Influence of Body Mass Index and Duration of Disease on Chromosome Damage in Lymphocytes of Patients with Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Cytogenetic Procedures
2.3. Statistical Analysis
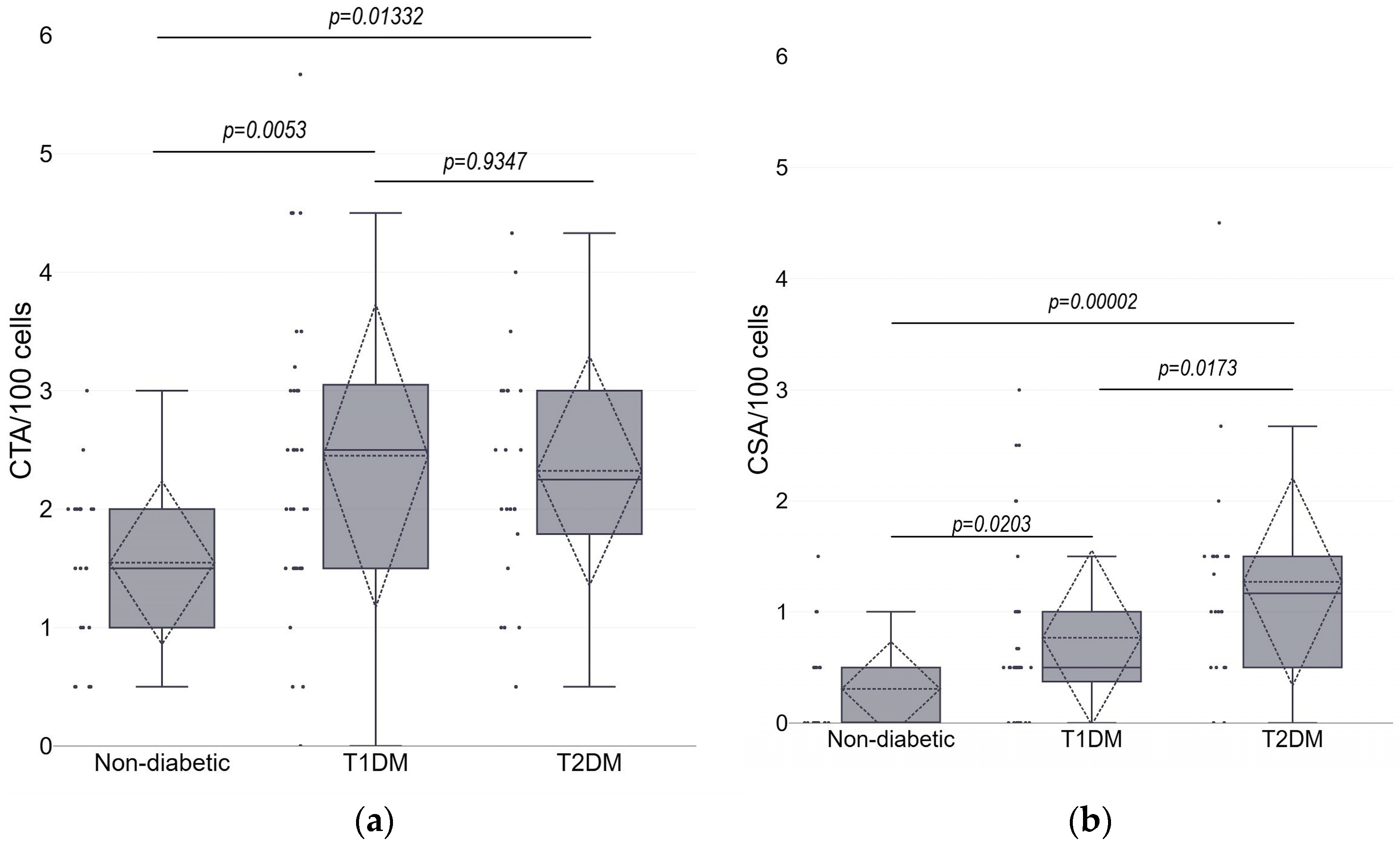
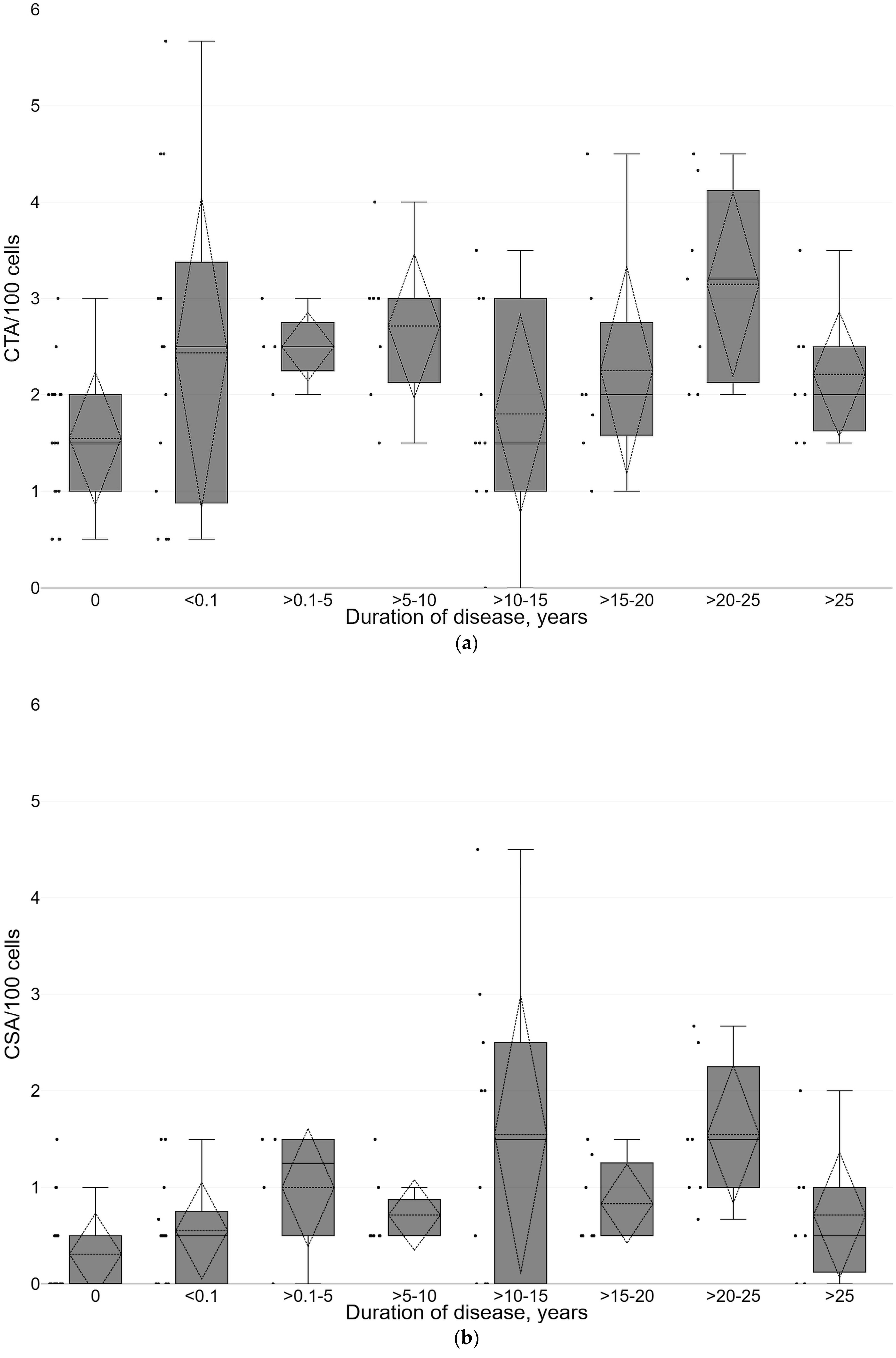
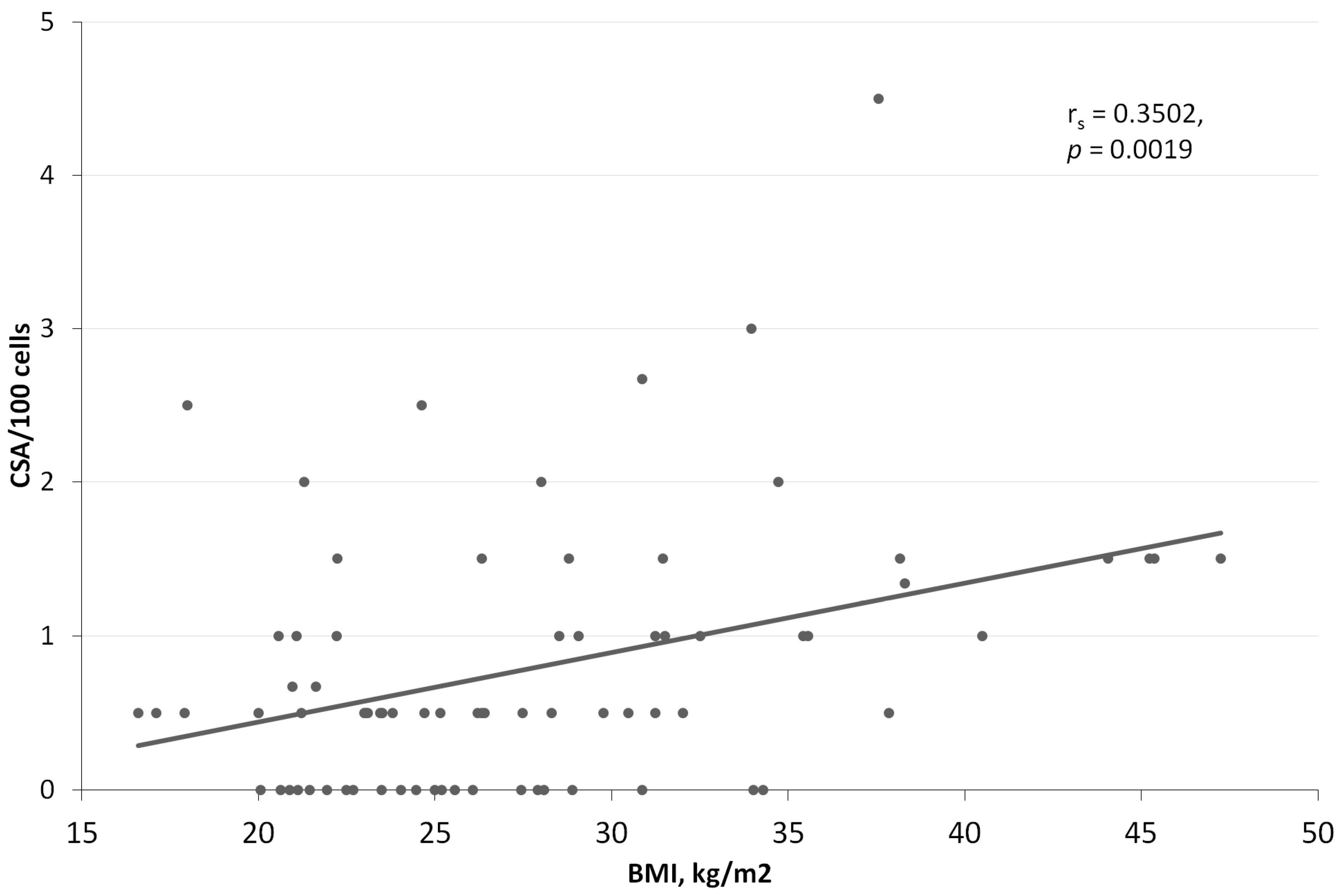
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- World Health Organization. International Diabetes Federation Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: Report of a WHO/IDF Consultation; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- What Is Diabetes? Available online: https://www.cdc.gov/diabetes/basics/diabetes.html (accessed on 27 June 2023).
- IDF Diabetes Atlas 10th Edition. Available online: https://diabetesatlas.org/data/ (accessed on 27 June 2023).
- Niedowicz, D.M.; Daleke, D.L. The Role of Oxidative Stress in Diabetic Complications. Cell Biochem. Biophys. 2005, 43, 289–330. [Google Scholar] [CrossRef]
- Masenga, S.K.; Kabwe, L.S.; Chakulya, M.; Kirabo, A. Mechanisms of Oxidative Stress in Metabolic Syndrome. Int. J. Mol. Sci. 2023, 24, 7898. [Google Scholar] [CrossRef]
- Bonagiri, P.R.; Shubrook, J.H. Review of Associations Between Type 2 Diabetes and Cancer. Clin. Diabetes 2020, 38, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Giovannucci, E.; Harlan, D.M.; Archer, M.C.; Bergenstal, R.M.; Gapstur, S.M.; Habel, L.A.; Pollak, M.; Regensteiner, J.G.; Yee, D. Diabetes and Cancer. Diabetes Care 2010, 33, 1674–1685. [Google Scholar] [CrossRef] [PubMed]
- Shahid, R.K.; Ahmed, S.; Le, D.; Yadav, S. Diabetes and Cancer: Risk, Challenges, Management and Outcomes. Cancers 2021, 13, 5735. [Google Scholar] [CrossRef] [PubMed]
- Sciacca, L.; Vigneri, R.; Tumminia, A.; Frasca, F.; Squatrito, S.; Frittitta, L.; Vigneri, P. Clinical and Molecular Mechanisms Favoring Cancer Initiation and Progression in Diabetic Patients. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 808–815. [Google Scholar] [CrossRef]
- Kay, J.; Thadhani, E.; Samson, L.; Engelward, B. Inflammation-Induced DNA Damage, Mutations and Cancer. DNA Repair 2019, 83, 102673. [Google Scholar] [CrossRef]
- Obe, G.; Pfeiffer, P.; Savage, J.R.K.; Johannes, C.; Goedecke, W.; Jeppesen, P.; Natarajan, A.T.; Martínez-López, W.; Folle, G.A.; Drets, M.E. Chromosomal Aberrations: Formation, Identification and Distribution. Mutat. Res. 2002, 504, 17–36. [Google Scholar] [CrossRef]
- Limoli, C.L.; Giedzinski, E. Induction of Chromosomal Instability by Chronic Oxidative Stress. Neoplasia 2003, 5, 339–346. [Google Scholar] [CrossRef]
- Norppa, H.; Bonassi, S.; Hansteen, I.-L.; Hagmar, L.; Strömberg, U.; Rössner, P.; Boffetta, P.; Lindholm, C.; Gundy, S.; Lazutka, J.; et al. Chromosomal Aberrations and SCEs as Biomarkers of Cancer Risk. Mutat. Res. 2006, 600, 37–45. [Google Scholar] [CrossRef]
- Boffetta, P.; van der Hel, O.; Norppa, H.; Fabianova, E.; Fucic, A.; Gundy, S.; Lazutka, J.; Cebulska-Wasilewska, A.; Puskailerova, D.; Znaor, A.; et al. Chromosomal Aberrations and Cancer Risk: Results of a Cohort Study from Central Europe. Am. J. Epidemiol. 2007, 165, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Shaw, J.F.; Kansal, P.C.; Gatti, R.A. Letter: Diabetes Mellitus, Chromosomal Aberration, and Malignancy. Lancet 1976, 2, 315. [Google Scholar] [CrossRef]
- Vormittag, W. Structural Chromosomal Aberration Rates and Sister-Chromatid Exchange Frequencies in Females with Type 2 (Non-Insulin-Dependent) Diabetes. Mutat. Res. 1985, 143, 117–119. [Google Scholar] [CrossRef] [PubMed]
- Deo, P.; Fenech, M.; Dhillon, V.S. Association between Glycation Biomarkers, Hyperglycemia, and Micronucleus Frequency: A Meta -Analysis. Mutat. Res./Rev. Mutat. Res. 2021, 787, 108369. [Google Scholar] [CrossRef] [PubMed]
- Eremina, N.V.; Zhanataev, A.K.; Lisitsyn, A.A.; Durnev, A.D. Genotoxic markers in patients with diabetes mellitus (Literature review). Ecol. Genet. 2021, 19, 143–168. [Google Scholar] [CrossRef]
- Milic, M.; Frustaci, A.; Del Bufalo, A.; Sánchez-Alarcón, J.; Valencia-Quintana, R.; Russo, P.; Bonassi, S. DNA Damage in Non-Communicable Diseases: A Clinical and Epidemiological Perspective. Mutat. Res. 2015, 776, 118–127. [Google Scholar] [CrossRef]
- Diagnostic Criteria for Diabetes. Available online: https://www.diabetes.org.uk/professionals/position-statements-reports/diagnosis-ongoing-management-monitoring/new_diagnostic_criteria_for_diabetes (accessed on 25 June 2023).
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice: Developed by the Task Force for Cardiovascular Disease Prevention in Clinical Practice with Representatives of the European Society of Cardiology and 12 Medical Societies With the Special Contribution of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Young, M.J.; Boulton, A.J.M.; Macleod, A.F.; Williams, D.R.R.; Sonksen, P.H. A Multicentre Study of the Prevalence of Diabetic Peripheral Neuropathy in the United Kingdom Hospital Clinic Population. Diabetologia 1993, 36, 150–154. [Google Scholar] [CrossRef]
- Spallone, V.; Bellavere, F.; Scionti, L.; Maule, S.; Quadri, R.; Bax, G.; Melga, P.; Viviani, G.L.; Esposito, K.; Morganti, R.; et al. Recommendations for the Use of Cardiovascular Tests in Diagnosing Diabetic Autonomic Neuropathy. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 69–78. [Google Scholar] [CrossRef]
- Whorton, E.B. Some Experimental Design and Analysis Considerations for Cytogenetics Studies. Environ. Mutagen. 1985, 7 (Suppl. 4), 9–15. [Google Scholar] [CrossRef]
- Statistics Online—Checks Assumptions, Interprets Results. Available online: https://www.statskingdom.com/ (accessed on 19 July 2023).
- Lazutka, J.R.; Lekevicius, R.; Dedonyte, V.; Maciuleviciute-Gervers, L.; Mierauskiene, J.; Rudaitiene, S.; Slapsyte, G. Chromosomal Aberrations and Sister-Chromatid Exchanges in Lithuanian Populations: Effects of Occupational and Environmental Exposures. Mutat. Res. 1999, 445, 225–239. [Google Scholar] [CrossRef] [PubMed]
- Lazutka, J.R. Chromosome Aberrations and Rogue Cells in Lymphocytes of Chernobyl Clean-up Workers. Mutat. Res. 1996, 350, 315–329. [Google Scholar] [CrossRef] [PubMed]
- Pappuswamy, M.; Rajesh, N.; Philip, A.M. Analysis of Chromosomal Aberrations and Micronuclei in Type 2 Diabetes Mellitus Patients. Asian Pac. J. Cancer Biol. 2020, 5, 15–18. [Google Scholar] [CrossRef]
- Boehm, B.O.; Möller, P.; Högel, J.; Winkelmann, B.R.; Renner, W.; Rosinger, S.; Seelhorst, U.; Wellnitz, B.; März, W.; Melzner, J.; et al. Lymphocytes of Type 2 Diabetic Women Carry a High Load of Stable Chromosomal Aberrations: A Novel Risk Factor for Disease-Related Early Death. Diabetes 2008, 57, 2950–2957. [Google Scholar] [CrossRef]
- Saraswathy, R.; Anand, S.; Kunnumpurath, S.K.; Kurian, R.J.; Kaye, A.D.; Vadivelu, N. Chromosomal Aberrations and Exon 1 Mutation in the AKR1B1 Gene in Patients with Diabetic Neuropathy. Ochsner J. 2014, 14, 339–342. [Google Scholar]
- Anand, S.; Nath, B.; Saraswathy, R. Diabetes—Increased Risk for Cancers through Chromosomal Aberrations? Asian Pac. J. Cancer Prev. 2014, 15, 4571–4573. [Google Scholar] [CrossRef]
- Cinkilic, N.; Kiyici, S.; Celikler, S.; Vatan, O.; Oz Gul, O.; Tuncel, E.; Bilaloglu, R. Evaluation of Chromosome Aberrations, Sister Chromatid Exchange and Micronuclei in Patients with Type-1 Diabetes Mellitus. Mutat. Res. 2009, 676, 1–4. [Google Scholar] [CrossRef]
- Salimi, M.; Broumand, B.; Mozdarani, H. Association of Elevated Frequency of Micronuclei in Peripheral Blood Lymphocytes of Type 2 Diabetes Patients with Nephropathy Complications. Mutagenesis 2016, 31, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Prasad, M.; Bronson, S.C.; Warrier, T.; Badarinath, A.; Rai, S.; Baid, K.; Sitaraman, S.; George, A.; Moses, A.; Saraswathy, R.; et al. Evaluation of DNA Damage in Type 2 Diabetes Mellitus Patients with and without Peripheral Neuropathy: A Study in South Indian Population. J. Nat. Sci. Biol. Med. 2015, 6, 80–84. [Google Scholar] [CrossRef]
- Quintero Ojeda, J.E.; Aguilar-Medina, M.; Olimón-Andalón, V.; García Jau, R.A.; Ayala Ham, A.; Romero Quintana, J.G.; Silva-Benítez, E.d.L.; Sanchez-Schmitz, G.; Ramos-Payán, R. Increased Micronuclei Frequency in Oral and Lingual Epithelium of Treated Diabetes Mellitus Patients. Biomed. Res. Int. 2018, 2018, 4898153. [Google Scholar] [CrossRef]
- Binici, D.N.; Karaman, A.; Coşkun, M.; Oğlu, A.U.; Uçar, F. Genomic Damage in Patients with Type-2 Diabetes Mellitus. Genet. Couns. 2013, 24, 149–156. [Google Scholar] [PubMed]
- Palazzo, R.P.; Bagatini, P.B.; Schefer, P.B.; de Andrade, F.M.; Maluf, S.W. Genomic Instability in Patients with Type 2 Diabetes Mellitus on Hemodialysis. Rev. Bras. Hematol. E Hemoter. 2012, 34, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Witczak, M.; Ferenc, T.; Gulczyńska, E.; Nowakowska, D.; Łopaczyńska, D.; Wilczyński, J. Elevated Frequencies of Micronuclei in Pregnant Women with Type 1 Diabetes Mellitus and in Their Newborns. Mutat. Res./Genet. Toxicol. Environ. Mutagen. 2014, 763, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Włodarczyk, M.; Nowicka, G. Obesity, DNA Damage, and Development of Obesity-Related Diseases. Int. J. Mol. Sci. 2019, 20, 1146. [Google Scholar] [CrossRef] [PubMed]
- Petrie, J.R.; Guzik, T.J.; Touyz, R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2018, 34, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.K.; Sindhu, K.K. Oxidative Stress and Metabolic Syndrome. Life Sci. 2009, 84, 705–712. [Google Scholar] [CrossRef]
- Donmez-Altuntas, H.; Sahin, F.; Bayram, F.; Bitgen, N.; Mert, M.; Guclu, K.; Hamurcu, Z.; Arıbas, S.; Gundogan, K.; Diri, H. Evaluation of Chromosomal Damage, Cytostasis, Cytotoxicity, Oxidative DNA Damage and Their Association with Body-Mass Index in Obese Subjects. Mutat. Res./Genet. Toxicol. Environ. Mutagen. 2014, 771, 30–36. [Google Scholar] [CrossRef]
- Karaman, A.; Aydın, H.; Geçkinli, B.; Çetinkaya, A.; Karaman, S. DNA Damage Is Increased in Lymphocytes of Patients with Metabolic Syndrome. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2015, 782, 30–35. [Google Scholar] [CrossRef]
- Corbi, S.C.T.; Bastos, A.S.; Orrico, S.R.P.; Secolin, R.; Dos Santos, R.A.; Takahashi, C.S.; Scarel-Caminaga, R.M. Elevated Micronucleus Frequency in Patients with Type 2 Diabetes, Dyslipidemia and Periodontitis. Mutagenesis 2014, 29, 433–439. [Google Scholar] [CrossRef]
- Tyson, J.; Caple, F.; Spiers, A.; Burtle, B.; Daly, A.K.; Williams, E.A.; Hesketh, J.E.; Mathers, J.C. Inter-Individual Variation in Nucleotide Excision Repair in Young Adults: Effects of Age, Adiposity, Micronutrient Supplementation and Genotype. Br. J. Nutr. 2009, 101, 1316–1323. [Google Scholar] [CrossRef]
- Crespo-Orta, I.; Ortiz, C.; Encarnación, J.; Suárez, E.; Matta, J. Association between DNA Repair Capacity and Body Mass Index in Women. Mutat. Res. 2023, 826, 111813. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Bai, Y.; Wang, S.; Nyamathira, S.M.; Zhang, X.; Zhang, W.; Wang, T.; Deng, Q.; He, M.; Zhang, X.; et al. Association of Body Mass Index with Chromosome Damage Levels and Lung Cancer Risk among Males. Sci. Rep. 2015, 5, 9458. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Manfredini, V.; Biancini, G.B.; Vanzin, C.S.; Dal Vesco, A.M.R.; Cipriani, F.; Biasi, L.; Treméa, R.; Deon, M.; Peralba, M.d.C.R.; Wajner, M.; et al. Simvastatin Treatment Prevents Oxidative Damage to DNA in Whole Blood Leukocytes of Dyslipidemic Type 2 Diabetic Patients. Cell Biochem. Funct. 2010, 28, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Tubić Vukajlović, J.; Simić, I.; Smiljanić, Z.; Grujičić, D.; Milošević-Djordjević, O. Genome Instability in Peripheral Blood Lymphocytes of Patients with Heart Failure and Reduced Ejection Fraction. Mutagenesis 2023, 38, 84–92. [Google Scholar] [CrossRef]
- Pernice, F.; Floccari, F.; Caccamo, C.; Belghity, N.; Mantuano, S.; Pacilè, M.E.; Romeo, A.; Nostro, L.; Barillà, A.; Crascì, E.; et al. Chromosomal Damage and Atherosclerosis. A Protective Effect from Simvastatin. Eur. J. Pharmacol. 2006, 532, 223–229. [Google Scholar] [CrossRef]
- Orsolin, P.C.; Silva-Oliveira, R.G.; Nepomuceno, J.C. Modulating Effect of Synthetic Statins against Damage Induced by Doxorubicin in Somatic Cells of Drosophila Melanogaster. Food Chem. Toxicol. 2015, 81, 111–119. [Google Scholar] [CrossRef]
- Orsolin, P.C.; Silva-Oliveira, R.G.; Nepomuceno, J.C. Modulating Effect of Simvastatin on the DNA Damage Induced by Doxorubicin in Somatic Cells of Drosophila Melanogaster. Food Chem. Toxicol. 2016, 90, 10–17. [Google Scholar] [CrossRef]

| Variable | Diabetes | Controls | p Values | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type 1 | Type 2 | Type 1 vs. Type 2 | Type 1 vs. Controls | Type 2 vs. Controls | ||||||
| N | % | N | % | N | % | |||||
| Demographic data | ||||||||||
| Sex | Female Male | 13 20 | 39.4 60.6 | 13 9 | 59.1 40.9 | 17 4 | 81.0 19.0 | 0.152 | 0.003 | 0.119 |
| Smoking | Nonsmoker Former/Current smoker | 15 18 | 45.5 54.5 | 16 6 | 72.7 27.3 | 15 6 | 71.4 28.6 | 0.046 | 0.061 | 0.924 |
| Age in years, mean (SD) | 39.8 (15.4) | 61.8 (14.1) | 38.1 (13.6) | 0.000 | 0.809 | 0.000 | ||||
| BMI, kg/m2, mean (SD) | 23.6 (3.7) | 35.5 (6.1) | 25.9 (4.6) | 0.000 | 0.181 | 0.000 | ||||
| Diabetes and complications | ||||||||||
| Time after diagnosis in years, mean (SD) | 13.5 (13.3) | 12.9 (7.7) | 0.672 | |||||||
| Family history of diabetes | No Yes | 19 14 | 57.6 42.4 | 5 17 | 22.7 77.3 | 15 6 | 71.4 28.6 | 0.011 | 0.304 | 0.001 |
| Nephropathy | No Yes | 26 7 | 78.8 21.2 | 18 4 | 81.8 18.2 | 0.783 | ||||
| Polyneuropathy | No Yes | 22 11 | 66.7 33.3 | 10 12 | 45.5 54.5 | 0.118 | ||||
| Autonomic heart neuropathy | No Probable Yes ND | 21 6 4 2 | 63.6 18.2 12.1 6.1 | 9 11 1 1 | 40.9 50.0 4.5 4.5 | 0.091 | ||||
| Concomitant diseases | ||||||||||
| Ischemic heart disease | No Yes | 31 2 | 93.9 6.1 | 14 8 | 63.6 36.4 | 21 0 | 100.0 0.0 | 0.004 | 0.250 | 0.002 |
| Arterial hypertension | No Yes | 20 13 | 60.6 39.4 | 2 20 | 9.1 90.9 | 19 2 | 90.5 9.5 | 0.000 | 0.017 | 0.000 |
| Dyslipidemia | No Yes | 16 17 | 48.5 51.5 | 3 19 | 13.6 86.4 | 19 2 | 90.5 9.5 | 0.008 | 0.002 | 0.000 |
| Thyroid diseases (excl. cancer) | No Yes | 24 9 | 72.7 27.3 | 13 9 | 59.1 40.9 | 16 5 | 76.2 23.8 | 0.291 | 0.777 | 0.232 |
| Use of prescribed medications | ||||||||||
| Insulin | No Yes | 7 26 | 21.2 78.8 | 7 15 | 31.8 68.2 | 0.376 | ||||
| Metformin | No Yes | 4 18 | 18.2 81.8 | |||||||
| Statins | No Yes | 23 10 | 69.7 30.3 | 12 10 | 54.5 45.5 | 19 2 | 90.5 9.5 | 0.252 | 0.073 | 0.009 |
| Antihypertensive drugs | No Yes | 20 13 | 60.6 39.4 | 2 20 | 9.1 90.9 | 19 2 | 90.5 9.5 | 0.000 | 0.017 | 0.000 |
| Groups | Aberrations per 100 Cells * | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CTB | CTE | CSB | CSE | Total CA | |||||||||||
| Mean | SD | Min–Max | Mean | SD | Min–Max | Mean | SD | Min–Max | Mean | SD | Min–Max | Mean | SD | Min–Max | |
| Non-diabetic | 1.48 | 0.68 | 0.50–3.00 | 0.07 | 0.18 | 0.00–0.50 | 0.21 | 0.29 | 0.00–1.00 | 0.10 | 0.22 | 0.00–0.67 | 1.83 | 0.90 | 0.50–4.00 |
| T1DM | 2.38 | 1.26 | 0.00–5.33 | 0.08 | 0.18 | 0.00–0.50 | 0.39 | 0.53 | 0.00–2.00 | 0.37 | 0.51 | 0.00–2.00 | 3.13 | 1.47 | 1.00–6.00 |
| T2DM | 2.26 | 0.93 | 0.50–4.00 | 0.06 | 0.16 | 0.00–0.50 | 0.80 | 0.53 | 0.00–2.00 | 0.47 | 0.65 | 0.00–2.50 | 3.60 | 1.47 | 1.00–7.50 |
| p-value ** | 0.0059 | 0.8981 | 0.0002 | 0.0503 | 0.0002 | ||||||||||
| Variables * | Diabetes | Controls | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type 1 | Type 2 | |||||||||
| CTA (SD) | CSA (SD) | CA (SD) | CTA (SD) | CSA (SD) | CA (SD) | CTA (SD) | CSA (SD) | CA (SD) | ||
| Sex | Female Male | 2.32 (1.28) 2.53 (1.34) | 0.97 (0.98) 0.63 (0.65) | 3.21 (1.54) 3.08 (1.45) | 2.41 (1.05) 2.20 (0.95) | 1.13 (0.77) 1.48 (1.20) | 3.54 (1.65) 3.68 (1.27) | 1.56 (0.75) 1.50 (0.58) | 0.24 (0.36) 0.63 (0.63) | 1.76 (0.87) 2.13 (1.11) |
| Smoking | NS CS/FS | 2.45 (1.12) 2.45 (1.47) | 0.84 (0.88) 0.70 (0.75) | 3.28 (1.68) 3.01 (1.30) | 2.35 (0.96) 2.25 (1.17) | 1.13 (0.69) 1.67 (1.47) | 3.48 (1.47) 3.92 (1.56) | 1.73 (0.62) 1.08 (0.74) | 0.37 (0.48) 0.17 (0.26) | 2.07 (0.84) 1.25 (0.82) |
| Thyroid diseases | No Yes | 2.49 (1.42) 2.36 (0.99) | 0.76 (0.83) 0.80 (0.75) | 3.13 (1.55) 3.13 (1.29) | 2.39 (1.17) 2.22 (0.71) | 1.50 (1.08) 0.94 (0.68) | 3.89 (1.58) 3.17 (1.27) | 1.50 (0.55) 1.70 (1.15) | 0.25 (0.41) 0.50 (0.50) | 1.72 (0.82) 2.20 (1.15) |
| Family history of DM | No Yes | 2.37 (1.23) 2.56 (1.43) | 0.95 (0.98) 0.52 (0.35) | 3.21 (1.54) 3.02 (1.41) | 2.32 (1.43) 2.32 (0.88) | 1.40 (0.81) 1.24 (1.02) | 3.73 (1.98) 3.56 (1.37) | 1.70 (0.68) 1.17 (0.68) | 0.27 (0.46) 0.42 (0.38) | 1.97 (0.90) 1.50 (0.89) |
| AH | No Yes | 2.61 (1.59) 2.21 (0.65) | 0.78 (0.86) 0.74 (0.72) | 3.26 (1.68) 2.94 (1.09) | 2.50 (0.71) 2.31 (1.03) | 1.00 (0.71) 1.30 (0.99) | 3.50 (1.41) 3.61 (1.52) | 1.55 (0.66) 1.50 (1.41) | 0.32 (0.45) 0.25 (0.35) | 1.84 (0.91) 1.75 (1.06) |
| Dyslipidemia | No Yes | 2.79 (1.60) 2.13 (0.87) | 0.82 (0.96) 0.72 (0.64) | 3.45 (1.73) 2.83 (1.14) | 1.93 (0.12) 2.39 (1.01) | 1.11 (0.54) 1.30 (1.02) | 3.04 (0.51) 3.68 (1.57) | 1.55 (0.66) 1.50 (1.41) | 0.32 (0.45) 0.25 (0.35) | 1.84 (0.91) 1.75 (1.06) |
| IHD | No Yes | 2.48 (1.33) 2.00 (0.71) | 0.74 (0.79) 1.25 (1.06) | 3.14 (1.46) 3.00 (2.12) | 2.27 (0.92) 2.42 (1.17) | 0.99 (0.61) 1.77 (1.27) | 3.26 (1.29) 4.19 (1.67) | N.A. | N.A. | N.A. |
| Nephropathy | No Yes | 2.51 (1.42) 2.21 (0.76) | 0.83 (0.87) 0.52 (0.41) | 3.24 (1.56) 2.74 (1.03) | 2.41 (1.03) 1.95 (0.82) | 1.12 (0.70) 1.96 (1.70) | 3.53 (1.56) 3.91 (1.15) | N.A. | N.A. | N.A. |
| PNP | No Yes | 2.64 (1.52) 2.06 (0.56) | 0.80 (0.84) 0.70 (0.75) | 3.33 (1.62) 2.74 (1.06) | 2.56 (1.11) 2.13 (0.88) | 1.30 (0.62) 1.25 (1.20) | 3.86 (1.50) 3.38 (1.48) | N.A. | N.A. | N.A. |
| CAN | No Yes MD | 2.54 (1.47) 2.35 (1.06) 2.00 (0.71) | 0.87 (0.91) 0.47 (0.38) 1.25 (1.06) | 3.30 (1.57) 2.82 (1.20) 3.00 (2.12) | 2.06 (0.98) 2.64 (0.92) 1.00 | 1.39 (1.27) 1.25 (0.72) 0.50 | 3.44 (1.33) 3.89 (1.53) 1.50 | N.A. | N.A. | N.A. |
| Insulin | No Yes | 2.52 (1.89) 2.43 (1.14) | 0.38 (0.39) 0.87 (0.85) | 2.74 (1.70) 3.24 (1.41) | 2.50 (1.08) 2.24 (0.98) | 1.29 (0.57) 1.27 (1.11) | 3.79 (1.32) 3.51 (1.58) | N.A. | N.A. | N.A. |
| Metformin | No Yes | N.A. | N.A. | N.A. | 2.13 (1.18) 2.37 (0.98) | 1.38 (0.25) 1.25 (1.06) | 3.50 (1.08) 3.62 (1.57) | N.A. | N.A. | N.A. |
| Statins | No Yes | 2.66 (1.44) 1.97 (0.76) | 0.88 (0.85) 0.52 (0.63) | 3.40 (1.53) 2.52 (1.16) | 2.47 (1.15) 2.15 (0.78) | 1.21 (0.65) 1.35 (1.27) | 3.68 (1.60) 3.50 (1.39) | 1.55 (0.66) 1.50 (1.41) | 0.32 (0.45) 0.25 (0.35) | 1.84 (0.91) 1.75 (1.06) |
| Antihypertensive drugs | No Yes | 2.56 (1.59) 2.28 (0.69) | 0.83 (0.88) 0.67 (0.69) | 3.26 (1.68) 2.94 (1.09) | 2.50 (0.71) 2.31 (1.03) | 1.00 (0.71) 1.30 (0.99) | 3.50 (1.41) 3.61 (1.52) | 1.55 (0.66) 1.50 (1.41) | 0.32 (0.45) 0.25 (0.35) | 1.84 (0.91) 1.75 (1.06) |
| Variables | Chromatid-Type Aberrations (CTA) | Chromosome-Type Aberrations (CSA) | Total Aberrations (CA) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression Coefficient | Standard Error | p | Regression Coefficient | Standard Error | p | Regression Coefficient | Standard Error | p | |
| Intercept | 1.7372 | 0.5614 | 0.0028 | −1.8857 | 0.5963 | 0.0023 | 0.7105 | 0.5762 | 0.2216 |
| BMI | −0.0882 | 0.1723 | 0.6104 | 0.4810 | 0.1831 | 0.0105 | 0.2608 | 0.1769 | 0.1448 |
| Duration of disease | 0.1654 | 0.0560 | 0.0042 | 0.26348 | 0.0595 | 0.00003 | 0.2609 | 0.0575 | 0.00002 |
| Use of statins | −0.1947 | 0.1372 | 0.1604 | −0.26218 | 0.145782 | 0.0763 | −0.2421 | 0.1409 | 0.0899 |
| Model properties | |||||||||
| Model * | CTAt = 1.737191 − 0.0882006 Ln(BMI) + 0.165427 Ln(Duration of disease) − 0.19466 Ln(Use of statins) | CSAt = 0.15173 × (BMI)0.480953 × (Duration of disease)0.26338 × (Use of statins)−0.26218 | CAt = 0.710502 + 0.260791 Ln(BMI) + 0.260852 Ln(Duration of disease) − 0.24212 Ln(Use of statins) | ||||||
| R-square | 0.1106 | 0.2950 | 0.2576 | ||||||
| Coefficient of multiple correlation | 0.3326 | 0.5432 | 0.5076 | ||||||
| Goodness of fit | F(3,72) = 2.9855, p = 0.0367 | F(3,72) = 10.0445, p = 0.00001 | F(3,72) = 8.3290, p = 0.00008 | ||||||
| Residual normality (Shapiro–Wilk test) | p = 0.4076 | p = 0.1005 | p = 0.6373 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šiaulienė, L.; Kazlauskaitė, J.; Jurkėnaitė, D.; Visockienė, Ž.; Lazutka, J.R. Influence of Body Mass Index and Duration of Disease on Chromosome Damage in Lymphocytes of Patients with Diabetes. Life 2023, 13, 1926. https://doi.org/10.3390/life13091926
Šiaulienė L, Kazlauskaitė J, Jurkėnaitė D, Visockienė Ž, Lazutka JR. Influence of Body Mass Index and Duration of Disease on Chromosome Damage in Lymphocytes of Patients with Diabetes. Life. 2023; 13(9):1926. https://doi.org/10.3390/life13091926
Chicago/Turabian StyleŠiaulienė, Laura, Jūratė Kazlauskaitė, Dalia Jurkėnaitė, Žydrūnė Visockienė, and Juozas R. Lazutka. 2023. "Influence of Body Mass Index and Duration of Disease on Chromosome Damage in Lymphocytes of Patients with Diabetes" Life 13, no. 9: 1926. https://doi.org/10.3390/life13091926
APA StyleŠiaulienė, L., Kazlauskaitė, J., Jurkėnaitė, D., Visockienė, Ž., & Lazutka, J. R. (2023). Influence of Body Mass Index and Duration of Disease on Chromosome Damage in Lymphocytes of Patients with Diabetes. Life, 13(9), 1926. https://doi.org/10.3390/life13091926







