Cardiometabolic Patient-Related Factors Influencing the Adherence to Lifestyle Changes and Overall Treatment: A Review of the Recent Literature
Abstract
1. Introduction
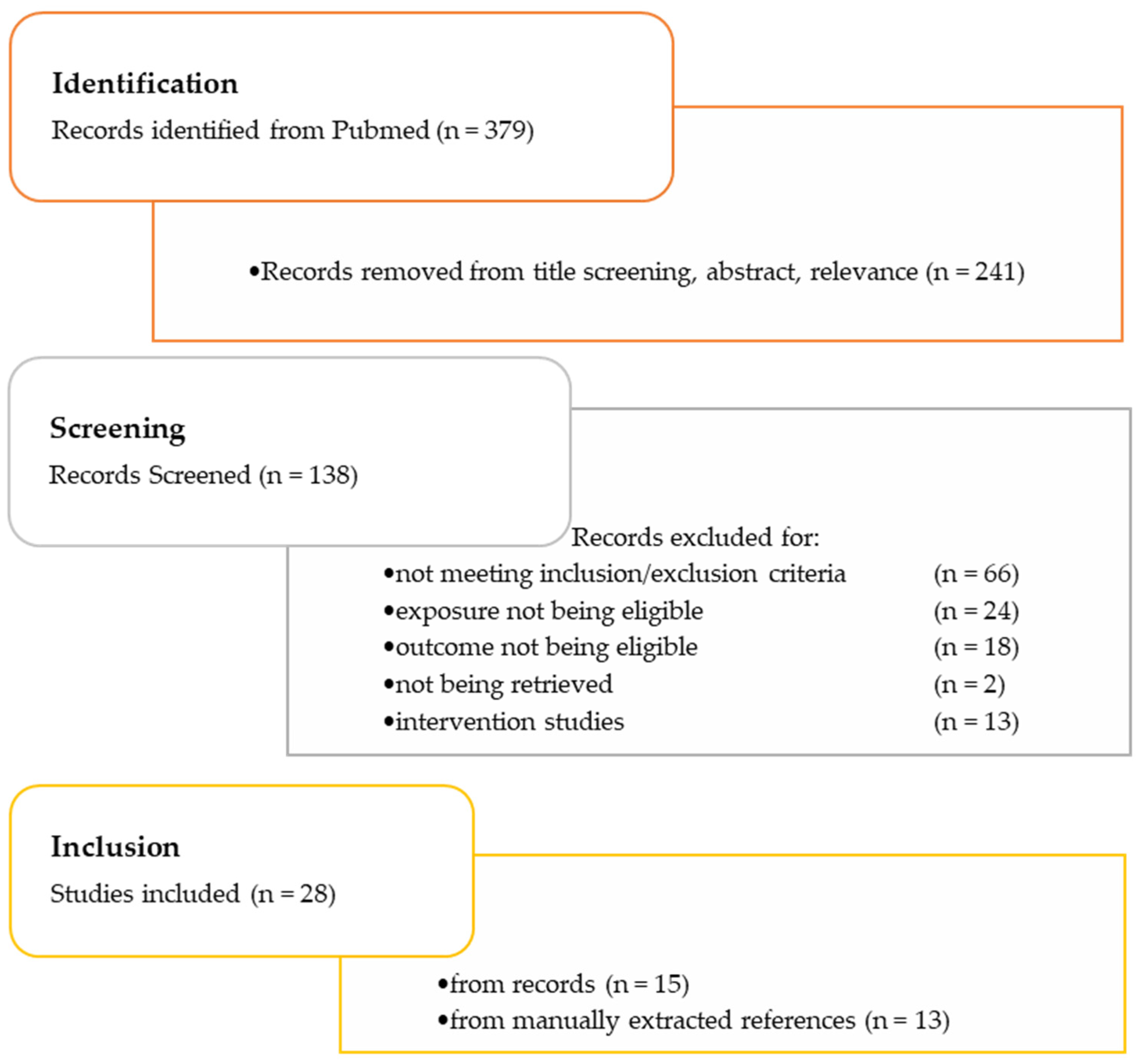
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
3. Results
3.1. General Characteristics of the Included Studies
| Authors | Year | Country | Type of Study | Population Characteristics (n, Sex, Age, and Condition) | Objectives | Data Collection Tools | Type of Adherence to Treatment Assessed | Outcome | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| Thomas | 2007 | USA | quantitative cross-sectional study | 97 adults diagnosed with HF from 2 large HF clinics (60 male, 37 female) Age (Mean ± SD): 62 ± 15 | To evaluate and understand how self-concept, components of self-concept and which aspects of self-concept influence adherence to prescribed regimens (diet, exercise, and medication) in individuals with HF |
| Diet Medication Exercise | Health regimens that are perceived by participants as threatening to self-concept are associated with lower adherence | [39] |
| Chiou et al. | 2009 | Taiwan | quantitative cross-sectional study | 156 patients diagnosed with CAD (116 male, and 40 female) Age (Mean ± SD): 70 ± 10.1 | To understand the modifying behaviors of CAD patients and recognize the factors that influence them |
| Lifestyle Medication | Self-efficacy was the strongest predictor of behavior influencing adherence to treatment | [23] |
| Ruf et al. | 2010 | South Africa | quantitative cross-sectional study | 200 patients with chronic heart failure (CHF) from a cardiology clinic, (109 male, 91 female) Age (Mean ± SD): 56 ± 14 | To investigate treatment adherence, self-care behavior and treatment knowledge in patients with CHF |
| Diet Medication Exercise | The higher the knowledge of the patients, the higher adherence to CHF management | [41] |
| Iyalomhe and Iyalomhe | 2010 | Nigeria | quantitative cross-sectional study | 108 hypertensive patients for at least a year that visited health facilities, (60 male, 48 female) Age (Mean ± SD): 59.05 ± 9.06 | To assess the knowledge, attitudes, perceptions and lifestyle practices of hypertensive patients as a means to ameliorate their health and adjust their treatment |
| Lifestyle (diet) Medication | The greater the impact of negative psychosocial factors on patients, the greater the non-adherence to treatment | [42] |
| Heydari et al. | 2011 | Iran | quantitative cross-sectional study | 108 patients with HF, duration of at least 2 months, recruited from hospitals (67% male, and 33% female) Age: >20 years | To investigate the relationship between self-concept cognitive perception (threat and challenge) and adherence to therapeutic regimens in patients with HF |
| Diet and medication |
Higher adherence depends on the following:
| [24] |
| Singh et al. | 2012 | UK | qualitative cross-sectional study | 20 patients with type 2 diabetes mellitus with duration approximately 10 years or more from a hospital’s diabetes care outpatient clinic (10 male, and 10 female) Median age: 60.5 years | To explore experiences of patients with diabetes as regards to their support systems and identify barriers to diabetes management (dietary and overall management) |
| Diet and Medication |
Non-adherence to recommended regimens was related with the following:
| [43] |
| Walker et al. | 2012 | USA | quantitative cross-sectional study | 378 patients with type 2 diabetes recruited from primary care clinics (117 male, and 261 female) Age: >18 years | To investigate the relation between diabetes fatalism and medication adherence and self-care behaviors (including diet, exercise and blood sugar testing) in patients with type 2 diabetes |
| Medication Self-care behaviors (diet, exercise, blood sugar testing) | Poor adherence to medication and self-care was related with diabetes fatalism | [44] |
| Goverwa | 2014 | Zimbabwe | quantitative cross-sectional study | 354 hypertensive patients on treatment from a hospital’s outpatient department with diagnosis of at least 6 months (132 male, and 222 female) Age: >18 years | To explore the prevalence of uncontrolled hypertension and the associated factors among hypertensive patients on treatment |
| Medication Salt intake Smoking alcohol | Health education and patients’ high perception of the associated risks leads to greater adherence to the regimen | [45] |
| Hardcastle et al. | 2015 | Australia | qualitative cross-sectional study | 18 patients who had received a genetic diagnosis for FH from a lipid disorders clinic involved in a genetic cascade screening program (10 male, and 8 female) Age (Mean ± SD): 50.2 ± 14.0 | To investigate FH patients’ perceptions towards adherence to medication and lifestyle changes |
| Lifestyle (diet, and physical activity) Medication | The lower the perceived seriousness of FH, the lower the adherence to lifestyle changes | [25] |
| Shawon et al. | 2016 | Bangladesh | quantitative cross-sectional study | 144 patients with type 2 diabetes attending a tertiary hospital (101 male, and 43 female) Age (Mean ± SD): 54.4 ± 11.7 | To explore the attitude towards diabetes and social and family support in patients with type II diabetes from Bangladesh |
| Diet Medication | The more positive the patients’ attitude towards diabetes management along with the social support, the greater the adherence | [26] |
| Jankowska-Polańska et al. | 2016 | Poland | quantitative cross-sectional study | 102 patients with hypertension (50 male, and 52 female) Age (Mean ± SD): 45.5 ± 7.7 | To evaluate the relationship between acceptance of illness and adherence to pharmacological and non-pharmacological therapy in hypertensive patients |
| Pharmacological and non-pharmacological treatment | The greater the illness acceptance, the greater the adherence | [47] |
| Long et al. | 2016 | USA | qualitative cross-sectional study | 34 male participants with hypertension, hyperlipidemia, or both conditions Age range: 40–65 | To investigate the knowledge, attitudes and beliefs of African American men, regarding the management of hypertension and hyperlipidemia |
| Diet Medication Exercise | Self-management Barriers:
| [48] |
| Herrera et al. | 2017 | Chile | qualitative cross-sectional study | 51 hypertensive patients with at least 1 month hypertensive medical treatment from two primary care public health institutions Age range: 25–80 | To understand hypertensive patients adherence and non-adherence to different types of treatment programs (diet, exercise, and medication) |
| Diet Medication Exercise | The higher the perceived significance of therapeutic treatment, the higher the adherence | [49] |
| Sarfo et al. | 2018 | Ghana | quantitative cross-sectional study | 2870 participants with hypertension with or without diabetes from hospitals (23.2% male, and 76.8% female) Age (Mean ± SD): 58.9 ± 16.6 | To investigate the causes of uncontrolled blood pressure in Ghanaian hypertensive patients focusing on improving the access to hypertension treatment |
| Medication Salt intake | The higher the degree to control the disease, the higher the adherence to therapeutic treatment | [27] |
| Espejo et al. | 2019 | USA | qualitative cross-sectional study | 21 African American participants with essential hypertension, on single or combined oral antihypertensive regimen (24% male, and 76% female) Age (Mean ± SD): 58.1 ± 10.1 | To investigate the knowledge, perception, and behaviors among African Americans with hypertension and interpret reasons behind poor blood pressure control |
| Diet Medication |
Low adherence of patients was attributed to the following:
| [28] |
| Henao López and Triviño Vargas | 2020 | Colombia | quantitative cross-sectional study | 128 patients with acute coronary syndrome who underwent percutaneous coronary angioplasty in a clinic in the last 3–4 months (84 male, and 44 female) Mean age: 65.12 | To investigate the relationship between adherence to secondary prevention and factors that impact the adherence in people with acute coronary syndrome, who have undergone percutaneous coronary angioplasty |
| Diet Medication | The higher the patients’ knowledge and perception of the adherence process, the higher the adherence | [29] |
| Alageel et al. | 2020 | UK | qualitative cross-sectional study | 22 participants that had received a health check in the last 6 months at NHS and were assessed at medium to high risk (>10% risk) of developing CVD in next 10 years (12 male, and 10 female) Age range: 40–74 | To investigate factors that possibly impact the engagement and adherence to lifestyle change interventions and medication in individuals with medium or high risk of CVD |
| Lifestyle Medication |
Low adherence was related with the following:
| [30] |
| Farooqi et al. | 2000 | UK | qualitative cross-sectional study | 44 participants with high risk of heart disease that had visited general practices (24 male, and 20 female) Age: >40 years | To explore the knowledge and attitudes of individuals with high risk for heart disease as regards to the lifestyle risk factors for CHD |
| Lifestyle (diet and exercise) |
| [37] |
| Thomas et al. | 2004 | UK | quantitative cross-sectional study | 406 diabetic patients that had visited the diabetes center of a hospital with mean diabetes duration being 10 years (224 male, and 182 female) Mean age: 56.5 years | To explore the perceived factors that prevent patients from engaging to more physical activity |
| Physical activity |
Barriers to low adherence to PA:
| [38] |
| Serour et al. | 2007 | Kuwait | quantitative cross-sectional study | 334 adults with hypertension, type 2 diabetes, or both (125 male, and 209 female) Age (Mean ± SD): 53.52 ± 10.36 | To understand the barriers to adherence to lifestyle changes |
| Lifestyle (diet and exercise) |
Main barriers to diet adherence:
| [22] |
| Darr et al. | 2008 | UK | qualitative cross-sectional study | 65 subjects from hospitals that had been diagnosed within the previous year with unstable angina or myocardial infraction, or coronary artery bypass surgery. (36 male, and 29 female) Age: >30 years | To evaluate and access the illness beliefs of patients with coronary heart disease (CHD) relating to causal attributions and lifestyle changes |
| Lifestyle | The higher the patients’ health beliefs, the higher the likelihood to adopt healthier lifestyle changes | [40] |
| Claassen et al. | 2010 | Netherlands | quantitative cross-sectional study | 81 participants diagnosed with FH traced in a nationwide family cascade screening program (48% male, and 52% female) Age (Mean ± SD): 48 ± 16 | To investigate the perceived risk and representations of CVD and preventative behaviors of individuals diagnosed with FH via DNA testing |
| Diet Physical activity | Incorrect risk perception was considered as a barrier to patients’ lifestyle changes | [31] |
| Ranasinghe et al. | 2015 | Sri Lanka | qualitative cross-sectional study | 50 patients with diabetes mellitus attending medical clinics (23 male, and 27 female) Age (Mean ± SD): 61.2 ± 9.9 | To examine the perception about diet and physical activity in adults with diabetes mellitus |
| Diet Physical activity | The higher the wrong perception on what constitutes a healthy diet, the lower the adherence | [46] |
| Pizzato Galdino et al. | 2016 | Brazil | quantitative cross-sectional study | 142 patients with cardiovascular risk who held their first nutritional consultation and had two or more cardiovascular risk factors (14.29% male, and 85.71% female) Age (Mean ± SD): 44.02 ± 13.33 | To evaluate the abandonment of dietary treatments of patients with cardiovascular risk treated on an outpatient basis and explore the causes for treatment non-adherence |
Telephone contact:
| Diet |
Non-adherence to treatment was related with the following:
| [32] |
| Craig and Kapysheva | 2018 | Kazakhstan | qualitative cross-sectional study | 122 patients with CVD and Type II diabetes from various clinics and hospitals throughout two regions of Kazakhstan that were currently being treated for health conditions, such as heart disease, hypertension, diabetes (46 male, and 76 female) Mean age: 53.7 | To recognize the perceived barriers to lifestyle changes |
Focus group discussions accessing
| diet and physical activity |
Low adherence to therapeutic protocol was attributed to:
| [33] |
| Gupta et al. | 2018 | Australia | qualitative cross-sectional study | 57 participants from hospitals, clinics and community groups with self-reported type 2 diabetes and/or CVD (29 male, 28 female) Age: >18 years | To evaluate and aggregate the perceptions and experiences of participants with type 2 diabetes and/or CVD regarding disease management through diet and dietary practices |
| Diet Physical activity |
Adherence was linked with:
| [34] |
| Moore et al. | 2018 | UK | qualitative cross-sectional study | 67 participants (overweight or obese, with high blood pressure and/or high cholesterol) at high CVD risk from Northern Europe (27 male, and 40 female) Age (Mean ± SD): 64.00 ± 10.00 | To explore the attitudes towards dietary change to the Mediterranean diet in persons with high CVD risk |
| Diet |
The higher the perceived CVD risk, the higher the adherence to dietary changes. Identified barriers:
| [35] |
| Finn et al. | 2022 | Ireland | quantitative cross-sectional study | 72 participants with T1DM for greater than 1 year (34 male, and 38 female) Age (Mean ± SD): 44.9 ± 12.9 | To evaluate the adherence to physical activity guidelines and relating barriers, and assess the relationship between accelerometer-measured PA and CVD risk factors |
| Physical activity |
Low adherence to PA was attributed to the following:
| [36] |
3.2. Adherence to Overall Treatment (Both Medication and Lifestyle Changes)
3.3. Adherence to Recommended Lifestyle Changes (Exclusively Studied)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention; CDC WONDER Online Database, National Center for Health Statistics. Underlying Cause of Death 1999–2018; Data are from the Multiple Cause of Death Files, 1999–2018, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- Tilson, H.H. Adherence or compliance? Changes in terminology. Ann. Pharmacother. 2004, 38, 161–162. [Google Scholar] [CrossRef]
- Sabaté, E.; Cluster, W. Adherence to Long-Term Therapies: Policy for Action: Meeting Report. 2001. Available online: https://apps.who.int/iris/handle/10665/66984 (accessed on 29 March 2023).
- Haynes, R.B. Determinants of Compliance: The Disease and the Mechanics of Treatment; Johns Hopkins University Press: Baltimore, MD, USA, 1979. [Google Scholar]
- Rand, C.S. Measuring adherence with therapy for chronic diseases: Implications for the treatment of heterozygous familial hypercholesterolemia. Am. J. Cardiol. 1993, 72, 68D–74D. [Google Scholar] [CrossRef] [PubMed]
- American Heart Association. The American Heart Association Diet and Lifestyle Recommendations; American Heart Association: Anchorage, AK, USA, 2021; Available online: https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/aha-diet-and-lifestyle-recommendations (accessed on 29 March 2023).
- United States Department of Agriculture. Dietary Guidelines for Americans 2020–2025; United States Department of Agriculture: Washington, DC, USA, 2020. Available online: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf (accessed on 29 March 2023).
- Ogungbe, O.; Byiringiro, S.; Adedokun-Afolayan, A.; Seal, S.M.; Dennison Himmelfarb, C.R.; Davidson, P.M.; Commodore-Mensah, Y. Medication Adherence Interventions for Cardiovascular Disease in Low- and Middle-Income Countries: A Systematic Review. Patient Prefer. Adherence 2021, 15, 885–897. [Google Scholar] [CrossRef] [PubMed]
- De Bacquer, D.; Astin, F.; Kotseva, K.; Pogosova, N.; De Smedt, D.; De Backer, G.; Rydén, L.; Wood, D.; Jennings, C. EUROASPIRE IV and V surveys of the European Observational Research Programme of the European Society of Cardiology. Poor adherence to lifestyle recommendations in patients with coronary heart disease: Results from the EUROASPIRE surveys. Eur. J. Prev. Cardiol. 2022, 29, 383–395. [Google Scholar] [CrossRef] [PubMed]
- European Society of Cardiology. Guidelines on Cardiovascular Disease Prevention in Clinical Practice ESC Clinical Practice Guidelines. 2021. Available online: https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/2021-ESC-Guidelines-on-cardiovascular-disease-prevention-in-clinical-practice (accessed on 29 March 2023).
- Lichtenstein, A.H.; Appel, L.J.; Vadiveloo, M.; Hu, F.B.; Kris-Etherton, P.M.; Rebholz, C.M.; Sacks, F.; Thorndike, A.N.; Van Horn, L.; Wylie-Rosett, J.; et al. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation 2021, 144, e472–e487. [Google Scholar] [CrossRef]
- World Health Organization. Diabetes Fact Sheet. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 29 March 2023).
- Galaviz, K.I.; Narayan, K.M.V.; Lobelo, F.; Weber, M.B. Lifestyle and the Prevention of Type 2 Diabetes: A Status Report. Am. J. Lifestyle Med. 2015, 12, 4–20. [Google Scholar] [CrossRef]
- Wändell, P.E.; de Waard, A.K.; Holzmann, M.J.; Gornitzki, C.; Lionis, C.; de Wit, N.; Søndergaardf, J.; Sønderlund, A.L.; Kral, N.; Seifert, B.; et al. Barriers and facilitators among health professionals in primary care to prevention of cardiometabolic diseases: A systematic review. Fam. Pract. 2018, 35, 383–398. [Google Scholar] [CrossRef]
- Sabaté, E. WHO Adherence Meeting Report; World Health Organization: Geneva, Switzerland, 2001.
- Krishnamoorthy, Y.; Rajaa, S.; Rehman, T.; Thulasingam, M. Patient and provider’s perspective on barriers and facilitators for medication adherence among adult patients with cardiovascular diseases and diabetes mellitus in India: A qualitative evidence synthesis. BMJ Open 2022, 12, e055226. [Google Scholar] [CrossRef]
- Piña, I.L.; Di Palo, K.E.; Brown, M.T.; Choudhry, N.K.; Cvengros, J.; Whalen, D.; Whitsel, L.P.; Johnson, J. Medication adherence: Importance, issues and policy: A policy statement from the American Heart Association. Prog. Cardiovasc. Dis. 2021, 64, 111–120. [Google Scholar] [CrossRef]
- Xu, H.Y.; Yu, Y.J.; Zhang, Q.H.; Hu, H.Y.; Li, M. Tailored Interventions to Improve Medication Adherence for Cardiovascular Diseases. Front. Pharmacol. 2020, 11, 510339. [Google Scholar] [CrossRef]
- Schneider, A.P.H.; Gaedke, M.Â.; Garcez, A.; Barcellos, N.T.; Paniz, V.M.V. Effect of characteristics of pharmacotherapy on non-adherence in chronic cardiovascular disease: A systematic review and meta-analysis of observational studies. Int. J. Clin. Pract. 2018, 72, e13044. [Google Scholar] [CrossRef] [PubMed]
- Ferdinand, K.C.; Senatore, F.F.; Clayton-Jeter, H.; Cryer, D.R.; Lewin, J.C.; Nasser, S.A.; Fiuzat, M.; Califf, R.M. Improving Medication Adherence in Cardiometabolic Disease: Practical and Regulatory Implications. J. Am. Coll. Cardiol. 2017, 69, 437–451. [Google Scholar] [CrossRef] [PubMed]
- Khunti, K.; Seidu, S.; Kunutsor, S.; Davies, M. Association Between Adherence to Pharmacotherapy and Outcomes in Type 2 Diabetes: A Meta-analysis. Diabetes Care 2017, 40, 1588–1596. [Google Scholar] [CrossRef] [PubMed]
- Serour, M.; Alqhenaei, H.; Al-Saqabi, S.; Mustafa, A.R.; Ben-Nakhi, A. Cultural factors and patients’ adherence to lifestyle measures. Br. J. Gen. Pract. 2007, 57, 291–295. [Google Scholar]
- Chiou, A.F.; Wang, H.L.; Chan, P.; Ding, Y.A.; Hsu, K.L.; Kao, H.L. Factors associated with behavior modification for cardiovascular risk factors in patients with coronary artery disease in northern Taiwan. J. Nurs. Res. JNR 2009, 17, 221–230. [Google Scholar] [CrossRef]
- Heydari, A.; Ahrari, S.; Vaghee, S. The relationship between self-concept and adherence to therapeutic regimens in patients with heart failure. J. Cardiovasc. Nurs. 2011, 26, 475–480. [Google Scholar] [CrossRef]
- Hardcastle, S.J.; Legge, E.; Laundy, C.S.; Egan, S.J.; French, R.; Watts, G.F.; Hagger, M.S. Patients’ perceptions and experiences of familial hypercholesterolemia, cascade genetic screening and treatment. Int. J. Behav. Med. 2015, 22, 92–100. [Google Scholar] [CrossRef]
- Shawon, M.S.; Hossain, F.B.; Adhikary, G.; Das Gupta, R.; Hashan, M.R.; Rabbi, M.F.; Ahsan, G.U. Attitude towards diabetes and social and family support among type 2 diabetes patients attending a tertiary-care hospital in Bangladesh: A cross-sectional study. BMC Res. Notes 2016, 9, 286. [Google Scholar] [CrossRef]
- Sarfo, F.S.; Mobula, L.M.; Burnham, G.; Ansong, D.; Plange-Rhule, J.; Sarfo-Kantanka, O.; Ofori-Adjei, D. Factors associated with uncontrolled blood pressure among Ghanaians: Evidence from a multicenter hospital-based study. PLoS ONE 2018, 13, e0193494. [Google Scholar] [CrossRef]
- Espejo, M.; Magabo, S.; Rivera-Castro, A.; Faiz, M.; Ramirez, L.; Robles, C.; Shabarek, T.; Shariff, M.A.; Kanna, B. Qualitative Study of Knowledge, Perception, and Behavior Related to Hypertension and Cardiovascular Disease Risk Reduction Among Hypertensive African-Americans in Urban Inner City of South Bronx, New York. J. Racial Ethn. Health Disparities 2019, 6, 197–206. [Google Scholar] [CrossRef]
- Henao López, V.; Triviño Vargas, Z. Adherence to Secondary Prevention and Influential Factors in Individuals with Coronary Angioplasty. Investig. Educ. Enfermería 2020, 38, e05. [Google Scholar] [CrossRef] [PubMed]
- Alageel, S.; Gulliford, M.C.; Wright, A.; Khoshaba, B.; Burgess, C. Engagement with advice to reduce cardiovascular risk following a health check programme: A qualitative study. Health Expect. 2020, 23, 193–201. [Google Scholar] [CrossRef]
- Claassen, L.; Henneman, L.; Kindt, I.; Marteau, T.M.; Timmermans, D.R. Perceived risk and representations of cardiovascular disease and preventive behaviour in people diagnosed with familial hypercholesterolemia: A cross-sectional questionnaire study. J. Health Psychol. 2010, 15, 33–43. [Google Scholar] [CrossRef]
- Galdino, T.P.; de Lima, V.C.O.; de Souza, I.M.; Fayh, P.T. Abandonment to therapeutic diet on patients at risk cardiovascular in a health care clinic. Nutr. Hosp. 2016, 33, 1400–1404. [Google Scholar] [CrossRef]
- Craig, B.J.; Kapysheva, A. Situated influences on perceived barriers to health behavior change: Cultural identity and context in Kazakhstan. Ethn. Health 2018, 23, 831–846. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.S.; Teede, H.; Aroni, R. Spicing up your advice for South Asian and Anglo-Australians with type 2 diabetes and CVD: Do cultural constructions of diet matter? Appetite 2018, 120, 679–697. [Google Scholar] [CrossRef]
- Moore, S.E.; McEvoy, C.T.; Prior, L.; Lawton, J.; Patterson, C.C.; Kee, F.; Cupples, M.; Young, I.S.; Appleton, K.; McKinley, M.C.; et al. Barriers to adopting a Mediterranean diet in Northern European adults at high risk of developing cardiovascular disease. J. Hum. Nutr. Diet. 2018, 31, 451–462. [Google Scholar] [CrossRef]
- Finn, M.; Sherlock, M.; Feehan, S.; Guinan, E.M.; Moore, K.B. Adherence to physical activity recommendations and barriers to physical activity participation among adults with type 1 diabetes. Ir. J. Med. Sci. 2022, 191, 1639–1646. [Google Scholar] [CrossRef]
- Farooqi, A.; Nagra, D.; Edgar, T.; Khunti, K. Attitudes to lifestyle risk factors for coronary heart disease amongst South Asians in Leicester: A focus group study. Fam. Pract. 2000, 17, 293–297. [Google Scholar] [CrossRef]
- Thomas, N.; Alder, E.; Leese, G.P. Barriers to physical activity in patients with diabetes. Postgrad. Med. J. 2004, 80, 287–291. [Google Scholar] [CrossRef]
- Thomas, C.M. The influence of self-concept on adherence to recommended health regimens in adults with heart failure. J. Cardiovasc. Nurs. 2007, 22, 405–416. [Google Scholar] [CrossRef]
- Darr, A.; Astin, F.; Atkin, K. Causal attributions, lifestyle change, and coronary heart disease: Illness beliefs of patients of South Asian and European origin living in the United Kingdom. Heart Lung 2008, 37, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Ruf, V.; Stewart, S.; Pretorius, S.; Kubheka, M.; Lautenschläger, C.; Presek, P.; Sliwa, K. Medication adherence, self-care behaviour and knowledge on heart failure in urban South Africa: The Heart of Soweto study. Cardiovasc. J. Afr. 2010, 21, 86–92. [Google Scholar] [PubMed]
- Iyalomhe, G.B.S.; Iyalomhe, S.I. Hypertension-related knowledge, attitudes and life-style practices among hypertensive patients in a sub-urban Nigerian community. J. Public Health Epidemiol. 2010, 2, 71–77. [Google Scholar]
- Singh, H.; Cinnirella, M.; Bradley, C. Support systems for and barriers to diabetes management in South Asians and Whites in the UK: Qualitative study of patients’ perspectives. BMJ Open 2012, 2, e001459. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.J.; Smalls, B.L.; Hernandez-Tejada, M.A.; Campbell, J.A.; Davis, K.S.; Egede, L.E. Effect of diabetes fatalism on medication adherence and self-care behaviors in adults with diabetes. Gen. Hosp. Psychiatry 2012, 34, 598–603. [Google Scholar] [CrossRef]
- Goverwa, T.P.; Masuka, N.; Tshimanga, M.; Gombe, N.T.; Takundwa, L.; Bangure, D.; Wellington, M. Uncontrolled hypertension among hypertensive patients on treatment in Lupane District, Zimbabwe, 2012. BMC Res. Notes 2014, 7, 703. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Pigera, A.S.; Ishara, M.H.; Jayasekara, L.M.; Jayawardena, R.; Katulanda, P. Knowledge and perceptions about diet and physical activity among Sri Lankan adults with diabetes mellitus: A qualitative study. BMC Public Health 2015, 15, 1160. [Google Scholar] [CrossRef]
- Jankowska-Polańska, B.; Blicharska, K.; Uchmanowicz, I.; Morisky, D. The influence of illness acceptance on the adherence to pharmacological and non-pharmacological therapy in patients with hypertension. Eur. J. Cardiovasc. Nurs. 2016, 15, 559–568. [Google Scholar] [CrossRef]
- Long, E.; Ponder, M.; Bernard, S. Knowledge, attitudes, and beliefs related to hypertension and hyperlipidemia self-management among African-American men living in the southeastern United States. Patient Educ. Couns. 2016, 100, 1000–1006. [Google Scholar] [CrossRef]
- Herrera, P.A.; Moncada, L.; Defey, D. Understanding Non-Adherence From the Inside: Hypertensive Patients’ Motivations for Adhering and Not Adhering. Qual. Health Res. 2017, 27, 1023–1034. [Google Scholar] [CrossRef] [PubMed]
- Neill, J. Definitions of Various Self Constructs: Self-Esteem, Self-Efficacy, Self-Confidence & Self-Concept; Wilderdom: New Delhi, India, 2005. [Google Scholar]
- Kvarnström, K.; Westerholm, A.; Airaksinen, M.; Liira, H. Factors Contributing to Medication Adherence in Patients with a Chronic Condition: A Scoping Review of Qualitative Research. Pharmaceutics 2021, 13, 1100. [Google Scholar] [CrossRef] [PubMed]
- Hultgren, F.; Jonasson, G.; Billhult, A. From resistance to rescue--patients’ shifting attitudes to antihypertensives: A qualitative study. Scand. J. Prim. Health Care 2014, 32, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Rimando, M. Perceived barriers to and facilitators of hypertension management among underserved African-American older adults. Ethn. Dis. 2015, 25, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.A.; Smith, S.M.; Hart, N.; Cupples, M.E. Do practitioners and friends support patients with coronary heart disease in lifestyle change? a qualitative study. BMC Fam. Pract. 2013, 14, 126. [Google Scholar] [CrossRef]
- Gupta, C.; Bell, S.P.; Schildcrout, J.S.; Fletcher, S.; Goggins, K.M.; Kripalani, S. Vanderbilt Inpatient Cohort Study (VICS). Predictors of health care system and physician distrust in hospitalized cardiac patients. J. Health Commun. 2014, 2, 44–60. [Google Scholar] [CrossRef]
- Pizga, A.; Karatzanos, E.; Tsikrika, S.; Gioni, V.; Vasileiadis, I.; Nanas, S.; Kordoutis, P. Psychosocial Interventions to Enhance Treatment Adherence to Lifestyle Changes in Cardiovascular Disease: A Review of the Literature 2011–2021. Eur. J. Environ. Public Health 2022, 6, em0102. [Google Scholar]
- Tarn, D.M.; Barrientos, M.; Pletcher, M.J.; Cox, K.; Turner, J.; Fernandez, A.; Schwartz, J.B. Perceptions of Patients with Primary Nonadherence to Statin Medications. J. Am. Board Fam. Med. 2021, 34, 123–131. [Google Scholar] [CrossRef]
- Murray, J.; Grania, F.; Honey, S.; Bara, A.C.; Hill, K.M.; House, A. A qualitative synthesis of factors influencing maintenance of lifestyle behaviour change in individuals with high cardiovascular risk. BMC Cardiovasc. Disord. 2013, 13, 48. [Google Scholar] [CrossRef]
- Murray, J.; Craigs, C.; Hill, K.; Honey, S.; House, A. A systematic review of patient reported factors associated with uptake and completion of cardiovascular lifestyle behaviour change. BMC Cardiovasc. Disord. 2012, 12, 120. [Google Scholar] [CrossRef]
- Urke, E.B.; Søbye, S.; Ellingvåg, A.; Langslet, G.; Retterstøl, K.; Wandel, M. Familial hypercholesterolemia and young patients’ thoughts on own condition and treatment. Patient Educ. Couns. 2019, 102, 1005–1012. [Google Scholar] [CrossRef]
- Amankwah-Poku, M. Wavering Diabetic Diet: “I Break the Diet and Then I Feel Guilty and Then I Don’t Go Back to It, In Case I Feel Guilty Again”. SAGE Open 2020, 10, 2158244020914577. [Google Scholar] [CrossRef]
- Yildirim, D.; Baykal, D. Evaluation of treatment adherence and illness perception in cardiology patients. Niger. J. Clin. Pract. 2020, 23, 1305–1311. [Google Scholar] [CrossRef] [PubMed]
- Grace, C.; Begum, R.; Subhani, S.; Kopelman, P.; Greenhalgh, T. Prevention of type 2 diabetes in British Bangladeshis: Qualitative study of community, religious, and professional perspectives. BMJ 2008, 337, a1931. [Google Scholar] [CrossRef] [PubMed]
- Shobana, R.; Augustine, C.; Ramachandran, A.; Vijay, V. Improving psycho-social care: The Indian experience. Diabetes Voice 2005, 50, 19–21. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalantzi, V.; Kalafati, I.P.; Belitsi, V.; Tsiampalis, T.; Koutsonasios, I.; Androutsos, O.; Bonoti, F.; Panagiotakos, D.B.; Kosti, R.I. Cardiometabolic Patient-Related Factors Influencing the Adherence to Lifestyle Changes and Overall Treatment: A Review of the Recent Literature. Life 2023, 13, 1153. https://doi.org/10.3390/life13051153
Kalantzi V, Kalafati IP, Belitsi V, Tsiampalis T, Koutsonasios I, Androutsos O, Bonoti F, Panagiotakos DB, Kosti RI. Cardiometabolic Patient-Related Factors Influencing the Adherence to Lifestyle Changes and Overall Treatment: A Review of the Recent Literature. Life. 2023; 13(5):1153. https://doi.org/10.3390/life13051153
Chicago/Turabian StyleKalantzi, Vasiliki, Ioanna Panagiota Kalafati, Vasiliki Belitsi, Thomas Tsiampalis, Ioannis Koutsonasios, Odysseas Androutsos, Fotini Bonoti, Demosthenes B. Panagiotakos, and Rena I. Kosti. 2023. "Cardiometabolic Patient-Related Factors Influencing the Adherence to Lifestyle Changes and Overall Treatment: A Review of the Recent Literature" Life 13, no. 5: 1153. https://doi.org/10.3390/life13051153
APA StyleKalantzi, V., Kalafati, I. P., Belitsi, V., Tsiampalis, T., Koutsonasios, I., Androutsos, O., Bonoti, F., Panagiotakos, D. B., & Kosti, R. I. (2023). Cardiometabolic Patient-Related Factors Influencing the Adherence to Lifestyle Changes and Overall Treatment: A Review of the Recent Literature. Life, 13(5), 1153. https://doi.org/10.3390/life13051153







