Coronary Vasospastic Angina: A Review of the Pathogenesis, Diagnosis, and Management
Abstract
1. Introduction
2. Epidemiology
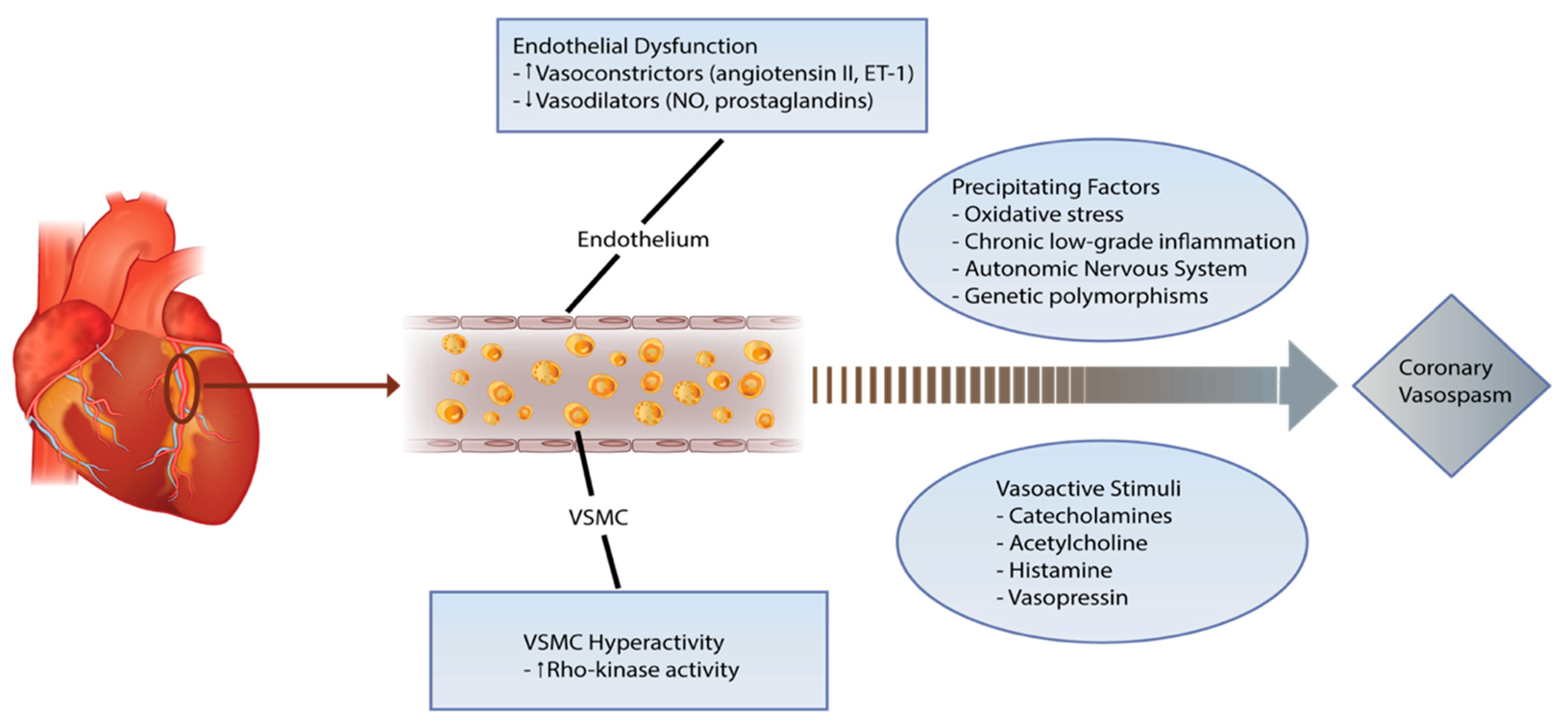
3. Pathophysiology
4. Clinical Spectrum
5. Diagnostic Approach
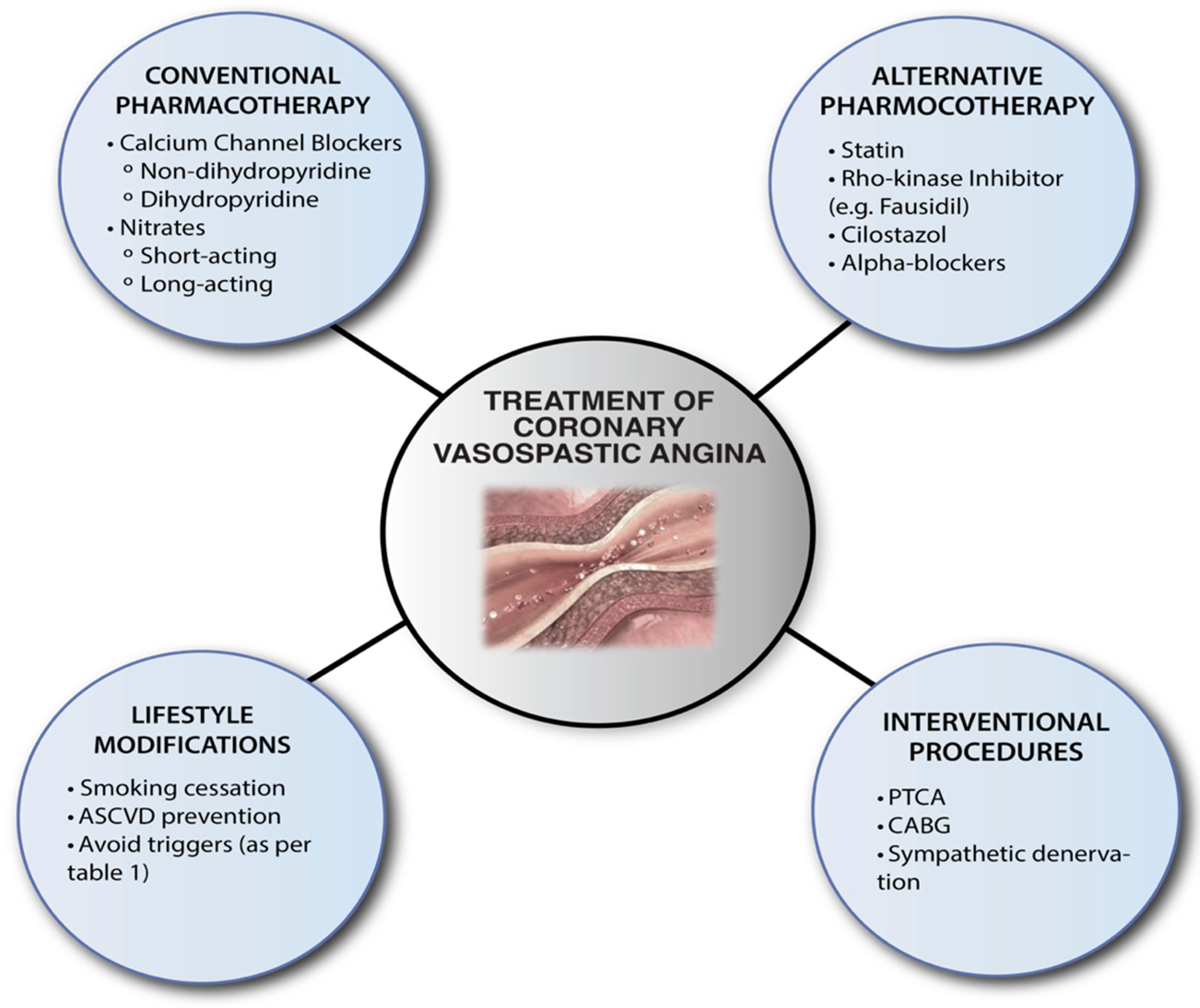
6. Management
7. Prognosis
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prinzmetal, M.; Kennamer, R.; Merliss, R.; Wada, T.; Bor, N. Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am. J. Med. 1959, 27, 375–388. [Google Scholar] [CrossRef]
- Yasue, H.; Touyama, M.; Shimamoto, M.; Kato, H.; Tanaka, S. Role of autonomic nervous system in the pathogenesis of Prinzmetal’s variant form of angina. Circulation 1974, 50, 534–539. [Google Scholar] [CrossRef]
- Yasue, H.; Touyama, M.; Kato, H.; Tanaka, S.; Akiyama, F. Prinzmetal’s variant form of angina as a manifestation of alpha-adrenergic receptor-mediated coronary artery spasm: Documentation by coronary arteriography. Am. Heart J. 1976, 91, 148–155. [Google Scholar] [CrossRef]
- Maseri, A.; Severi, S.; Nes, M.D.; L’Abbate, A.; Chierchia, S.; Marzilli, M.; Ballestra, A.M.; Parodi, O.; Biagini, A.; Distante, A. “Variant” angina: One aspect of a continuous spectrum of vasospastic myocardial ischemia. Pathogenetic mechanisms, estimated incidence and clinical and coronary arteriographic findings in 138 patients. Am. J. Cardiol. 1978, 42, 1019–1035. [Google Scholar] [CrossRef]
- Yasue, H.; Omote, S.; Takizawa, A.; Masao, N.; Hyon, H.; Nishida, S.; Horie, M. Comparison of coronary arteriographic findings during angina pectoris associated with S-T elevation or depression. Am. J. Cardiol. 1981, 47, 539–546. [Google Scholar] [CrossRef]
- Tateishi, K.; Saito, Y.; Kitahara, H.; Shoji, T.; Kadohira, T.; Nakayama, T.; Fujimoto, Y.; Kobayashi, Y. Safety and usefulness of acetylcholine provocation test in patients with no culprit lesions on emergency coronary angiography. Int. J. Cardiol. 2018, 269, 27–30. [Google Scholar] [CrossRef]
- Bertrand, M.E.; LaBlanche, J.M.; Tilmant, P.Y.; Thieuleux, F.A.; Delforge, M.R.; Carre, A.G.; Asseman, P.; Berzin, B.; Libersa, C.; Laurent, J.M. Frequency of provoked coronary arterial spasm in 1089 consecutive patients undergoing coronary arteriography. Circulation 1982, 65, 1299–1306. [Google Scholar] [CrossRef]
- Hung, M.Y.; Hsu, K.H.; Hung, M.J.; Cheng, C.W.; Cherng, W.J. Interactions among gender, age, hypertension and C-reactive protein in coronary vasospasm. Eur. J. Clin. Investig. 2010, 40, 1094–1103. [Google Scholar] [CrossRef]
- Sueda, S.; Kohno, H.; Fukuda, H.; Ochi, N.; Kawada, H.; Hayashi, Y.; Uraoka, T. Frequency of provoked coronary spasms in patients undergoing coronary arteriography using a spasm provocation test via intracoronary administration of ergonovine. Angiology 2004, 55, 403–411. [Google Scholar] [CrossRef]
- JCS Joint Working Group. Guidelines for Diagnosis and Treatment of Patients with Vasospastic Angina (Coronary Spastic Angina) (JCS 2013) (Digest Version). Circ. J. 2014, 78, 2779–2801. [Google Scholar] [CrossRef]
- Beltrame, J.F.; Sasayama, S.; Maseri, A. Racial heterogeneity in coronary artery vasomotor reactivity: Differences between Japanese and Caucasian patients. J. Am. Coll. Cardiol. 1999, 33, 1442–1452. [Google Scholar] [CrossRef]
- Walling, A.; Waters, D.D.; Miller, D.D.; Roy, D.; Pelletier, G.B.; Théroux, P. Long-term prognosis of patients with variant angina. Circulation 1987, 76, 990–997. [Google Scholar] [CrossRef]
- Haddock, R.E.; Hill, C.E. Rhythmicity in arterial smooth muscle. J. Physiol. 2005, 566, 645–656. [Google Scholar] [CrossRef]
- Yasue, H.; Mizuno, Y.; Harada, E. Coronary artery spasm—Clinical features, pathogenesis and treatment. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2019, 95, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Lanza, G.A.; Careri, G.; Crea, F. Mechanisms of coronary artery spasm. Circulation 2011, 124, 1774–1782. [Google Scholar] [CrossRef] [PubMed]
- Nakano, T.; Osanai, T.; Tomita, H.; Sekimata, M.; Homma, Y.; Okumura, K. Enhanced activity of variant phospholipase C-delta1 protein (R257H) detected in patients with coronary artery spasm. Circulation 2002, 105, 2024–2029. [Google Scholar] [CrossRef] [PubMed]
- Chutkow, W.A.; Pu, J.; Wheeler, M.T.; Wada, T.; Makielski, J.C.; Burant, C.F.; McNally, E.M. Episodic coronary artery vasospasm and hypertension develop in the absence of Sur2 K(ATP) channels. J. Clin. Investig. 2002, 110, 203–208. [Google Scholar] [CrossRef]
- Büssemaker, E.; Pistrosch, F.; Förster, S.; Herbrig, K.; Gross, P.; Passauer, J.; Brandes, R.P. Rho kinase contributes to basal vascular tone in humans: Role of endothelium-derived nitric oxide. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H541–H547. [Google Scholar] [CrossRef]
- Kakkar, R.; Ye, B.; Stoller, D.A.; Smelley, M.; Shi, N.Q.; Galles, K.; Hadhazy, M.; Makielski, J.C.; McNally, E.M. Spontaneous coronary vasospasm in KATP mutant mice arises from a smooth muscle-extrinsic process. Circ. Res. 2006, 98, 682–689. [Google Scholar] [CrossRef]
- Sandoo, A.; van Zanten, J.J.; Metsios, G.S.; Carroll, D.; Kitas, G.D. The endothelium and its role in regulating vascular tone. Open Cardiovasc. Med. J. 2010, 4, 302–312. [Google Scholar] [CrossRef]
- Shimokawa, H. 2014 Williams Harvey Lecture: Importance of coronary vasomotion abnormalities—from bench to bedside†. Eur. Heart J. 2014, 35, 3180–3193. [Google Scholar] [CrossRef] [PubMed]
- Takaoka, K.; Yoshimura, M.; Ogawa, H.; Kugiyama, K.; Nakayama, M.; Shimasaki, Y.; Mizuno, Y.; Sakamoto, T.; Yasue, H. Comparison of the risk factors for coronary artery spasm with those for organic stenosis in a Japanese population: Role of cigarette smoking. Int. J. Cardiol. 2000, 72, 121–126. [Google Scholar] [CrossRef]
- Ong, P.; Aziz, A.; Hansen, H.S.; Prescott, E.; Athanasiadis, A.; Sechtem, U. Structural and Functional Coronary Artery Abnormalities in Patients with Vasospastic Angina Pectoris. Circ. J. 2015, 79, 1431–1438. [Google Scholar] [CrossRef]
- Yoo, S.-Y.; Kim, J.-Y. Recent insights into the mechanisms of vasospastic angina. Korean Circ. J. 2009, 39, 505–511. [Google Scholar] [CrossRef]
- Yasue, H.; Hirai, N.; Mizuno, Y.; Harada, E.; Itoh, T.; Yoshimura, M.; Kugiyama, K.; Ogawa, H. Low-grade inflammation, thrombogenicity, and atherogenic lipid profile in cigarette smokers. Circ. J. 2006, 70, 8–13. [Google Scholar] [CrossRef]
- Ohyama, K.; Matsumoto, Y.; Takanami, K.; Ota, H.; Nishimiya, K.; Sugisawa, J.; Tsuchiya, S.; Amamizu, H.; Uzuka, H.; Suda, A.; et al. Coronary Adventitial and Perivascular Adipose Tissue Inflammation in Patients with Vasospastic Angina. J. Am. Coll. Cardiol. 2018, 71, 414–425. [Google Scholar] [CrossRef] [PubMed]
- Waters, D.D.; Miller, D.D.; Bouchard, A.; Bosch, X.; Theroux, P. Circadian variation in variant angina. Am. J. Cardiol. 1984, 54, 61–64. [Google Scholar] [CrossRef]
- Robertson, R.M.; Bernard, Y.; Robertson, D. Arterial and coronary sinus catecholamines in the course of spontaneous coronary artery spasm. Am. Heart J. 1983, 105, 901–906. [Google Scholar] [CrossRef]
- King, M.J.; Zir, L.M.; Kaltman, A.J.; Fox, A.C. Variant angina associated with angiographically demonstrated coronary artery spasm and REM sleep. Am. J. Med. Sci. 1973, 265, 419–422. [Google Scholar] [CrossRef]
- Pristipino, C.; Beltrame, J.F.; Finocchiaro, M.L.; Hattori, R.; Fujita, M.; Mongiardo, R.; Cianflone, D.; Sanna, T.; Sasayama, S.; Maseri, A. Major racial differences in coronary constrictor response between Japanese and Caucasians with recent myocardial infarction. Circulation 2000, 101, 1102–1108. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Takahashi, J.; Odaka, Y.; Suda, A.; Sueda, S.; Teragawa, H.; Ishii, K.; Kiyooka, T.; Hirayama, A.; Sumiyoshi, T.; et al. Clinical characteristics and long-term prognosis of contemporary patients with vasospastic angina: Ethnic differences detected in an international comparative study. Int. J. Cardiol. 2019, 291, 13–18. [Google Scholar] [CrossRef]
- Park, J.S.; Zhang, S.Y.; Jo, S.H.; Seo, J.B.; Li, L.; Park, K.W.; Oh, B.H.; Park, Y.B.; Kim, H.S. Common adrenergic receptor polymorphisms as novel risk factors for vasospastic angina. Am. Heart J. 2006, 151, 864–869. [Google Scholar] [CrossRef]
- Oike, Y.; Hata, A.; Ogata, Y.; Numata, Y.; Shido, K.; Kondo, K. Angiotensin converting enzyme as a genetic risk factor for coronary artery spasm. Implication in the pathogenesis of myocardial infarction. J. Clin. Investig. 1995, 96, 2975–2979. [Google Scholar] [CrossRef] [PubMed]
- Murase, Y.; Yamada, Y.; Hirashiki, A.; Ichihara, S.; Kanda, H.; Watarai, M.; Takatsu, F.; Murohara, T.; Yokota, M. Genetic risk and gene-environment interaction in coronary artery spasm in Japanese men and women. Eur. Heart J. 2004, 25, 970–977. [Google Scholar] [CrossRef]
- Ito, T.; Yasue, H.; Yoshimura, M.; Nakamura, S.; Nakayama, M.; Shimasaki, Y.; Harada, E.; Mizuno, Y.; Kawano, H.; Ogawa, H. Paraoxonase gene Gln192Arg (Q192R) polymorphism is associated with coronary artery spasm. Hum. Genet. 2002, 110, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Inoue, N.; Kawashima, S.; Kanazawa, K.; Yamada, S.; Akita, H.; Yokoyama, M. Polymorphism of the NADH/NADPH oxidase p22 phox gene in patients with coronary artery disease. Circulation 1998, 97, 135–137. [Google Scholar] [CrossRef]
- Chen, C.H.; Ferreira, J.C.; Gross, E.R.; Mochly-Rosen, D. Targeting aldehyde dehydrogenase 2: New therapeutic opportunities. Physiol. Rev. 2014, 94, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Park, C.S.; Kim, I.; Oh, G.C.; Han, J.-K.; Yang, H.-M.; Park, K.W.; Cho, H.-J.; Kang, H.-J.; Koo, B.-K.; Chung, W.-Y.; et al. Diagnostic Utility and Pathogenic Role of Circulating MicroRNAs in Vasospastic Angina. J. Clin. Med. 2020, 9, 1313. [Google Scholar] [CrossRef] [PubMed]
- Miyagi, H.; Yasue, H.; Okumura, K.; Ogawa, H.; Goto, K.; Oshima, S. Effect of magnesium on anginal attack induced by hyperventilation in patients with variant angina. Circulation 1989, 79, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Yasue, H.; Okumura, K.; Matsuyama, K.; Kugiyama, K.; Miyagi, H.; Higashi, T. Magnesium deficiency detected by intravenous loading test in variant angina pectoris. Am. J. Cardiol. 1990, 65, 709–712. [Google Scholar] [CrossRef]
- Libby, P.; Bornfeldt, K.E.; Tall, A.R. Atherosclerosis: Successes, Surprises, and Future Challenges. Circ. Res. 2016, 118, 531–534. [Google Scholar] [CrossRef]
- Yasue, H.; Nakagawa, H.; Itoh, T.; Harada, E.; Mizuno, Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J. Cardiol. 2008, 51, 2–17. [Google Scholar] [CrossRef]
- Yasue, H.; Kugiyama, K. Coronary spasm: Clinical features and pathogenesis. Intern. Med. 1997, 36, 760–765. [Google Scholar] [CrossRef]
- Nakagawa, H.; Morikawa, Y.; Mizuno, Y.; Harada, E.; Ito, T.; Matsui, K.; Saito, Y.; Yasue, H. Coronary spasm preferentially occurs at branch points: An angiographic comparison with atherosclerotic plaque. Circ. Cardiovasc. Interv. 2009, 2, 97–104. [Google Scholar] [CrossRef]
- Rapold, H.J.; Grimaudo, V.; Declerck, P.J.; Kruithof, E.K.; Bachmann, F. Plasma levels of plasminogen activator inhibitor type 1, beta-thromboglobulin, and fibrinopeptide A before, during, and after treatment of acute myocardial infarction with alteplase. Blood 1991, 78, 1490–1495. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, S.; Ogawa, H.; Soejima, H.; Takazoe, K.; Sakamoto, T.; Yoshimura, M.; Kugiyama, K.; Yasue, H. Formation of platelet aggregates after attacks of coronary spastic angina pectoris. Am. J. Cardiol. 2000, 85, 494–497. [Google Scholar] [CrossRef]
- Ong, P.; Athanasiadis, A.; Hill, S.; Vogelsberg, H.; Voehringer, M.; Sechtem, U. Coronary artery spasm as a frequent cause of acute coronary syndrome: The CASPAR (Coronary Artery Spasm in Patients with Acute Coronary Syndrome) Study. J. Am. Coll. Cardiol. 2008, 52, 523–527. [Google Scholar] [CrossRef]
- Morimoto, S.-I.; Shiga, Y.; Hiramitsu, S.; Yamada, K.; Nomura, S.; Miyagi, Y.; Nomura, M.; Mizuno, Y. Plaque rupture possibly induced by coronary spasm: An autopsy case of acute myocardial infarction. Jpn. Circ. J. 1988, 52, 1286–1292. [Google Scholar] [CrossRef] [PubMed]
- Oshima, S.; Yasue, H.; Ogawa, H.; Okumura, K.; Matsuyama, K. Fibrinopeptide A is released into the coronary circulation after coronary spasm. Circulation 1990, 82, 2222–2225. [Google Scholar] [CrossRef]
- Kaikita, K.; Ogawa, H.; Yasue, H.; Sakamoto, T.; Suefuji, H.; Sumida, H.; Okumura, K. Soluble P-selectin is released into the coronary circulation after coronary spasm. Circulation 1995, 92, 1726–1730. [Google Scholar] [CrossRef]
- Misumi, I.; Ogawa, H.; Masuda, T.; Sakamoto, T.; Okumura, K.; Yasue, H. Increased plasma plasminogen activator inhibitor activity after coronary spasm. Int. J. Cardiol. 1993, 41, 21–29. [Google Scholar] [CrossRef]
- Kobayashi, N.; Takano, M.; Hata, N.; Yamamoto, M.; Shinada, T.; Takahashi, Y.; Tomita, K.; Kitamura, M.; Mizuno, K. Optical coherence tomography findings in a case of acute coronary syndrome caused by coronary vasospasm. Int. Heart J. 2010, 51, 291–292. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bott-Silverman, C.; Heupler, F.A., Jr. Natural history of pure coronary artery spasm in patients treated medically. J. Am. Coll. Cardiol. 1983, 2, 200–205. [Google Scholar] [CrossRef]
- Girotti, A.L.; Rutitzky, B.; Schmidberg, J.; Crosatto, J.; Rosenbaum, M.B. Spontaneous remission in variant angina. Br. Heart J. 1981, 45, 517–521. [Google Scholar] [CrossRef]
- MacAlpin, R.N.; Kattus, A.A.; Alvaro, A.B. Angina pectoris at rest with preservation of exercise capacity: Prinzmetal’s variant angina. Circulation 1973, 47, 946–958. [Google Scholar] [CrossRef]
- Yasue, H.; Omote, S.; Takizawa, A.; Nagao, M.; Miwa, K.; Tanaka, S. Circadian variation of exercise capacity in patients with Prinzmetal’s variant angina: Role of exercise-induced coronary arterial spasm. Circulation 1979, 59, 938–948. [Google Scholar] [CrossRef]
- Watanabe, T.; Kim, S.; Akishita, M.; Kario, K.; Sekiguchi, H.; Fujikawa, H.; Mitsuhashi, T.; Ouchi, Y.; Shimada, K. Circadian variation of autonomic nervous activity in patients with multivessel coronary spasm. Jpn. Circ. J. 2001, 65, 593–598. [Google Scholar] [CrossRef]
- Yasue, H.; Horio, Y.; Nakamura, N.; Fujii, H.; Imoto, N.; Sonoda, R.; Kugiyama, K.; Obata, K.; Morikami, Y.; Kimura, T. Induction of coronary artery spasm by acetylcholine in patients with variant angina: Possible role of the parasympathetic nervous system in the pathogenesis of coronary artery spasm. Circulation 1986, 74, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Kounis, N.G.; Mazarakis, A.; Tsigkas, G.; Giannopoulos, S.; Goudevenos, J. Kounis syndrome: A new twist on an old disease. Future Cardiol. 2011, 7, 805–824. [Google Scholar] [CrossRef]
- Kounis, N.G. Coronary hypersensitivity disorder: The Kounis syndrome. Clin. Ther. 2013, 35, 563–571. [Google Scholar] [CrossRef]
- Takagi, S.; Goto, Y.; Hirose, E.; Terashima, M.; Sakuragi, S.; Suzuki, S.; Tsutsumi, Y.; Miyazaki, S.; Nonogi, H. Successful Treatment of Refractory Vasospastic Angina with Corticosteroids Coronary Arterial Hyperreactivity Caused by Local Inflammation? Circ. J. 2004, 68, 17–22. [Google Scholar] [CrossRef]
- Omri, M.; Kraiem, H.; Mejri, O.; Naija, M.; Chebili, N. Management of Kounis syndrome: Two case reports. J. Med. Case Rep. 2017, 11, 145. [Google Scholar] [CrossRef] [PubMed]
- Arslan, Z.; Iyisoy, A.; Tavlasoglu, M. Acute myocardial infarction after prednisolone administration for the treatment of anaphylaxis caused by a wasp sting: Online article-case report. Cardiovasc. J. Afr. 2013, 24, 4–6. [Google Scholar] [CrossRef]
- de Luna, A.B.; Cygankiewicz, I.; Baranchuk, A.; Fiol, M.; Birnbaum, Y.; Nikus, K.; Goldwasser, D.; Garcia-Niebla, J.; Sclarovsky, S.; Wellens, H.; et al. Prinzmetal Angina: ECG Changes and Clinical Considerations: A Consensus Paper. Ann. Noninvasive Electrocardiol. 2014, 19, 442–453. [Google Scholar] [CrossRef] [PubMed]
- Feldman, R.L.; Hill, J.A.; Whittle, J.L.; Conti, C.R.; Pepine, C.J. Electrocardiographic changes with coronary artery spasm. Am. Heart J. 1983, 106, 1288–1297. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Nishizaki, M.; Arita, M.; Ashikaga, T.; Yamawake, N.; Kakuta, T.; Numano, F.; Hiraoka, M. Increased QT dispersion in patients with vasospastic angina. Circulation 1998, 98, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Elbadawi, A.; Elgendy, I.Y.; Naqvi, S.Y.; Mohamed, A.H.; Ogunbayo, G.O.; Omer, M.A.; Mentias, A.; Saad, M.; Abbott, J.D.; Jneid, H.; et al. Temporal Trends and Outcomes of Hospitalizations with Prinzmetal Angina: Perspectives from a National Database. Am. J. Med. 2019, 132, 1053–1061.e1051. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Shinozaki, N.; Hirasawa, M.; Kato, R.; Shiraishi, K.; Kida, H.; Usuda, K.; Ishikawa, T. Prevalence of migraine and Raynaud’s phenomenon in Japanese patients with vasospastic angina. Jpn. Circ. J. 2000, 64, 239–242. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Beltrame, J.F.; Crea, F.; Kaski, J.C.; Ogawa, H.; Ong, P.; Sechtem, U.; Shimokawa, H.; Bairey Merz, C.N. International standardization of diagnostic criteria for vasospastic angina. Eur. Heart J. 2017, 38, 2565–2568. [Google Scholar] [CrossRef]
- Beltrame, J.F.; Crea, F.; Kaski, J.C.; Ogawa, H.; Ong, P.; Sechtem, U.; Shimokawa, H.; Bairey Merz, C.N. The Who, What, Why, When, How and Where of Vasospastic Angina. Circ. J. 2016, 80, 289–298. [Google Scholar] [CrossRef]
- Ford, T.J.; Ong, P.; Sechtem, U.; Beltrame, J.; Camici, P.G.; Crea, F.; Kaski, J.C.; Bairey Merz, C.N.; Pepine, C.J.; Shimokawa, H.; et al. Assessment of Vascular Dysfunction in Patients without Obstructive Coronary Artery Disease: Why, How, and When. JACC Cardiovasc. Interv. 2020, 13, 1847–1864. [Google Scholar] [CrossRef] [PubMed]
- Waters, D.D.; Szlachcic, J.; Bonan, R.; Miller, D.D.; Dauwe, F.; Theroux, P. Comparative sensitivity of exercise, cold pressor and ergonovine testing in provoking attacks of variant angina in patients with active disease. Circulation 1983, 67, 310–315. [Google Scholar] [CrossRef]
- Crea, F.; Chierchia, S.; Kaski, J.C.; Davies, G.J.; Margonato, A.; Miran, D.O.; Maseri, A. Provocation of coronary spasm by dopamine in patients with active variant angina pectoris. Circulation 1986, 74, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Okumura, K.; Yasue, H.; Horio, Y.; Takaoka, K.; Matsuyama, K.; Kugiyama, K.; Fujii, H.; Morikami, Y. Multivessel coronary spasm in patients with variant angina: A study with intracoronary injection of acetylcholine. Circulation 1988, 77, 535–542. [Google Scholar] [CrossRef]
- Clarke, J.G.; Davies, G.J.; Kerwin, R.; Hackett, D.; Larkin, S.; Dawbarn, D.; Lee, Y.; Bloom, S.R.; Yacoub, M.; Maseri, A. Coronary artery infusion of neuropeptide Y in patients with angina pectoris. Lancet 1987, 1, 1057–1059. [Google Scholar] [CrossRef]
- Hackett, D.; Larkin, S.; Chierchia, S.; Davies, G.; Kaski, J.C.; Maseri, A. Induction of coronary artery spasm by a direct local action of ergonovine. Circulation 1987, 75, 577–582. [Google Scholar] [CrossRef]
- Takagi, Y.; Yasuda, S.; Takahashi, J.; Tsunoda, R.; Ogata, Y.; Seki, A.; Sumiyoshi, T.; Matsui, M.; Goto, T.; Tanabe, Y.; et al. Clinical implications of provocation tests for coronary artery spasm: Safety, arrhythmic complications, and prognostic impact: Multicentre registry study of the Japanese Coronary Spasm Association. Eur. Heart J. 2013, 34, 258–267. [Google Scholar] [CrossRef]
- Ong, P.; Athanasiadis, A.; Borgulya, G.; Vokshi, I.; Bastiaenen, R.; Kubik, S.; Hill, S.; Schäufele, T.; Mahrholdt, H.; Kaski, J.C.; et al. Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation 2014, 129, 1723–1730. [Google Scholar] [CrossRef] [PubMed]
- Ludmer, P.L.; Selwyn, A.P.; Shook, T.L.; Wayne, R.R.; Mudge, G.H.; Alexander, R.W.; Ganz, P. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N. Engl. J. Med. 1986, 315, 1046–1051. [Google Scholar] [CrossRef]
- Chen, K.Y.; Rha, S.W.; Li, Y.J.; Poddar, K.L.; Jin, Z.; Minami, Y.; Saito, S.; Park, J.H.; Na, J.O.; Choi, C.U.; et al. Impact of hypertension on coronary artery spasm as assessed with intracoronary acetylcholine provocation test. J. Hum. Hypertens. 2010, 24, 77–85. [Google Scholar] [CrossRef]
- Ford, T.J.; Stanley, B.; Good, R.; Rocchiccioli, P.; McEntegart, M.; Watkins, S.; Eteiba, H.; Shaukat, A.; Lindsay, M.; Robertson, K.; et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina: The CorMicA Trial. J. Am. Coll. Cardiol. 2018, 72, 2841–2855. [Google Scholar] [CrossRef] [PubMed]
- Ong, P.; Athanasiadis, A.; Sechtem, U. Intracoronary Acetylcholine Provocation Testing for Assessment of Coronary Vasomotor Disorders. J. Vis. Exp. JoVE 2016, 114, e54295. [Google Scholar] [CrossRef] [PubMed]
- Pargaonkar, V.S.; Lee, J.H.; Chow, E.K.H.; Nishi, T.; Ball, R.L.; Kobayashi, Y.; Kimura, T.; Lee, D.P.; Stefanick, M.L.; Fearon, W.F.; et al. Dose-Response Relationship Between Intracoronary Acetylcholine and Minimal Lumen Diameter in Coronary Endothelial Function Testing of Women and Men with Angina and No Obstructive Coronary Artery Disease. Circ. Cardiovasc. Interv. 2020, 13, e008587. [Google Scholar] [CrossRef]
- Suyama, A.; Kuriyama, H. Mechanisms of the ergonovine-induced vasoconstriction in the rabbit main coronary artery. Naunyn-Schmiedebergs Arch. Pharm. 1984, 326, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Müller-Schweinitzer, E. The mechanism of ergometrine-induced coronary arterial spasm: In vitro studies on canine arteries. J. Cardiovasc. Pharm. 1980, 2, 645–655. [Google Scholar] [CrossRef]
- Egashira, S.; Mitsuoka, W.; Tagawa, H.; Kuga, T.; Tomoike, H.; Nakamura, M.; Takeshita, A. Mechanisms of ergonovine-induced hyperconstriction of coronary artery after X-ray irradiation in pigs. Basic Res. Cardiol. 1995, 90, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Harding, M.B.; Leithe, M.E.; Mark, D.B.; Nelson, C.L.; Harrison, J.K.; Hermiller, J.B.; Davidson, C.J.; Pryor, D.B.; Bashore, T.M. Ergonovine maleate testing during cardiac catheterization: A 10-year perspective in 3,447 patients without significant coronary artery disease or Prinzmetal’s variant angina. J. Am. Coll. Cardiol. 1992, 20, 107–111. [Google Scholar] [CrossRef][Green Version]
- Heupler, F.A., Jr.; Proudfit, W.L.; Razavi, M.; Shirey, E.K.; Greenstreet, R.; Sheldon, W.C. Ergonovine maleate provocative test for coronary arterial spasm. Am. J. Cardiol. 1978, 41, 631–640. [Google Scholar] [CrossRef]
- Kim, D.W.; Her, S.H.; Ahn, Y.; Shin, D.I.; Han, S.H.; Kim, D.S.; Choi, D.J.; Kwon, H.M.; Gwon, H.C.; Jo, S.H.; et al. Clinical outcome according to spasm type of single coronary artery provoked by intracoronary ergonovine tests in patients without significant organic stenosis. Int. J. Cardiol. 2018, 252, 6–12. [Google Scholar] [CrossRef]
- Ham, H.S.; Kim, K.H.; Park, J.; Song, Y.J.; Kim, S.; Kim, D.K.; Seol, S.H.; Kim, D.I. Feasibility of right coronary artery first ergonovine provocation test. Acta Cardiol. 2021, 76, 38–45. [Google Scholar] [CrossRef]
- Shin, D.I.; Baek, S.H.; Her, S.H.; Han, S.H.; Ahn, Y.; Park, K.H.; Kim, D.S.; Yang, T.H.; Choi, D.J.; Suh, J.W.; et al. The 24-Month Prognosis of Patients with Positive or Intermediate Results in the Intracoronary Ergonovine Provocation Test. JACC Cardiovasc. Interv. 2015, 8, 914–923. [Google Scholar] [CrossRef]
- Yun, K.H.; Shin, S.N.; Ko, J.S.; Rhee, S.J.; Kim, N.H.; Oh, S.K.; Jeong, J.W. Coronary artery responsiveness to ergonovine provocation in patients without vasospatic angina: A quantitative coronary angiography analysis. Int. Heart J. 2011, 52, 338–342. [Google Scholar] [CrossRef]
- Sueda, S.; Kohno, H.; Ochi, T.; Uraoka, T.; Tsunemitsu, K. Overview of the pharmacological spasm provocation test: Comparisons between acetylcholine and ergonovine. J. Cardiol. 2017, 69, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Song, J.K.; Park, S.W.; Kang, D.H.; Hong, M.K.; Kim, J.J.; Lee, C.W.; Park, S.J. Safety and clinical impact of ergonovine stress echocardiography for diagnosis of coronary vasospasm. J. Am. Coll. Cardiol. 2000, 35, 1850–1856. [Google Scholar] [CrossRef]
- Om, S.Y.; Yoo, S.Y.; Cho, G.Y.; Kim, M.; Woo, Y.; Lee, S.; Kim, D.H.; Song, J.M.; Kang, D.H.; Cheong, S.S.; et al. Diagnostic and Prognostic Value of Ergonovine Echocardiography for Noninvasive Diagnosis of Coronary Vasospasm. JACC Cardiovasc. Imaging 2020, 13, 1875–1887. [Google Scholar] [CrossRef] [PubMed]
- Tsujita, K.; Sakamoto, K.; Kojima, S.; Kojima, S.; Takaoka, N.; Nagayoshi, Y.; Sakamoto, T.; Tayama, S.; Kaikita, K.; Hokimoto, S.; et al. Coronary plaque component in patients with vasospastic angina: A virtual histology intravascular ultrasound study. Int. J. Cardiol. 2013, 168, 2411–2415. [Google Scholar] [CrossRef]
- Miyao, Y.; Kugiyama, K.; Kawano, H.; Motoyama, T.; Ogawa, H.; Yoshimura, M.; Sakamoto, T.; Yasue, H. Diffuse intimal thickening of coronary arteries in patients with coronary spastic angina. J. Am. Coll. Cardiol. 2000, 36, 432–437. [Google Scholar] [CrossRef]
- Young Joon, H.; Myung Ho, J.; Yun Ha, C.; Eun Hye, M.; Jum Suk, K.; Min Goo, L.; Keun Ho, P.; Doo Sun, S.; Nam Sik, Y.; Hyun Ju, Y.; et al. Plaque components at coronary sites with focal spasm in patients with variant angina: Virtual histology-intravascular ultrasound analysis. Int. J. Cardiol. 2010, 144, 367–372. [Google Scholar] [CrossRef]
- Shin, E.S.; Ann, S.H.; Singh, G.B.; Lim, K.H.; Yoon, H.J.; Hur, S.H.; Her, A.Y.; Koo, B.K.; Akasaka, T. OCT-Defined Morphological Characteristics of Coronary Artery Spasm Sites in Vasospastic Angina. JACC Cardiovasc. Imaging 2015, 8, 1059–1067. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Shimada, K.; Tearney, G.J.; Kitabata, H.; Taguchi, H.; Fukuda, S.; Kashiwagi, M.; Kubo, T.; Takarada, S.; Hirata, K.; et al. Conformational change in coronary artery structure assessed by optical coherence tomography in patients with vasospastic angina. J. Am. Coll. Cardiol. 2011, 58, 1608–1613. [Google Scholar] [CrossRef]
- Itoh, T.; Mizuno, Y.; Harada, E.; Yoshimura, M.; Ogawa, H.; Yasue, H. Coronary spasm is associated with chronic low-grade inflammation. Circ. J. 2007, 71, 1074–1078. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, Y.; Harada, E.; Morita, S.; Kinoshita, K.; Hayashida, M.; Shono, M.; Morikawa, Y.; Murohara, T.; Nakayama, M.; Yoshimura, M.; et al. East asian variant of aldehyde dehydrogenase 2 is associated with coronary spastic angina: Possible roles of reactive aldehydes and implications of alcohol flushing syndrome. Circulation 2015, 131, 1665–1673. [Google Scholar] [CrossRef] [PubMed]
- Raizner, A.E.; Chahine, R.A.; Ishimori, T.; Verani, M.S.; Zacca, N.; Jamal, N.; Miller, R.R.; Luchi, R.J. Provocation of coronary artery spasm by the cold pressor test. Hemodynamic, arteriographic and quantitative angiographic observations. Circulation 1980, 62, 925–932. [Google Scholar] [CrossRef]
- Yeung, A.C.; Vekshtein, V.I.; Krantz, D.S.; Vita, J.A.; Ryan, T.J.; Ganz, P.; Selwyn, A.P. The Effect of Atherosclerosis on the Vasomotor Response of Coronary Arteries to Mental Stress. N. Engl. J. Med. 1991, 325, 1551–1556. [Google Scholar] [CrossRef] [PubMed]
- Nakao, K.; Ohgushi, M.; Yoshimura, M.; Morooka, K.; Okumura, K.; Ogawa, H.; Kugiyama, K.; Oike, Y.; Fujimoto, K.; Yasue, H. Hyperventilation as a specific test for diagnosis of coronary artery spasm. Am. J. Cardiol. 1997, 80, 545–549. [Google Scholar] [CrossRef]
- Harris, J.R.; Hale, G.M.; Dasari, T.W.; Schwier, N.C. Pharmacotherapy of Vasospastic Angina. J. Cardiovasc. Pharm. Ther. 2016, 21, 439–451. [Google Scholar] [CrossRef]
- Chahine, R.A.; Feldman, R.L.; Giles, T.D.; Nicod, P.; Raizner, A.E.; Weiss, R.J.; Vanov, S.K. Randomized placebo-controlled trial of amlodipine in vasospastic angina. Amlodipine Study 160 Group. J. Am. Coll. Cardiol. 1993, 21, 1365–1370. [Google Scholar] [CrossRef]
- Brozovich, F.V.; Nicholson, C.J.; Degen, C.V.; Gao, Y.Z.; Aggarwal, M.; Morgan, K.G. Mechanisms of Vascular Smooth Muscle Contraction and the Basis for Pharmacologic Treatment of Smooth Muscle Disorders. Pharm. Rev. 2016, 68, 476–532. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.J.; Hu, P.; Hung, M.Y. Coronary artery spasm: Review and update. Int. J. Med. Sci. 2014, 11, 1161–1171. [Google Scholar] [CrossRef]
- Rodríguez-Mañero, M.; Oloriz, T.; le Polain de Waroux, J.B.; Burri, H.; Kreidieh, B.; de Asmundis, C.; Arias, M.A.; Arbelo, E.; Díaz Fernández, B.; Fernández-Armenta, J.; et al. Long-term prognosis of patients with life-threatening ventricular arrhythmias induced by coronary artery spasm. Europace 2018, 20, 851–858. [Google Scholar] [CrossRef]
- Takahashi, J.; Nihei, T.; Takagi, Y.; Miyata, S.; Odaka, Y.; Tsunoda, R.; Seki, A.; Sumiyoshi, T.; Matsui, M.; Goto, T.; et al. Prognostic impact of chronic nitrate therapy in patients with vasospastic angina: Multicentre registry study of the Japanese coronary spasm association. Eur. Heart J. 2015, 36, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Daiber, A.; Münzel, T. Organic Nitrate Therapy, Nitrate Tolerance, and Nitrate-Induced Endothelial Dysfunction: Emphasis on Redox Biology and Oxidative Stress. Antioxid. Redox Signal. 2015, 23, 899–942. [Google Scholar] [CrossRef] [PubMed]
- Svendsen, T.L. Central Hemodynamics of β-Adrenoceptor Blocking Drugs. J. Cardiovasc. Pharm. 1983, 5, S21–S25. [Google Scholar] [CrossRef]
- Howlett, J.G. Nebivolol: Vasodilator Properties and Evidence for Relevance in Treatment of Cardiovascular Disease. Can. J. Cardiol. 2014, 30, S29–S37. [Google Scholar] [CrossRef][Green Version]
- Yasue, H.; Mizuno, Y.; Harada, E.; Itoh, T.; Nakagawa, H.; Nakayama, M.; Ogawa, H.; Tayama, S.; Honda, T.; Hokimoto, S.; et al. Effects of a 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, fluvastatin, on coronary spasm after withdrawal of calcium-channel blockers. J. Am. Coll. Cardiol. 2008, 51, 1742–1748. [Google Scholar] [CrossRef]
- Sauzeau, V.; Rolli-Derkinderen, M.; Marionneau, C.; Loirand, G.; Pacaud, P. RhoA expression is controlled by nitric oxide through cGMP-dependent protein kinase activation. J. Biol. Chem. 2003, 278, 9472–9480. [Google Scholar] [CrossRef]
- Rikitake, Y.; Liao, J.K. Rho GTPases, statins, and nitric oxide. Circ. Res. 2005, 97, 1232–1235. [Google Scholar] [CrossRef]
- Masumoto, A.; Mohri, M.; Shimokawa, H.; Urakami, L.; Usui, M.; Takeshita, A. Suppression of coronary artery spasm by the Rho-kinase inhibitor fasudil in patients with vasospastic angina. Circulation 2002, 105, 1545–1547. [Google Scholar] [CrossRef]
- Shimokawa, H.; Sunamura, S.; Satoh, K. RhoA/Rho-Kinase in the Cardiovascular System. Circ. Res. 2016, 118, 352–366. [Google Scholar] [CrossRef]
- Nihei, T.; Takahashi, J.; Hao, K.; Kikuchi, Y.; Odaka, Y.; Tsuburaya, R.; Nishimiya, K.; Matsumoto, Y.; Ito, K.; Miyata, S.; et al. Prognostic impacts of Rho-kinase activity in circulating leucocytes in patients with vasospastic angina. Eur. Heart J. 2018, 39, 952–959. [Google Scholar] [CrossRef]
- Mohri, M.; Shimokawa, H.; Hirakawa, Y.; Masumoto, A.; Takeshita, A. Rho-kinase inhibition with intracoronary fasudil prevents myocardial ischemia in patients with coronary microvascular spasm. J. Am. Coll. Cardiol. 2003, 41, 15–19. [Google Scholar] [CrossRef]
- Stone, W.M.; Demaerschalk, B.M.; Fowl, R.J.; Money, S.R. Type 3 phosphodiesterase inhibitors may be protective against cerebrovascular events in patients with claudication. J. Stroke Cerebrovasc. Dis. 2008, 17, 129–133. [Google Scholar] [CrossRef]
- Watanabe, K.; Ikeda, S.; Komatsu, J.; Inaba, S.; Suzuki, J.; Sueda, S.; Funada, J.; Kitakaze, M.; Sekiya, M. Effect of cilostazol on vasomotor reactivity in patients with vasospastic angina pectoris. Am. J. Cardiol. 2003, 92, 21–25. [Google Scholar] [CrossRef]
- Shin, E.S.; Lee, J.H.; Yoo, S.Y.; Park, Y.; Hong, Y.J.; Kim, M.H.; Lee, J.Y.; Nam, C.W.; Tahk, S.J.; Kim, J.S.; et al. A randomised, multicentre, double blind, placebo controlled trial to evaluate the efficacy and safety of cilostazol in patients with vasospastic angina. Heart 2014, 100, 1531–1536. [Google Scholar] [CrossRef] [PubMed]
- Kaski, J.C. Management of vasospastic angina--role of nicorandil. Cardiovasc. Drugs Ther. 1995, 9 (Suppl. S2), 221–227. [Google Scholar] [CrossRef]
- Omae, T.; Nagaoka, T.; Tanano, I.; Yoshida, A. Pioglitazone, a peroxisome proliferator-activated receptor-γ agonist, induces dilation of isolated porcine retinal arterioles: Role of nitric oxide and potassium channels. Investig. Ophthalmol. Vis. Sci. 2011, 52, 6749–6756. [Google Scholar] [CrossRef]
- Motoyama, T.; Kawano, H.; Kugiyama, K.; Hirashima, O.; Ohgushi, M.; Tsunoda, R.; Moriyama, Y.; Miyao, Y.; Yoshimura, M.; Ogawa, H.; et al. Vitamin E administration improves impairment of endothelium-dependent vasodilation in patients with coronary spastic angina. J. Am. Coll. Cardiol. 1998, 32, 1672–1679. [Google Scholar] [CrossRef]
- Kugiyama, K.; Motoyama, T.; Hirashima, O.; Ohgushi, M.; Soejima, H.; Misumi, K.; Kawano, H.; Miyao, Y.; Yoshimura, M.; Ogawa, H.; et al. Vitamin C attenuates abnormal vasomotor reactivity in spasm coronary arteries in patients with coronary spastic angina. J. Am. Coll. Cardiol. 1998, 32, 103–109. [Google Scholar] [CrossRef][Green Version]
- Gaspardone, A.; Tomai, F.; Versaci, F.; Ghini, A.S.; Polisca, P.; Crea, F.; Chiariello, L.; Gioffrè, P.A. Coronary artery stent placement in patients with variant angina refractory to medical treatment. Am. J. Cardiol. 1999, 84, 96–98, a98. [Google Scholar] [CrossRef]
- Nakamura, T.; Furukawa, K.; Uchiyama, H.; Seo, Y.; Okuda, S.; Ebizawa, T. Stent placement for recurrent vasospastic angina resistant to medical treatment. Catheter. Cardiovasc. Diagn. 1997, 42, 440–443. [Google Scholar] [CrossRef]
- Fischell, T.A.; Derby, G.; Tse, T.M.; Stadius, M.L. Coronary artery vasoconstriction routinely occurs after percutaneous transluminal coronary angioplasty. A quantitative arteriographic analysis. Circulation 1988, 78, 1323–1334. [Google Scholar] [CrossRef] [PubMed]
- Cardona-Guarache, R.; Pozen, J.; Jahangiri, A.; Koneru, J.; Shepard, R.; Roberts, C.; Abbate, A.; Cassano, A. Thoracic Sympathectomy for Severe Refractory Multivessel Coronary Artery Spasm. Am. J. Cardiol. 2016, 117, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Meisel, S.R.; Mazur, A.; Chetboun, I.; Epshtein, M.; Canetti, M.; Gallimidi, J.; Katz, A.; Strasberg, B.; Peled, B. Usefulness of implantable cardioverter-defibrillators in refractory variant angina pectoris complicated by ventricular fibrillation in patients with angiographically normal coronary arteries. Am. J. Cardiol. 2002, 89, 1114–1116. [Google Scholar] [CrossRef]
- Chevalier, P.; Dacosta, A.; Defaye, P.; Chalvidan, T.; Bonnefoy, E.; Kirkorian, G.; Isaaz, K.; Denis, B.; Touboul, P. Arrhythmic Cardiac Arrest Due to Isolated Coronary Artery Spasm: Long-Term Outcome of Seven Resuscitated Patients. J. Am. Coll. Cardiol. 1998, 31, 57–61. [Google Scholar] [CrossRef]
- Ahn, J.M.; Lee, K.H.; Yoo, S.Y.; Cho, Y.R.; Suh, J.; Shin, E.S.; Lee, J.H.; Shin, D.I.; Kim, S.H.; Baek, S.H.; et al. Prognosis of Variant Angina Manifesting as Aborted Sudden Cardiac Death. J. Am. Coll. Cardiol. 2016, 68, 137–145. [Google Scholar] [CrossRef]
- Yasue, H.; Takizawa, A.; Nagao, M.; Nishida, S.; Horie, M.; Kubota, J.; Omote, S.; Takaoka, K.; Okumura, K. Long-term prognosis for patients with variant angina and influential factors. Circulation 1988, 78, 1–9. [Google Scholar] [CrossRef]
- Waters, D.D.; Miller, D.D.; Szlachcic, J.; Bouchard, A.; Méthé, M.; Kreeft, J.; Théroux, P. Factors influencing the long-term prognosis of treated patients with variant angina. Circulation 1983, 68, 258–265. [Google Scholar] [CrossRef]
- Kawana, A.; Takahashi, J.; Takagi, Y.; Yasuda, S.; Sakata, Y.; Tsunoda, R.; Ogata, Y.; Seki, A.; Sumiyoshi, T.; Matsui, M.; et al. Gender Differences in the Clinical Characteristics and Outcomes of Patients with Vasospastic Angina—A Report from the Japanese Coronary Spasm Association. Circ. J. 2013, 77, 1267–1274. [Google Scholar] [CrossRef]
- Rodriguez Ziccardi, M.; Hatcher, J.D. Prinzmetal Angina. In StatPearls; StatPearls Publishing Copyright©2022; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2022. [Google Scholar]
- MacAlpin, R.N. Cardiac arrest and sudden unexpected death in variant angina: Complications of coronary spasm that can occur in the absence of severe organic coronary stenosis. Am. Heart J. 1993, 125, 1011–1017. [Google Scholar] [CrossRef]
- Togashi, I.; Sato, T.; Soejima, K.; Takatsuki, S.; Miyoshi, S.; Fukumoto, K.; Nishiyama, N.; Suzuki, M.; Hori, S.; Ogawa, S.; et al. Sudden cardiac arrest and syncope triggered by coronary spasm. Int. J. Cardiol. 2013, 163, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.H.; Kuo, L.T.; Hung, M.J.; Cherng, W.J. Coronary vasospasm as a possible cause of elevated cardiac troponin I in patients with acute coronary syndrome and insignificant coronary artery disease. Am. Heart J. 2002, 144, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Takagi, Y.; Yasuda, S.; Tsunoda, R.; Ogata, Y.; Seki, A.; Sumiyoshi, T.; Matsui, M.; Goto, T.; Tanabe, Y.; Sueda, S.; et al. Clinical Characteristics and Long-Term Prognosis of Vasospastic Angina Patients Who Survived Out-of-Hospital Cardiac Arrest. Circ. Arrhythmia Electrophysiol. 2011, 4, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Takagi, Y.; Takahashi, J.; Yasuda, S.; Miyata, S.; Tsunoda, R.; Ogata, Y.; Seki, A.; Sumiyoshi, T.; Matsui, M.; Goto, T.; et al. Prognostic stratification of patients with vasospastic angina: A comprehensive clinical risk score developed by the Japanese Coronary Spasm Association. J. Am. Coll. Cardiol. 2013, 62, 1144–1153. [Google Scholar] [CrossRef] [PubMed]
| Physiological | Pharmacological |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| COVADIS Group | Japanese Circulation Society |
|---|---|
Class I
| Class I
|
Class IIa
| Class IIa
|
Class IIb
| Class IIb
|
Class III
| Class III
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rehan, R.; Weaver, J.; Yong, A. Coronary Vasospastic Angina: A Review of the Pathogenesis, Diagnosis, and Management. Life 2022, 12, 1124. https://doi.org/10.3390/life12081124
Rehan R, Weaver J, Yong A. Coronary Vasospastic Angina: A Review of the Pathogenesis, Diagnosis, and Management. Life. 2022; 12(8):1124. https://doi.org/10.3390/life12081124
Chicago/Turabian StyleRehan, Rajan, James Weaver, and Andy Yong. 2022. "Coronary Vasospastic Angina: A Review of the Pathogenesis, Diagnosis, and Management" Life 12, no. 8: 1124. https://doi.org/10.3390/life12081124
APA StyleRehan, R., Weaver, J., & Yong, A. (2022). Coronary Vasospastic Angina: A Review of the Pathogenesis, Diagnosis, and Management. Life, 12(8), 1124. https://doi.org/10.3390/life12081124





