Pediatric Obesity: Complications and Current Day Management
Abstract
1. Introduction
2. Definitions and Classification
3. Complications of Pediatric Obesity
3.1. Type 2 Diabetes and Prediabetes
3.2. Dyslipidemia
3.3. Hypertension
3.4. Non-Alcoholic Fatty Liver Disease
3.5. Obstructive Sleep Apnea
3.6. Polycystic Ovary Syndrome
3.7. Weight Stigma, Depression, and Quality of Life
4. Management of Pediatric Obesity
4.1. Lifestyle Interventions
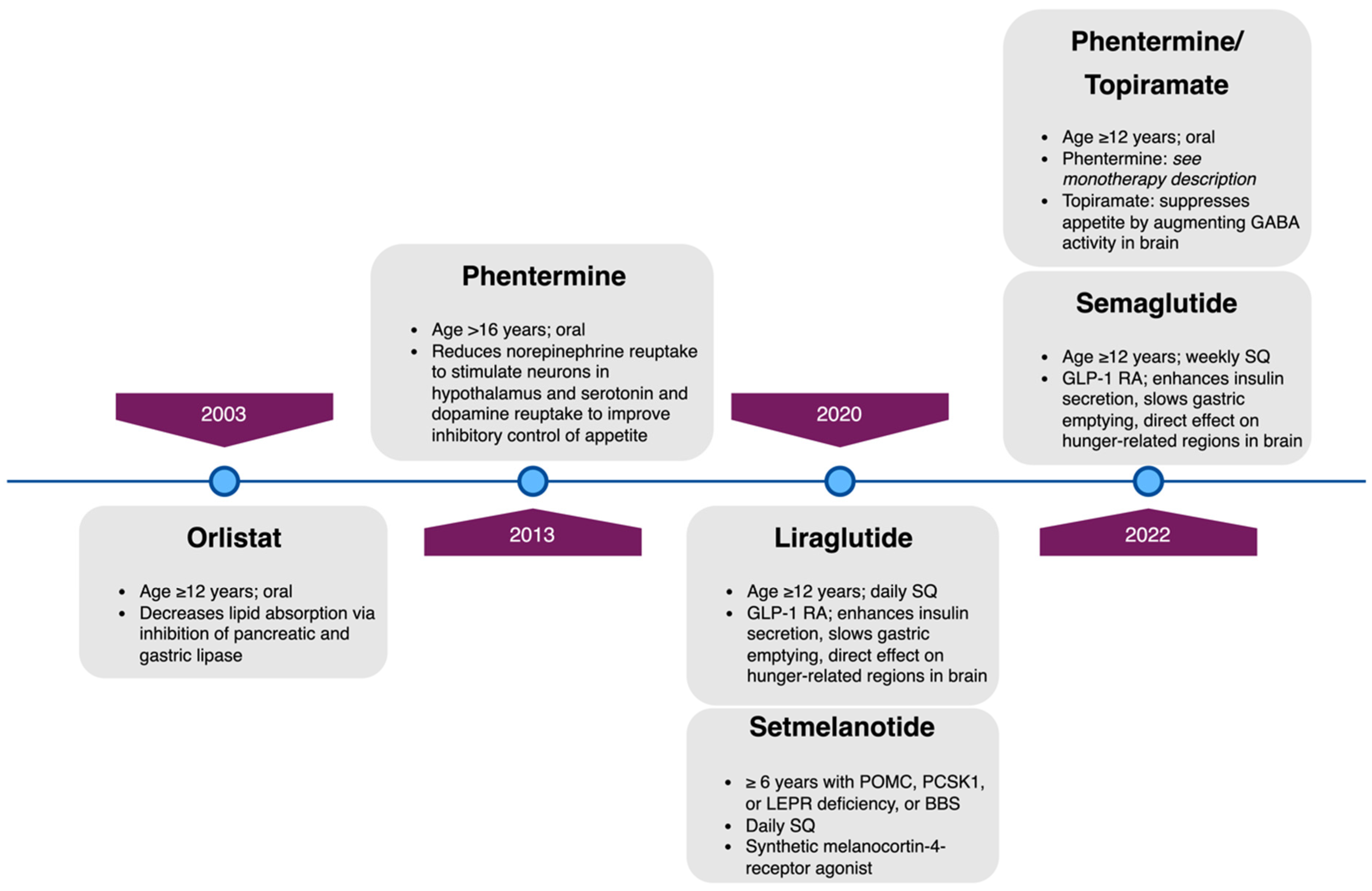
4.2. Weight-Loss Pharmacotherapy
4.3. Orlistat
4.4. Phentermine Monotherapy and Phentermine/Topiramate Combined Therapy
4.5. Glucagon-like Peptide-1 Receptor Agonists (GLP-1 RA): Liraglutide and Semaglutide
4.6. Setmelanotide
4.7. Metabolic and Bariatric Surgery
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Childhood Obesity Facts. Available online: https://www.cdc.gov/obesity/data/childhood.html (accessed on 16 March 2023).
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 16 March 2023).
- Di Cesare, M.; Soric, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Fryar, C.D.; Martin, C.B.; Freedman, D.S.; Carroll, M.D.; Gu, Q.; Hales, C.M. Trends in Obesity Prevalence by Race and Hispanic Origin-1999–2000 to 2017–2018. JAMA 2020, 324, 1208–1210. [Google Scholar] [CrossRef] [PubMed]
- Anekwe, C.V.; Jarrell, A.R.; Townsend, M.J.; Gaudier, G.I.; Hiserodt, J.M.; Stanford, F.C. Socioeconomics of Obesity. Curr. Obes. Rep. 2020, 9, 272–279. [Google Scholar] [CrossRef]
- Dinsa, G.D.; Goryakin, Y.; Fumagalli, E.; Suhrcke, M. Obesity and socioeconomic status in developing countries: A systematic review. Obes. Rev. 2012, 13, 1067–1079. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, J.M.; Divers, J.; Isom, S.; Saydah, S.; Imperatore, G.; Pihoker, C.; Marcovina, S.M.; Mayer-Davis, E.J.; Hamman, R.F.; Dolan, L.; et al. Trends in Prevalence of Type 1 and Type 2 Diabetes in Children and Adolescents in the US, 2001–2017. JAMA 2021, 326, 717–727. [Google Scholar] [CrossRef]
- Mayer-Davis, E.J.; Lawrence, J.M.; Dabelea, D.; Divers, J.; Isom, S.; Dolan, L.; Imperatore, G.; Linder, B.; Marcovina, S.; Pettitt, D.J.; et al. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002–2012. N. Engl. J. Med. 2017, 376, 1419–1429. [Google Scholar] [CrossRef]
- Hampl, S.E.; Hassink, S.G.; Skinner, A.C.; Armstrong, S.C.; Barlow, S.E.; Bolling, C.F.; Avila Edwards, K.C.; Eneli, I.; Hamre, R.; Joseph, M.M.; et al. Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents with Obesity. Pediatrics 2023, 151, e2022060640. [Google Scholar] [CrossRef]
- Griggs, S.; Redeker, N.S.; Jeon, S.; Grey, M. Daily variations in sleep and glucose in adolescents with type 1 diabetes. Pediatr. Diabetes 2020, 21, 1493–1501. [Google Scholar] [CrossRef]
- Inge, T.H.; Coley, R.Y.; Bazzano, L.A.; Xanthakos, S.A.; McTigue, K.; Arterburn, D.; Williams, N.; Wellman, R.; Coleman, K.J.; Courcoulas, A.; et al. Comparative effectiveness of bariatric procedures among adolescents: The PCORnet bariatric study. Surg. Obes. Relat. Dis. 2018, 14, 1374–1386. [Google Scholar] [CrossRef]
- Blackburn, H.; Jacobs, D., Jr. Commentary: Origins and evolution of body mass index (BMI): Continuing saga. Int. J. Epidemiol. 2014, 43, 665–669. [Google Scholar] [CrossRef]
- Vanderwall, C.; Randall Clark, R.; Eickhoff, J.; Carrel, A.L. BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr. 2017, 17, 135. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Khan, L.K.; Serdula, M.K.; Dietz, W.H.; Srinivasan, S.R.; Berenson, G.S. Racial differences in the tracking of childhood BMI to adulthood. Obes. Res. 2005, 13, 928–935. [Google Scholar] [CrossRef]
- Dietz, W.H.; Robinson, T.N. Use of the body mass index (BMI) as a measure of overweight in children and adolescents. J. Pediatr. 1998, 132, 191–193. [Google Scholar] [CrossRef]
- Hall, D.M.; Cole, T.J. What use is the BMI? Arch. Dis. Child. 2006, 91, 283–286. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Defining Child BMI Categories. Available online: https://www.cdc.gov/obesity/basics/childhood-defining.html (accessed on 21 March 2023).
- Magge, S.N.; Wolf, R.M.; Pyle, L.; Brown, E.A.; Benavides, V.C.; Bianco, M.E.; Chao, L.C.; Cymbaluk, A.; Gumus Balikcioglu, P.; Halpin, K.; et al. The COVID-19 pandemic is associated with a substantial rise in frequency and severity of presentation of youth-onset type 2 diabetes. J. Pediatr. 2022, 251, 51–59. [Google Scholar] [CrossRef]
- Divers, J.; Mayer-Davis, E.J.; Lawrence, J.M.; Isom, S.; Dabelea, D.; Dolan, L.; Imperatore, G.; Marcovina, S.; Pettitt, D.J.; Pihoker, C.; et al. Trends in Incidence of Type 1 and Type 2 Diabetes Among Youths—Selected Counties and Indian Reservations, United States, 2002–2015. Morb. Mortal Wkly. Rep. 2020, 69, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.A.; O’Rourke, N.E.; O’Grady, M.J. Prepubertal onset of type 2 diabetes in Shashi-Pena syndrome due to ASXL2 mutation. Am. J. Med. Genet. A 2022, 188, 2803–2807. [Google Scholar] [CrossRef] [PubMed]
- Astudillo, M.; Tosur, M.; Castillo, B.; Rafaey, A.; Siller, A.F.; Nieto, J.; Sisley, S.; McKay, S.; Nella, A.A.; Balasubramanyam, A.; et al. Type 2 diabetes in prepubertal children. Pediatr. Diabetes 2021, 22, 946–950. [Google Scholar] [CrossRef] [PubMed]
- Kautzky-Willer, A.; Harreiter, J.; Pacini, G. Sex and Gender Differences in Risk, Pathophysiology and Complications of Type 2 Diabetes Mellitus. Endocr. Rev. 2016, 37, 278–316. [Google Scholar] [CrossRef]
- Copeland, K.C.; Zeitler, P.; Geffner, M.; Guandalini, C.; Higgins, J.; Hirst, K.; Kaufman, F.R.; Linder, B.; Marcovina, S.; McGuigan, P.; et al. Characteristics of adolescents and youth with recent-onset type 2 diabetes: The TODAY cohort at baseline. J. Clin. Endocrinol. Metab. 2011, 96, 159–167. [Google Scholar] [CrossRef]
- Today Study Group; Bjornstad, P.; Drews, K.L.; Caprio, S.; Gubitosi-Klug, R.; Nathan, D.M.; Tesfaldet, B.; Tryggestad, J.; White, N.H.; Zeitler, P. Long-Term Complications in Youth-Onset Type 2 Diabetes. N. Engl. J. Med. 2021, 385, 416–426. [Google Scholar] [CrossRef] [PubMed]
- Dabelea, D.; Stafford, J.M.; Mayer-Davis, E.J.; D’Agostino, R., Jr.; Dolan, L.; Imperatore, G.; Linder, B.; Lawrence, J.M.; Marcovina, S.M.; Mottl, A.K.; et al. Association of Type 1 Diabetes vs Type 2 Diabetes Diagnosed During Childhood and Adolescence with Complications During Teenage Years and Young Adulthood. JAMA 2017, 317, 825–835. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.E.; Pettitt, D.J.; Bennett, P.H.; Knowler, W.C. Duration of obesity increases the incidence of NIDDM. Diabetes 1992, 41, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Perng, W.; Conway, R.; Mayer-Davis, E.; Dabelea, D. Youth-Onset Type 2 Diabetes: The Epidemiology of an Awakening Epidemic. Diabetes Care 2023, 46, 490–499. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 14. Children and Adolescents: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46, S230–S253. [Google Scholar] [CrossRef]
- Shah, A.S.; Zeitler, P.S.; Wong, J.; Pena, A.S.; Wicklow, B.; Arslanian, S.; Chang, N.; Fu, J.; Dabadghao, P.; Pinhas-Hamiel, O.; et al. ISPAD Clinical Practice Consensus Guidelines 2022: Type 2 diabetes in children and adolescents. Pediatr. Diabetes 2022, 23, 872–902. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46, S19–S40. [Google Scholar] [CrossRef]
- Liu, J.; Li, Y.; Zhang, D.; Yi, S.S.; Liu, J. Trends in Prediabetes among Youths in the US from 1999 through 2018. JAMA Pediatr. 2022, 176, 608–611. [Google Scholar] [CrossRef]
- Mehreen, T.S.; Kamalesh, R.; Pandiyan, D.; Kumar, D.S.; Anjana, R.M.; Mohan, V.; Ranjani, H. Incidence and Predictors of Dysglycemia and Regression to Normoglycemia in Indian Adolescents and Young Adults: 10-Year Follow-up of the ORANGE Study. Diabetes Technol. Ther. 2020, 22, 875–882. [Google Scholar] [CrossRef]
- Love-Osborne, K.A.; Sheeder, J.L.; Nadeau, K.J.; Zeitler, P. Longitudinal follow up of dysglycemia in overweight and obese pediatric patients. Pediatr. Diabetes 2017, 19, 199–204. [Google Scholar] [CrossRef]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [PubMed]
- Sam, S.; Edelstein, S.L.; Arslanian, S.A.; Barengolts, E.; Buchanan, T.A.; Caprio, S.; Ehrmann, D.A.; Hannon, T.S.; Tjaden, A.H.; Kahn, S.E.; et al. Baseline Predictors of Glycemic Worsening in Youth and Adults with Impaired Glucose Tolerance or Recently Diagnosed Type 2 Diabetes in the Restoring Insulin Secretion (RISE) Study. Diabetes Care 2021, 44, 1938–1947. [Google Scholar] [CrossRef] [PubMed]
- Ormazabal, V.; Nair, S.; Elfeky, O.; Aguayo, C.; Salomon, C.; Zuniga, F.A. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc. Diabetol. 2018, 17, 122. [Google Scholar] [CrossRef] [PubMed]
- Koskinen, J.S.; Kyto, V.; Juonala, M.; Viikari, J.S.A.; Nevalainen, J.; Kahonen, M.; Lehtimaki, T.; Hutri-Kahonen, N.; Laitinen, T.P.; Tossavainen, P.; et al. Childhood Dyslipidemia and Carotid Atherosclerotic Plaque in Adulthood: The Cardiovascular Risk in Young Finns Study. J. Am. Heart Assoc. 2023, 12, e027586. [Google Scholar] [CrossRef]
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Expert Panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 2011, 128 (Suppl. S5), S213–S256. [Google Scholar] [CrossRef]
- Skinner, A.C.; Perrin, E.M.; Moss, L.A.; Skelton, J.A. Cardiometabolic Risks and Severity of Obesity in Children and Young Adults. N. Engl. J. Med. 2015, 373, 1307–1317. [Google Scholar] [CrossRef]
- Brzezinski, M.; Metelska, P.; Mysliwiec, M.; Szlagatys-Sidorkiewicz, A. Lipid disorders in children living with overweight and obesity- large cohort study from Poland. Lipids Health Dis. 2020, 19, 47. [Google Scholar] [CrossRef]
- Eichberger, L.; Kern, L.; Wang, H.; Crow, J.; Rhee, K.E. Universal Lipid Screening Among 9- to 11-Year-Old Children: Screening Results and Physician Management. Clin. Pediatr. 2022, 61, 280–288. [Google Scholar] [CrossRef]
- Sriram, S.; St Sauver, J.L.; Jacobson, D.J.; Fan, C.; Lynch, B.A.; Cristiani, V.; Kullo, I.J.; Lteif, A.N.; Kumar, S. Temporal trends in lipid testing among children and adolescents: A population based study. Prev. Med. Rep. 2017, 8, 267–272. [Google Scholar] [CrossRef]
- Zachariah, J.P.; McNeal, C.J.; Copeland, L.A.; Fang-Hollingsworth, Y.; Stock, E.M.; Sun, F.; Song, J.J.; Gregory, S.T.; Tom, J.O.; Wright, E.A.; et al. Temporal trends in lipid screening and therapy among youth from 2002 to 2012. J. Clin. Lipidol. 2015, 9, S77–S87. [Google Scholar] [CrossRef]
- Dixon, D.B.; Kornblum, A.P.; Steffen, L.M.; Zhou, X.; Steinberger, J. Implementation of lipid screening guidelines in children by primary pediatric providers. J. Pediatr. 2014, 164, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Theodore, R.F.; Broadbent, J.; Nagin, D.; Ambler, A.; Hogan, S.; Ramrakha, S.; Cutfield, W.; Williams, M.J.; Harrington, H.; Moffitt, T.E.; et al. Childhood to Early-Midlife Systolic Blood Pressure Trajectories: Early-Life Predictors, Effect Modifiers, and Adult Cardiovascular Outcomes. Hypertension 2015, 66, 1108–1115. [Google Scholar] [CrossRef] [PubMed]
- Bell, C.S.; Samuel, J.P.; Samuels, J.A. Prevalence of Hypertension in Children. Hypertension 2019, 73, 148–152. [Google Scholar] [CrossRef]
- Chinali, M.; de Simone, G.; Roman, M.J.; Best, L.G.; Lee, E.T.; Russell, M.; Howard, B.V.; Devereux, R.B. Cardiac markers of pre-clinical disease in adolescents with the metabolic syndrome: The strong heart study. J. Am. Coll. Cardiol. 2008, 52, 932–938. [Google Scholar] [CrossRef] [PubMed]
- Urbina, E.M.; Mendizabal, B.; Becker, R.C.; Daniels, S.R.; Falkner, B.E.; Hamdani, G.; Hanevold, C.; Hooper, S.R.; Ingelfinger, J.R.; Lanade, M.; et al. Association of Blood Pressure Level with Left Ventricular Mass in Adolescents. Hypertension 2019, 74, 590–596. [Google Scholar] [CrossRef]
- Newton, K.P.; Hou, J.; Crimmins, N.A.; Lavine, J.E.; Barlow, S.E.; Xanthakos, S.A.; Africa, J.; Behling, C.; Donithan, M.; Clark, J.M.; et al. Prevalence of Prediabetes and Type 2 Diabetes in Children with Nonalcoholic Fatty Liver Disease. JAMA Pediatr. 2016, 170, e161971. [Google Scholar] [CrossRef]
- Vos, M.B.; Abrams, S.H.; Barlow, S.E.; Caprio, S.; Daniels, S.R.; Kohli, R.; Mouzaki, M.; Sathya, P.; Schwimmer, J.B.; Sundaram, S.S.; et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J. Pediatr. Gastroenterol. Nutr. 2017, 64, 319–334. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef]
- Tana, C.; Ballestri, S.; Ricci, F.; Di Vincenzo, A.; Ticinesi, A.; Gallina, S.; Giamberardino, M.A.; Cipollone, F.; Sutton, R.; Vettor, R.; et al. Cardiovascular Risk in Non-Alcoholic Fatty Liver Disease: Mechanisms and Therapeutic Implications. Int. J. Environ. Res. Public. Health 2019, 16, 3104. [Google Scholar] [CrossRef]
- Tas, E.; Bai, S.; Ou, X.; Mercer, K.; Lin, H.; Mansfield, K.; Buchmann, R.; Diaz, E.C.; Oden, J.; Borsheim, E.; et al. Fibroblast Growth Factor-21 to Adiponectin Ratio: A Potential Biomarker to Monitor Liver Fat in Children with Obesity. Front. Endocrinol. 2020, 11, 654. [Google Scholar] [CrossRef]
- Xanthakos, S.A.; Lavine, J.E.; Yates, K.P.; Schwimmer, J.B.; Molleston, J.P.; Rosenthal, P.; Murray, K.F.; Vos, M.B.; Jain, A.K.; Scheimann, A.O.; et al. Progression of Fatty Liver Disease in Children Receiving Standard of Care Lifestyle Advice. Gastroenterology 2020, 159, 1731–1751.e10. [Google Scholar] [CrossRef] [PubMed]
- Simon, T.G.; Roelstraete, B.; Hartjes, K.; Shah, U.; Khalili, H.; Arnell, H.; Ludvigsson, J.F. Non-alcoholic fatty liver disease in children and young adults is associated with increased long-term mortality. J. Hepatol. 2021, 75, 1034–1041. [Google Scholar] [CrossRef] [PubMed]
- Zezos, P.; Renner, E.L. Liver transplantation and non-alcoholic fatty liver disease. World J. Gastroenterol. 2014, 20, 15532–15538. [Google Scholar] [CrossRef]
- Shin, J.; Kim, M.J.; Shin, H.J.; Yoon, H.; Kim, S.; Koh, H.; Lee, M.J. Quick assessment with controlled attenuation parameter for hepatic steatosis in children based on MRI-PDFF as the gold standard. BMC Pediatr. 2019, 19, 112. [Google Scholar] [CrossRef] [PubMed]
- Dulai, P.S.; Sirlin, C.B.; Loomba, R. MRI and MRE for non-invasive quantitative assessment of hepatic steatosis and fibrosis in NAFLD and NASH: Clinical trials to clinical practice. J. Hepatol. 2016, 65, 1006–1016. [Google Scholar] [CrossRef]
- Morkem, R.; Theal, R.; Barber, D.; Flemming, J.; Queenan, J.; Kehar, M. Screening Patterns of Nonalcoholic Fatty Liver Disease in Children with Obesity in Canadian Primary Care: A Cross-Sectional Study. Can. J. Gastroenterol. Hepatol. 2022, 2022, 8435581. [Google Scholar] [CrossRef] [PubMed]
- Andersen, I.G.; Holm, J.C.; Homoe, P. Obstructive sleep apnea in children and adolescents with and without obesity. Eur. Arch. Otorhinolaryngol. 2019, 276, 871–878. [Google Scholar] [CrossRef]
- Hannon, T.S.; Lee, S.; Chakravorty, S.; Lin, Y.; Arslanian, S.A. Sleep-disordered breathing in obese adolescents is associated with visceral adiposity and markers of insulin resistance. Int. J. Pediatr. Obes. 2011, 6, 157–160. [Google Scholar] [CrossRef]
- Siriwat, R.; Wang, L.; Shah, V.; Mehra, R.; Ibrahim, S. Obstructive sleep apnea and insulin resistance in children with obesity. J. Clin. Sleep Med. 2020, 16, 1081–1090. [Google Scholar] [CrossRef]
- Chen, L.D.; Chen, M.X.; Chen, G.P.; Lin, X.J.; Huang, J.F.; Zeng, A.M.; Huang, Y.P.; Lin, Q.C. Association between obstructive sleep apnea and non-alcoholic fatty liver disease in pediatric patients: A meta-analysis. Pediatr. Obes. 2021, 16, e12718. [Google Scholar] [CrossRef]
- Chuang, H.H.; Hsu, J.F.; Wang, C.Y.; Chuang, L.P.; Chen, M.C.; Chen, N.H.; Huang, Y.S.; Li, H.Y.; Lee, L.A. Hypertension in Children with Obstructive Sleep Apnea Syndrome-Age, Weight Status, and Disease Severity. Int. J. Environ. Res. Public Health 2021, 18, 6902. [Google Scholar] [CrossRef] [PubMed]
- Hannon, T.S.; Rofey, D.L.; Ryan, C.M.; Clapper, D.A.; Chakravorty, S.; Arslanian, S.A. Relationships among obstructive sleep apnea, anthropometric measures, and neurocognitive functioning in adolescents with severe obesity. J. Pediatr. 2012, 160, 732–735. [Google Scholar] [CrossRef] [PubMed]
- Witchel, S.F.; Oberfield, S.E.; Pena, A.S. Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment with Emphasis on Adolescent Girls. J. Endocr. Soc. 2019, 3, 1545–1573. [Google Scholar] [CrossRef] [PubMed]
- Barber, T.M.; Franks, S. Obesity and polycystic ovary syndrome. Clin. Endocrinol. 2021, 95, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Meczekalski, B.; Niwczyk, O.; Kostrzak, A.; Maciejewska-Jeske, M.; Bala, G.; Szeliga, A. PCOS in Adolescents-Ongoing Riddles in Diagnosis and Treatment. J. Clin. Med. 2023, 12, 1221. [Google Scholar] [CrossRef] [PubMed]
- Seif, M.W.; Diamond, K.; Nickkho-Amiry, M. Obesity and menstrual disorders. Best. Pract. Res. Clin. Obstet. Gynaecol. 2015, 29, 516–527. [Google Scholar] [CrossRef] [PubMed]
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J.; International, P.N. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum. Reprod. 2018, 33, 1602–1618. [Google Scholar] [CrossRef]
- Witchel, S.F.; Teede, H.J.; Pena, A.S. Curtailing PCOS. Pediatr. Res. 2020, 87, 353–361. [Google Scholar] [CrossRef]
- Haqq, A.M.; Kebbe, M.; Tan, Q.; Manco, M.; Salas, X.R. Complexity and Stigma of Pediatric Obesity. Child. Obes. 2021, 17, 229–240. [Google Scholar] [CrossRef]
- Ma, L.; Chu, M.; Li, Y.; Wu, Y.; Yan, A.F.; Johnson, B.; Wang, Y. Bidirectional relationships between weight stigma and pediatric obesity: A systematic review and meta-analysis. Obes. Rev. 2021, 22, e13178. [Google Scholar] [CrossRef]
- van Geel, M.; Vedder, P.; Tanilon, J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the correlation between weight status and bullying. Int. J. Obes. 2014, 38, 1263–1267. [Google Scholar] [CrossRef] [PubMed]
- Pont, S.J.; Puhl, R.; Cook, S.R.; Slusser, W.; Section On, O.; Obesity, S. Stigma Experienced by Children and Adolescents with Obesity. Pediatrics 2017, 140, e20173034. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, L.; Hagman, E.; Danielsson, P.; Marcus, C.; Persson, M. Anxiety and depression in children and adolescents with obesity: A nationwide study in Sweden. BMC Med. 2020, 18, 30. [Google Scholar] [CrossRef] [PubMed]
- Sutaria, S.; Devakumar, D.; Yasuda, S.S.; Das, S.; Saxena, S. Is obesity associated with depression in children? Systematic review and meta-analysis. Arch. Dis. Child. 2019, 104, 64–74. [Google Scholar] [CrossRef]
- Quek, Y.H.; Tam, W.W.S.; Zhang, M.W.B.; Ho, R.C.M. Exploring the association between childhood and adolescent obesity and depression: A meta-analysis. Obes. Rev. 2017, 18, 742–754. [Google Scholar] [CrossRef]
- Kokka, I.; Mourikis, I.; Bacopoulou, F. Psychiatric Disorders and Obesity in Childhood and Adolescence—A Systematic Review of Cross-Sectional Studies. Children 2023, 10, 285. [Google Scholar] [CrossRef]
- Latzer, Y.; Stein, D. A review of the psychological and familial perspectives of childhood obesity. J. Eat. Disord. 2013, 1, 7. [Google Scholar] [CrossRef]
- Naughton, M.J.; Ruggiero, A.M.; Lawrence, J.M.; Imperatore, G.; Klingensmith, G.J.; Waitzfelder, B.; McKeown, R.E.; Standiford, D.A.; Liese, A.D.; Loots, B.; et al. Health-related quality of life of children and adolescents with type 1 or type 2 diabetes mellitus: SEARCH for Diabetes in Youth Study. Arch. Pediatr. Adolesc. Med. 2008, 162, 649–657. [Google Scholar] [CrossRef]
- Trent, M.E.; Rich, M.; Austin, S.B.; Gordon, C.M. Quality of life in adolescent girls with polycystic ovary syndrome. Arch. Pediatr. Adolesc. Med. 2002, 156, 556–560. [Google Scholar] [CrossRef]
- Tran, K.D.; Nguyen, C.D.; Weedon, J.; Goldstein, N.A. Child behavior and quality of life in pediatric obstructive sleep apnea. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 52–57. [Google Scholar] [CrossRef]
- Skinner, A.C.; Staiano, A.E.; Armstrong, S.C.; Barkin, S.L.; Hassink, S.G.; Moore, J.E.; Savage, J.S.; Vilme, H.; Weedn, A.E.; Liebhart, J.; et al. Appraisal of Clinical Care Practices for Child Obesity Treatment. Part I: Interventions. Pediatrics 2023, 151, e2022060642. [Google Scholar] [CrossRef] [PubMed]
- Weghuber, D.; Barrett, T.; Barrientos-Perez, M.; Gies, I.; Hesse, D.; Jeppesen, O.K.; Kelly, A.S.; Mastrandrea, L.D.; Sorrig, R.; Arslanian, S.; et al. Once-Weekly Semaglutide in Adolescents with Obesity. N. Engl. J. Med. 2022, 387, 2245–2257. [Google Scholar] [CrossRef] [PubMed]
- U.S. Preventive Services Task Force; Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W., Jr.; Kemper, A.R.; Krist, A.H.; et al. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 317, 2417–2426. [Google Scholar] [CrossRef] [PubMed]
- Bean, M.K.; Caccavale, L.J.; Adams, E.L.; Burnette, C.B.; LaRose, J.G.; Raynor, H.A.; Wickham, E.P., 3rd; Mazzeo, S.E. Parent Involvement in Adolescent Obesity Treatment: A Systematic Review. Pediatrics 2020, 146, e20193315. [Google Scholar] [CrossRef]
- Berge, J.M.; Everts, J.C. Family-Based Interventions Targeting Childhood Obesity: A Meta-Analysis. Child. Obes. 2011, 7, 110–121. [Google Scholar] [CrossRef]
- Skelton, J.A.; Beech, B.M. Attrition in paediatric weight management: A review of the literature and new directions. Obes. Rev. 2011, 12, e273–e281. [Google Scholar] [CrossRef]
- Morales, E.; Torres-Castillo, N.; Garaulet, M. Infancy and Childhood Obesity Grade Predicts Weight Loss in Adulthood: The ONTIME Study. Nutrients 2021, 13, 2132. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute. NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US); National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 1998.
- American Medical Association. Recognition of Obesity as a Disease H-440.842; American Medical Association: Chicago, IL, USA, 2013. [Google Scholar]
- Woodard, K.; Louque, L.; Hsia, D.S. Medications for the treatment of obesity in adolescents. Ther. Adv. Endocrinol. Metab. 2020, 11, 2042018820918789. [Google Scholar] [CrossRef]
- U.S. Food & Drug Administration. FDA Approves Weight Management Drug for Patients Aged 12 and Older; U.S. Food & Drug Administration: Silver Spring, MD, USA, 2020.
- U.S. Food & Drug Administration. FDA Approves Treatment for Chronic Weight Management in Pediatric Patients Aged 12 Years and Older; U.S. Food & Drug Administration: Silver Spring, MD, USA, 2022.
- Novo Nordisk USA. FDA Approves Once-Weekly Wegovy® Injection for the Treatment of Obesity in Teens Aged 12 Years and Older; Novo Nordisk USA: Plainsboro, NJ, USA, 2022. [Google Scholar]
- Teva. Prescribing Information for ADIPEX-P (R); Teva: Parsippany-Troy Hills, NJ, USA, 2013. [Google Scholar]
- U.S. Food & Drug Administration. FDA Approves First Treatment for Weight Management for People with Certain Rare Genetic Conditions; U.S. Food & Drug Administration: Silver Spring, MD, USA, 2020.
- Czepiel, K.S.; Perez, N.P.; Campoverde Reyes, K.J.; Sabharwal, S.; Stanford, F.C. Pharmacotherapy for the Treatment of Overweight and Obesity in Children, Adolescents, and Young Adults in a Large Health System in the US. Front. Endocrinol. 2020, 11, 290. [Google Scholar] [CrossRef]
- Mead, E.; Atkinson, G.; Richter, B.; Metzendorf, M.I.; Baur, L.; Finer, N.; Corpeleijn, E.; O’Malley, C.; Ells, L.J. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst. Rev. 2016, 11, CD012436. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, A.; Mousavi, S.M.; Mokhtari, T.; Parohan, M.; Milajerdi, A. Metformin Therapy Reduces Obesity Indices in Children and Adolescents: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Child. Obes. 2020, 16, 174–191. [Google Scholar] [CrossRef]
- Singhal, V.; Sella, A.C.; Malhotra, S. Pharmacotherapy in pediatric obesity: Current evidence and landscape. Curr. Opin. Endocrinol. Diabetes Obes. 2021, 28, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Chanoine, J.P.; Hampl, S.; Jensen, C.; Boldrin, M.; Hauptman, J. Effect of orlistat on weight and body composition in obese adolescents: A randomized controlled trial. JAMA 2005, 293, 2873–2883. [Google Scholar] [CrossRef] [PubMed]
- Haddock, C.K.; Poston, W.S.; Dill, P.L.; Foreyt, J.P.; Ericsson, M. Pharmacotherapy for obesity: A quantitative analysis of four decades of published randomized clinical trials. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 262–273. [Google Scholar] [CrossRef]
- Grabarczyk, T.R. Observational Comparative Effectiveness of Pharmaceutical Treatments for Obesity within the Veterans Health Administration. Pharmacotherapy 2018, 38, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.S.; Bensignor, M.O.; Hsia, D.S.; Shoemaker, A.H.; Shih, W.; Peterson, C.; Varghese, S.T. Phentermine/Topiramate for the Treatment of Adolescent Obesity. NEJM Evid. 2022, 1, EVIDoa2200014. [Google Scholar] [CrossRef]
- VIVUS LLC. Risk Evaluation and Mitigation Strategy (REMS). Available online: https://qsymiarems.com/ (accessed on 7 May 2023).
- Kelly, A.S.; Auerbach, P.; Barrientos-Perez, M.; Gies, I.; Hale, P.M.; Marcus, C.; Mastrandrea, L.D.; Prabhu, N.; Arslanian, S.; Investigators, N.N.T. A Randomized, Controlled Trial of Liraglutide for Adolescents with Obesity. N. Engl. J. Med. 2020, 382, 2117–2128. [Google Scholar] [CrossRef]
- Clement, K.; van den Akker, E.; Argente, J.; Bahm, A.; Chung, W.K.; Connors, H.; De Waele, K.; Farooqi, I.S.; Gonneau-Lejeune, J.; Gordon, G.; et al. Efficacy and safety of setmelanotide, an MC4R agonist, in individuals with severe obesity due to LEPR or POMC deficiency: Single-arm, open-label, multicentre, phase 3 trials. Lancet Diabetes Endocrinol. 2020, 8, 960–970. [Google Scholar] [CrossRef]
- Haqq, A.M.; Chung, W.K.; Dollfus, H.; Haws, R.M.; Martos-Moreno, G.A.; Poitou, C.; Yanovski, J.A.; Mittleman, R.S.; Yuan, G.; Forsythe, E.; et al. Efficacy and safety of setmelanotide, a melanocortin-4 receptor agonist, in patients with Bardet-Biedl syndrome and Alstrom syndrome: A multicentre, randomised, double-blind, placebo-controlled, phase 3 trial with an open-label period. Lancet Diabetes Endocrinol. 2022, 10, 859–868. [Google Scholar] [CrossRef]
- Maahs, D.; de Serna, D.G.; Kolotkin, R.L.; Ralston, S.; Sandate, J.; Qualls, C.; Schade, D.S. Randomized, double-blind, placebo-controlled trial of orlistat for weight loss in adolescents. Endocr. Pract. 2006, 12, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Safety and Efficacy of Xenical in Children and Adolescents with Obesity-Related Diseases—Study Results—ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/results/NCT00001723 (accessed on 5 May 2023).
- National Center for Biotechnology Information. PubChem Compound Summary for CID 4771, Phentermine; National Center for Biotechnology Information: Bethesda, MD, USA, 2005.
- National Center for Biotechnology Information. PubChem Compound Summary for CID 5284627, Topiramate; National Center for Biotechnology Information: Bethesda, MD, USA, 2005.
- VIVUS LLC. Prescribing Information: QSYMIA (Phentermine and Topiramate Extended-Release Capsules), for Oral Use, CIV; VIVUS LLC.: Campbell, CA, USA, 2012; Revised 06/2022. [Google Scholar]
- Ard, J.; Fitch, A.; Fruh, S.; Herman, L. Weight Loss and Maintenance Related to the Mechanism of Action of Glucagon-Like Peptide 1 Receptor Agonists. Adv. Ther. 2021, 38, 2821–2839. [Google Scholar] [CrossRef] [PubMed]
- Bezin, J.; Gouverneur, A.; Penichon, M.; Mathieu, C.; Garrel, R.; Hillaire-Buys, D.; Pariente, A.; Faillie, J.L. GLP-1 Receptor Agonists and the Risk of Thyroid Cancer. Diabetes Care 2023, 46, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Novo Nordisk. Prescribing Information: SAXENDA (Liraglutide) Injection, for Subcutaneous Use; Novo Nordisk: Plainsboro, NJ, USA, April 2023. [Google Scholar]
- Novo Nordisk. Prescribing Information: VICTOZA® (Liraglutide) Injection, for Subcutaneous Use; Novo Nordisk: Plainsboro, NJ, USA, June 2022. [Google Scholar]
- Novo Nordisk. Prescribing Information: WEGOVY® (Semaglutide) Injection, for Subcutaneous Use; Novo Nordisk: Plainsboro, NJ, USA, December 2022. [Google Scholar]
- Kelly, A.S.; Arslanian, S.; Hesse, D.; Iversen, A.T.; Korner, A.; Schmidt, S.; Sorrig, R.; Weghuber, D.; Jastreboff, A.M. Reducing BMI below the obesity threshold in adolescents treated with once-weekly subcutaneous semaglutide 2.4 mg. Obesity, 2023; in press. [Google Scholar] [CrossRef]
- Rhythm Pharmaceuticals. Prescribing Information: IMCIVREE® (Setmelanotide) Injection, for Subcutaneous Use; Rhythm Pharmaceuticals: Boston, MA, USA, June 2022. [Google Scholar]
- Clapp, B.; Ponce, J.; DeMaria, E.; Ghanem, O.; Hutter, M.; Kothari, S.; LaMasters, T.; Kurian, M.; English, W. American Society for Metabolic and Bariatric Surgery 2020 estimate of metabolic and bariatric procedures performed in the United States. Surg. Obes. Relat. Dis. 2022, 18, 1134–1140. [Google Scholar] [CrossRef]
- Singhal, V.; Youssef, S.; Misra, M. Use of sleeve gastrectomy in adolescents and young adults with severe obesity. Curr. Opin. Pediatr. 2020, 32, 547–553. [Google Scholar] [CrossRef]
- Chang, S.H.; Stoll, C.R.; Song, J.; Varela, J.E.; Eagon, C.J.; Colditz, G.A. The effectiveness and risks of bariatric surgery: An updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014, 149, 275–287. [Google Scholar] [CrossRef]
- Pedroso, F.E.; Angriman, F.; Endo, A.; Dasenbrock, H.; Storino, A.; Castillo, R.; Watkins, A.A.; Castillo-Angeles, M.; Goodman, J.E.; Zitsman, J.L. Weight loss after bariatric surgery in obese adolescents: A systematic review and meta-analysis. Surg. Obes. Relat. Dis. 2018, 14, 413–422. [Google Scholar] [CrossRef]
- Ahn, S.M. Current Issues in Bariatric Surgery for Adolescents with Severe Obesity: Durability, Complications, and Timing of Intervention. J. Obes. Metab. Syndr. 2020, 29, 4–11. [Google Scholar] [CrossRef]
- Inge, T.H.; Jenkins, T.M.; Xanthakos, S.A.; Dixon, J.B.; Daniels, S.R.; Zeller, M.H.; Helmrath, M.A. Long-term outcomes of bariatric surgery in adolescents with severe obesity (FABS-5+): A prospective follow-up analysis. Lancet Diabetes Endocrinol. 2017, 5, 165–173. [Google Scholar] [CrossRef]
- Cadena-Obando, D.; Ramirez-Renteria, C.; Ferreira-Hermosillo, A.; Albarran-Sanchez, A.; Sosa-Eroza, E.; Molina-Ayala, M.; Espinosa-Cardenas, E. Are there really any predictive factors for a successful weight loss after bariatric surgery? BMC Endocr. Disord. 2020, 20, 20. [Google Scholar] [CrossRef]
- Courcoulas, A.P.; Christian, N.J.; O’Rourke, R.W.; Dakin, G.; Patchen Dellinger, E.; Flum, D.R.; Melissa Kalarchian, P.D.; Mitchell, J.E.; Patterson, E.; Pomp, A.; et al. Preoperative factors and 3-year weight change in the Longitudinal Assessment of Bariatric Surgery (LABS) consortium. Surg. Obes. Relat. Dis. 2015, 11, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Jensen, A.B.; Renstrom, F.; Aczel, S.; Folie, P.; Biraima-Steinemann, M.; Beuschlein, F.; Bilz, S. Efficacy of the Glucagon-Like Peptide-1 Receptor Agonists Liraglutide and Semaglutide for the Treatment of Weight Regain After Bariatric surgery: A Retrospective Observational Study. Obes. Surg. 2023, 33, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
- Lautenbach, A.; Wernecke, M.; Huber, T.B.; Stoll, F.; Wagner, J.; Meyhofer, S.M.; Meyhofer, S.; Aberle, J. The Potential of Semaglutide Once-Weekly in Patients without Type 2 Diabetes with Weight Regain or Insufficient Weight Loss After Bariatric Surgery-a Retrospective Analysis. Obes. Surg. 2022, 32, 3280–3288. [Google Scholar] [CrossRef] [PubMed]
| ADA | AAP | ISPAD | |
|---|---|---|---|
| Maternal history of diabetes or gestational diabetes during child’s gestation | x | x | x |
| Family history of type 2 diabetes in 1st or 2nd-degree relative | x | x | x |
| Race/ethnicity (Native American, African American, Latino, Asian American, Pacific Islander) | x | x | |
| Signs of insulin resistance or associated conditions (acanthosis nigricans, hypertension, dyslipidemia, PCOS, small-for-gestational-age birth weight) | x | x | x |
| Use of obesogenic psychotropic medications | x | x |
| Generic (Trade) Name | Mechanism | Age | Dose | Weight-Related Efficacy | Comorbidity Impact | Adverse Effects |
|---|---|---|---|---|---|---|
| Orlistat (Xenical®) | Inhibition of pancreatic and gastric lipase | ≥12 years | 120 mg three times daily by mouth with meals | Wt: −2.5 kg (−4.3, −0.7); BMI: −0.79 kg/m2 (−1.08, −0.51) [101] | FG, HDL, LDL, TG: NS; SBP: NS, DBP: −0.51 vs. +1.3 vs. placebo; ALT: NR [104] | Abdominal pain, steatorrhea, flatus, fecal urgency and incontinence, and fat-soluble vitamin deficiency |
| Phentermine alone (Adipex-P®, Lomaira™) | Reduces norepinephrine reuptake to stimulate neurons in hypothalamus | >16 years | 15 mg, 30 mg, or 37.5 mg daily, oral | Wt: −3.6 kg (range −0.6 to −6.0) [105] (review, adult studies) | HbA1c, HDL, LDL, TG, SBP, DBP: NS, ALT: NR [106] (observational study, adults) | Insomnia, dry mouth, tremor, headache, dizziness, mood alteration, heart rate and blood pressure elevation |
| Phentermine/topiramate extended-release (Qsymia®) | Topiramate: suppresses appetite by augmenting GABA activity in brain | ≥12 years | 7.5 mg/46 mg or 15 mg/92 mg | % change in BMI at 56 weeks vs. placebo: −8.11% (−11.92, −4.31%) and −10.44% (−13.89, −6.99%) for top and mid-doses [107] | HbA1c: NS, HDL: +10% and +9% for mid- and top-dose; LDL: NS; TG: −21% for mid- and top-dose; SBP, DBP: NS; ALT: NR [107] | Topiramate: reversible cognitive dysfunction, paresthesia, metabolic acidosis; teratogenic (orofacial defects) and may decrease oral Contraceptive efficacy; counseling, serial pregnancy testing recommended [108] |
| Liraglutide (Saxenda®) | GLP-1 RA | ≥12 years | 3.0 mg subcutaneous once daily | BMI SDS at 56 weeks vs. placebo: −0.22 (−0.37, −0.08); relative: −4.64% (−7.14, −2.14); BMI reduction of ≥5% 43.3% vs. 18.7% [109] | HbA1c: NS; HDL, LDL, TG: NS; SBP, DBP: NS; ALT: NR [109] | Nausea, vomiting, diarrhea; increased heart rate from baseline; hypoglycemia in adolescents without type 2 diabetes (15%) |
| Semaglutide (Wegovy®) | GLP-1 RA | ≥12 years | 2.4 mg subcutaneous once weekly | Mean change in BMI from baseline to week 68 vs. placebo: −16.7% (−20.3, −13.2%); Weight reduction of ≥5% 73% vs. 18% [85] | HbA1c: −0.3%; HDL: NS, LDL: −7.0 mg/dL, TG: −30.2 mg/dL; SBP, DBP: NS; ALT: −14.1 IU/mL [85] | Nausea, vomiting, diarrhea |
| Setmelanotide (Imcivree®) | Melanocortin-4-receptor agonist | ≥6 years with BBS or POMC, PCSK1, LEPR deficiency | 3 mg subcutaneous once daily | POMC, LEPR: ≥10% weight loss in 80% of POMC and 45% of LEPR participants [110] | % change from baseline for (1) POMC or (2) LEPR (Clement): FG: (1) −17.2%, (2) NS; HDL: (1) +45.0%, (2) +19.6%; LDL: (1) NS, (2) −10.0%; TG: (1) −36.6%, (2) NS; SBP, DBP: (1) NS, (2) NS; ALT: NR [110] | New/worsened depression or suicidal ideation; sexual adverse reactions; skin hyperpigmentation (most common); injection site reaction; nausea, vomiting |
| BBS: 7.9% average BMI loss [111] | % change from baseline: FG, HbA1c: NR; HDL: +4.3%; LDL: −8.8%; TG: −10.7%; SBP, DBP: NR; ALT: NR [111] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vajravelu, M.E.; Tas, E.; Arslanian, S. Pediatric Obesity: Complications and Current Day Management. Life 2023, 13, 1591. https://doi.org/10.3390/life13071591
Vajravelu ME, Tas E, Arslanian S. Pediatric Obesity: Complications and Current Day Management. Life. 2023; 13(7):1591. https://doi.org/10.3390/life13071591
Chicago/Turabian StyleVajravelu, Mary Ellen, Emir Tas, and Silva Arslanian. 2023. "Pediatric Obesity: Complications and Current Day Management" Life 13, no. 7: 1591. https://doi.org/10.3390/life13071591
APA StyleVajravelu, M. E., Tas, E., & Arslanian, S. (2023). Pediatric Obesity: Complications and Current Day Management. Life, 13(7), 1591. https://doi.org/10.3390/life13071591






