Comparison between Novel Anatomical Locking Guide Plate and Conventional Locking Plate for Acetabular Fractures: A Finite Element Analysis
Abstract
1. Introduction
2. Methods
2.1. Three-Dimensional Modeling of the TAF
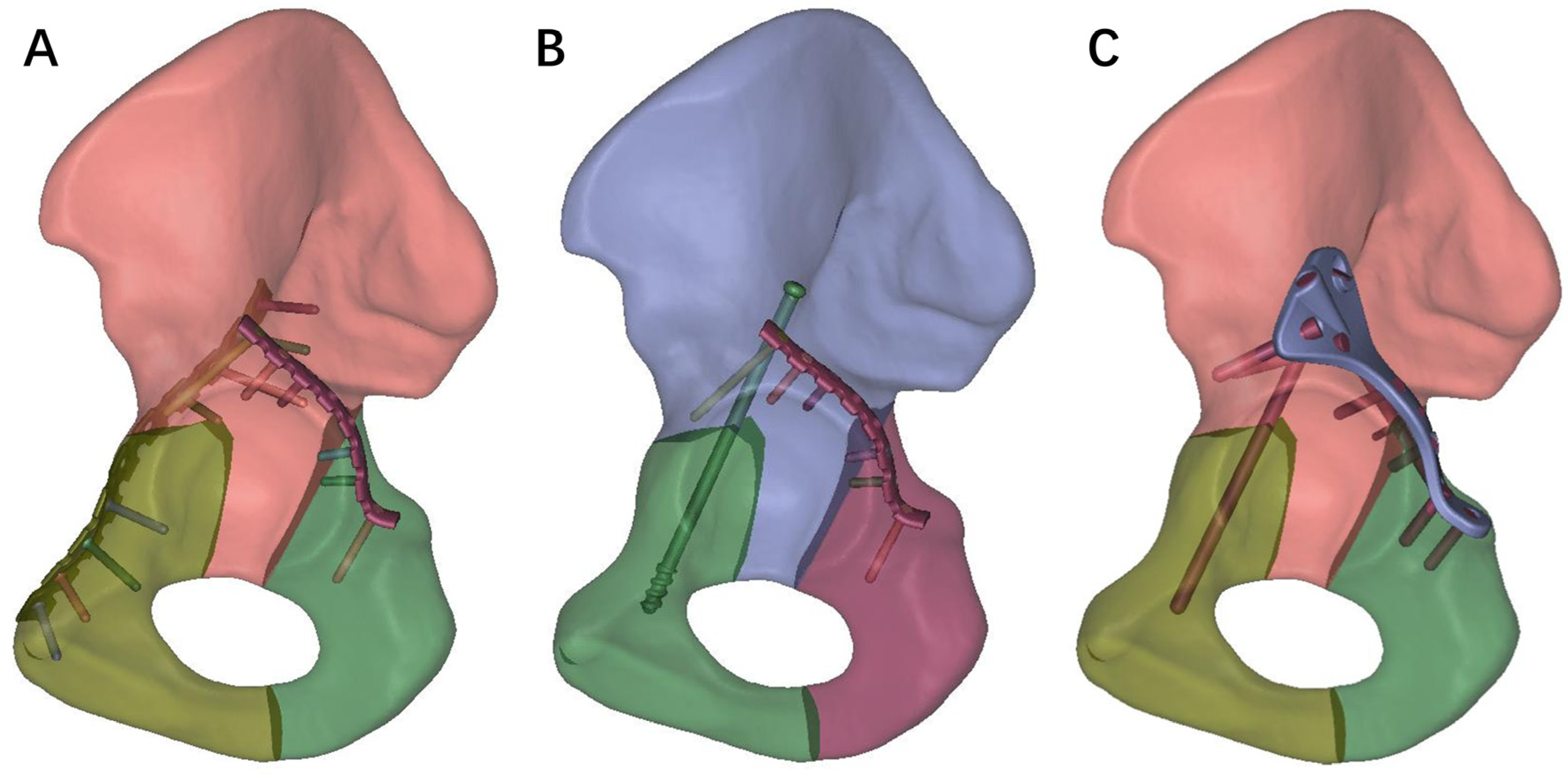
2.2. Geometric Modeling of Different Internal Fixations for TAF
2.3. Definition of the Boundary Conditions, Material Properties, and the Loading Modes
2.4. Evaluation Index of Three Internal Fixation Methods
3. Results
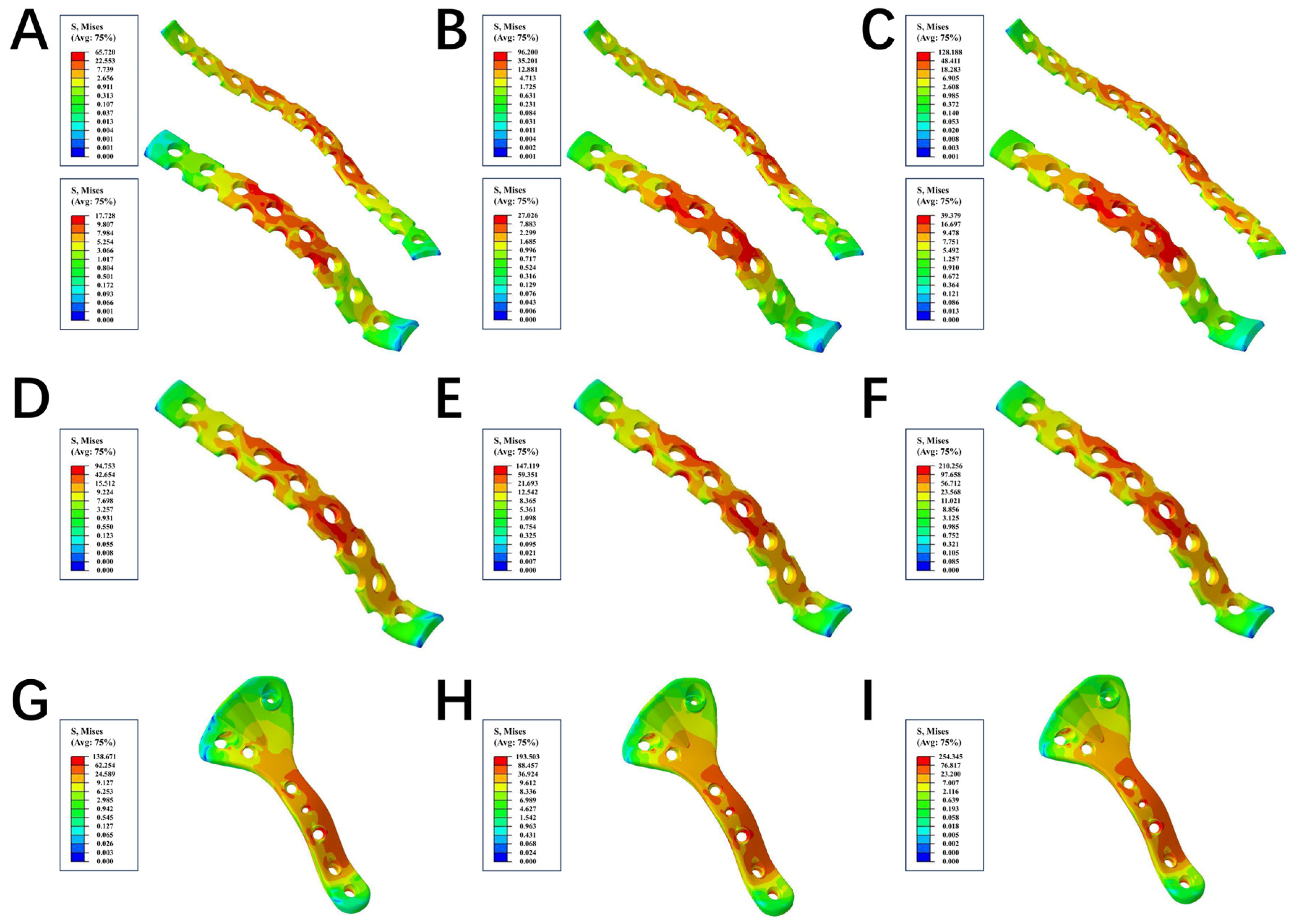
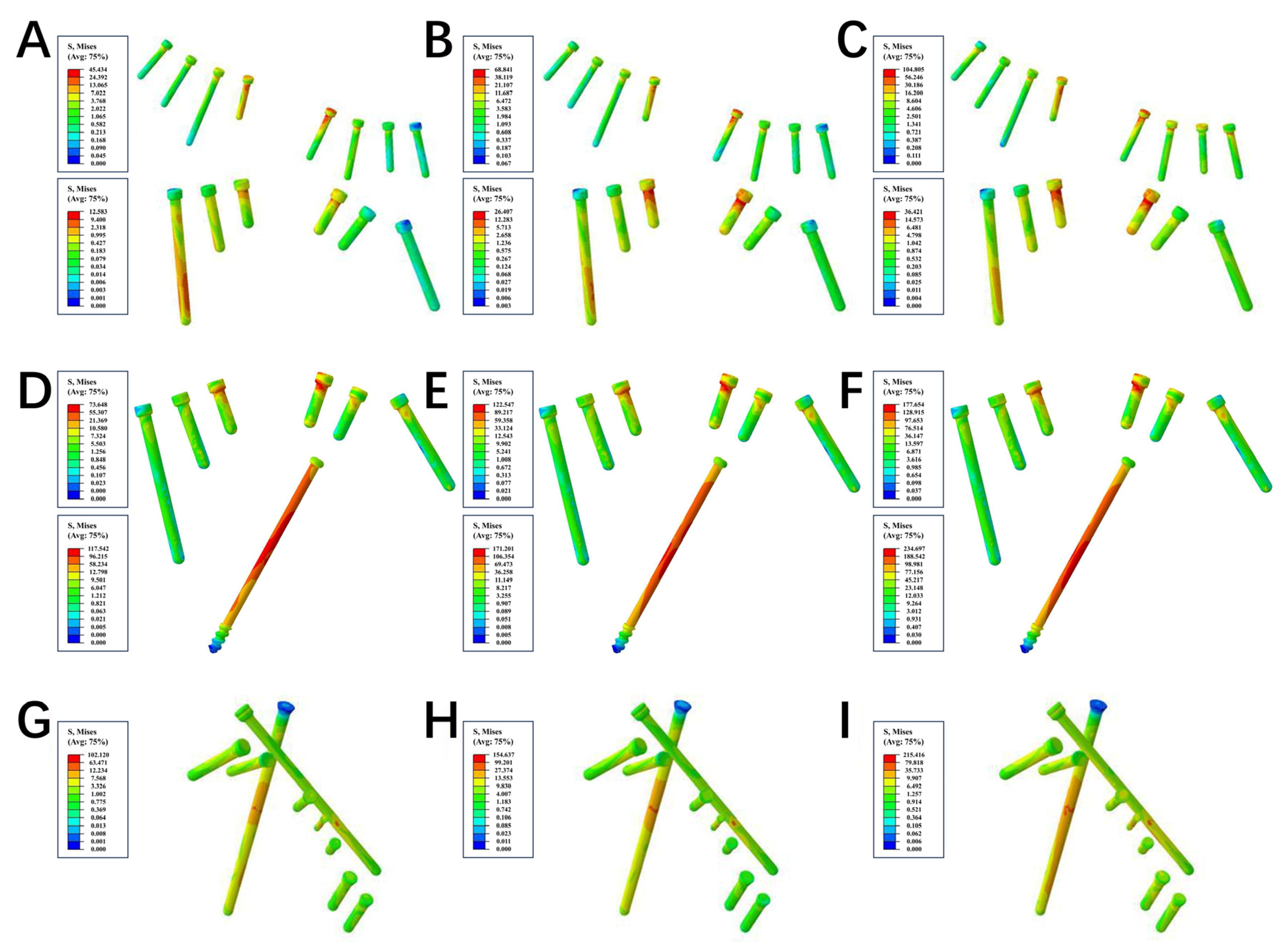
3.1. Stress Distribution and Stress Peak
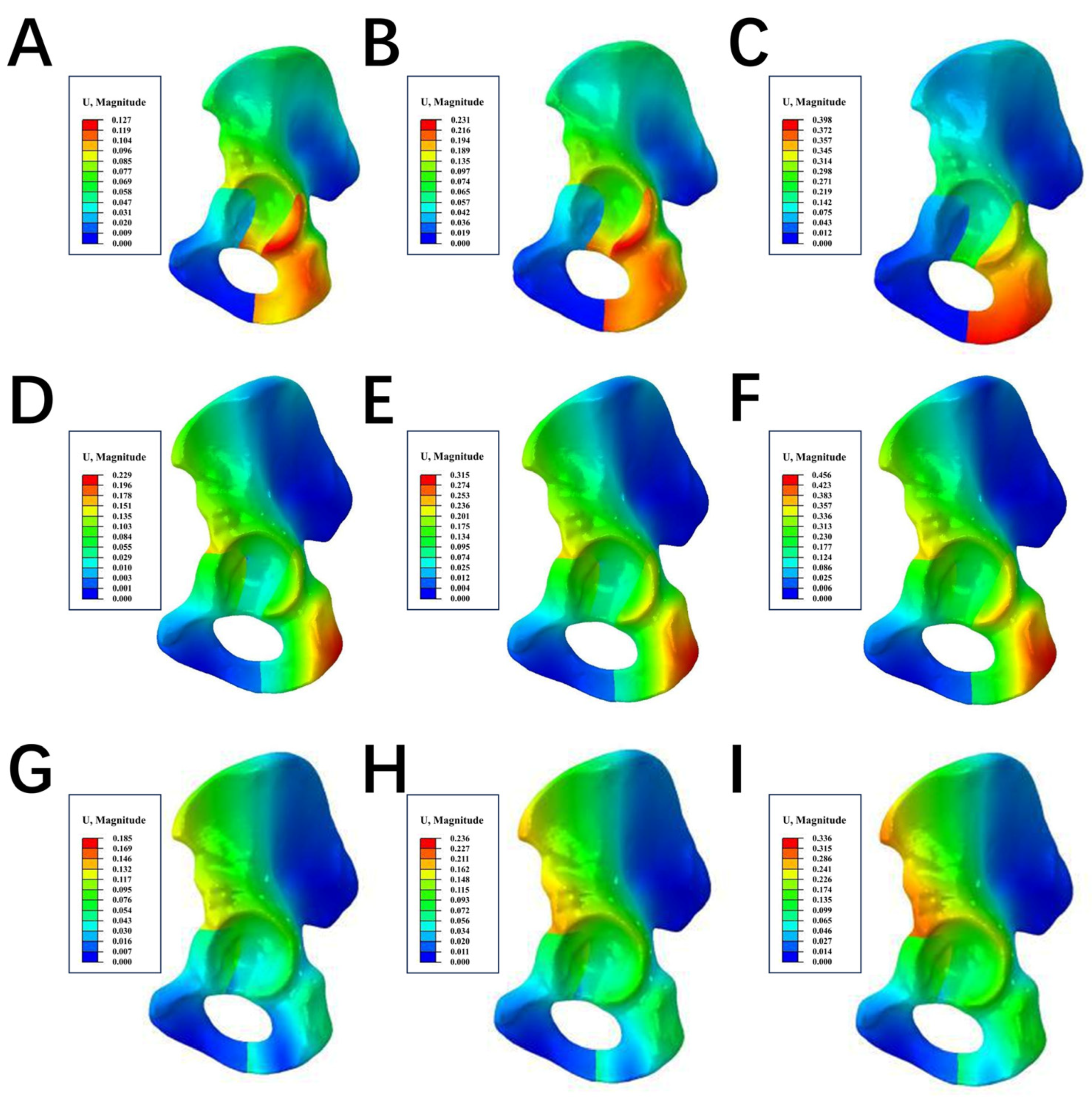
3.2. Displacement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Kelly, J.; Ladurner, A.; Rickman, M. Surgical management of acetabular fractures—A contemporary literature review. Injury 2020, 51, 2267–2277. [Google Scholar] [CrossRef] [PubMed]
- Letournel, E. Acetabulum Fractures: Classification and Management. J. Orthop. Trauma 2019, 33 (Suppl. S2), S1–S2. [Google Scholar] [CrossRef]
- Raobaikady, R.; Redman, J.; Ball, J.A.; Maloney, G.; Grounds, R.M. Use of activated recombinant coagulation factor VII in patients undergoing reconstruction surgery for traumatic fracture of pelvis or pelvis and acetabulum: A double-blind, randomized, placebo-controlled trial. Br. J. Anaesth. 2005, 94, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Küper, M.A.; Röhm, B.; Audretsch, C.; Stöckle, U.; Höch, A.; Histing, T.; Stuby, F.M.; Trulson, A.; Herath, S.C. Pararectus approach vs. Stoppa approach for the treatment of acetabular fractures—A comparison of approach-related complications and operative outcome parameters from the German Pelvic Registry. Orthop. Traumatol. Surg. Res. OTSR 2022, 108, 103275. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.L.; Tang, Y.Y. Displaced acetabular fractures in the elderly: Results after open reduction and internal fixation. Injury 2014, 45, 1908–1913. [Google Scholar] [CrossRef]
- Melhem, E.; Riouallon, G.; Habboubi, K.; Gabbas, M.; Jouffroy, P. Epidemiology of pelvic and acetabular fractures in France. Orthop. Traumatol. Surg. Res. OTSR 2020, 106, 831–839. [Google Scholar] [CrossRef]
- Papotto, G.; Testa, G.; Mobilia, G.; Perez, S.; Dimartino, S.; Giardina, S.M.C.; Sessa, G.; Pavone, V. Use of 3D printing and pre-contouring plate in the surgical planning of acetabular fractures: A systematic review. Orthop. Traumatol. Surg. Res. OTSR 2022, 108, 103111. [Google Scholar] [CrossRef]
- Zhang, L.; Lin, C.; Cao, S.; Wang, Y.; Peng, G.; Xu, Y.; Feng, Y.; Wang, G. Designation and Validation of a Posterior Anatomical Plate for the Anterior Column of the Acetabulum. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 948–952. [Google Scholar] [CrossRef]
- Wu, H.; Shang, R.; Cai, X.; Liu, X.; Song, C.; Chen, Y. Single Ilioinguinal Approach to Treat Complex Acetabular Fractures with Quadrilateral Plate Involvement: Outcomes Using a Novel Dynamic Anterior Plate-Screw System. Orthop. Surg. 2020, 12, 488–497. [Google Scholar] [CrossRef]
- Sakong, S.Y.; Cho, J.W.; Kim, B.S.; Park, S.J.; Lim, E.J.; Oh, J.K. The Clinical Efficacy of Contouring Periarticular Plates on a 3D Printed Bone Model. J. Pers. Med. 2023, 13, 1145. [Google Scholar] [CrossRef]
- Hsu, C.L.; Chou, Y.C.; Li, Y.T.; Chen, J.E.; Hung, C.C.; Wu, C.C.; Shen, H.C.; Yeh, T.T. Pre-operative virtual simulation and three-dimensional printing techniques for the surgical management of acetabular fractures. Int. Orthop. 2019, 43, 1969–1976. [Google Scholar] [CrossRef] [PubMed]
- Khajavi, K.; Lee, A.T.; Lindsey, D.P.; Leucht, P.; Bellino, M.J.; Giori, N.J. Single column locking plate fixation is inadequate in two column acetabular fractures. A biomechanical analysis. J. Orthop. Surg. Res. 2010, 5, 30. [Google Scholar] [CrossRef] [PubMed]
- Ferrante, H.; Schemitsch, E.H.; Zdero, R.; Bagheri, Z.S. Biomechanical analysis of fixation methods for acetabular fractures: A review. Med. Eng. Phys. 2021, 89, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Ye, P.; Guo, J.; Tian, S.; Wang, Z.; Li, J.; Zhao, R.; Hou, Z.; Zhang, Y. Is the T-shaped acetabular fracture really likes a “T”? A study based on three-dimensional fracture mapping. Injury 2022, 53, 3786–3794. [Google Scholar] [CrossRef]
- Yang, Y.; Zou, C.; Fang, Y.; Shakya, S. Clinical efficacy and its influencing factors of surgical treatment for T-shaped associated with posterior wall acetabular fractures using combined surgical approaches. BMC Surg. 2022, 22, 65. [Google Scholar] [CrossRef]
- Harris, A.M.; Althausen, P.; Kellam, J.F.; Bosse, M.J. Simultaneous anterior and posterior approaches for complex acetabular fractures. J. Orthop. Trauma 2008, 22, 494–497. [Google Scholar] [CrossRef]
- Stöckle, U.; Hoffmann, R.; Südkamp, N.P.; Reindl, R.; Haas, N.P. Treatment of complex acetabular fractures through a modified extended iliofemoral approach. J. Orthop. Trauma 2002, 16, 220–230. [Google Scholar] [CrossRef]
- Griffin, D.B.; Beaulé, P.E.; Matta, J.M. Safety and efficacy of the extended iliofemoral approach in the treatment of complex fractures of the acetabulum. J. Bone Jt. Surg. Br. Vol. 2005, 87, 1391–1396. [Google Scholar] [CrossRef]
- Bilekdemir, U.; Civan, O.; Cavit, A.; Özdemir, H. Acetabular fractures treated surgically: Which of the parameters affect prognosis. Ulus. Travma Ve Acil Cerrahi Derg. = Turk. J. Trauma Emerg. Surg. TJTES 2020, 26, 265–273. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Grotz, M.R.; Papakostidis, C.; Dinopoulos, H. Operative treatment of displaced fractures of the acetabulum. Meta-Anal. J. Bone Jt. Surg. Br. Vol. 2005, 87, 2–9. [Google Scholar] [CrossRef]
- Pavelka, T.; Houcek, P. [Complications associated with the surgical treatment of acetabular fractures]. Acta Chir. Orthop. Traumatol. Cechoslov. 2009, 76, 186–193. [Google Scholar] [CrossRef]
- Shaath, M.K.; Avilucea, F.R.; Routt, M.L.C., Jr. Transverse and transverse-variant acetabular fractures with ipsilateral sacroiliac joint injuries: A technical note for reduction and stabilization. Injury 2021, 52, 1083–1088. [Google Scholar] [CrossRef]
- Hammad, A.S.; El-Khadrawe, T.A.; Waly, A.H.; Abu-Sheasha, G.A. The efficacy of posterior plating and anterior column screw fixation in the management of T-shaped acetabular fractures—CART analysis of prospective cohort study. Injury 2017, 48, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Kistler, B.J.; Smithson, I.R.; Cooper, S.A.; Cox, J.L.; Nayak, A.N.; Santoni, B.G.; Sagi, H.C. Are quadrilateral surface buttress plates comparable to traditional forms of transverse acetabular fracture fixation? Clin. Orthop. Relat. Res. 2014, 472, 3353–3361. [Google Scholar] [CrossRef] [PubMed]
- Krappinger, D.; Schwendinger, P.; Lindtner, R.A. Fluoroscopically guided acetabular posterior column screw fixation via an anterior approach. Oper. Orthop. Traumatol. 2019, 31, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Zhang, S.; Luo, Q.; Fang, J.; Lin, C.; Leung, F.; Chen, B. Definition of a safe zone for antegrade lag screw fixation of fracture of posterior column of the acetabulum by 3D technology. Injury 2016, 47, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Le Quang, H.; Schmoelz, W.; Lindtner, R.A.; Schwendinger, P.; Blauth, M.; Krappinger, D. Biomechanical comparison of fixation techniques for transverse acetabular fractures—Single-leg stance vs. sit-to-stand loading. Injury 2020, 51, 2158–2164. [Google Scholar]
- Yildirim, A.O.; Alemdaroglu, K.B.; Yuksel, H.Y.; Öken, Ö.F.; Ucaner, A. Finite element analysis of the stability of transverse acetabular fractures in standing and sitting positions by different fixation options. Injury 2015, 46 (Suppl. S2), S29–S35. [Google Scholar] [CrossRef]
- Maini, L.; Verma, T.; Sharma, A.; Sharma, A.; Mishra, A.; Jha, S. Evaluation of accuracy of virtual surgical planning for patient-specific pre-contoured plate in acetabular fracture fixation. Arch. Orthop. Trauma Surg. 2018, 138, 495–504. [Google Scholar] [CrossRef]
- Baumgaertner, M.R. Fractures of the posterior wall of the acetabulum. J. Am. Acad. Orthop. Surg. 1999, 7, 54–65. [Google Scholar] [CrossRef]
- Xu, M.; Zhang, L.H.; Zhang, Y.Z.; He, C.Q.; Zhang, L.C.; Wang, Y.; Tang, P.-F. Development of site-specific locking plates for acetabular fractures. Orthopedics 2013, 36, e593–e600. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Zhang, L.H.; Zhang, Y.Z.; Zhang, L.C.; He, C.Q.; Wang, Y.; Tang, P.-F. Custom-made locked plating for acetabular fracture: A pilot study in 24 consecutive cases. Orthopedics 2014, 37, e660–e670. [Google Scholar] [CrossRef] [PubMed]
- Gusic, N.; Sabalic, S.; Pavic, A.; Ivkovic, A.; Sotosek-Tokmadzic, V.; Cicvaric, T. Rationale for more consistent choice of surgical approaches for acetabular fractures. Injury 2015, 46 (Suppl. S6), S78–S86. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, W.; Mullis, B.; Liu, D.; Xiong, Q.; Lv, H.; Ji, X.; Peng, Y.; Tang, P. Percutaneous Anterior Column Fixation for Acetabulum Fractures, Does It Have to Be Difficult?-The New Axial Pedicle View of the Anterior Column for Percutaneous Fixation. J. Orthop. Trauma 2016, 30, e30–e35. [Google Scholar] [CrossRef]
- Zhang, L.H.; Zhang, L.C.; Si, Q.H.; Gao, Y.; Su, X.Y.; Zhao, Z.; Tang, P.-F. Experimental study on treatment of acetabular anterior column fractures: Applyment of a minimally invasive percutaneous lag screw guide apparatus. BMC Musculoskelet. Disord. 2016, 17, 27. [Google Scholar] [CrossRef]
- Pierannunzii, L.; Fischer, F.; Tagliabue, L.; Calori, G.M.; d’Imporzano, M. Acetabular both-column fractures: Essentials of operative management. Injury 2010, 41, 1145–1149. [Google Scholar] [CrossRef]
- Anderson, A.E.; Peters, C.L.; Tuttle, B.D.; Weiss, J.A. Subject-specific finite element model of the pelvis: Development, validation and sensitivity studies. J. Biomech. Eng. 2005, 127, 364–373. [Google Scholar] [CrossRef]
- Dalstra, M.; Huiskes, R. Load transfer across the pelvic bone. J. Biomech. 1995, 28, 715–724. [Google Scholar] [CrossRef]
- Letournel, E. Acetabulum fractures: Classification and management. Clin. Orthop. Relat. Res. 1980, 151, 81–106. [Google Scholar] [CrossRef]
- Durkee, N.J.; Jacobson, J.; Jamadar, D.; Karunakar, M.A.; Morag, Y.; Hayes, C. Classification of common acetabular fractures: Radiographic and CT appearances. AJR Am. J. Roentgenol. 2006, 187, 915–925. [Google Scholar] [CrossRef]
- Deng, J.; Li, M.; Li, J.; Li, Z.; Meng, F.; Zhou, Y.; Tang, P.; Zhao, Y.; Zhang, L. Finite Element Analysis of a Novel Anatomical Locking Guide Plate for Anterior Column and Posterior Hemi-Transverse Acetabular Fractures. J. Med. Biol. Eng. 2021, 41, 895–903. [Google Scholar] [CrossRef]
- Niinomi, M. Mechanical biocompatibilities of titanium alloys for biomedical applications. J. Mech. Behav. Biomed. Mater. 2008, 1, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Becker, C.A.; Kammerlander, C.; Cavalcanti Kußmaul, A.; Dotzauer, F.; Woiczinski, M.; Rubenbauer, B.; Sommer, F.; Linhart, C.; Weidert, S.; Zeckey, C.; et al. Minimally invasive screw fixation is as stable as anterior plating in acetabular T-Type fractures—A biomechanical study. Orthop. Traumatol. Surg. Res. OTSR 2018, 104, 1055–1061. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Yang, F.; Yao, S.; Xiong, Z.; Sun, T.; Guo, X. Biomechanical Comparison of Different Fixation Techniques for Typical Acetabular Fractures in the Elderly: The Role of Special Quadrilateral Surface Buttress Plates. J. Bone Jt. Surg. Am. Vol. 2020, 102, e81. [Google Scholar] [CrossRef] [PubMed]
- Ji, T.; Guo, W.; Tang, X.D.; Yang, Y. Reconstruction of type II+III pelvic resection with a modular hemipelvic endoprosthesis: A finite element analysis study. Orthop. Surg. 2010, 2, 272–277. [Google Scholar] [CrossRef]
- Li, D.; Ren, H.; Zhang, X.; Ao, R.; Yi, C.; Yu, B. Finite Element Analysis of Channel Screw and Conventional Plate Technique in Tile B2 Pelvic Fracture. J. Pers. Med. 2023, 13, 506. [Google Scholar] [CrossRef]
- Zhang, D.; Liu, N.; Chen, Y.; Zhang, G.; Tian, J.; Kong, F.; Xiao, S.; Sun, J. Microstructure Evolution and Mechanical Properties of PM-Ti43Al9V0.3Y Alloy. Materials 2020, 13, 198. [Google Scholar] [CrossRef]
- Chang, J.K.; Gill, S.S.; Zura, R.D.; Krause, W.R.; Wang, G.J. Comparative strength of three methods of fixation of transverse acetabular fractures. Clin. Orthop. Relat. Res. 2001, 392, 433–441. [Google Scholar] [CrossRef]
- Steiner, M.; Claes, L.; Ignatius, A.; Simon, U.; Wehner, T. Numerical simulation of callus healing for optimization of fracture fixation stiffness. PLoS ONE 2014, 9, e101370. [Google Scholar] [CrossRef]

| Model | Acetabular | Internal Fixations | ||
|---|---|---|---|---|
| Nodes | Elements | Nodes | Elements | |
| DLP | 188916 | 1006841 | 203938 | 122873 |
| LPACS | 187144 | 1000072 | 273578 | 178458 |
| NALGP | 188507 | 1001865 | 314224 | 204542 |
| Material Type | Elastic Modulus (MPa) | Poisson’s Ratio |
|---|---|---|
| Cortical bone | 12,400 | 0.3 |
| Cancellous bone | 77 | 0.3 |
| Instrument | 110,000 | 0.3 |
| Stress (MPa) | |||
|---|---|---|---|
| 200 N | 400 N | 600 N | |
| DLP (anterior plate) | 65.72 | 96.2 | 128.188 |
| DLP (posterior plate) | 17.728 | 27.026 | 39.379 |
| LPACS (posterior plate) | 94.753 | 147.119 | 210.256 |
| NALGP (posterior plate) | 138.671 | 193.503 | 254.345 |
| Stress (MPa) | |||
|---|---|---|---|
| 200 N | 400 N | 600 N | |
| DLP (anterior screw) | 45.434 | 68.841 | 104.805 |
| DLP (posterior screw) | 12.583 | 26.407 | 36.421 |
| LPACS (anterior screw) | 117.542 | 171.201 | 234.697 |
| LPACS (posterior screw) | 73.648 | 122.547 | 177.654 |
| NALGP (posterior screw) | 102.12 | 154.637 | 215.416 |
| The Maximum Displacement (mm) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| ACF | PCF | IPBF | |||||||
| 200 N | 400 N | 600 N | 200 N | 400 N | 600 N | 200 N | 400 N | 600 N | |
| DLP | 0.090 | 0.188 | 0.274 | 0.126 | 0.227 | 0.306 | 0.117 | 0.223 | 0.338 |
| LPACS | 0.164 | 0.255 | 0.367 | 0.158 | 0.249 | 0.352 | 0.130 | 0.225 | 0.341 |
| NALGP | 0.145 | 0.215 | 0.326 | 0.113 | 0.157 | 0.216 | 0.124 | 0.152 | 0.195 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, X.; Gao, J.; Wu, X.; Deng, J.; Li, Z.; Li, R.; Zhang, L.; Liu, J.; Li, M. Comparison between Novel Anatomical Locking Guide Plate and Conventional Locking Plate for Acetabular Fractures: A Finite Element Analysis. Life 2023, 13, 2108. https://doi.org/10.3390/life13112108
Liu X, Gao J, Wu X, Deng J, Li Z, Li R, Zhang L, Liu J, Li M. Comparison between Novel Anatomical Locking Guide Plate and Conventional Locking Plate for Acetabular Fractures: A Finite Element Analysis. Life. 2023; 13(11):2108. https://doi.org/10.3390/life13112108
Chicago/Turabian StyleLiu, Xiao, Jianpeng Gao, Xiaoyong Wu, Junhao Deng, Zijian Li, Ran Li, Licheng Zhang, Jianheng Liu, and Ming Li. 2023. "Comparison between Novel Anatomical Locking Guide Plate and Conventional Locking Plate for Acetabular Fractures: A Finite Element Analysis" Life 13, no. 11: 2108. https://doi.org/10.3390/life13112108
APA StyleLiu, X., Gao, J., Wu, X., Deng, J., Li, Z., Li, R., Zhang, L., Liu, J., & Li, M. (2023). Comparison between Novel Anatomical Locking Guide Plate and Conventional Locking Plate for Acetabular Fractures: A Finite Element Analysis. Life, 13(11), 2108. https://doi.org/10.3390/life13112108







