Biologics for Chronic Rhinosinusitis—A Modern Option for Therapy
Abstract
1. Introduction
2. Pathophysiology
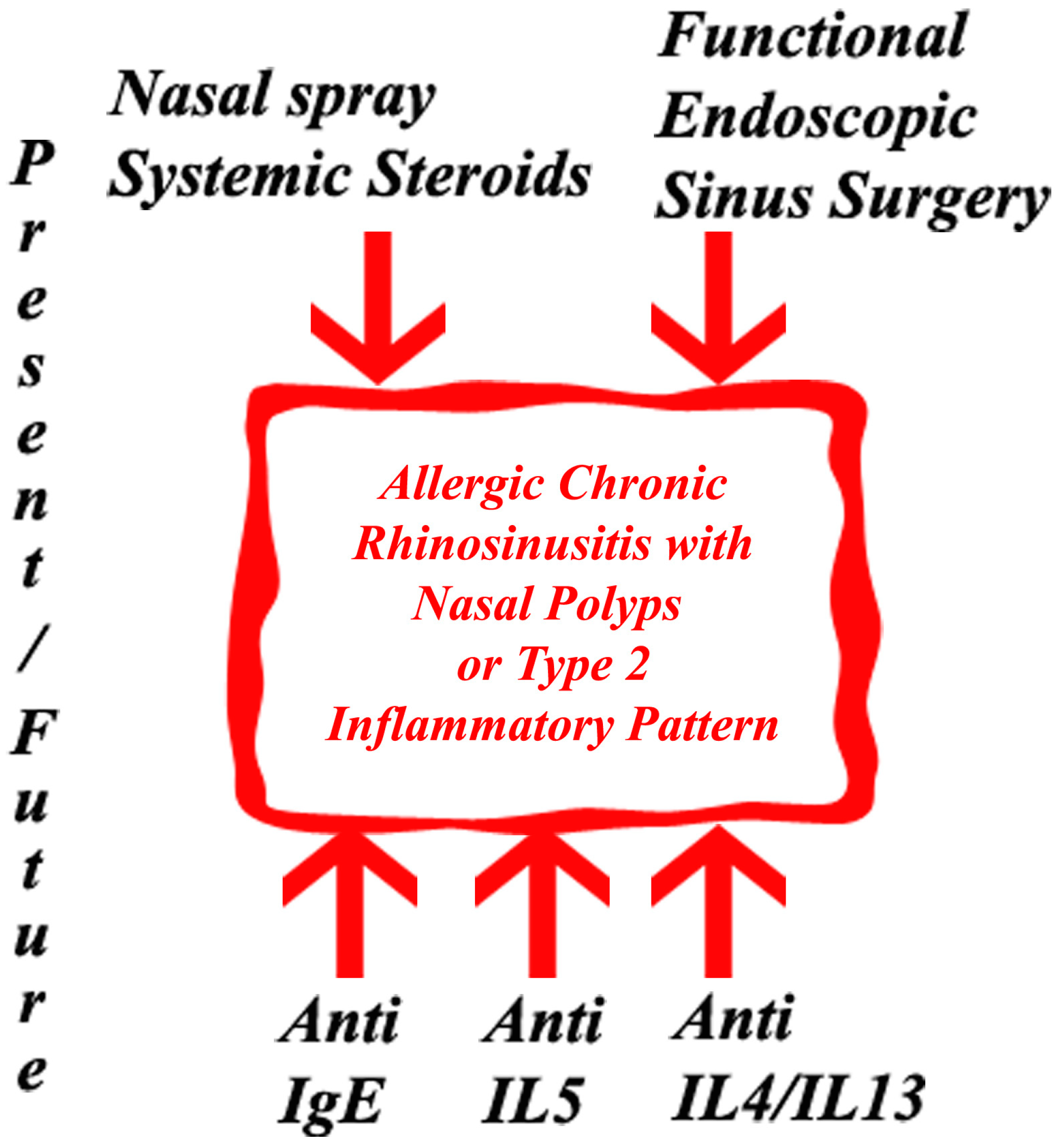
3. Biologics Used in the Field of Rhinology
3.1. Anti-IgE
3.2. Anti-IL5
3.3. Anti-IL4/IL13
4. Comparative Studies between Biologics
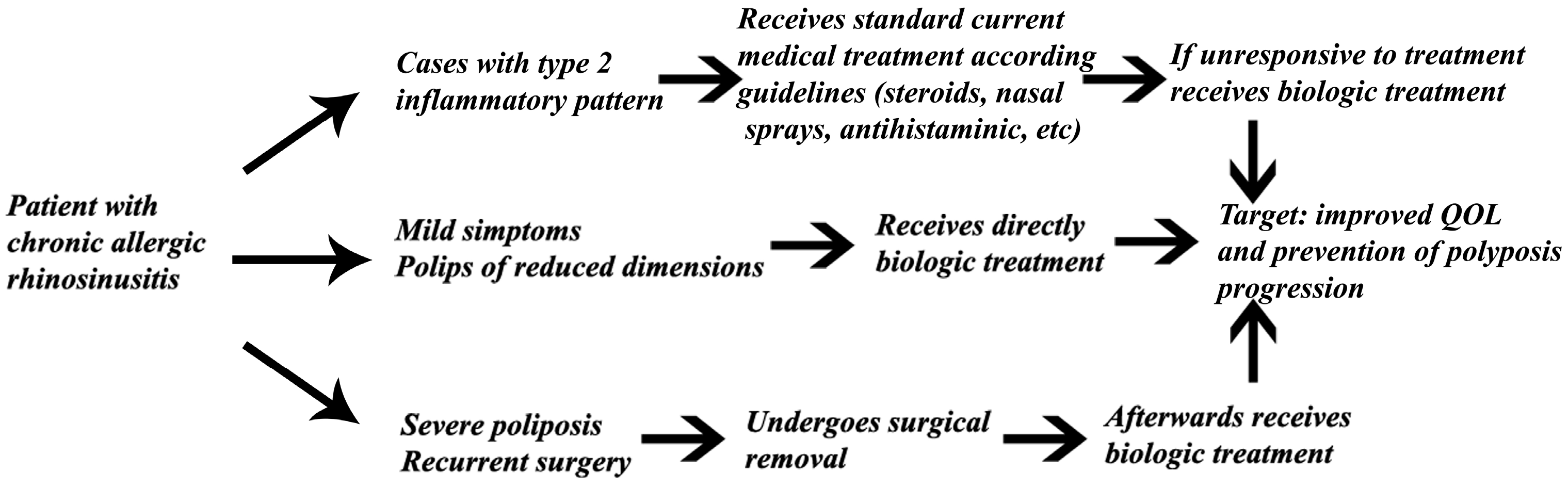
5. Future Clinical Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Seah, J.J.; Thong, M.; Wang, D.Y. The Diagnostic and Prognostic Role of Biomarkers in Chronic Rhinosinusitis. Diagnostics 2023, 13, 715. [Google Scholar] [CrossRef] [PubMed]
- Czerwaty, K.; Piszczatowska, K.; Brzost, J.; Ludwig, N.; Szczepański, M.J.; Dżaman, K. Immunological Aspects of Chronic Rhinosinusitis. Diagnostics 2022, 12, 2361. [Google Scholar] [CrossRef] [PubMed]
- Kato, A.; Peters, A.T.; Stevens, W.W.; Schleimer, R.P.; Tan, B.K.; Kern, R.C. Endotypes of chronic rhinosinusitis: Relationships to disease phenotypes, pathogenesis, clinical findings, and treatment approaches. Allergy 2021, 77, 812–826. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, T.; Suzuki, M.; Kato, Y.; Kidoguchi, M.; Kumai, T.; Fujieda, S.; Sakashita, M. The current findings in eosinophilic chronic rhinosinusitis. Auris Nasus Larynx, 2023; in press. [Google Scholar] [CrossRef]
- Yao, Y.; Zhu, H.; Zeng, M.; Liu, Z. Immunological mechanisms and treatable traits of chronic rhinosinusitis in Asia: A narrative review. Clin. Otolaryngol. 2022, 48, 363–370. [Google Scholar] [CrossRef]
- Chapurin, N.; Wu, J.; Labby, A.B.; Chandra, R.K.; Chowdhury, N.I.; Turner, J.H. Current insight into treatment of chronic rhinosinusitis: Phenotypes, endotypes, and implications for targeted therapeutics. J. Allergy Clin. Immunol. 2022, 150, 22–32. [Google Scholar] [CrossRef]
- Grayson, J.W.; Hopkins, C.; Mori, E.; Senior, B.; Harvey, R.J. Contemporary Classification of Chronic Rhinosinusitis Beyond Polyps vs No Polyps. JAMA Otolaryngol. Neck Surg. 2020, 146, 831–838, Erratum in JAMA Otolaryngol. Head Neck Surg. 2020, 146, 876. [Google Scholar] [CrossRef]
- Kim, S.-D.; Cho, K.-S. Treatment Strategy of Uncontrolled Chronic Rhinosinusitis with Nasal Polyps: A Review of Recent Evidence. Int. J. Mol. Sci. 2023, 24, 5015. [Google Scholar] [CrossRef]
- Ha, J.-G.; Cho, H.-J. Unraveling the Role of Epithelial Cells in the Development of Chronic Rhinosinusitis. Int. J. Mol. Sci. 2023, 24, 14229. [Google Scholar] [CrossRef]
- Xu, Z.; Huang, Y.; Meese, T.; Van Nevel, S.; Holtappels, G.; Vanhee, S.; Bröker, B.M.; Li, Z.; de Meester, E.; De Ruyck, N.; et al. The multi-omics single-cell landscape of sinus mucosa in uncontrolled severe chronic rhinosinusitis with nasal polyps. Clin. Immunol. 2023, 256, 109791. [Google Scholar] [CrossRef]
- Cui, N.; Zhu, X.; Zhao, C.; Meng, C.; Sha, J.; Zhu, D. A Decade of Pathogenesis Advances in Non-Type 2 Inflammatory Endotypes in Chronic Rhinosinusitis: 2012–2022. Int. Arch. Allergy Immunol. 2023, 1–17. [Google Scholar] [CrossRef]
- Wang, X.; Sima, Y.; Zhao, Y.; Zhang, N.; Zheng, M.; Du, K.; Wang, M.; Wang, Y.; Hao, Y.; Li, Y.; et al. Endotypes of chronic rhinosinusitis based on inflammatory and remodeling factors. J. Allergy Clin. Immunol. 2022, 151, 458–468. [Google Scholar] [CrossRef]
- Brzost, J.; Czerwaty, K.; Dżaman, K.; Ludwig, N.; Piszczatowska, K.; Szczepański, M.J. Perspectives in Therapy of Chronic Rhinosinusitis. Diagnostics 2022, 12, 2301. [Google Scholar] [CrossRef]
- Fokkens, W.; Lund, V.; Hopkins, C.; Hellings, P.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J. Executive Summary of EPOS 2020 Including Integrated Care Pathways. Rhinol. J. 2020, 58, 82–111. [Google Scholar] [CrossRef] [PubMed]
- Wei, B.; Liu, F.; Zhang, J.; Liu, Y.; Du, J.; Liu, S.; Zhang, N.; Bachert, C.; Meng, J. Multivariate analysis of inflammatory endo-types in recurrent nasal polyposis in a Chinese population. Rhinology 2018, 56, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Baba, S.; Kondo, K.; Toma-Hirano, M.; Kanaya, K.; Suzukawa, K.; Ushio, M.; Suzukawa, M.; Ohta, K.; Yamasoba, T. Local increase in IgE and class switch recombination to IgE in nasal polyps in chronic rhinosinusitis. Clin. Exp. Allergy 2014, 44, 701–712. [Google Scholar] [CrossRef] [PubMed]
- Riechelmann, H.; Deutschle, T.; Rozsasi, A.; Keck, T.; Polzehl, D.; Bürner, H. Nasal biomarker profiles in acute and chronic rhinosinusitis. Clin. Exp. Allergy 2005, 35, 1186–1191. [Google Scholar] [CrossRef]
- Chong, L.-Y.; Piromchai, P.; Sharp, S.; Snidvongs, K.; E Webster, K.; Philpott, C.; Hopkins, C.; Burton, M.J. Biologics for chronic rhinosinusitis. Cochrane Database Syst. Rev. 2021, 2021, CD013513. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Kanda, A.; Van Bui, D.; Yun, Y.; Nguyen, L.M.; Chu, H.H.; Mitani, A.; Suzuki, K.; Asako, M.; Iwai, H. Omalizumab Restores Response to Corticosteroids in Patients with Eosinophilic Chronic Rhinosinusitis and Severe Asthma. Biomedicines 2021, 9, 787. [Google Scholar] [CrossRef]
- Zhu, R.; Owen, R.; Wilkins, J.; Schoemaker, R.; Tian, X.; Gautier, A.; She, G.; Vadhavkar, S.; Cheu, M.; Wong, K.; et al. Pharmacokinetics and exposure-efficacy relationships of omalizumab in patients with nasal polyps. Pulm. Pharmacol. Ther. 2021, 71, 102080. [Google Scholar] [CrossRef]
- Pinto, J.; Mehta, N.; DiTineo, M.; Wang, J.; Baroody, F.; Naclerio, R. A randomized, double-blind, placebo-controlled trial of anti-IgE for chronic rhinosinusitis. Rhinol. J. 2010, 48, 318–324. [Google Scholar] [CrossRef]
- Tajiri, T.; Matsumoto, H.; Hiraumi, H.; Ikeda, H.; Morita, K.; Izuhara, K.; Ono, J.; Ohta, S.; Ito, I.; Oguma, T.; et al. Efficacy of omalizumab in eosinophilic chronic rhinosinusitis patients with asthma. Ann. Allergy Asthma Immunol. 2013, 110, 387–388. [Google Scholar] [CrossRef]
- Gevaert, P.; Omachi, T.A.; Corren, J.; Mullol, J.; Han, J.; Lee, S.E.; Kaufman, D.; Ligueros-Saylan, M.; Howard, M.; Zhu, R.; et al. Efficacy and safety of omalizumab in nasal polyposis: 2 randomized phase 3 trials. J. Allergy Clin. Immunol. 2020, 146, 595–605, Erratum in J. Allergy Clin. Immunol. 2021, 147, 416. [Google Scholar] [CrossRef] [PubMed]
- Gevaert, P.; Saenz, R.; Corren, J.; Han, J.K.; Mullol, J.; Lee, S.E.; Ow, R.A.; Zhao, R.; Howard, M.; Wong, K.; et al. Long-term efficacy and safety of omalizumab for nasal polyposis in an open-label extension study. J. Allergy Clin. Immunol. 2021, 149, 957–965.e3. [Google Scholar] [CrossRef]
- Damask, C.; Chen, M.; Holweg, C.T.J.; Yoo, B.; Millette, L.A.; Franzese, C. Defining the Efficacy of Omalizumab in Nasal Polyposis: A POLYP 1 and POLYP 2 Subgroup Analysis. Am. J. Rhinol. Allergy 2021, 36, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Haxel, B.; Hummel, T.; Fruth, K.; Lorenz, K.; Gunder, N.; Nahrath, P.; Cuevas, M. Real-world-effectiveness of biological treatment for severe chronic rhinosinusitis with nasal polyps. Rhinol. J. 2022, 60, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Bidder, T.; Sahota, J.; Rennie, C.; Lund, V.; Robinson, D.; Kariyawasam, H. Omalizumab treats chronic rhinosinusitis with nasal polyps and asthma together-a real life study. Rhinol. J. 2018, 56, 42–45. [Google Scholar] [CrossRef]
- Armengot-Carceller, M.; Gómez-Gómez, M.J.; García-Navalón, C.; Doménech-Campos, E.; Muñoz-Fernández, N.; de Miguel, A.G.-L.; Marco-Algarra, J.; Palop-Cervera, M.; Piñero, A.G. Effects of Omalizumab Treatment in Patients with Recalcitrant Nasal Polyposis and Mild Asthma: A Multicenter Retrospective Study. Am. J. Rhinol. Allergy 2020, 35, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Tat, T.S. Omalizumab is effective in nasal polyposis with or without asthma, a real-life study. World Allergy Organ. J. 2022, 15, 100670. [Google Scholar] [CrossRef]
- Zheng, M.; Sima, Y.; Liu, C.; Zhao, J.; Shao, S.; Wang, X.; Wang, Y.; Cao, F.; Xiong, W.; Wang, X.; et al. Clinical effectiveness and potential predictability of omalizumab in patients with difficult-to-treat chronic rhinosinusitis with nasal polyps and asthma based on the noninvasive markers–A real-life prospective study. World Allergy Organ. J. 2022, 15, 100702. [Google Scholar] [CrossRef]
- DeConde, A.S.; Mace, J.C.; Levy, J.M.; Rudmik, L.; Alt, J.A.; Smith, T.L. Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Laryngoscope 2017, 127, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Canonica, G.W.; Harrison, T.W.; Chanez, P.; Menzella, F.; Louis, R.; Cosio, B.G.; Lugogo, N.L.; Mohan, A.; Burden, A.; Gil, E.G. Benralizumab improves symptoms of patients with severe, eosinophilic asthma with a diagnosis of nasal polyposis. Allergy 2021, 77, 150–161. [Google Scholar] [CrossRef]
- Tversky, J.; Lane, A.P.; Azar, A. Benralizumab effect on severe chronic rhinosinusitis with nasal polyps (CRSwNP): A randomized double-blind placebo-controlled trial. Clin. Exp. Allergy 2021, 51, 836–844. [Google Scholar] [CrossRef]
- Takabayashi, T.; Asaka, D.; Okamoto, Y.; Himi, T.; Haruna, S.; Yoshida, N.; Kondo, K.; Yoshikawa, M.; Sakuma, Y.; Shibata, K.; et al. A Phase II, Multicenter, Randomized, Placebo-Controlled Study of Benralizumab, a Humanized Anti-IL-5R Alpha Monoclonal Antibody, in Patients with Eosinophilic Chronic Rhinosinusitis. Am. J. Rhinol. Allergy 2021, 35, 861–870. [Google Scholar] [CrossRef]
- Bachert, C.; Han, J.K.; Desrosiers, M.Y.; Gevaert, P.; Heffler, E.; Hopkins, C.; Tversky, J.R.; Barker, P.; Cohen, D.; Emson, C.; et al. Efficacy and safety of benralizumab in chronic rhinosinusitis with nasal polyps: A randomized, placebo-controlled trial. J. Allergy Clin. Immunol. 2021, 149, 1309–1317.e12. [Google Scholar] [CrossRef]
- Matsuno, O.; Minamoto, S. Rapid effect of benralizumab for severe asthma with chronic rhinosinusitis with nasal polyps. Pulm. Pharmacol. Ther. 2020, 64, 101965. [Google Scholar] [CrossRef] [PubMed]
- Chitguppi, C.; Patel, P.; Gandler, A.; Murphy, K.; Khoury, T.; Monostra, P.; Bork, S.; Toskala, E.; Rabinowitz, M.; Rosen, M.; et al. Effect of Benralizumab in Patients with Severe Eosinophilic Asthma and Chronic Rhinosinusitis With Nasal Polyps: A Case Series. Am. J. Rhinol. Allergy 2020, 35, 559–567. [Google Scholar] [CrossRef]
- Lombardo, N.; Pelaia, C.; Ciriolo, M.; Della Corte, M.; Piazzetta, G.; Lobello, N.; Viola, P.; Pelaia, G. Real-life effects of benralizumab on allergic chronic rhinosinusitis and nasal polyposis associated with severe asthma. Int. J. Immunopathol. Pharmacol. 2020, 34, 2058738420950851. [Google Scholar] [CrossRef] [PubMed]
- Nolasco, S.; Crimi, C.; Pelaia, C.; Benfante, A.; Caiaffa, M.F.; Calabrese, C.; Carpagnano, G.E.; Ciotta, D.; D’Amato, M.; Macchia, L.; et al. Benralizumab Effectiveness in Severe Eosinophilic Asthma with and without Chronic Rhinosinusitis with Nasal Polyps: A Real-World Multicenter Study. J. Allergy Clin. Immunol. Pract. 2021, 9, 4371–4380.e4. [Google Scholar] [CrossRef]
- Cavaliere, C.; Segatto, M.; Ciofalo, A.; Colizza, A.; Minni, A.; Messineo, D.; Lambiase, A.; Greco, A.; de Vincentiis, M.; Masieri, S. Benralizumab reduces eosinophils and inflammatory markers in patients with severe eosinophilic asthma and chronic rhinosinusitis with nasal polyps: A pilot real-life study. Immunol. Lett. 2022, 248, 70–77. [Google Scholar] [CrossRef]
- Santomasi, C.; Buonamico, E.; Dragonieri, S.; Iannuzzi, L.; Portacci, A.; Quaranta, N.; Carpagnano, G.E. Effects of benralizumab in a population of patients affected by severe eosinophilic asthma and chronic rhinosinusitis with nasal polyps: A real life study. Acta Biomed. 2023, 94, e2023028. [Google Scholar] [CrossRef]
- Fokkens, W.J.; Mullol, J.; Kennedy, D.; Philpott, C.; Seccia, V.; Kern, R.C.; Coste, A.; Sousa, A.R.; Howarth, P.H.; Benson, V.S.; et al. Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): In-depth sinus surgery analysis. Allergy 2022, 78, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Sousa, A.R.; Lund, V.J.; Scadding, G.K.; Gevaert, P.; Nasser, S.; Durham, S.R.; Cornet, M.E.; Kariyawasam, H.H.; Gilbert, J.; et al. Reduced need for surgery in severe nasal polyposis with mepolizumab: Randomized trial. J. Allergy Clin. Immunol. 2017, 140, 1024–1031.e14. [Google Scholar] [CrossRef] [PubMed]
- Han, J.K.; Bachert, C.; Fokkens, W.; Desrosiers, M.; Wagenmann, M.; E Lee, S.; Smith, S.G.; Martin, N.; Mayer, B.; Yancey, S.W.; et al. Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir. Med. 2021, 9, 1141–1153. [Google Scholar] [CrossRef]
- Bachert, C.; Sousa, A.R.; Han, J.K.; Schlosser, R.J.; Sowerby, L.J.; Hopkins, C.; Maspero, J.F.; Smith, S.G.; Kante, O.; Karidi-Andrioti, D.E.; et al. Mepolizumab for chronic rhinosinusitis with nasal polyps: Treatment efficacy by comorbidity and blood eosinophil count. J. Allergy Clin. Immunol. 2022, 149, 1711–1721.e6. [Google Scholar] [CrossRef] [PubMed]
- Gallo, S.; Castelnuovo, P.; Spirito, L.; Feduzi, M.; Seccia, V.; Visca, D.; Spanevello, A.; Statuti, E.; Latorre, M.; Montuori, C.; et al. Mepolizumab Improves Outcomes of Chronic Rhinosinusitis with Nasal Polyps in Severe Asthmatic Patients: A Multicentric Real-Life Study. J. Pers. Med. 2022, 12, 1304. [Google Scholar] [CrossRef]
- Detoraki, A.; Tremante, E.; D’amato, M.; Calabrese, C.; Casella, C.; Maniscalco, M.; Poto, R.; Brancaccio, R.; Boccia, M.; Martino, M.; et al. Mepolizumab improves sino-nasal symptoms and asthma control in severe eosinophilic asthma patients with chronic rhinosinusitis and nasal polyps: A 12-month real-life study. Ther. Adv. Respir. Dis. 2021, 15, 17534666211009398. [Google Scholar] [CrossRef]
- Domínguez-Sosa, M.S.; Cabrera-Ramírez, M.S.; Marrero-Ramos, M.d.C.; Dávila-Quintana, D.; Cabrera-López, C.; Carrillo-Díaz, T.; del Rosario, J.J.B. Real-Life Effectiveness of Mepolizumab in Refractory Chronic Rhinosinusitis with Nasal Polyps. Biomedicines 2023, 11, 485. [Google Scholar] [CrossRef]
- Gevaert, P.; Langloidolt, D.; Lackner, A.; Stammberger, H.; Staudinger, H.; Vanzele, T.; Holtappels, G.; Tavernier, J.; Vancauwenberge, P.; Bachert, C. Nasal IL-5 levels determine the response to anti–IL-5 treatment in patients with nasal polyps. J. Allergy Clin. Immunol. 2006, 118, 1133–1141. [Google Scholar] [CrossRef]
- Bhatt, S.P.; Rabe, K.F.; Hanania, N.A.; Vogelmeier, C.F.; Cole, J.; Bafadhel, M.; Christenson, S.A.; Papi, A.; Singh, D.; Laws, E.; et al. Dupilumab for COPD with Type 2 Inflammation Indicated by Eosinophil Counts. N. Engl. J. Med. 2023, 389, 205–214. [Google Scholar] [CrossRef]
- Jonstam, K.; Swanson, B.N.; Mannent, L.P.; Cardell, L.; Tian, N.; Wang, Y.; Zhang, D.; Fan, C.; Holtappels, G.; Hamilton, J.D.; et al. Dupilumab reduces local type 2 pro-inflammatory biomarkers in chronic rhinosinusitis with nasal polyposis. Allergy 2018, 74, 743–752. [Google Scholar] [CrossRef]
- Bachert, C.; Hellings, P.W.; Mullol, J.; Naclerio, R.M.; Chao, J.; Amin, N.; Grabher, A.; Swanson, B.N.; Hamilton, J.D.; Guillonneau, S.; et al. Dupilumab improves patient-reported outcomes in patients with chronic rhinosinusitis with nasal polyps and comorbid asthma. J. Allergy Clin. Immunol. Pract. 2019, 7, 2447–2449.e2. [Google Scholar] [CrossRef]
- Bachert, C.; Han, J.K.; Desrosiers, M.; Hellings, P.W.; Amin, N.; E Lee, S.; Mullol, J.; Greos, L.S.; Bosso, J.V.; Laidlaw, T.M.; et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 2019, 394, 1638–1650, Erratum in Lancet 2019, 394, 1618. [Google Scholar] [CrossRef]
- Chuang, C.; Guillemin, I.; Bachert, C.; Lee, S.E.; Hellings, P.W.; Fokkens, W.J.; Duverger, N.; Fan, C.; Daizadeh, N.; Amin, N.; et al. Dupilumab in CRSwNP: Responder Analysis Using Clinically Meaningful Efficacy Outcome Thresholds. Laryngoscope 2021, 132, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Zinreich, S.J.; Hellings, P.W.; Mullol, J.; Hamilos, D.L.; Gevaert, P.; Naclerio, R.M.; Amin, N.; Joish, V.N.; Fan, C.; et al. Dupilumab reduces opacification across all sinuses and related symptoms in patients with CRSwNP. Rhinol. J. 2019, 58, 10–17. [Google Scholar] [CrossRef]
- Fujieda, S.; Matsune, S.; Takeno, S.; Asako, M.; Takeuchi, M.; Fujita, H.; Takahashi, Y.; Amin, N.; Deniz, Y.; Rowe, P.; et al. The Effect of Dupilumab on Intractable Chronic Rhinosinusitis with Nasal Polyps in Japan. Laryngoscope 2020, 131, E1770–E1777. [Google Scholar] [CrossRef] [PubMed]
- Desrosiers, M.; Mannent, L.; Amin, N.; Canonica, G.; Hellings, P.; Gevaert, P.; Mullol, J.; Lee, S.; Fujieda, S.; Han, J.; et al. Dupilumab reduces systemic corticosteroid use and sinonasal surgery rate in CRSwNP. Rhinol. J. 2021, 59, 301–311. [Google Scholar] [CrossRef]
- Hopkins, C.; Wagenmann, M.; Bachert, C.; Desrosiers, M.; Han, J.K.; Hellings, P.W.; Lee, S.E.; Msihid, J.; Radwan, A.; Rowe, P.; et al. Efficacy of dupilumab in patients with a history of prior sinus surgery for chronic rhinosinusitis with nasal polyps. Int. Forum Allergy Rhinol. 2021, 11, 1087–1101. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.E.; Hopkins, C.; Mullol, J.; Msihid, J.; Guillemin, I.; Amin, N.; Mannent, L.P.; Li, Y.; Siddiqui, S.; Chuang, C.; et al. Dupilumab improves health related quality of life: Results from the phase 3 SINUS studies. Allergy 2022, 77, 2211–2221. [Google Scholar] [CrossRef]
- Mullol, J.; Bachert, C.; Amin, N.; Desrosiers, M.; Hellings, P.W.; Han, J.K.; Jankowski, R.; Vodicka, J.; Gevaert, P.; Daizadeh, N.; et al. Olfactory Outcomes with Dupilumab in Chronic Rhinosinusitis with Nasal Polyps. J. Allergy Clin. Immunol. Pract. 2021, 10, 1086–1095.e5. [Google Scholar] [CrossRef]
- Berger, P.; Menzies-Gow, A.; Peters, A.T.; Kuna, P.; Rabe, K.F.; Altincatal, A.; Soler, X.; Pandit-Abid, N.; Siddiqui, S.; Jacob-Nara, J.A.; et al. Long-term efficacy of dupilumab in asthma with or without chronic rhinosinusitis and nasal polyps. Ann. Allergy Asthma Immunol. 2022, 130, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Laidlaw, T.M.; Bachert, C.; Amin, N.; Desrosiers, M.; Hellings, P.W.; Mullol, J.; Maspero, J.F.; Gevaert, P.; Zhang, M.; Mao, X.; et al. Dupilumab improves upper and lower airway disease control in chronic rhinosinusitis with nasal polyps and asthma. Ann. Allergy Asthma Immunol. 2021, 126, 584–592.e1. [Google Scholar] [CrossRef] [PubMed]
- Maspero, J.F.; Katelaris, C.H.; Busse, W.W.; Castro, M.; Corren, J.; Chipps, B.E.; Peters, A.T.; Pavord, I.D.; Ford, L.B.; Sher, L.; et al. Dupilumab Efficacy in Uncontrolled, Moderate-to-Severe Asthma with Self-Reported Chronic Rhinosinusitis. J. Allergy Clin. Immunol. Pract. 2020, 8, 527–539.e9. [Google Scholar] [CrossRef] [PubMed]
- Jansen, F.; Becker, B.; Eden, J.K.; Breda, P.C.; Hot, A.; Oqueka, T.; Betz, C.S.; Hoffmann, A.S. Dupilumab (Dupixent®) tends to be an effective therapy for uncontrolled severe chronic rhinosinusitis with nasal polyps: Real data of a single-centered, retrospective single-arm longitudinal study from a university hospital in Germany. Eur. Arch. Oto-Rhino-Laryngol. 2022, 280, 1741–1755. [Google Scholar] [CrossRef]
- De Corso, E.; Settimi, S.; Montuori, C.; Corbò, M.; Passali, G.C.; Porru, D.P.; Verde, S.L.; Spanu, C.; Penazzi, D.; Di Bella, G.A.; et al. Effectiveness of Dupilumab in the Treatment of Patients with Severe Uncontrolled CRSwNP: A “Real-Life” Observational Study in the First Year of Treatment. J. Clin. Med. 2022, 11, 2684. [Google Scholar] [CrossRef] [PubMed]
- Ottaviano, G.; Saccardo, T.; Roccuzzo, G.; Bernardi, R.; Di Chicco, A.; Pendolino, A.L.; Scarpa, B.; Mairani, E.; Nicolai, P. Effectiveness of Dupilumab in the Treatment of Patients with Uncontrolled Severe CRSwNP: A “Real-Life” Observational Study in Naïve and Post-Surgical Patients. J. Pers. Med. 2022, 12, 1526. [Google Scholar] [CrossRef]
- Galletti, C.; Barbieri, M.A.; Ciodaro, F.; Freni, F.; Galletti, F.; Spina, E.; Galletti, B. Effectiveness and Safety Profile of Dupilumab in Chronic Rhinosinusitis with Nasal Polyps: Real-Life Data in Tertiary Care. Pharmaceuticals 2023, 16, 630. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, T.; Sailer, M.M.; Capitani, F.; van Schaik, C.; Löwenheim, H.; Becker, S. Real-world evidence for the effectiveness and safety of dupilumab in patients with CRSwNP after 1 year of therapy. World Allergy Organ. J. 2023, 16, 100780. [Google Scholar] [CrossRef]
- Barroso, B.; Valverde-Monge, M.; Alobid, I.; Olaguibel, J.; Rial, M.; Quirce, S.; Arismendi, E.; Barranco, P.; Betancor, D.; Bobolea, I.; et al. Smell improvement by anti-IgE and anti-IL 5 biologics in patients with CRSwNP and severe asthma. A real life study. J. Investig. Allergol. Clin. Immunol. 2022, 33, 37–44. [Google Scholar] [CrossRef]
- Meier, E.C.; Schmid-Grendelmeier, P.; Steiner, U.C.; Soyka, M.B. Real-Life Experience of Monoclonal Antibody Treatments in Chronic Rhinosinusitis with Nasal Polyposis. Int. Arch. Allergy Immunol. 2021, 182, 736–743. [Google Scholar] [CrossRef]
- Otten, J.; van der Lans, R.; de Corso, E.; Dziadziulia, K.; Hilvering, B.; Weersink, E.; Bonini, M.; Hagemann, J.; Thaitrakool, W.; Montuori, C.; et al. Evaluation of switching or simultaneous use of biologic treatment in patients with severe chronic rhinosinusitis with nasal polyps and severe asthma. Considerations in clinical decision making. Expert Rev. Clin. Immunol. 2023, 19, 1041–1049. [Google Scholar] [CrossRef] [PubMed]
- Förster-Ruhrmann, U.; Stergioudi, D.; Szczepek, A.J.; Fluhr, J.W.; Zuberbier, T.; Olze, H.; Bergmann, K.-C. A real-life comparison of pulmonary and nasal outcomes in patients with severe asthma and nasal polyposis treated with T2-biologics. World Allergy Organ. J. 2023, 16, 100746. [Google Scholar] [CrossRef] [PubMed]
- Cai, S.; Xu, S.; Lou, H.; Zhang, L. Comparison of Different Biologics for Treating Chronic Rhinosinusitis with Nasal Polyps: A Network Analysis. J. Allergy Clin. Immunol. Pract. 2022, 10, 1876–1886.e7. [Google Scholar] [CrossRef]
- Miglani, A.; Soler, Z.M.; Smith, T.L.; Mace, J.C.; Schlosser, R.J. A comparative analysis of endoscopic sinus surgery versus biologics for treatment of chronic rhinosinusitis with nasal polyposis. Int. Forum Allergy Rhinol. 2022, 13, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wang, H.; Zhang, C.; Shi, L.; Zhang, Q.; Song, X.; Wang, D.; Hu, L.; Yu, H.; Sun, X. Comparative short-term efficacy of endoscopic sinus surgery and biological therapies in chronic rhinosinusitis with nasal polyps: A network meta-analysis. Clin. Transl. Allergy 2023, 13, e12269. [Google Scholar] [CrossRef]
- Maza-Solano, J.; Calvo-Henríquez, C.; Alobid, I.; Álvarez-Cendrero, M.; Palomares, Ó.; Moreno-Luna, R.; Santos-Perez, J.; González-García, J.; Sánchez-Gómez, S. Nasal Symptoms in Asthmatic Patients under Treatment with Anti-IL-5 Monoclonal Antibodies. A Real-Life Cohort Study. J. Clin. Med. 2022, 11, 7056. [Google Scholar] [CrossRef]
- Borish, L.; Cohen, N.A.; Chupp, G.; Hopkins, C.; Wagenmann, M.; Sousa, A.R.; Smith, S.G.; Silver, J.; Yang, S.; Mayer, B.; et al. Evaluating enrollment and outcome criteria in trials of biologics for chronic rhinosinusitis with nasal polyps. Ann. Allergy Asthma Immunol. 2022, 129, 160–168. [Google Scholar] [CrossRef]
- Siméon, R.; Soufflet, B.; Delacour, I.S. Coblation turbinate reduction in childhood allergic rhinitis. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2010, 127, 77–82. [Google Scholar] [CrossRef][Green Version]
- Abdullah, B.; Singh, S. Surgical Interventions for Inferior Turbinate Hypertrophy: A Comprehensive Review of Current Techniques and Technologies. Int. J. Environ. Res. Public Health 2021, 18, 3441. [Google Scholar] [CrossRef]
- Mimari, C.; Radulesco, T.; Penicaud, M.; Dessi, P.; Michel, J. Surgical management of chronic rhinosinusitis with nasal polyps under local anaesthesia: Indications and results. Acta Otorhinolaryngol. Ital. 2023, 43, 42–48. [Google Scholar] [CrossRef]
- Thamboo, A.; Kilty, S.; Witterick, I.; Chan, Y.; Chin, C.J.; Janjua, A.; Javer, A.; Lee, J.; Monterio, E.; Rotenberg, B.; et al. Canadian Rhinology Working Group consensus statement: Biologic therapies for chronic rhinosinusitis. J. Otolaryngol. Head Neck Surg. 2021, 50, 15. [Google Scholar] [CrossRef] [PubMed]
- Rizzi, A.; Gammeri, L.; Cordiano, R.; Valentini, M.; Centrone, M.; Marrone, S.; Inchingolo, R.; Lohmeyer, F.M.; Cavaliere, C.; Ria, F.; et al. Therapeutic Strategies to Prevent the Recurrence of Nasal Polyps after Surgical Treatment: An Update and In Vitro Study on Growth Inhibition of Fibroblasts. J. Clin. Med. 2023, 12, 2841. [Google Scholar] [CrossRef] [PubMed]
- Bai, J.; Huang, J.H.; Price, C.P.; Schauer, J.M.; Suh, L.A.; Harmon, R.; Conley, D.B.; Welch, K.C.; Kern, R.C.; Shintani-Smith, S.; et al. Prognostic factors for polyp recurrence in chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2022, 150, 352–361.e7. [Google Scholar] [CrossRef] [PubMed]
- Gelardi, M.; Bocciolini, C.; Notargiacomo, M.; Schiavetti, I.; Lingua, C.; Pecoraro, P.; Iannuzzi, L.; Quaranta, V.A.; Giancaspro, R.; Ronca, G.; et al. Chronic rhinosinusitis with nasal polyps: How to identify eligible patients for biologics in clinical practice. Acta Otorhinolaryngol. Ital. 2022, 42, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Mullol, J.; Azar, A.; Buchheit, K.M.; Hopkins, C.; Bernstein, J.A. Chronic Rhinosinusitis with Nasal Polyps: Quality of Life in the Biologics Era. J. Allergy Clin. Immunol. Pract. 2022, 10, 1434–1453.e9. [Google Scholar] [CrossRef]
- Fokkens, W.J.; Viskens, A.-S.; Backer, V.; Conti, D.; De Corso, E.; Gevaert, P.; Scadding, G.K.; Wagemann, M.; Bernal-Sprekelsen, M.; Chaker, A.; et al. EPOS/EUFOREA update on indication and evaluation of Biologics in Chronic Rhinosinusitis with Nasal Polyps 2023. Rhinol. J. 2023, 61, 194–202. [Google Scholar] [CrossRef]
| Study | Year | Patients | Controls | Country | Age | Type of Study | Duration of Treatment | Prior Surgical Intervention |
|---|---|---|---|---|---|---|---|---|
| Pinto JM [21] | 2010 | 7 | 7 | USA | Adults (18–75) | Randomized, placebo-controlled double-blind study | 24 weeks | Yes |
| Tajiri T [22] | 2013 | 6 | 0 | Japan | Adults | Prospective, uncontrolled study | 16 weeks | No |
| Gevaert P [23] | 2020 | 127 | 127 | USA, Europe | Adults (18–75) | Two randomized phase 3 trials | 24 weeks | |
| Kobayashi [24] | 2021 | 25 | 0 | Japan | Adults | Real-life study ECRS + Asthma | 52 weeks | No |
| Bidder T [27] | 2018 | 13 | 24 (surgery) | United Kingdom | Adults | Prospective study | 16 weeks | Yes |
| Carceller M [28] | 2020 | 23 | 0 | Spain | Adults | Multicenter retrospective analysis | 52 weeks | No |
| Haxel BR [26] | 2022 | 21 omalizumab | 49 dupilumab | Germany | Adults | Per protocol analysis—this real-world study | Yes | |
| Tat T [29] | 2022 | 17 | 0 | Turkey | Adults | Real-life experience study | 36 weeks | Yes |
| Zheng M [30] | 2022 | 22 | 0 | China | Adults | Real-life prospective study | 24 weeks | No |
| Study | Year | Patients | Controls | Country | Age | Type of Study | Duration of Treatment | Prior Surgical Intervention |
|---|---|---|---|---|---|---|---|---|
| Tversky (benralizumab) [33] | 2021 | 12 | 12 | USA | Adults | Randomized double-blind placebo-controlled trial | 20 weeks | Yes |
| Takabayashi (benralizumab) [34] | 2021 | 46 | 11 | Japan | Adults | A phase II, multicenter, randomized, placebo-controlled study | 12 weeks | No |
| Matsuno O (benralizumab) [36] | 2020 | 17 | 0 | Japan | Adults | Retrospectively real-life, single-center study | 52 weeks | No |
| Lombardo M (benralizumab) [38] | 2020 | 10 | 0 | Italy | Adults | Observational study | 24 weeks | Yes |
| Chitguppi (benralizumab) [37] | 2021 | 23 | 0 | USA | Adults | Retrospective review | 16 weeks | Yes |
| Nolasco S (benralizumab) [39] | 2021 | 137 | 0 | Italy | Adults | Multicenter observational study | 24 weeks | Yes |
| Bachert C (benralizumab) [35] | 2021 | 207 | 206 | Europe | Adults | Randomized, placebo-controlled trial | 12 weeks | Yes |
| Cavaliere C (benralizumab) [40] | 2022 | 11 | 10 | Italy | Adults | Retrospective study | 52 weeks | Yes |
| Santomasi C (benralizumab) [41] | 2023 | 17 | 0 | Italy | Adults | Bse | 52 weeks | No |
| Bachert C (mepolizumab) [43] | 2017 | 54 | 51 | Europe | Adults (18–79 years) | Randomized, double-blind, placebo-controlled trial | 25 weeks | |
| Joseph K Han (mepolizumab) [44] | 2021 | 206 | 201 | Europe, North America | Adults | Randomized, double-blind, placebo-controlled, phase 3 trial | 52 weeks | |
| Detoraki A (mepolizumab) [47] | 2021 | 44 | 0 | Italy | Adults | Prospective observational study | 48 weeks | Yes |
| Bachert C (mepolizumab) [45] | 2022 | 206 | 201 | Europe, North America | Adults | Phase 3, randomized, double-blind, placebo-controlled, parallel-group study | 52 weeks | |
| Gallo S (mepolizumab) [46] | 2022 | 43 | 0 | Italy | Adults | Multicentric retrospective no-profit observational study on severe asthmatic patients, treated with mepolizumab, and comorbid CRSwNP | 52 weeks | |
| Dominguez-Sosa (mepolizumab) [48] | 2023 | 55 | 0 | Spain | Adults | Single-center retrospective observational study | 24 weeks | Yes |
| Gevaert P (reslizumab) [49] | 2006 | 24 | Belgium | Adults | Double-blind, placebo-controlled, randomized, two-center safety and pharmacokinetic study | 8 weeks |
| Study | Year | Patients | Controls | Country | Age | Type of Study | Duration of Treatment | Prior Surgical Intervention |
|---|---|---|---|---|---|---|---|---|
| Jonstam K [51] | 2019 | 30 | 30 | USA, Europe | Adults | Randomized, double-blind, placebo-controlled, parallel-group study | 16 weeks | |
| Bachert C [52] | 2019 | 16 | 19 | Europe | Adults (18–65) | Randomized, double-blind, placebo-controlled study | 20 weeks | |
| Bachert C [53] | 2019 | 143 (SINUS-24) 150 (SINUS-52) | 133 (SINUS-24) 153 (SINUS-52) | 14 countries | Adults | Two multinational, multicenter, randomized, double-blind, placebo-controlled, parallel-group studies | 24 weeks SINUS 24 52 weeks SINUS 52 | |
| Bachert C [55] | 2020 | 30 | 30 | USA, Europe | Adults (18–65) | Randomized, double-blind, placebo-controlled, parallel-group study | 16 weeks | |
| Fujieda S [56] | 2021 | 33 | 16 | Japan | Adults | Phase 3, international, multicenter, randomized, placebo-controlled, double-blind SINUS-52 study | 52 weeks | |
| Berger P [61] | 2023 | 1101 | 611 | Europe, USA | Adults | TRAVERSE (NCT02134028) was an OLE that enrolled patients who had completed a previous phase 2 or 3 dupilumab asthma study | 96 weeks | |
| Hoffman A [64] | 2022 | 40 | 0 | Germany | Adults | Single-center, retrospective single-arm longitudinal study | 53 weeks | Yes |
| De Corso E [65] | 2023 | 57 | 0 | Italy | Adults | Monocentric observational study in a real-life setting | 48 weeks | Yes |
| Ottaviano G [66] | 2023 | 47 | 0 | Italy | Adults | Observational study in a real-life setting | 48 weeks | Yes |
| Galletti C [67] | 2023 | 63 | 0 | Italy | Adults | Observational cohort study | 48 weeks | Yes |
| Albrecht T [68] | 2023 | 68 | 0 | Germany | Adults | Prospective study | 48 weeks | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cergan, R.; Berghi, O.N.; Dumitru, M.; Vrinceanu, D.; Manole, F.; Serboiu, C.S. Biologics for Chronic Rhinosinusitis—A Modern Option for Therapy. Life 2023, 13, 2165. https://doi.org/10.3390/life13112165
Cergan R, Berghi ON, Dumitru M, Vrinceanu D, Manole F, Serboiu CS. Biologics for Chronic Rhinosinusitis—A Modern Option for Therapy. Life. 2023; 13(11):2165. https://doi.org/10.3390/life13112165
Chicago/Turabian StyleCergan, Romica, Ovidiu Nicolae Berghi, Mihai Dumitru, Daniela Vrinceanu, Felicia Manole, and Crenguta Sorina Serboiu. 2023. "Biologics for Chronic Rhinosinusitis—A Modern Option for Therapy" Life 13, no. 11: 2165. https://doi.org/10.3390/life13112165
APA StyleCergan, R., Berghi, O. N., Dumitru, M., Vrinceanu, D., Manole, F., & Serboiu, C. S. (2023). Biologics for Chronic Rhinosinusitis—A Modern Option for Therapy. Life, 13(11), 2165. https://doi.org/10.3390/life13112165










