Gut Microbiota Dysbiosis in Diabetic Retinopathy—Current Knowledge and Future Therapeutic Targets
Abstract
1. Introduction
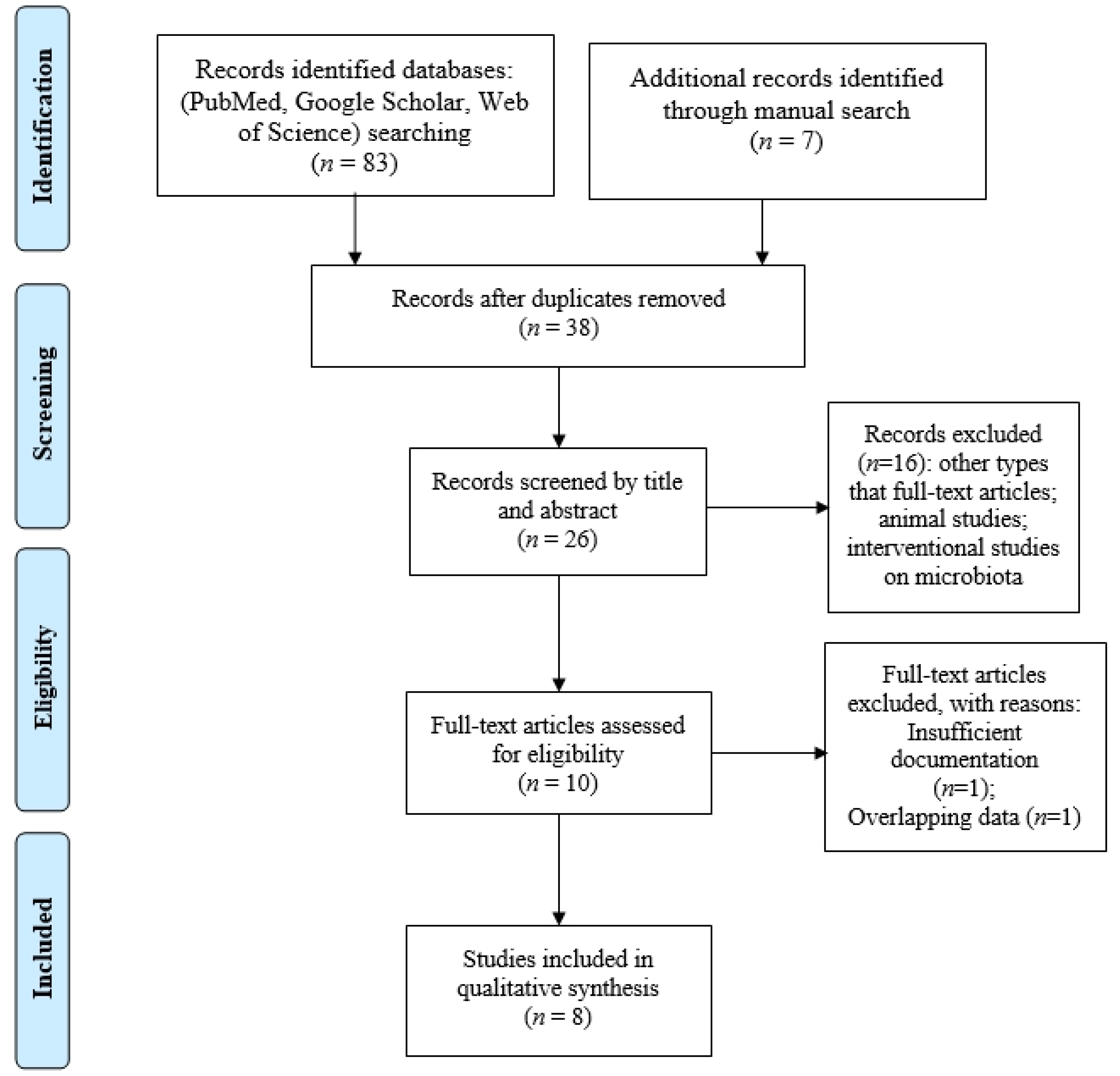
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Data Extraction and Analysis
3. Results
3.1. General Characteristics of the Included Studies
3.2. Richness and Diversity Changes in the Gut Microbiome in DR vs. T2DM and HC
3.3. Changes at Phylum, Genera, and Species Levels
4. Discussion
4.1. SCFA Producers
4.2. Akkermansiaceae and A. muciniphila
4.3. Tauroursodeoxycholic Acid (TUDCA)-Producing Species
4.4. Probiotics and DR
4.5. “Leaky Gut” and LPS Endotoxemia
4.6. Metabolic Changes Related to Gut Dysbiosis in DR
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hong, J.; Fu, T.; Liu, W.; Du, Y.; Min, C.; Lin, D. Specific alterations of gut microbiota in diabetic microvascular complications: A systematic review and meta-analysis. Front. Endocrinol. 2022, 13, 1053900. [Google Scholar] [CrossRef]
- Saeedi, P.; Salpea, P.; Karuranga, S.; Petersohn, I.; Malanda, B.; Gregg, E.W.; Unwin, M.; Wild, S.H.; Williams, R. Mortality attributable to diabetes in 20–79 years old adults 2019 estimates: Results from the international diabetes federation diabetes atlas. Diabetes Res. Clin. Pract. 2020, 162, 108086. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.S.; Aiello, L.; Gardner, T.W.; King, G.L.; Blankenship, G.; Cavallerano, J.D.; Ferris, F.L., 3rd; Klein, R.; American Diabetes Association. Retinopathy indiabetes. Diabetes Care 2004, 27 (Suppl. S1), S84–S87. [Google Scholar] [CrossRef] [PubMed]
- Serban, D.; Papanas, N.; Dascalu, A.M.; Stana, D.; Nicolae, V.A.; Vancea, G.; Badiu, C.D.; Tanasescu, D.; Tudor, C.; Balasescu, S.A.; et al. Diabetic Retinopathy in Patients with Diabetic Foot Ulcer: A Systematic Review. Int. J. Low. Extrem. Wounds 2021, 20, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Leasher, J.L.; Bourne, R.R.; Flaxman, S.R.; Jonas, J.B.; Keeffe, J.; Naidoo, K.; Pesudovs, K.; Price, H.; White, R.A.; Wong, T.Y.; et al. Global estimates on the number of people blind or visually impaired by diabetic retinopathy: A meta-analysis from 1990 to 2010. Diabetes Care 2016, 39, 1643–1649. [Google Scholar] [CrossRef]
- Kowluru, R.A.; Chan, P.S. Oxidative stress and diabetic retinopathy. Exp. Diabetes Res. 2007, 2007, 43603. [Google Scholar] [CrossRef]
- Kang, Q.; Yang, C. Oxidative stress and diabetic retinopathy: Molecular mechanisms, pathogenetic role and therapeutic implications. Redox Biol. 2020, 37, 101799. [Google Scholar] [CrossRef]
- Dascalu, A.M.; Stoian, A.P.; Cherecheanu, A.P.; Serban, D.; Costea, D.O.; Tudosie, M.S.; Stana, D.; Tanasescu, D.; Sabau, A.D.; Gangura, G.A.; et al. Outcomes of Diabetic Retinopathy Post-Bariatric Surgery in Patients with Type 2 Diabetes Mellitus. J. Clin. Med. 2021, 10, 3736. [Google Scholar] [CrossRef]
- Serban, D.; Papanas, N.; Dascalu, A.M.; Kempler, P.; Raz, I.; Rizvi, A.A.; Rizzo, M.; Tudor, C.; Silviu Tudosie, M.; Tanasescu, D.; et al. Significance of Neutrophil to Lymphocyte Ratio [NLR] and Platelet Lymphocyte Ratio [PLR] in Diabetic Foot Ulcer and Potential New Therapeutic Targets. Int. J. Low. Extrem. Wounds 2021. [Google Scholar] [CrossRef]
- Floyd, J.L.; Grant, M.B. The Gut-Eye Axis: Lessons Learned from Murine Models. Ophthalmol. Ther. 2020, 9, 499–513. [Google Scholar] [CrossRef]
- Bai, X.; Xu, Q.; Zhang, W.; Wang, C. The Gut–Eye Axis: Correlation Between the Gut Microbiota and Autoimmune Dry Eye in Individuals with Sjögren Syndrome. Eye Contact Lens Sci. Clin. Pract. 2023, 49, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Scuderi, G.; Troiani, E.; Minnella, A.M. Gut Microbiome in Retina Health: The Crucial Role of the Gut-Retina Axis. Front. Microbiol. 2022, 12, 726792. [Google Scholar] [CrossRef] [PubMed]
- Jiao, J.; Yu, H.; Yao, L.; Li, L.; Yang, X.; Liu, L. Recent Insights into the Role of Gut Microbiota in Diabetic Retinopathy. J. Inflamm. Res. 2021, 14, 6929–6938. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.R.; Shin, J.; Guevarra, R.; Lee, J.H.; Kim, D.W.; Seol, K.H.; Lee, J.H.; Kim, H.B.; Isaacson, R. Deciphering Diversity Indices for a Better Understanding of Microbial Communities. J. Microbiol. Biotechnol. 2017, 27, 2089–2093. [Google Scholar] [CrossRef] [PubMed]
- Rowan, S.; Taylor, A. The Role of Microbiota in Retinal Disease. Adv. Exp. Med. Biol. 2018, 1074, 429–435. [Google Scholar] [CrossRef]
- Rowan, S.; Jiang, S.; Korem, T.; Szymanski, J.; Chang, M.L.; Szelog, J.; Cassalman, C.; Dasuri, K.; McGuire, C.; Nagai, R.; et al. Involvement of a gut-retina axis in protection against dietary glycemia-induced age-related macular degeneration. Proc. Natl. Acad. Sci. USA 2017, 114, E4472–E4481. [Google Scholar] [CrossRef]
- Shivaji, S. A systematic review of gut microbiome and ocular inflammatory diseases: Are they associated? Ind. J. Ophthalmol. 2021, 69, 535–542. [Google Scholar] [CrossRef]
- Ye, P.; Zhang, X.; Xu, Y.; Xu, J.; Song, X.; Yao, K. Alterations of the gut microbiome and metabolome in patients with proliferative diabetic retinopathy. Front. Microbiol. 2021, 12, 667632. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, Z.; Ma, H.; Ji, S.; Chen, Z.; Cui, Z.; Chen, J.; Tang, S. Dysbiosis and Implication of the Gut Microbiota in Diabetic Retinopathy. Front. Cell Infect. Microbiol. 2021, 11, 646348. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale [N.O.S.] for Assessing the Quality of Nonrandomized Studies in Meta-Analyses; The Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2011; Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 28 February 2023).
- Zhou, Z.; Zheng, Z.; Xiong, X.; Chen, X.; Peng, J.; Yao, H.; Zheng, M. Gut microbiota composition and fecal metabolic profiling in patients with diabetic retinopathy. Front. Cell Dev. Biol. 2021, 9, 732204. [Google Scholar] [CrossRef]
- Bai, J.; Wan, Z.; Zhang, Y.; Wang, T.; Xue, Y.; Peng, Q. Composition and diversity of gut microbiota in diabetic retinopathy. Front. Microbiol. 2022, 13, 926926. [Google Scholar] [CrossRef] [PubMed]
- Das, T.; Jayasudha, R.; Chakravarthy, S.; Prashanthi, G.S.; Bhargava, A.; Tyagi, M.; Rani, P.K.; Pappuru, R.R.; Sharma, S.; Shivaji, S. Alterations in the gut bacterial microbiome in people with type 2 diabetes mellitus and diabetic retinopathy. Sci. Rep. 2021, 11, 2738. [Google Scholar] [CrossRef] [PubMed]
- Moubayed, N.M.; Bhat, R.S.; Al Farraj, D.; Dihani, N.A.; El Ansary, A.; Fahmy, R.M. Screening and identification of gut anaerobes [Bacteroidetes] from human diabetic stool samples with and without retinopathy in comparison to control subjects. Microb. Pathog. 2019, 129, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Yang, K.; Li, C.; Zhang, H.; Yu, H.; Chen, K.; Yang, X.; Liu, L. Metagenomic shotgun sequencing and metabolomic profiling identify specific human gut microbiota associated with diabetic retinopathy in patients with type 2 diabetes. Front. Immunol. 2022, 13, 943325. [Google Scholar] [CrossRef] [PubMed]
- Khan, R.; Sharma, A.; Ravikumar, R.; Parekh, A.; Srinivasan, R.; George, R.J.; Raman, R. Association Between Gut Microbial Abundance and Sight-Threatening Diabetic Retinopathy. Invest. Ophthalmol. Vis. Sci. 2021, 62, 19. [Google Scholar] [CrossRef]
- Liu, W.; Zhang, R.; Shu, R.; Yu, J.; Li, H.; Long, H.; Jin, S.; Li, S.; Hu, Q.; Yao, F.; et al. Study of the Relationship between Microbiome and Colorectal Cancer Susceptibility Using 16SrRNA Sequencing. Biomed. Res. Int. 2020, 2020, 7828392. [Google Scholar] [CrossRef]
- Wagner, B.D.; Grunwald, G.K.; Zerbe, G.O.; Mikulich-Gilbertson, S.K.; Robertson, C.E.; Zemanick, E.T.; Harris, J.K. On the Use of Diversity Measures in Longitudinal Sequencing Studies of Microbial Communities. Front. Microbiol. 2018, 9, 1037. [Google Scholar] [CrossRef]
- Van Hul, M.; Le Roy, T.; Prifti, E.; Dao, M.C.; Paquot, A.; Zucker, J.D.; Delzenne, N.M.; Muccioli, G.; Clément, K.; Cani, P.D. From correlation to causality: The case of Subdoligranulum. Gut Microbes 2020, 12, 1849998. [Google Scholar] [CrossRef]
- Dang, F.; Jiang, Y.; Pan, R.; Zhou, Y.; Wu, S.; Wang, R.; Zhuang, K.; Li, T.; Man, C. Administration of lactobacillus paracasei ameliorates type 2 diabetes in mice. Food Funct. 2018, 9, 3630–3639. [Google Scholar] [CrossRef]
- Malinen, E.; Krogius-Kurikka, L.; Lyra, A.; Nikkilä, J.; Jääskeläinen, A.; Rinttilä, T.; Vilpponen-Salmela, T.; von Wright, A.J.; Palva, A. Association of symptoms with gastrointestinal microbiota in irritable bowel syndrome. World J. Gastroenterol. 2010, 16, 4532–4540. [Google Scholar] [CrossRef]
- Deaver, J.A.; Eum, S.Y.; Toborek, M. Circadian Disruption Changes Gut Microbiome Taxa and Functional Gene Composition. Front. Microbiol. 2018, 9, 737. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Q.; Cen, S.; Jiang, J.; Zhao, J.; Zhang, H.; Chen, W. Disturbance of trace element and gut microbiota profiles as indicators of autism spectrum disorder: A pilot study of Chinese children. Environ. Res. 2019, 171, 501–509. [Google Scholar] [CrossRef]
- Yang, J.; Li, Y.; Wen, Z.; Liu, W.; Meng, L.; Huang, H. Oscillospira—A candidate for the next-generation probiotics. Gut Microbes 2021, 13, 1987783. [Google Scholar] [CrossRef] [PubMed]
- Waters, J.L.; Ley, R.E. The human gut bacteria Christensenellaceae are widespread, heritable, and associated with health. BMC Biol. 2019, 17, 83. [Google Scholar] [CrossRef] [PubMed]
- Brooks, A.W.; Priya, S.; Blekhman, R.; Bordenstein, S.R. Gut microbiota diversity across ethnicities in the United States. PLoS Biol. 2018, 16, e2006842. [Google Scholar] [CrossRef]
- He, X.; Sun, J.; Liu, C.; Yu, X.; Li, H.; Zhang, W.; Li, Y.; Geng, Y.; Wang, Z. Compositional Alterations of Gut Microbiota in Patients with Diabetic Kidney Disease and Type 2 Diabetes Mellitus. Diabetes Metab. Syndr. Obes. 2022, 15, 755–765. [Google Scholar] [CrossRef]
- Nam, J.H.; Yun, Y.; Kim, H.S.; Kim, H.N.; Jung, H.J.; Chang, Y.; Ryu, S.; Shin, H.; Kim, H.L.; Kim, W.S. Rosacea and its association with enteral microbiota in Korean females. Exp. Dermatol. 2018, 27, 37–42. [Google Scholar] [CrossRef]
- Shimizu, J.; Kubota, T.; Takada, E.; Takai, K.; Fujiwara, N.; Arimitsu, N.; Ueda, Y.; Wakisaka, S.; Suzuki, T.; Suzuki, N. Relative abundance of Megamonas hypermegale and Butyrivibrio species decreased in the intestine and its possible association with the T cell aberration by metabolite alteration in patients with Behcet’s disease [210 characters]. Clin. Rheumatol. 2019, 38, 1437–1445. [Google Scholar] [CrossRef]
- Gough, E.K.; Stephens, D.A.; Moodie, E.E.; Prendergast, A.J.; Stoltzfus, R.J.; Humphrey, J.H.; Manges, A.R. Linear growth faltering in infants is associated with Acidaminococcus sp. and community-level changes in the gut microbiota. Microbiome 2015, 3, 24. [Google Scholar] [CrossRef]
- Morinaga, K.; Kusada, H.; Tamaki, H. Bile Salt Hydrolases with Extended Substrate Specificity Confer a High Level of Resistance to Bile Toxicity on Atopobiaceae Bacteria. Int. J. Mol. Sci. 2022, 23, 10980. [Google Scholar] [CrossRef]
- Larsen, J.M. The immune response to Prevotella bacteria in chronic inflammatory disease. Immunology 2017, 151, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Ezeji, J.C.; Sarikonda, D.K.; Hopperton, A.; Erkkila, H.L.; Cohen, D.E.; Martinez, S.P.; Cominelli, F.; Kuwahara, T.; Dichosa, A.E.K.; Good, C.E.; et al. Parabacteroides distasonis: Intriguing aerotolerant gut anaerobe with emerging antimicrobial resistance and pathogenic and probiotic roles in human health. Gut Microbes 2021, 13, 1922241. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.T.; Chen, J.W. Direct CCL4 Inhibition Modulates Gut Microbiota, Reduces Circulating Trimethylamine N-Oxide, and Improves Glucose and Lipid Metabolism in High-Fat-Diet-Induced Diabetes Mellitus. J. Inflamm. Res. 2021, 14, 6237–6250. [Google Scholar] [CrossRef]
- Kim, J.; Choi, S.H.; Kim, Y.J.; Jeong, H.J.; Ryu, J.S.; Lee, H.J.; Kim, T.W.; Im, S.-H.; Oh, J.Y.; Kim, M.K. Clinical Effect of IRT-5 Probiotics on Immune Modulation of Autoimmunity or Alloimmunity in the Eye. Nutrients 2017, 9, 1166. [Google Scholar] [CrossRef] [PubMed]
- Prasad, R.; Asare-Bediko, B.; Harbour, A.; Floyd, J.L.; Chakraborty, D.; Duan, Y.; Lamendella, R.; Wright, J.; Grant, M.B. Microbial Signatures in The Rodent Eyes with Retinal Dysfunction and Diabetic Retinopathy. Investig. Ophthalmol. Vis. Sci. 2022, 63, 5. [Google Scholar] [CrossRef]
- Ioniță-Mîndrican, C.B.; Ziani, K.; Mititelu, M.; Oprea, E.; Neacșu, S.M.; Moroșan, E.; Dumitrescu, D.E.; Roșca, A.C.; Drăgănescu, D.; Negrei, C. Therapeutic Benefits and Dietary Restrictions of Fiber Intake: A State of the Art Review. Nutrients 2022, 14, 2641. [Google Scholar] [CrossRef]
- Statovci, D.; Aguilera, M.; MacSharry, J.; Melgar, S. The Impact of Western Diet and Nutrients on the Microbiota and Immune Response at Mucosal Interfaces. Front. Immunol. 2017, 8, 838. [Google Scholar] [CrossRef]
- Desjardins, D.; Liu, Y.; Crosson, C.E.; Ablonczy, Z. Histone Deacetylase Inhibition Restores Retinal Pigment Epithelium Function in Hyperglycemia. PLoS ONE 2016, 11, e0162596. [Google Scholar] [CrossRef]
- Dewanjee, S.; Dua, T.K.; Paul, P.; Dey, A.; Vallamkondu, J.; Samanta, S.; Kandimalla, R.; De Feo, V. Probiotics: Evolving as a Potential Therapeutic Option against Acetaminophen-Induced Hepatotoxicity. Biomedicines 2022, 10, 1498. [Google Scholar] [CrossRef]
- Chen, N.; Wu, J.; Wang, J.; Piri, N.; Chen, F.; Xiao, T.; Zhao, Y.; Sun, D.; Kaplan, H.J.; Shao, H. Short chain fatty acids inhibit endotoxin-induced uveitis and inflammatory responses of retinal astrocytes. Exp. Eye Res. 2021, 206, 108520. [Google Scholar] [CrossRef]
- Chen, S.; Wang, Y.; Liu, Y.; Li, F.; Chen, Y.; Fang, X.; Wen, T.; Xu, S.; Kermany, D.; Deng, S.; et al. Dysbiosis of gut microbiome contributes to glaucoma pathogenesis. MedComm—Future Med. 2022, 1, e28. [Google Scholar] [CrossRef]
- Shang, J.; Liu, F.; Zhang, B.; Dong, K.; Lu, M.; Jiang, R.; Xu, Y.; Diao, L.; Zhao, J.; Tanh, H. Liraglutide-induced structural modulation of the gut microbiota in patients with type 2 diabetes mellitus. PeerJ 2021, 9, e11128. [Google Scholar] [CrossRef]
- Zhao, L.; Chen, Y.; Xia, F.; Abudukerimu, B.; Zhang, W.; Guo, Y.; Wang, N.; Lu, Y. A glucagon-like peptide-1 receptor agonist lowers weight by modulating the structure of gut microbiota. Front. Endocrinol. 2018, 9, 233. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; Li, D.; He, Y.; Li, Y.; Yang, Z.; Zhao, X.; Liu, Y.; Wang, Y.; Sun, J.; Feng, X.; et al. Discrepant gut microbiota markers for the classification of obesity-related metabolic abnormalities. Sci. Rep. 2019, 9, 13424. [Google Scholar] [CrossRef] [PubMed]
- Therdtatha, P.; Song, Y.; Tanaka, M.; Mariyatun, M.; Almunifah, M.; Manurung, N.E.P.; Indriarsih, S.; Lu, Y.; Nagata, K.; Fukami, K.; et al. Gut Microbiome of Indonesian Adults Associated with Obesity and Type 2 Diabetes: A Cross-Sectional Study in an Asian City, Yogyakarta. Microorganisms 2021, 9, 897. [Google Scholar] [CrossRef]
- Zhang, F.; Yue, L.; Fang, X.; Wang, G.; Li, C.; Sun, X.; Jia, X.; Yang, J.; Song, J.; Zhang, Y.; et al. Altered gut microbiota in Parkinson’s disease patients/healthy spouses and its association with clinical features. Parkinsonism Relat. Disord. 2020, 81, 84–88. [Google Scholar] [CrossRef]
- Cao, C.; Liu, M.; Qu, S.; Huang, R.; Qi, M.; Zhu, Z.; Zheng, J.; Chen, Z.; Wang, Z.; Han, Z.; et al. Chinese medicine formula kai-xin-san ameliorates depression-like behaviours in chronic unpredictable mild stressed mice by regulating gut microbiota-inflammation-stress system. J. Ethnopharmacol. 2020, 261, 113055. [Google Scholar] [CrossRef]
- Wang, Y.; Ye, X.; Ding, D.; Lu, Y. Characteristics of the intestinal flora in patients with peripheral neuropathy associated with type 2 diabetes. J. Int. Med. Res. 2020, 48, 0300060520936806. [Google Scholar] [CrossRef]
- Derrien, M.; Belzer, C.; de Vos, W.M. Akkermansia muciniphila and its role in regulating host functions. Microb. Pathog. 2017, 106, 171–181. [Google Scholar] [CrossRef]
- Everard, A.; Lazarevic, V.; Derrien, M.; Girard, M.; Muccioli, G.M.; Neyrinck, A.M.; Possemiers, S.; Van, H.A.; Francois, P.; de Vos, W.M.; et al. Responses of gut microbiota and glucose and lipid metabolism to prebiotics in genetic obese and diet-induced leptin-resistant mice. Diabetes 2011, 60, 2775–2786. [Google Scholar] [CrossRef]
- Depommier, C.; Everard, A.; Druart, C.; Plovier, H.; Van Hul, M.; Vieira-Silva, S.; Falony, G.; Raes, J.; Maiter, D.; Delzenne, N.M.; et al. Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: A proof-of-concept exploratory study. Nat. Med. 2019, 25, 1096–1103. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, Y.; Kim, Y.; Seo, Y.; Lee, H.; Ha, J.; Lee, J.; Choi, Y.; Oh, H.; Yoon, Y. Akkermansia muciniphila Prevents Fatty Liver Disease, Decreases Serum Triglycerides, and Maintains Gut Homeostasis. Appl. Environ. Microbiol. 2020, 86, e03004–e03019. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, H.D.; Gerhard, G.S. Bile Acids Induce Neurite Outgrowth in Nsc-34 Cells via TGR5 and a Distinct Transcriptional Profile. Pharmaceuticals 2023, 16, 174. [Google Scholar] [CrossRef]
- Beli, E.; Yan, Y.; Moldovan, L.; Vieira, C.P.; Gao, R.; Duan, Y.; Prasad, R.; Bhatwadekar, A.; White, F.A.; Townsend, S.D.; et al. Restructuring of the Gut Microbiome by Intermittent Fasting Prevents Retinopathy and Prolongs Survival in db/db Mice. Diabetes 2018, 67, 1867–1879. [Google Scholar] [CrossRef]
- Cho, J.G.; Lee, J.H.; Hong, S.H.; Lee, H.N.; Kim, C.M.; Kim, S.Y.; Yoon, K.J.; Oh, B.J.; Kim, J.H.; Jung, S.Y.; et al. Tauroursodeoxycholic acid, a bile acid, promotes blood vessel repair by recruiting vasculogenic progenitor cells. Stem Cells 2015, 33, 792–805. [Google Scholar] [CrossRef]
- Iovieno, A.; Lambiase, A.; Sacchetti, M.; Stampachiacchiere, B.; Micera, A.; Bonini, S. Preliminary evidence of the efficacy of probiotic eye-drop treatment in patients with vernal keratoconjunctivitis. Graefes Arch. Clin. Exp. Ophthalmol. 2008, 246, 435–441. [Google Scholar] [CrossRef]
- Morita, Y.; Miwa, Y.; Jounai, K.; Fujiwara, D.; Kurihara, T.; Kanauchi, O. Lactobacillus paracasei KW3110 Prevents Blue Light-Induced Inflammation and Degeneration in the Retina. Nutrients 2018, 10, 1991. [Google Scholar] [CrossRef]
- Serban, D.; Popa Cherecheanu, A.; Dascalu, A.M.; Socea, B.; Vancea, G.; Stana, D.; Smarandache, G.C.; Sabau, A.D.; Costea, D.O. Hypervirulent Klebsiella pneumoniae Endogenous Endophthalmitis—A Global Emerging Disease. Life 2021, 11, 676. [Google Scholar] [CrossRef]
- Fernandes, R.; Viana, S.D.; Nunes, S.; Reis, F. Diabetic gut microbiota dysbiosis as an inflammaging and immunosenescence condition that fosters progression of retinopathy and nephropathy. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 1876–1897. [Google Scholar] [CrossRef]
- Vagaja, N.N.; Binz, N.; McLenachan, S.; Rakoczy, E.P.; McMenamin, P.G. Influence of endotoxin-mediated retinal inflammation on phenotype of diabetic retinopathy in Ins2 Akita mice. Br. J. Ophthalmol. 2013, 97, 1343–1350. [Google Scholar] [CrossRef]
- Orihuela, R.; McPherson, C.A.; Harry, G.J. Microglial M1/M2 polarization and metabolic states. Br. J. Pharmacol. 2016, 173, 649–665. [Google Scholar] [CrossRef] [PubMed]
- Lv, Q.; Li, Z.; Sui, A.; Yang, X.; Han, Y.; Yao, R. The role and mechanisms of gut microbiota in diabetic nephropathy, diabetic retinopathy and cardiovascular diseases. Front. Microbiol. 2022, 13, 977187. [Google Scholar] [CrossRef] [PubMed]
- Yam, M.; Engel, A.L.; Wang, Y.; Zhu, S.; Hauer, A.; Zhang, R.; Lohner, D.; Huang, J.; Dinterman, M.; Zhao, C.; et al. Proline mediates metabolic communication between retinal pigment epithelial cells and the retina. J. Biol. Chem. 2019, 294, 10278–10289. [Google Scholar] [CrossRef]
- Maiuolo, J.; Carresi, C.; Gliozzi, M.; Mollace, R.; Scarano, F.; Scicchitano, M.; Macrì, R.; Nucera, S.; Bosco, F.; Oppedisano, F.; et al. The Contribution of Gut Microbiota and Endothelial Dysfunction in the Development of Arterial Hypertension in Animal Models and in Humans. Int. J. Mol. Sci. 2022, 23, 3698. [Google Scholar] [CrossRef] [PubMed]
- Elbere, I.; Kalnina, I.; Silamikelis, I.; Konrade, I.; Zaharenko, L.; Sekace, K.; Radovica-Spalvina, I.; Fridmanis, D.; Gudra, D.; Pirags, V.; et al. Association of metformin administration with gut microbiome dysbiosis in healthy volunteers. PLoS ONE 2018, 13, e0204317. [Google Scholar] [CrossRef] [PubMed]
- Silamiķele, L.; Silamiķelis, I.; Ustinova, M.; Kalniņa, Z.; Elbere, I.; Petrovska, R.; Kalniņa, I.; Kloviņš, J. Metformin Strongly Affects Gut Microbiome Composition in High-Fat Diet-Induced Type 2 Diabetes Mouse Model of Both Sexes. Front. Endocrinol. 2021, 12, 626359. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Xu, K.; Du, T.; Zhu, P.; Liang, Z.; Liao, S.; Zhang, J.; Raizada, M.K.; Grant, M.B.; Li, Q. Expression of Human ACE2 in Lactobacillus and Beneficial Effects in Diabetic Retinopathy in Mice. Mol. Methods Clin. Dev. 2019, 14, 161–170. [Google Scholar] [CrossRef]
| Study, Year | Comparison | No. of Patients | Sex Ratio (M/F) | Age (ys ± SD) | BMI (Mean ± SD) | History of DM (ys) | HbA1C (Mean ± SD) | Method of Analysis | Metformin Therapy |
|---|---|---|---|---|---|---|---|---|---|
| Zhou Z [21], 2021 | DR | 21 | 14/7 | 59.57 ± 9.09 | 22.79 ± 2.43 | 13 (5–19.5) | 6.44 ± 0.92 | 16S rRNA | 21 (100%) |
| T2DM | 14 | 8/6 | 61.93 ± 6.20 | 22.2 ± 1.65 | 11.5 (2.7–16.2) | 6.55 ± 1.19 | 14 (100%) | ||
| HC | 15 | 7/8 | 56.13 ± 8.88 | 21.23 ± 2.09 | - | 5.19 ± 1.14 | - | ||
| Ye P [18], 2021 | PDR | 45 | 25/20 | 59.9 ± 11.3 | 24.4 ± 2.7 | 10 (2.5–16.7) | 9.6 ± 2.2 | 16S rRNA | 22 (48.8%) |
| T2DM (NDR) | 90 | 50/40 | 60.9 ± 9.9 | 24.9 ± 3.8 | 10 (2.0–15.3) | 8.8 ± 2.3 | 48 (53.3%) | ||
| Bai J [22], 2022 | DR | 25 | 13/12 | 55.64 ± 6.1 | 24.11 ± 3.01 | 10–30 | No info | 16S rRNA | No info |
| HC (spouses) | 25 | 11/14 | 56.32 ± 6.56 | 23.73 ± 2.95 | - | - | |||
| Huang Y [20], 2021 | DR | 25 (16 PDR; 9 NPDR) | 15/10 | 60.28 ± 10.5 | 23.06 ± 2.44 | 11.69 ± 7.07 | No info | 16S rRNA | 15 (60%) |
| T2DM | 25 | 11/14 | 62.52 ± 7.58 | 23.83 ± 3.13 | 10.36 ± 8.08 | No info | 19 (76%) | ||
| HC | 25 | 9/16 | 57.80 ± 10.06 | 24.40 ± 3.51 | - | No info | - | ||
| Das T [23], 2021 | DR (NDPR; PDR) | 28 (9;19) | 21/7 | 55.07 (44–69) | No info | No info | No info | 16S rRNA | 28 (100%) |
| T2DM | 25 | 14/11 | 57.3 (41–71) | 25 (100%) | |||||
| HC | 30 | 17/13 | 52.2 (38–81) | - | |||||
| Moubayed, N. M. [24], 2019 | DR | 8 | 0/8 | 40–60 | No info | No info | No info | 16S rRNA | No info |
| T2DM | 9 | 0/9 | |||||||
| HC | 18 | 0/18 | |||||||
| Li L [25], 2022 | DR | 15 | 8/7 | 55 (51–63) | 26.0 (23.5–28.0) | 13 (8–17) | 8.7 (7.5–10.4) | Shotgun metagenomic sequencing | No info |
| T2DM | 15 | 7/8 | 57 (51–62) | 27.6 (25.5–30.3) | 10 (9–14) | 7.8 (6.9–9.5) | |||
| Khan R [26], 2021 | STDR (PDR; CSME) | 37 (21;16) | 25/12 | 57.45 ± 8.08 | 26.44 ± 5.23 | 12 (8–20) | 7.48 ± 1.44 | 16s rRNA | 4 (10.81%) |
| T2DM | 21 | 13/8 | 57.50 ± 7.60 | 26.53 ± 5.52 | 12 (10–20) | 7.49 ± 1.48 | 2 (9.52%) |
| Study, Year | Chao 1 | Sobs | ACE | OTUs | Shannon | Simpson/invSimpson | Heip Evenness Index | Beta Diversity PCoA/PLS-DA |
|---|---|---|---|---|---|---|---|---|
| Zhou Z [21], 2021 | ↑ | - | - | ↑ | Not significant | - | - | Significantly different |
| Bai J [22], 2022 | Not significant | ↑ | ↑ Not significant | - | ↑ Not significant | Not significant | Not significant | Significantly different |
| Huang Y [19], 2021 | Not significant | - | Not significant | - | Not significant | ↓ | ↓ | Significant diversity |
| Das T [23], 2021 | Not significant | - | - | Not significant | ↓ | Not significant | - | Significant diversity |
| Moubayed NM [24], 2019 | - | - | - | Not significant | - | - | - | Significant diversity |
| Study, Year | Chao 1 | ACE | OTUs | Shannon | Simpson | Heip Evenness Index | Beta Diversity PCoA |
|---|---|---|---|---|---|---|---|
| Zhou Z [21], 2021 | ↑ | - | ↑ | Not significant | - | Significantly different | |
| Ye P [18], 2021 | ↓ | - | ↓ | ↓ | ↓ | Significantly different | |
| Huang Y [19], 2021 | Not significant | Not significant | - | Not significant | Not significant | Not significant | Significant diversity |
| Das T [23], 2021 | Not significant | - | Not significant | Not significant | Not significant | - | Significant diversity |
| Moubayed NM [24], 2019 | - | - | Not significant | - | - | - | Significant diversity |
| Li L [25], 2022 | - | - | - | - | - | - | Significant diversity |
| Khan R [26], 2021 | - | - | - | - | - | - | No significant difference in relative abundance; different F/B ratio |
| Phylum | Genera/Species | Main Function | RDM vs. DM | Studies | RDM vs. HC | Studies |
|---|---|---|---|---|---|---|
| Firmicutes | All phylum | ↓ | Huang Y [19] | ↓ | Bai, Huang Y [19], Moubayed NM [25] | |
| Roseburia spp. |
| ↓ | Ye P [18] | ↓ | Zhou Z [21], Das T [23] | |
| Faecalibacterium spp. |
| ↓ | Ye P [18] | ↓ | Zhou Z [21], Huang Y [19], Das T [23] | |
| Ruminococcaceae |
| ↓ | Zhou Z [21], Ye P [18] | ↓ | Zhou Z [21] | |
| Lachnospira |
| ↓ | Das T [23] | |||
| Dorea, Anaerostipes |
| ↓ | Bai J [22] | |||
| Subdoligranulum |
| ↑ | Ye P [18] | |||
| Agathobacter (Eubacterium rectale) |
| ↑ ↓ | Zhou Z [21], Ye P [18] | |||
| Veillonellaceae |
| ↓ | Ye P [18] | |||
| Streptococcaceae |
| ↓ | Ye P [18] | |||
| Clostridium, Clostridiaceae |
| ↓ | Huang Y [19] | ↓ | Huang Y [19] | |
| Eubacterium_hallii_group |
| ↓ | Huang Y [19] | ↓ | Bai J [22], Huang Y [19] | |
| Blautia |
| ↓ | Huang Y [19] | ↑ ↓ | Huang Y [19], Das T [23], Bai J [22] | |
| Lactobacillus |
| ↓ | Huang Y [19], Li L [25] | ↑ | Huang Y [19] | |
| Lachnoclostridium |
| ↑ | Bai J [22] | |||
| Romboutsia |
| ↑ | Bai J [22] | |||
| Megamonas |
| ↑ | Bai J [22], Das T [23] | |||
| Ruminococcus_torques_group |
| ↑ | Bai J [22] | |||
| Peptostreptococcaceae |
| ↓ | Huang Y [19] | |||
| Oscillospiraceae |
| ↑ | Huang Y [19] | |||
| Christensenellaceae |
| ↑ | Huang Y [19] | |||
| Acidaminococcaceae |
| ↑ | Huang Y [19], Das T [23] | |||
| Actinobacter | All phylum | ↓ | Li L [26], Das T [23] | ↓ | Das T [23] | |
| Coriobacteriales |
| ↓ | Ye P [18] | |||
| Collinsella |
| ↓ | Bai J [22] | |||
| Bifidobacterium |
| ↓ | Das T [23], Li L [25] | ↓ ↑ | Das T [23], Huang Y [19] | |
| Atopobiaceae |
| ↑ | Huang Y [19] | ↑ | Huang Y [19] | |
| Bacteroidetes | All phylum |
| ↑ | Huang Y [19], Li L [25] | ↑ | Bai J [22], Huang Y [19], Moubayed NM [24] |
| Prevotella |
| ↑ | Zhou Z [21], | ↑ | Moubayed NM [24] | |
| Parabacteroides | ↑ | Das T [23] | ||||
| Muribaculacea |
| ↑ | Huang Y [19] | ↑ | Huang Y [19] | |
| Bacteroides |
| ↑ | Bai J [22], Das T [23] | |||
| Alistipes |
| ↑ | Li L [25], Bai J [22], Das T [23] | |||
| Proteobacteria | Burkholderiaceae |
| ↑ | Ye P [18] | ||
| Morganella |
| ↓ | Ye P [18] | |||
| Pasteurellaceae |
| ↓ | Huang Y [19] | ↓ | Huang Y [19] | |
| Escherischia |
| ↑ | Das T [23] | ↑ | Das T [23] | |
| Enterobacter |
| ↑ | Das T [23] | |||
| Verrucomicrobia | All phylum | ↑ | Bai J [22] | |||
| Akkermansia muciniphila, Akkermansiaceae |
| ↑ | Das T [23] | ↑ | Zhou Z [21], Das T [23] | |
| Desulfobacterota | All phylum |
| ↑ | Huang Y [19] | ↑ | Bai J [22] |
| Synergistota | All phylum |
| ↑ | Bai J [22] | ||
| F/B ratio | ↓ Not significant | Khan R [26], Huang Y [19], Ye P [18] | ↓ | Bai J [22], Huang Y [19], Moubayed NM [24] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serban, D.; Dascalu, A.M.; Arsene, A.L.; Tribus, L.C.; Vancea, G.; Pantea Stoian, A.; Costea, D.O.; Tudosie, M.S.; Stana, D.; Cristea, B.M.; et al. Gut Microbiota Dysbiosis in Diabetic Retinopathy—Current Knowledge and Future Therapeutic Targets. Life 2023, 13, 968. https://doi.org/10.3390/life13040968
Serban D, Dascalu AM, Arsene AL, Tribus LC, Vancea G, Pantea Stoian A, Costea DO, Tudosie MS, Stana D, Cristea BM, et al. Gut Microbiota Dysbiosis in Diabetic Retinopathy—Current Knowledge and Future Therapeutic Targets. Life. 2023; 13(4):968. https://doi.org/10.3390/life13040968
Chicago/Turabian StyleSerban, Dragos, Ana Maria Dascalu, Andreea Letitia Arsene, Laura Carina Tribus, Geta Vancea, Anca Pantea Stoian, Daniel Ovidiu Costea, Mihail Silviu Tudosie, Daniela Stana, Bogdan Mihai Cristea, and et al. 2023. "Gut Microbiota Dysbiosis in Diabetic Retinopathy—Current Knowledge and Future Therapeutic Targets" Life 13, no. 4: 968. https://doi.org/10.3390/life13040968
APA StyleSerban, D., Dascalu, A. M., Arsene, A. L., Tribus, L. C., Vancea, G., Pantea Stoian, A., Costea, D. O., Tudosie, M. S., Stana, D., Cristea, B. M., Nicolae, V. A., Tudor, C., Costea, A. C., Comandasu, M., Faur, M., & Tanasescu, C. (2023). Gut Microbiota Dysbiosis in Diabetic Retinopathy—Current Knowledge and Future Therapeutic Targets. Life, 13(4), 968. https://doi.org/10.3390/life13040968










