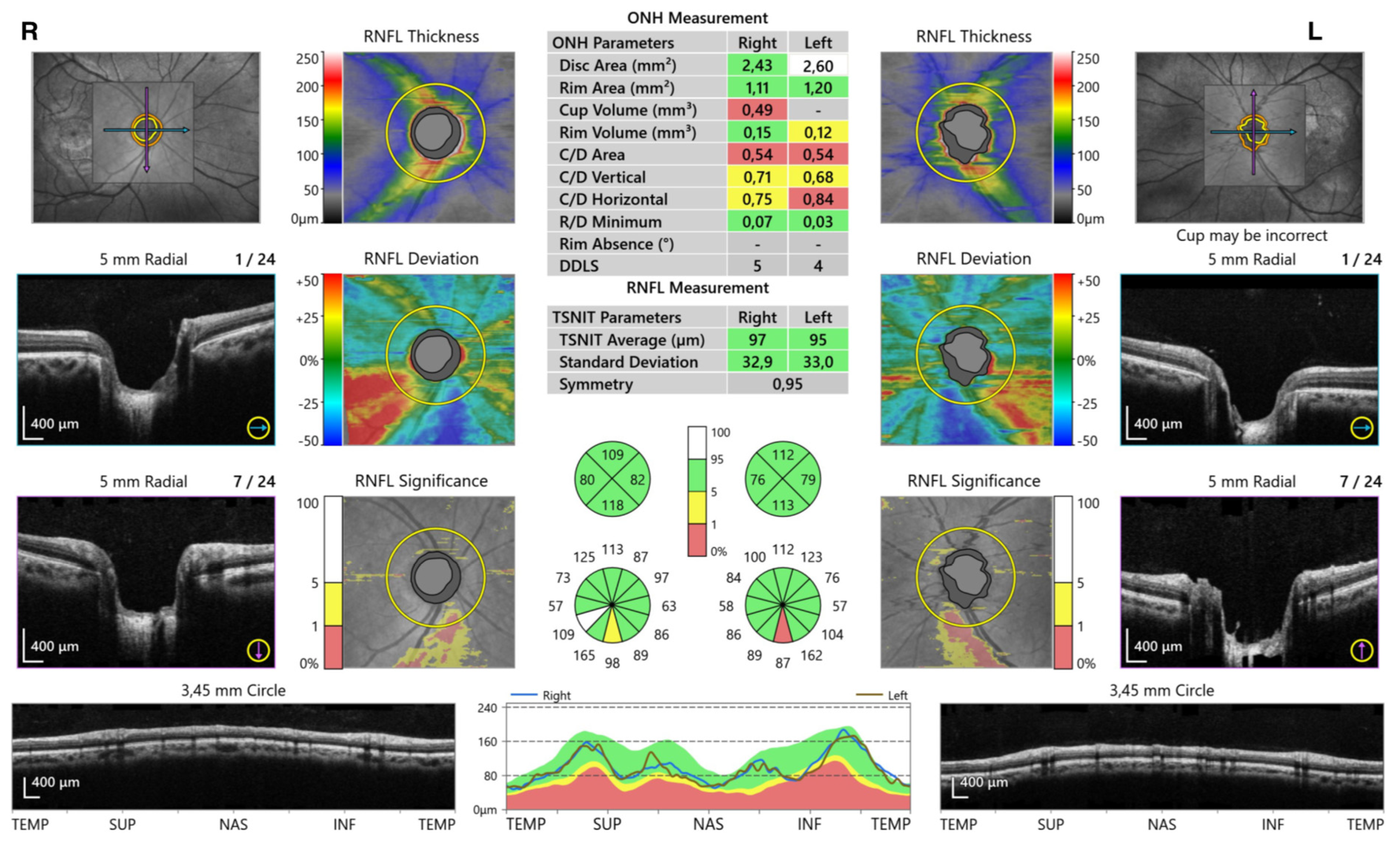
4.1. Glaucoma
4.2. Uveitis
4.3. Vitreous Body
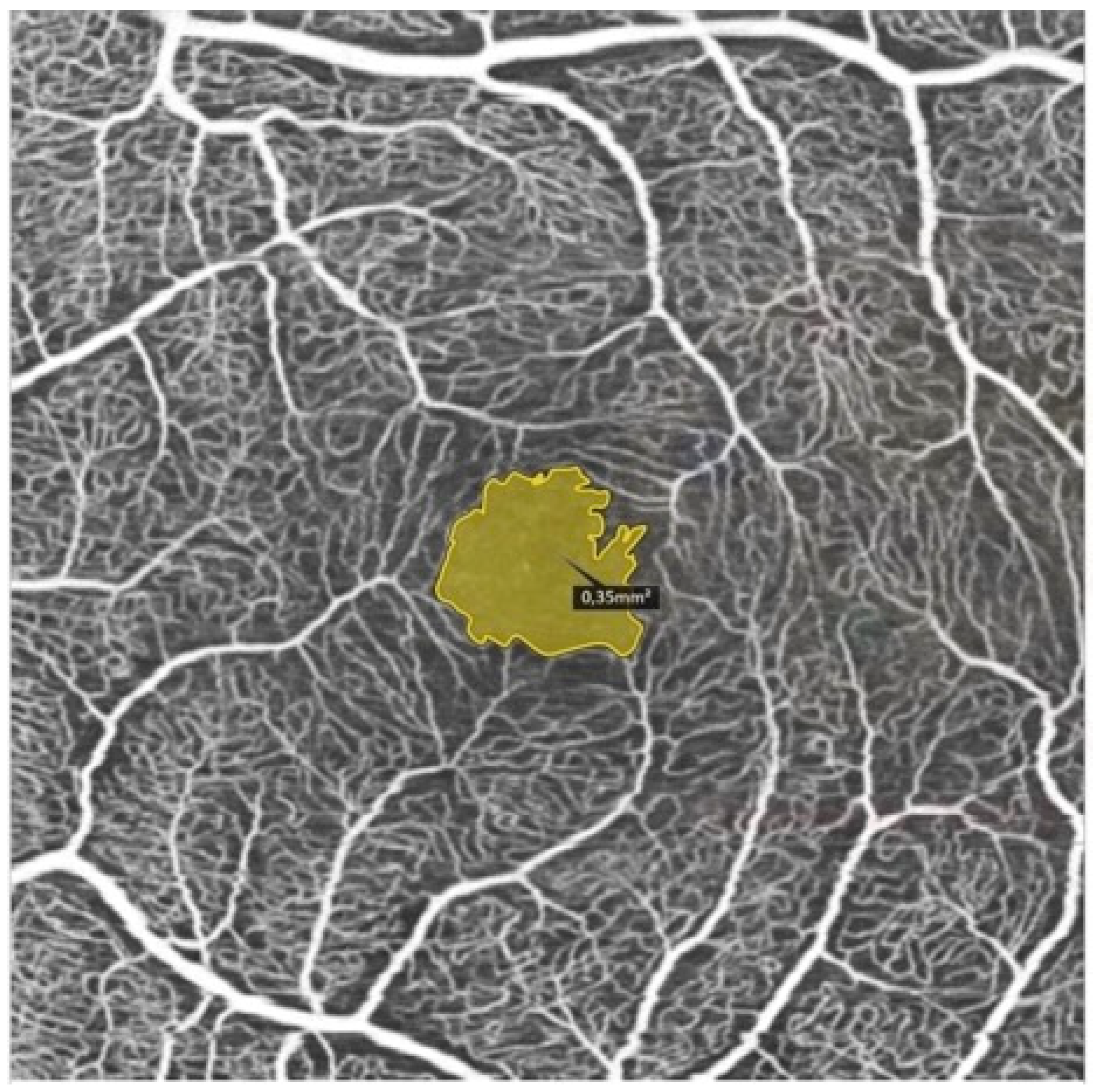
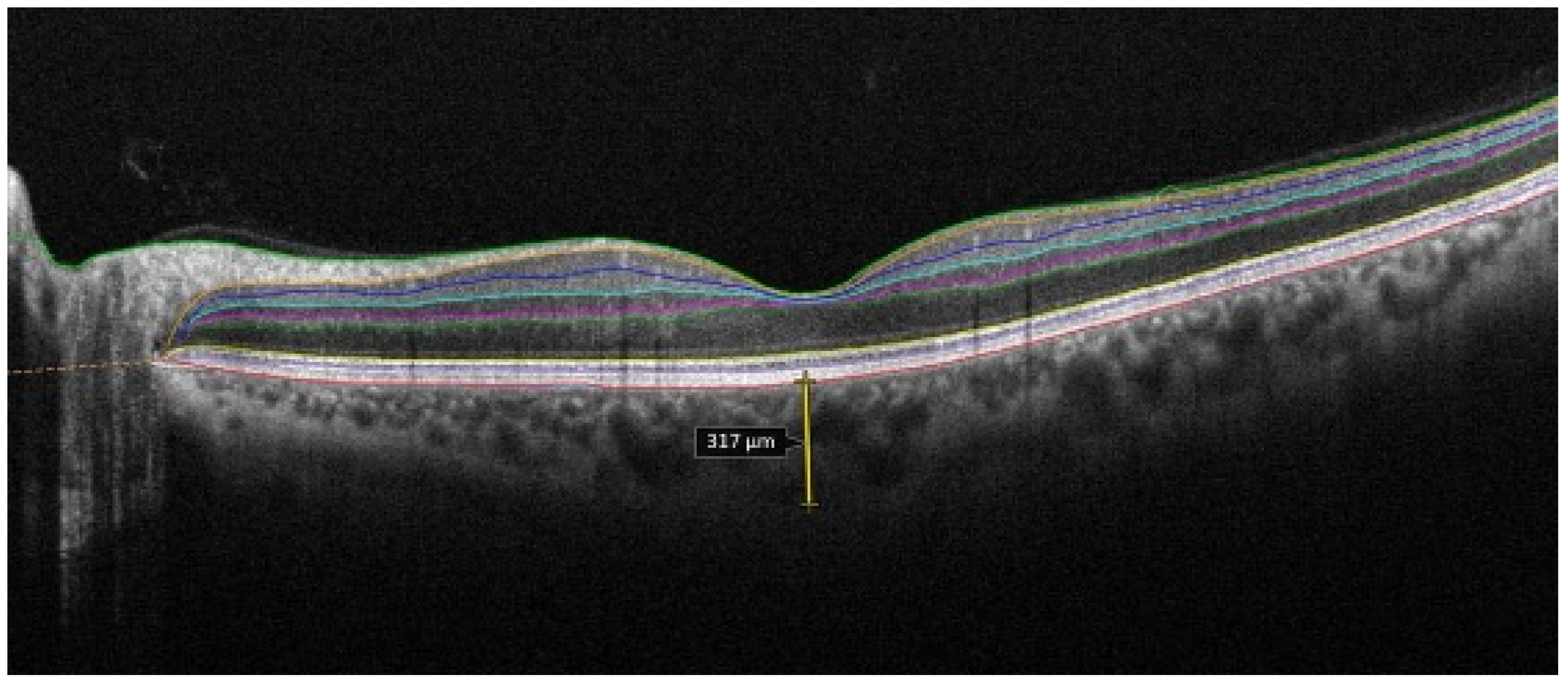
4.4. Retina and Choroid
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Glover, K.; Mishra, D.; Singh, T.R.R. Epidemiology of Ocular Manifestations in Autoimmune Disease. Front. Immunol. 2021, 12, 744396. [Google Scholar] [CrossRef]
- de AF Gomes, B.; Santhiago, M.R.; de Azevedo, M.N.; Moraes, H.V., Jr. Evaluation of dry eye signs and symptoms in patients with systemic sclerosis. Graefes Arch. Clin. Exp. Ophthalmol. 2012, 250, 1051–1056. [Google Scholar] [CrossRef]
- Denton, C.P.; Khanna, D. Systemic sclerosis. Lancet 2017, 390, 1685–1699. [Google Scholar] [CrossRef]
- Nikpour, M.; Stevens, W.M.; Herrick, A.L.; Proudman, S.M. Epidemiology of systemic sclerosis. Best Pract. Res. Clin. Rheumatol. 2010, 24, 857–869. [Google Scholar] [CrossRef]
- Sahin Atik, S.; Koc, F.; Akin Sari, S.; Sefi Yurdakul, N.; Ozmen, M.; Akar, S. Anterior segment parameters and eyelids in systemic sclerosis. Int. Ophthalmol. 2016, 36, 577–583. [Google Scholar] [CrossRef]
- Wollheim, F.A. Classification of systemic sclerosis. Visions and reality. Rheumatology 2005, 44, 1212–1216. [Google Scholar] [CrossRef]
- Gomes Bde, A.; Santhiago, M.R.; Magalhães, P.; Kara-Junior, N.; Azevedo, M.N.; Moraes, H.V., Jr. Ocular findings in patients with systemic sclerosis. Clinics 2011, 66, 379–385. [Google Scholar] [CrossRef]
- Tailor, R.; Gupta, A.; Herrick, A.; Kwartz, J. Ocular manifestations of scleroderma. Surv. Ophthalmol. 2009, 54, 292–304. [Google Scholar] [CrossRef]
- Szucs, G.; Szekanecz, Z.; Aszalos, Z.; Gesztelyi, R.; Zsuga, J.; Szodoray, P.; Kemeny-Beke, A. A Wide Spectrum of Ocular Manifestations Signify Patients with Systemic Sclerosis. Ocul. Immunol. Inflamm. 2021, 29, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, J.; Shen Lee, B.; Periman, L.M. Dry eye disease: Identification and therapeutic strategies for primary care clinicians and clinical specialists. Ann. Med. 2023, 55, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Hynnekleiv, L.; Magno, M.; Vernhardsdottir, R.R.; Moschowits, E.; Tønseth, K.A.; Dartt, D.A.; Vehof, J.; Utheim, T.P. Hyaluronic acid in the treatment of dry eye disease. Acta Ophthalmol. 2022, 100, 844–860. [Google Scholar] [CrossRef]
- Laovirojjanakul, W.; Yospaiboon, Y.; Anutarapongpan, O.; Mahakkanukrauh, A.; Suwannaroj, S.; Nanagara, R.; Foocharoen, C. Predictors for Dry Eye Diseases in Patients with Systemic Sclerosis. Clin. Ophthalmol. 2022, 16, 3447–3455. [Google Scholar] [CrossRef]
- Kudasiewicz-Kardaszewska, A.; Grant-Kels, J.M.; Grzybowski, A. Meibomian gland dysfunction and blepharitis: A common and still unsolved ophthalmic problem. Clin. Dermatol. 2023, 41, 491–502. [Google Scholar] [CrossRef]
- Wangkaew, S.; Kasitanon, N.; Sivasomboon, C.; Wichainun, R.; Sukitawut, W.; Louthrenoo, W. Sicca symptoms in Thai patients with rheumatoid arthritis, systemic lupus erythematosus and scleroderma: A comparison with age-matched controls and correlation with disease variables. Asian Pac. J. Allergy Immunol. 2006, 24, 213–221. [Google Scholar]
- Rentka, A.; Nagy, A.; Harsfalvi, J.; Szucs, G.; Szekanecz, Z.; Gesztelyi, R.; Szodoray, P.; Kemeny-Beke, A. Association between objective signs and subjective symptoms of dry eye disease in patients with systemic sclerosis. Rheumatol. Int. 2017, 37, 1835–1845. [Google Scholar] [CrossRef]
- Salliot, C.; Mouthon, L.; Ardizzone, M.; Sibilia, J.; Guillevin, L.; Gottenberg, J.E.; Mariette, X. Sjogren’s syndrome is associated with and not secondary to systemic sclerosis. Rheumatology 2007, 46, 321–326. [Google Scholar] [CrossRef]
- West, R.H.; Barnett, A.J. Ocular involvement in scleroderma. Br. J. Ophthalmol. 1979, 63, 845–847. [Google Scholar] [CrossRef]
- Mancel, E.; Janin, A.; Gosset, D.; Hatron, P.Y.; Gosselin, B. Conjunctival biopsy in scleroderma and primary Sjögren’s syndrome. Am. J. Ophthalmol. 1993, 115, 792–799. [Google Scholar] [CrossRef]
- Emre, S.; Kayikçioğlu, O.; Ateş, H.; Cinar, E.; Inceoğlu, N.; Yargucu, F.; Prldar, T.; Oksel, F. Corneal hysteresis, corneal resistance factor, and intraocular pressure measurement in patients with scleroderma using the reichert ocular response analyzer. Cornea 2010, 29, 628–631. [Google Scholar] [CrossRef]
- Gomes Bde, A.; Santhiago, M.R.; Kara-Junior, N.; Noé, R.A.; de Azevedo, M.N.; Moraes, H.V., Jr. Central corneal thickness in patients with systemic sclerosis: A controlled study. Cornea 2011, 30, 1125–1128. [Google Scholar] [CrossRef] [PubMed]
- Serup, L.; Serup, J.; Hagdrup, H.K. Increased central cornea thickness in systemic sclerosis. Acta Ophthalmol. 1984, 62, 69–74. [Google Scholar] [CrossRef]
- Waszczykowska, A.; Goś, R.; Waszczykowska, E.; Dziankowska-Bartkowiak, B.; Jurowski, P. Prevalence of ocular manifestations in systemic sclerosis patients. Arch. Med. Sci. 2013, 9, 1107–1113. [Google Scholar] [CrossRef]
- Şahin, M.; Yüksel, H.; Şahin, A.; Cingü, A.K.; Türkcü, F.M.; Kaya, S.; Yazmalar, L.; Batmaz, İ. Evaluation of the anterior segment parameters of the patients with scleroderma. Ocul. Immunol. Inflamm. 2017, 25, 233–238. [Google Scholar] [CrossRef]
- Szalai, E.; Szucs, G.; Szamosi, S.; Aszalos, Z.; Afra, I.; Kemeny-Beke, A. An in vivo confocal microscopy study of corneal changes in patients with systemic sclerosis. Sci. Rep. 2021, 11, 11111. [Google Scholar] [CrossRef]
- Anayol, M.A.; Coşkun, M.; Raza, S.; Çağil, N.; Çakmak, H.B.; ŞimşekŞ. Keratoconus in a case with scleroderma: A rarecoexistence. Turk. Klin. J. Ophthalmol. 2018, 27, 81–84. [Google Scholar] [CrossRef][Green Version]
- Del Rosso, A.; Bertinotti, L.; Pietrini, U.; Messori, A.; Fanciullacci, M.; Casale, R.; Giacomelli, R.; Generini, S.; Sicuteri, R.; Pignone, A.; et al. Pupillocynetic activity of substance P in systemic sclerosis. J. Rheumatol. 2003, 30, 1231–1237. [Google Scholar]
- Kozikowska, M.; Luboń, W.; Kucharz, E.J.; Mrukwa-Kominek, E. Ocular manifestations in patients with systemic sclerosis. Reumatologia 2020, 58, 401–406. [Google Scholar] [CrossRef]
- Gomes, B.F.; Souza, R.; Valadão, T.; Kara-Junior, N.; Moraes, H.V.; Santhiago, M.R. Is there an association between glaucoma and capillaroscopy in patients with systemic sclerosis? Int. Ophthalmol. 2018, 38, 251–256. [Google Scholar] [CrossRef]
- Sahin-Atik, S.; Koc, F.; Akin-Sari, S.; Ozmen, M. Retinal nerve fiber and optic disc morphology using spectral-domain optical coherence tomography in scleroderma patients. Eur. J. Ophthalmol. 2017, 27, 281–284. [Google Scholar] [CrossRef]
- Bolad, W. Anterior Uveitis in a Patient with Scleroderma: A Case Report. Ocul. Immunol. Inflamm. 2013, 21, 11–12. [Google Scholar] [CrossRef]
- Khalayli, N.; Hodifa, Y.; Tarcha, R.; Hodaifa, A.; Kudsi, M. Recurrent uveitis in a patient with CREST syndrome: A case report. Ann. Med. Surg. 2023, 85, 5679–5681. [Google Scholar] [CrossRef]
- Kılınç Hekimsoy, H.; Şekeroğlu, M.A.; Koçer, A.M.; Akdoğan, A. Analysis of retinal and choroidal microvasculature in systemic sclerosis: An optical coherence tomography angiography study. Eye 2020, 34, 763–770. [Google Scholar] [CrossRef]
- Coşkun, E.; Zengin, O.; Kenan, S.; Kimyon, G.; Erdogan Er, K.; Okumus, S.; Mesut Onat, A.; Erbagcı, I.; Kısacık, B. Evaluation of choroidal thickness in patients with scleroderma. Eye 2016, 30, 588–592. [Google Scholar] [CrossRef]
- Ushiyama, O.; Ushiyama, K.; Yamada, T.; Koarada, S.; Tada, Y.; Suzuki, N.; Ohta, A.; Nagasawa, K. Retinal findings in systemic sclerosis: A comparison with nailfold capillaroscopic patterns. Ann. Rheum. Dis. 2003, 62, 204–207. [Google Scholar] [CrossRef]
- Serup, L.; Serup, J.; Hagdrup, H. Fundus fluorescein angiography in generalized scleroderma. Ophthalmic Res. 1987, 19, 303–308. [Google Scholar] [CrossRef]
- Aydin, E.; Atik, S.; Koc, F.; Balikoglu-Yilmaz, M.; Akin Sari, S.; Ozmen, M.; Akar, S. Choroidal and central foveal thickness in patients with scleroderma and its systemic associations. Clin. Exp. Optom. 2017, 100, 656–662. [Google Scholar] [CrossRef]
- Kök, M.; Ayan, A.; Fatih Küçük, M.; Erol, M.K.; Yaprak, L. Evaluation of the direct effects on retinal and choroidal microvascularity of systemic scleroderma. Microvasc. Res. 2021, 136, 104166. [Google Scholar] [CrossRef] [PubMed]
- Rommel, F.; Prangel, D.; Prasuhn, M.; Grisanti, S.; Ranjbar, M. Correlation of retinal and choroidal microvascular impairment in systemic sclerosis. Orphanet J. Rare Dis. 2021, 16, 27. [Google Scholar] [CrossRef]
- Busquets, J.; Lee, Y.; Santamarina, L.; Federman, J.L.; Abel, A.; Del Galdo, F.; Eagle, R.C., Jr.; Jimenez, S.A. Acute retinal artery occlusion in systemic sclerosis: A rare manifestation of systemic sclerosis fibroproliferative vasculopathy. Semin. Arthritis Rheum. 2013, 43, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Mihailovic, N.; Lahme, L.; Braasch, S.; Rosenberger, F.; Eter, N.; Ehrchen, J.; Alnawaiseh, M. Altered ocular microvasculature in patients with systemic sclerosis and very early disease of systemic sclerosis using optical coherence tomography angiography. Sci. Rep. 2022, 12, 10990. [Google Scholar] [CrossRef] [PubMed]
- Cutolo, C.A.; Cere, A.; Toma, P.; Cannavacciuolo, T.; Toma, C.; Balito, S.; Gerli, V.; Smith, V.; Sulli, A.; Paolino, S.; et al. Peripheral and ocular microvascular alterations in systemic sclerosis: Observations from capillaroscopic assessments, perfusion peripheral analysis, and optical coherence tomography angiography. Rheumatol. Int. 2024, 44, 107–118. [Google Scholar] [CrossRef]
- Paczwa, K.; Rerych, M.; Romanowska-Próchnicka, K.; Olesińska, M.; Różycki, R.; Gołębiewska, J. Retinal Microvasculature in Systemic Sclerosis Patients and the Correlation between Nailfold Capillaroscopic Findings and Optical Coherence Angiography Results. J. Clin. Med. 2024, 13, 2025. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paczwa, K.; Rerych, M.; Romanowska-Próchnicka, K.; Różycki, R.; Gołębiewska, J. Ocular Manifestation in Systemic Sclerosis—A Literature Review. Life 2024, 14, 627. https://doi.org/10.3390/life14050627
Paczwa K, Rerych M, Romanowska-Próchnicka K, Różycki R, Gołębiewska J. Ocular Manifestation in Systemic Sclerosis—A Literature Review. Life. 2024; 14(5):627. https://doi.org/10.3390/life14050627
Chicago/Turabian StylePaczwa, Katarzyna, Magdalena Rerych, Katarzyna Romanowska-Próchnicka, Radosław Różycki, and Joanna Gołębiewska. 2024. "Ocular Manifestation in Systemic Sclerosis—A Literature Review" Life 14, no. 5: 627. https://doi.org/10.3390/life14050627
APA StylePaczwa, K., Rerych, M., Romanowska-Próchnicka, K., Różycki, R., & Gołębiewska, J. (2024). Ocular Manifestation in Systemic Sclerosis—A Literature Review. Life, 14(5), 627. https://doi.org/10.3390/life14050627




