Optimal Timing of the Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Early Predictors of Neurological Outcomes in Postcardiac Arrest Patients
Abstract
1. Introduction
2. Materials and Methods
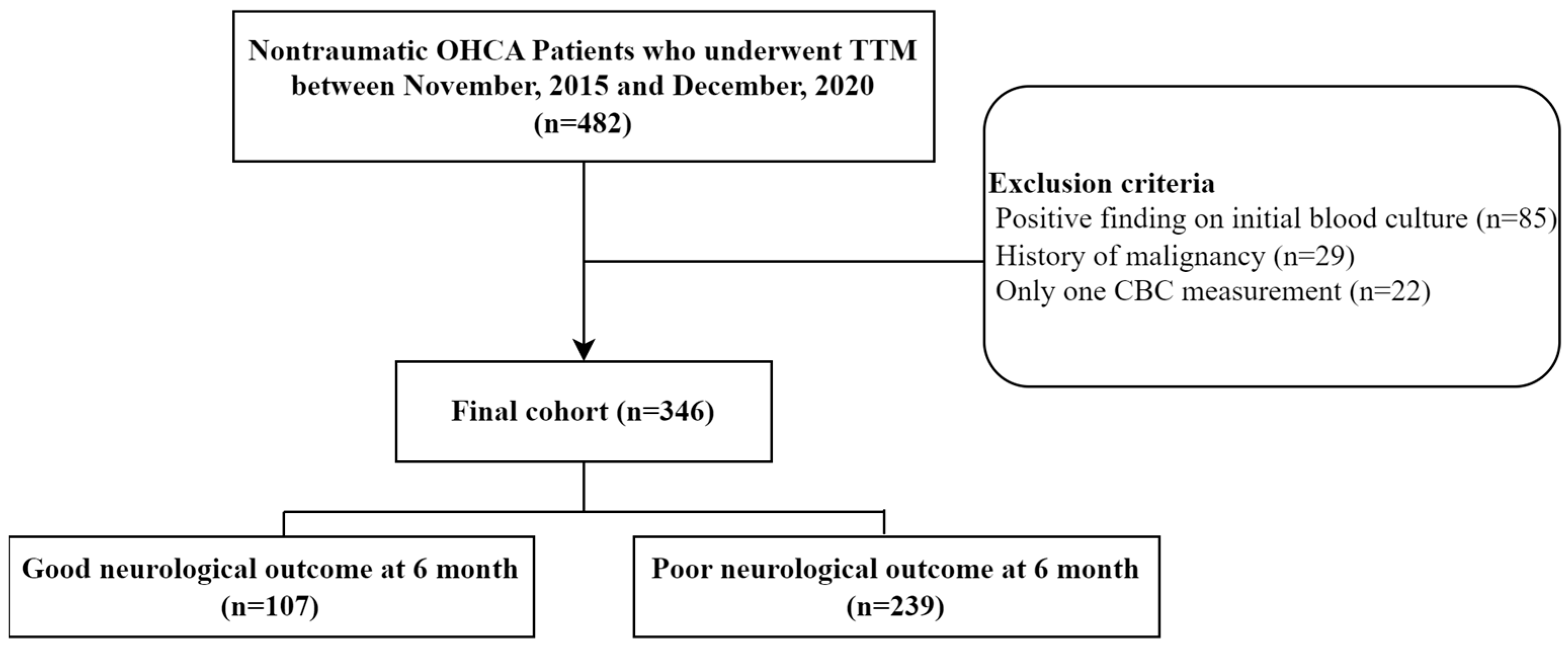
2.1. Study Design and Population
2.2. Data Collection and Outcomes
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Comparison of Early Post-ROSC Adverse Events and Cardiac Interventions
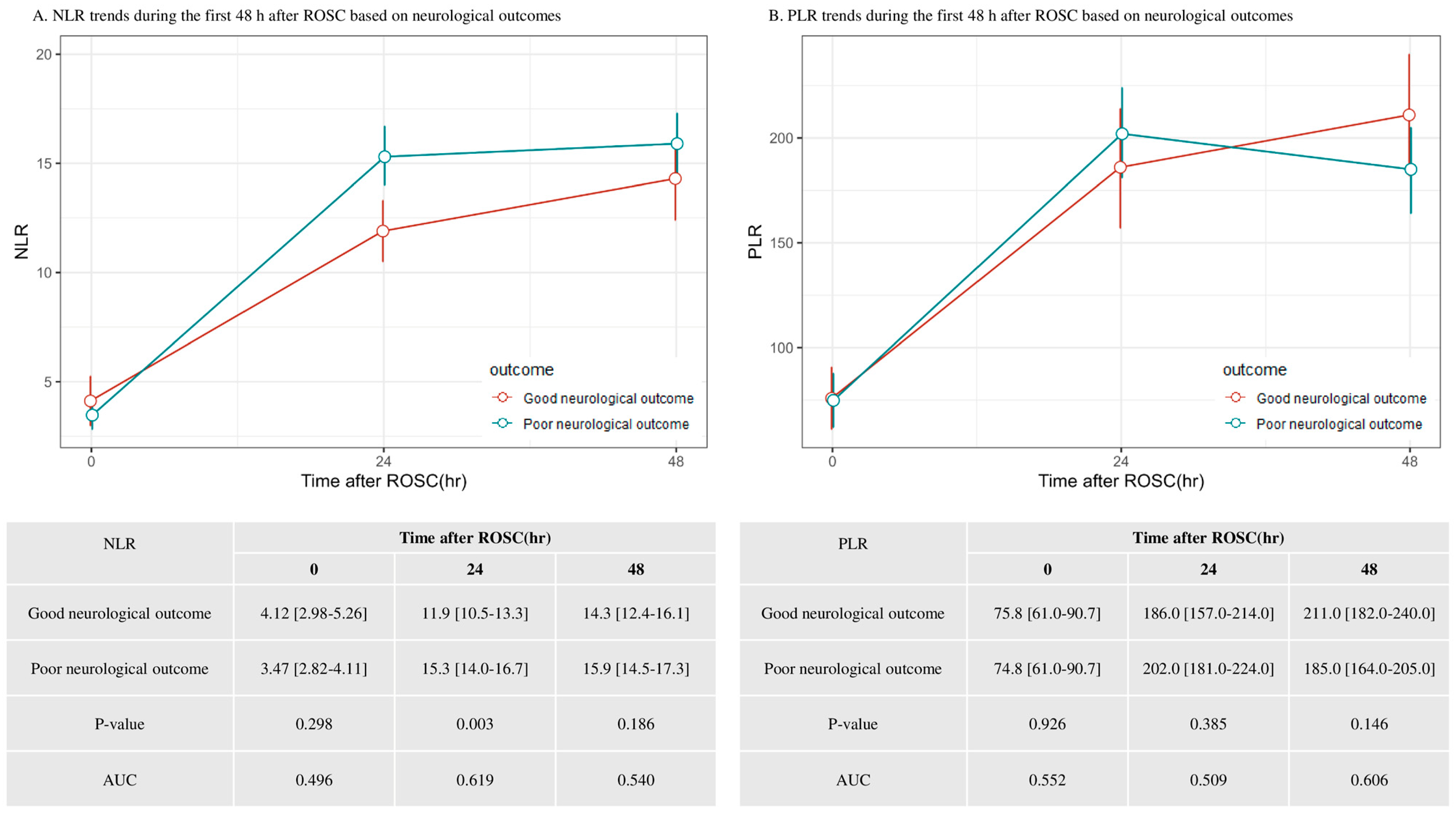
3.3. Trends in the NLR and PLR During the First 48 h After ROSC
3.4. Factors Associated with Poor Neurologic Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-M.; Jeung, K.W.; Kim, W.Y.; Park, Y.S.; Oh, J.S.; You, Y.H.; Lee, D.H.; Chae, M.K.; Jeong, Y.J.; Kim, M.C.; et al. 2020 Korean Guidelines for Cardiopulmonary Resuscitation. Part 5. Post-Cardiac Arrest Care. Clin. Exp. Emerg. Med. 2021, 8, S41–S64. [Google Scholar] [CrossRef]
- Laver, S.; Farrow, C.; Turner, D.; Nolan, J. Mode of Death after Admission to an Intensive Care Unit Following Cardiac Arrest. Intensive Care Med. 2004, 30, 2126–2128. [Google Scholar] [CrossRef] [PubMed]
- Dufner, M.C.; Andre, F.; Stiepak, J.; Zelniker, T.; Chorianopoulos, E.; Preusch, M.; Katus, H.A.; Leuschner, F. Therapeutic Hypothermia Impacts Leukocyte Kinetics after Cardiac Arrest. Cardiovasc. Diagn. Ther. 2016, 6, 199. [Google Scholar] [CrossRef] [PubMed]
- Cotoia, A.; Franchi, F.; De Fazio, C.; Vincent, J.-L.; Creteur, J.; Taccone, F.S. Platelet Indices and Outcome after Cardiac Arrest. BMC Emerg. Med. 2018, 18, 31. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.H.; Lee, W.J.; Kim, D.H.; Cho, Y.; Cho, G.C. Initial Red Cell Distribution Width as a Predictor of Poor Neurological Outcomes in Out-of-Hospital Cardiac Arrest Survivors in a Prospective, Multicenter Observational Study (the KoCARC Study). Sci. Rep. 2020, 10, 17549. [Google Scholar] [CrossRef]
- Cao, C.; Yu, M.; Chai, Y. Pathological Alteration and Therapeutic Implications of Sepsis-Induced Immune Cell Apoptosis. Cell Death Dis. 2019, 10, 782. [Google Scholar] [CrossRef]
- Li, S.; Hu, L.; Wang, J.; Zou, F.; Han, B.; Wang, Y.; Liu, K. Prolonged Increased Neutrophil-to-Lymphocyte Ratio Is Associated with Mortality after Successful Revascularization for Treatment of Acute Ischemic Stroke. BMC Neurol. 2022, 22, 326. [Google Scholar] [CrossRef]
- Fest, J.; Ruiter, T.R.; Groot Koerkamp, B.; Rizopoulos, D.; Ikram, M.A.; van Eijck, C.H.J.; Stricker, B.H. The Neutrophil-to-Lymphocyte Ratio Is Associated with Mortality in the General Population: The Rotterdam Study. Eur. J. Epidemiol. 2019, 34, 463–470. [Google Scholar] [CrossRef]
- White, B.C.; Grossman, L.I.; O’Neil, B.J.; DeGracia, D.J.; Neumar, R.W.; Rafols, J.A.; Krause, G.S. Global Brain Ischemia and Reperfusion. Ann. Emerg. Med. 1996, 27, 588–594. [Google Scholar] [CrossRef]
- Huang, Y.-H.; Lin, Y.-S.; Wu, C.-H.; How, C.-K.; Chen, C.-T. Prognostic Value of Neutrophil-Lymphocyte Ratio in out-of-Hospital Cardiac Arrest Patients Receiving Targeted Temperature Management: An Observational Cohort Study. J. Formos. Med. Assoc. 2023, 122, 890–898. [Google Scholar] [CrossRef] [PubMed]
- Başer, K. Changes in Neutrophil-to-Lymphocyte Ratios in Postcardiac Arrest Patients Treated with Targeted Temperature Management. Anatol. J. Cardiol. 2017, 18, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Tanrikulu, C.S. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Cardiac and Non-Cardiac Arrest Distinction: A Retrospective Cohort Study. Acta Medica 2016, 32, 1617–1623. [Google Scholar] [CrossRef]
- Huang, L.; Peng, J.; Wang, X.; Li, F. High Platelet-Lymphocyte Ratio Is a Risk Factor for 30-Day Mortality In In-Hospital Cardiac Arrest Patients: A Case-Control Study. Expert Rev. Clin. Immunol. 2021, 17, 1231–1239. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, K.N.; Kim, S.H.; Lee, B.K.; Oh, S.H.; Moon, H.K.; Jeung, K.W.; Choi, S.P.; Cho, I.S.; Youn, C.S. Association between the Neutrophil-to-Lymphocyte Ratio and Neurological Outcomes in Patients Undergoing Targeted Temperature Management after Cardiac Arrest. J. Crit. Care 2018, 47, 227–231. [Google Scholar] [CrossRef]
- Wang, D.; Yang, J.-X.; Cao, D.-Y.; Wan, X.-R.; Feng, F.-Z.; Huang, H.-F.; Shen, K.; Xiang, Y. Preoperative Neutrophil-Lymphocyte and Platelet-Lymphocyte Ratios as Independent Predictors of Cervical Stromal Involvement in Surgically Treated Endometrioid Adenocarcinoma. Onco Targets Ther. 2013, 6, 211–216. [Google Scholar] [CrossRef]
- Weiser, C.; Schwameis, M.; Sterz, F.; Herkner, H.; Lang, I.M.; Schwarzinger, I.; Spiel, A.O. Mortality in Patients Resuscitated from Out-of-Hospital Cardiac Arrest Based on Automated Blood Cell Count and Neutrophil Lymphocyte Ratio at Admission. Resuscitation 2017, 116, 49–55. [Google Scholar] [CrossRef]
- Yokoyama, H.; Nagao, K.; Hase, M.; Tahara, Y.; Hazui, H.; Arimoto, H.; Kashiwase, K.; Sawano, H.; Yasuga, Y.; Kuroda, Y.; et al. Impact of Therapeutic Hypothermia in the Treatment of Patients with Out-of-Hospital Cardiac Arrest From the J-PULSE-HYPO Study Registry. Circ. J. 2011, 75, 1063–1070. [Google Scholar] [CrossRef]
- Gando, S.; Wada, T. Disseminated Intravascular Coagulation in Cardiac Arrest and Resuscitation. J. Thromb. Haemost. 2019, 17, 1205–1216. [Google Scholar] [CrossRef]
- Onsrud, M.; Thorsby, E. Influence of in Vivo Hydrocortisone on Some Human Blood Lymphocyte Subpopulations. Scand. J. Immunol. 1981, 13, 573–579. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, J.; Lou, J.; Zhou, Y.; Bo, L.; Zhu, J.; Zhu, K.; Wan, X.; Cai, Z.; Deng, X. Upregulation of Programmed Death-1 on T Cells and Programmed Death Ligand-1 on Monocytes in Septic Shock Patients. Crit. Care 2011, 15, R70. [Google Scholar] [CrossRef] [PubMed]
- Taha Sert, E.; Kokulu, K.; Mutlu, H.; Gül, M.; Uslu, Y. Performance of the Systemic Immune-Inflammation Index in Predicting Survival to Discharge in out-of-Hospital Cardiac Arrest. Resusc. Plus 2023, 14, 100382. [Google Scholar] [CrossRef] [PubMed]
- Balta, S.; Ozturk, C. The Platelet-Lymphocyte Ratio: A Simple, Inexpensive and Rapid Prognostic Marker for Cardiovascular Events. Platelets 2015, 26, 680–681. [Google Scholar] [CrossRef]
- Zhou, X.; Du, Y.; Huang, Z.; Xu, J.; Qiu, T.; Wang, J.; Wang, T.; Zhu, W.; Liu, P. Prognostic Value of PLR in Various Cancers: A Meta-Analysis. PLoS ONE 2014, 9, e101119. [Google Scholar] [CrossRef]
- Kim, Y.J.; Kang, J.; Ryoo, S.M.; Ahn, S.; Huh, J.W.; Kim, W.Y. Platelet-lymphocyte ratio after granulocyte colony stimulating factor administration: An early prognostic marker in septic shock patients with chemotherapy-induced febrile neutropenia. Shock 2019, 52, 160–165. [Google Scholar] [CrossRef]
- Seo, M.; Yamada, T.; Morita, T.; Furukawa, Y.; Tamaki, S.; Iwasaki, Y.; Kawasaki, M.; Kikuchi, A.; Kawai, T.; Ikeda, I.; et al. P589 Prognostic Value of Systemic Immune-Inflammation Index in Patients with Chronic Heart Failure. Eur. Heart J. 2018, 39, 70–71. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, K.N.; Kim, S.H.; Lee, B.K.; Oh, S.H.; Jeung, K.W.; Cho, I.S.; Youn, C.S. Time Course of Platelet Counts in Relation to the Neurologic Outcome in Patients Undergoing Targeted Temperature Management after Cardiac Arrest. Resuscitation 2019, 140, 113–119. [Google Scholar] [CrossRef]
- Böttiger, B.W.; Motsch, J.; Böhrer, H.; Böker, T.; Aulmann, M.; Nawroth, P.P.; Martin, E. Activation of Blood Coagulation After Cardiac Arrest Is Not Balanced Adequately by Activation of Endogenous Fibrinolysis. Circulation 1995, 92, 2572–2578. [Google Scholar] [CrossRef]
- Ames, A.; Wright, R.L.; Kowada, M.; Thurston, J.M.; Majno, G. Cerebral Ischemia. II. The No-Reflow Phenomenon. Am. J. Pathol. 1968, 52, 437–453. [Google Scholar]
- Wada, T. Coagulofibrinolytic Changes in Patients with Post-Cardiac Arrest Syndrome. Front. Med. 2017, 4, 156. [Google Scholar] [CrossRef]
- Nolan, J.P.; Neumar, R.W.; Adrie, C.; Aibiki, M.; Berg, R.A.; Böttiger, B.W.; Callaway, C.; Clark, R.S.B.; Geocadin, R.G.; Jauch, E.C.; et al. Post-Cardiac Arrest Syndrome: Epidemiology, Pathophysiology, Treatment, and Prognostication. A Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation 2008, 79, 350–379. [Google Scholar] [CrossRef] [PubMed]
- Roberts, B.W.; Kilgannon, J.H.; Chansky, M.E.; Mittal, N.; Wooden, J.; Parrillo, J.E.; Trzeciak, S. Multiple Organ Dysfunction after Return of Spontaneous Circulation in Postcardiac Arrest Syndrome. Crit. Care Med. 2013, 41, 1492–1501. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 346) | Good Neurological Outcomes (n = 107) | Poor Neurological Outcomes (n = 239) | p-Value | |
|---|---|---|---|---|
| Age | 58.0 [46.0–69.8] | 52.0 [40.0–61.5] | 60.0 [49.0–73.0] | <0.001 |
| Sex (male) | 242 (69.9%) | 82 (76.6%) | 160 (66.9%) | 0.069 |
| Medical history | ||||
| Hypertension | 119 (34.4%) | 33 (30.8%) | 86 (36.0%) | 0.352 |
| DM | 81 (23.4%) | 15 (14.0%) | 66 (27.6%) | 0.006 |
| Acute coronary syndrome | 57 (16.5%) | 25 (23.4%) | 37 (13.4%) | 0.021 |
| Arrhythmia | 18 (5.2%) | 7 (6.5%) | 11 (4.6%) | 0.453 |
| Heart failure | 11 (3.2%) | 14 (3.7%) | 7 (2.9%) | 0.948 |
| Cerebrovascular disease | 35 (10.1%) | 5 (4.7%) | 30 (12.6%) | 0.040 |
| Chronic renal disease | 32 (9.2%) | 4 (3.7%) | 28 (11.7%) | 0.030 |
| Arrest characteristics | ||||
| Witnessed arrest | 220 (63.6%) | 85 (79.4%) | 135 (56.5%) | <0.001 |
| Bystander CPR | 207 (59.8%) | 72 (67.3%) | 135 (56.5%) | 0.058 |
| Initial shockable rhythm | 120 (34.7%) | 73 (68.2%) | 47 (19.7%) | <0.001 |
| Presumed cardiac cause | 204 (59.0%) | 91 (85.0%) | 113 (47.3%) | <0.001 |
| Prehospital down time, min | 7.0 [4.5–12.0] | 7.0 [5.0–11.0] | 7.0 [4.0–12.0] | 0.190 |
| CPR duration, min | 29.0 [17.0–41.8] | 17.0 [11.0–25.0] | 34.0 [22.0–46.0] | <0.001 |
| Total time to ROSC, min | 38.0 [23.0–55.0] | 28.5 [20.0–36.0] | 43.0 [30.0–58.0] | <0.001 |
| Vital signs | ||||
| Systolic pressure, mmHg | 120.0 [90.0–156.0] | 120.0 [100.0–160.0] | 120.0 [86.0–156.0] | 0.190 |
| Diastolic pressure, mmHg | 70.0 [53.0–90.0] | 78.0 [50.0–89.8] | 69.5 [50.0–89.8] | 0.011 |
| Pulse rate, beats/min | 105.3 ± 29.7 | 101.2 ± 28.1 | 107.0 ± 30.3 | 0.103 |
| Laboratory findings, Initial | ||||
| White blood cell, 103/µL | 12.8 [9.7–17.5] | 13.4 [10.0–17.3] | 12.4 [9.15–17.6] | 0.392 |
| Platelet, 103/µL | 184 [145–234] | 190 [156–247] | 180 [156–228] | 0.095 |
| Total bilirubin, mg/dL | 0.6 [0.4–0.8] | 0.6 [0.4–0.9] | 0.5 [0.3–0.8] | 0.009 |
| Creatinine, mg/dL | 1.30 [1.10–1.70] | 1.20 [1.00–1.10] | 1.35 [1.40–1.90] | <0.001 |
| Lactate, mmol/L | 10.4 [6.3–13.5] | 6.9 [4.5–11.0] | 11.2 [8.0–14.1] | <0.001 |
| Troponin I, ng/dL | 0.06 [0.01–0.30] | 0.06 [0.01–0.20] | 0.06 [0.01–0.40] | 0.998 |
| CRP, mg/dL | 0.14 [0.07–0.60] | 0.12 [0.06–0.50] | 0.17 [0.07–0.90] | 0.179 |
| Total (n = 346) | Good Neurological Outcomes (n = 107) | Poor Neurological Outcomes (n = 239) | p-Value | |
|---|---|---|---|---|
| Adverse events | ||||
| Significant bleeding requiring transfusion | 15 (4.3%) | 5 (4.7%) | 10 (4.2%) | 1.000 |
| Infection requiring antibiotics | 167 (48.3%) | 57 (53.3%) | 110 (46.0%) | 0.258 |
| Re-arrest | 36 (10.4%) | 6 (5.6%) | 30 (12.6%) | 0.057 |
| Intervention | ||||
| Extracorporeal membrane oxygenation | 25 (7.2%) | 10 (9.3%) | 15 (6.3%) | 0.427 |
| Coronary angiography | 148 (42.8%) | 75 (70.1%) | 73 (30.5%) | <0.001 |
| Percutaneous coronary intervention | 64 (18.5%) | 33 (30.8%) | 31 (13.0%) | <0.001 |
| Univariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| NLR at 24 h | 1.02 | 1.01–1.03 | 0.002 | 1.01 | 1.00–1.03 | 0.045 |
| Age | 1.02 | 1.01–1.02 | <0.001 | 1.01 | 1.01–1.02 | 0.001 |
| Sex (female) | 1.27 | 0.96–1.66 | 0.092 | 1.12 | 0.84–1.48 | 0.442 |
| Unwitnessed cardiac arrest | 1.67 | 1.28–2.17 | <0.001 | 0.98 | 0.74–1.32 | 0.918 |
| Non-shockable rhythm | 3.66 | 2.61–5.14 | <0.001 | 2.70 | 1.81–4.02 | <0.001 |
| Bystander CPR | 1.34 | 1.03–1.74 | 0.027 | 0.95 | 0.72–1.25 | 0.694 |
| Presumed cardiac cause | 2.36 | 1.82–3.07 | <0.001 | 1.24 | 0.91–1.70 | 0.177 |
| Total time to ROSC | 1.02 | 1.01–1.02 | <0.001 | 1.01 | 1.01–1.02 | <0.001 |
| Lactate | 1.05 | 1.03–1.07 | <0.001 | 1.05 | 1.02–1.07 | <0.001 |
| Cut Off | Sens | Spec | PPV | NPV | |
|---|---|---|---|---|---|
| NLR at 24 h | 9 | 72.5% | 47.7% | 75% | 44.4% |
| 1.07 | 99.2% | 0.1% | 68.8% | 0% | |
| 34.6 | 0.1% | 99.1% | 92.3% | 31.7% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.; Park, H.; Kim, S.-M.; Kim, W.Y. Optimal Timing of the Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Early Predictors of Neurological Outcomes in Postcardiac Arrest Patients. Life 2024, 14, 1421. https://doi.org/10.3390/life14111421
Kim D, Park H, Kim S-M, Kim WY. Optimal Timing of the Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Early Predictors of Neurological Outcomes in Postcardiac Arrest Patients. Life. 2024; 14(11):1421. https://doi.org/10.3390/life14111421
Chicago/Turabian StyleKim, Dongju, Hanna Park, Sang-Min Kim, and Won Young Kim. 2024. "Optimal Timing of the Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Early Predictors of Neurological Outcomes in Postcardiac Arrest Patients" Life 14, no. 11: 1421. https://doi.org/10.3390/life14111421
APA StyleKim, D., Park, H., Kim, S.-M., & Kim, W. Y. (2024). Optimal Timing of the Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Early Predictors of Neurological Outcomes in Postcardiac Arrest Patients. Life, 14(11), 1421. https://doi.org/10.3390/life14111421






