Evaluation of Cortical Bone Formation on Mandibular Condyle in Asymptomatic Adolescents and Young Adults Using Cone-Beam Computed Tomography
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
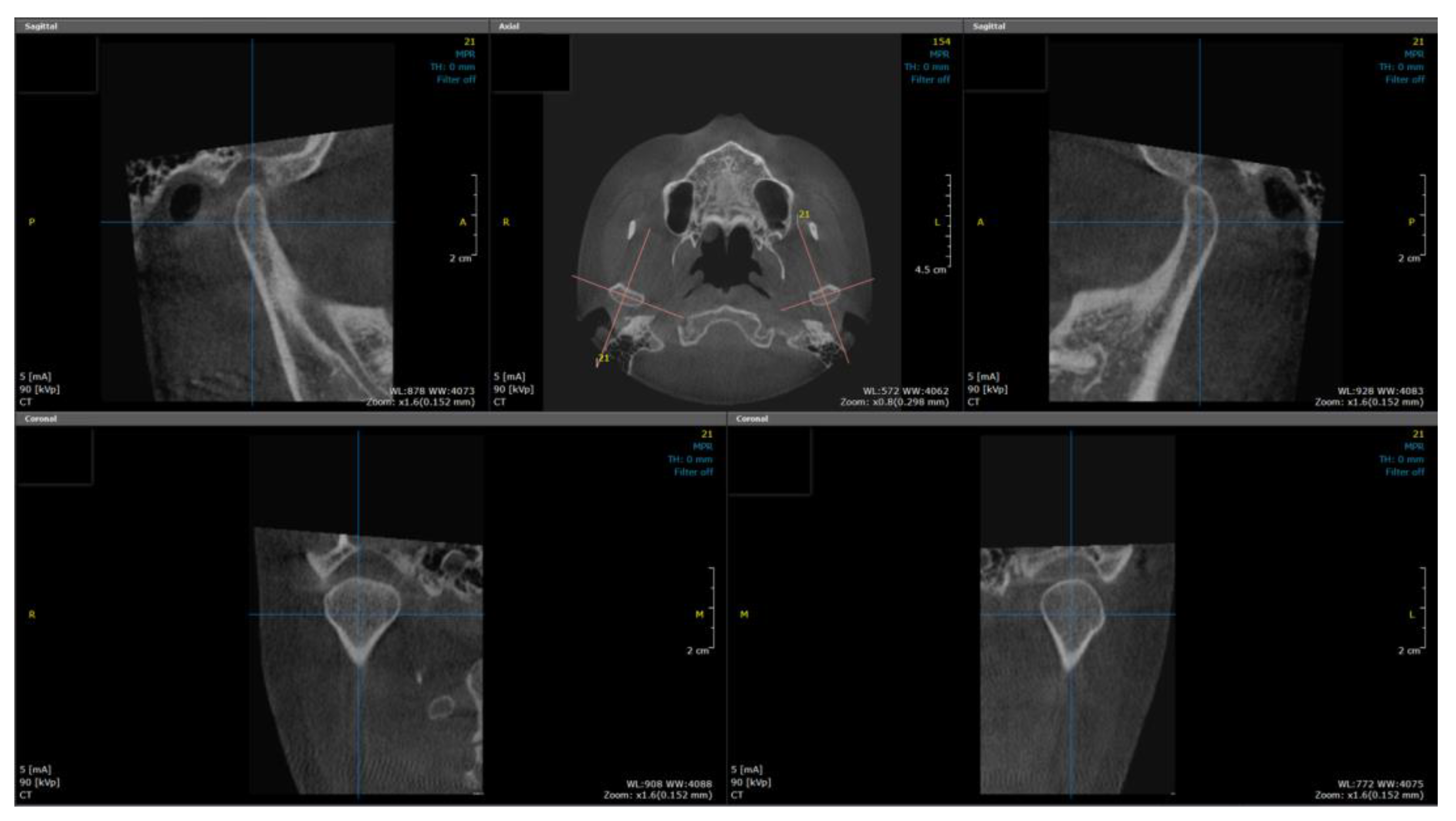
2.2. Image Reconstruction
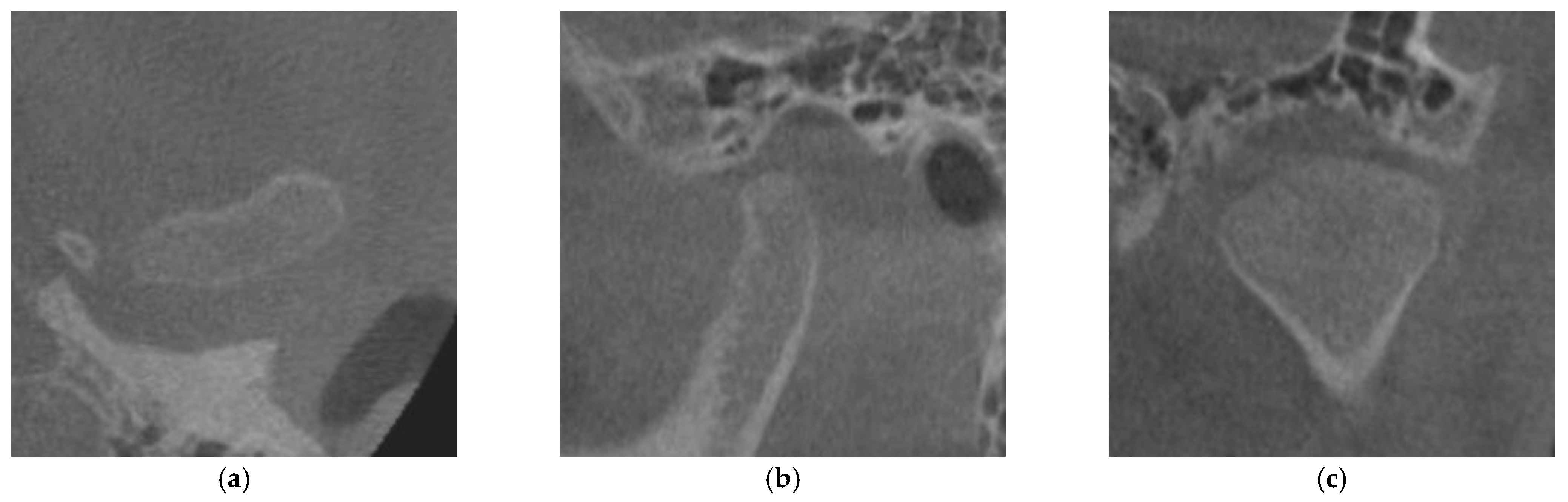
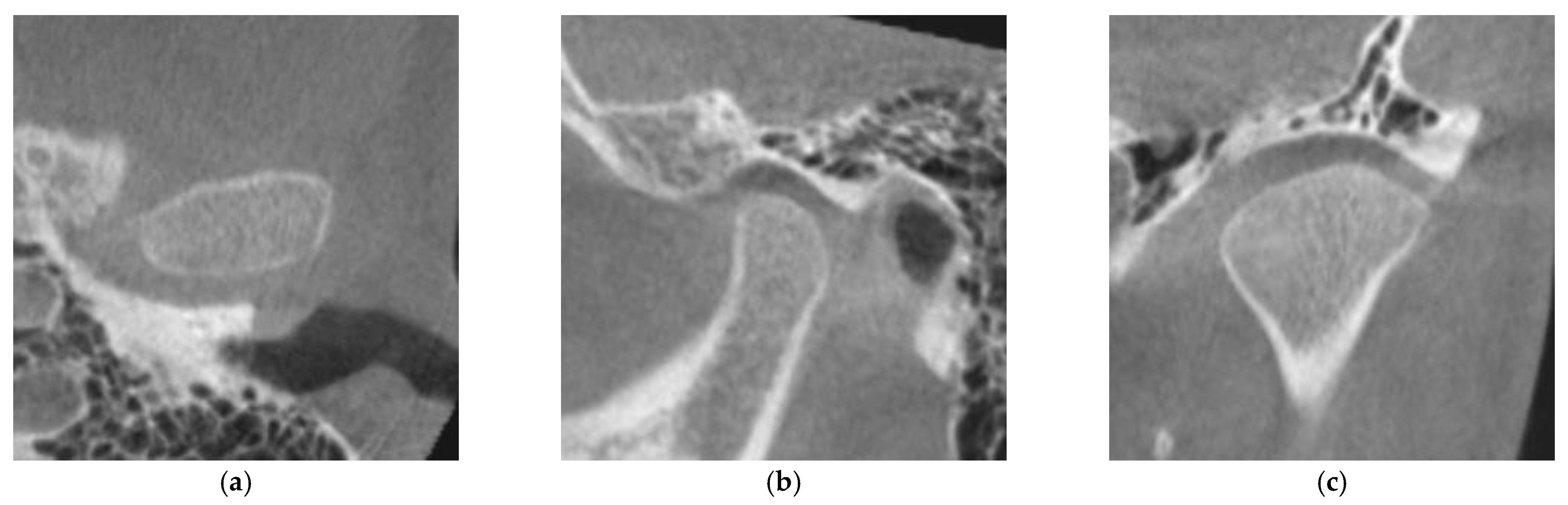
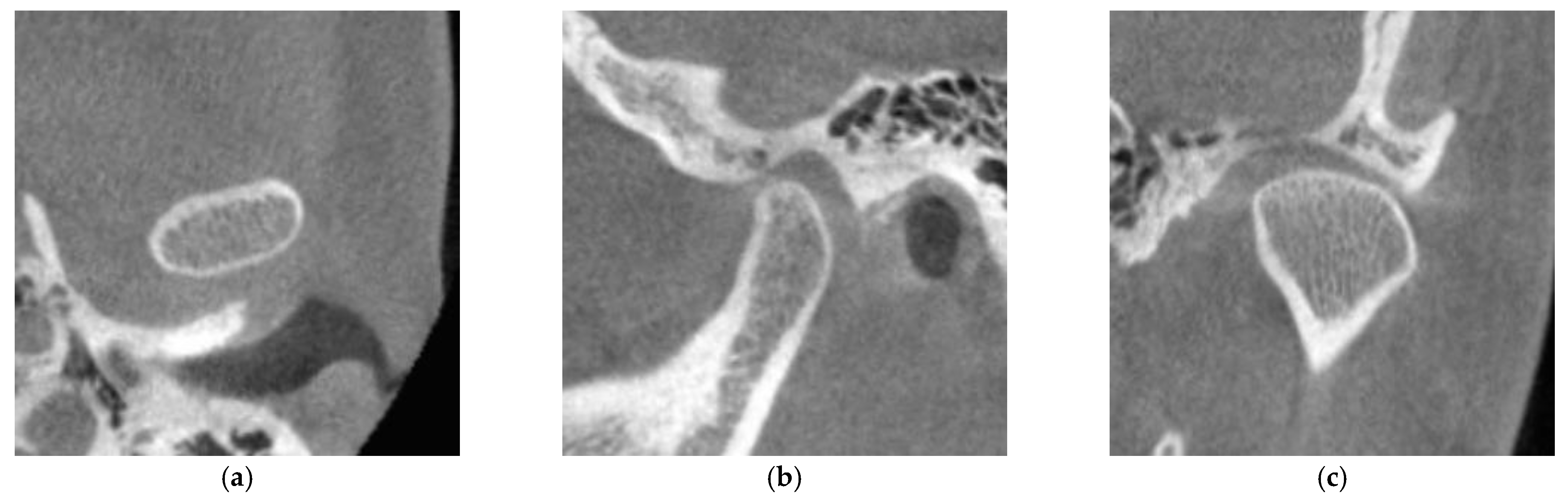
2.3. Evaluation of Cortical Bone Formation on the Mandibular Condyle
2.4. Statistical Analysis
3. Results
3.1. Inter-Examiner/Intra-Examiner Reliability
3.2. Frequency Distribution of the Degree of CMC according to Age and Sex
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Christidis, N.; Lindström Ndanshau, E.; Sandberg, A.; Tsilingaridis, G. Prevalence and treatment strategies regarding temporomandibular disorders in children and adolescents-A systematic review. J. Oral. Rehabil. 2019, 46, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Yang, Y.; Dutra, E.H.; Robinson, J.L.; Wadhwa, S. Temporomandibular Joint Disorders in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 1213–1217. [Google Scholar] [CrossRef] [PubMed]
- Okeson, J.P. Temporomandibular Joint Pains. In Bell’s Oral and Facial Pain, 7th ed.; Okeson, J.P., Ed.; Quintessence Publishing: Chicago, IL, USA, 2014; pp. 523–524. [Google Scholar]
- Howard, J.A. Temporomandibular joint disorders in children. Dent. Clin. North Am. 2013, 57, 99–127. [Google Scholar] [CrossRef]
- Bender, M.E.; Lipin, R.B.; Goudy, S.L. Development of the Pediatric Temporomandibular Joint. Oral. Maxillofac. Surg. Clin. North Am. 2018, 30, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Stocum, D.L.; Roberts, W.E. Part I: Development and Physiology of the Temporomandibular Joint. Curr. Osteoporos. Rep. 2018, 16, 360–368. [Google Scholar] [CrossRef]
- Genden, E.M.; Buchbinder, D.; Chaplin, J.M.; Lueg, E.; Funk, G.F.; Urken, M.L. Reconstruction of the pediatric maxilla and mandible. Arch. Otolaryngol. Head Neck Surg. 2000, 126, 293–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chouinard, A.F.; Kaban, L.B.; Peacock, Z.S. Acquired Abnormalities of the Temporomandibular Joint. Oral. Maxillofac. Surg. Clin. North Am. 2018, 30, 83–96. [Google Scholar] [CrossRef]
- Granquist, E.J. Treatment of the Temporomandibular Joint in a Child with Juvenile Idiopathic Arthritis. Oral. Maxillofac. Surg. Clin. North Am. 2018, 30, 97–107. [Google Scholar] [CrossRef]
- Rahimi, H.; Twilt, M.; Herlin, T.; Spiegel, L.; Pedersen, T.K.; Küseler, A.; Stoustrup, P. Orofacial symptoms and oral health-related quality of life in juvenile idiopathic arthritis: A two-year prospective observational study. Pediatr. Rheumatol. Online J. 2018, 16, 47. [Google Scholar] [CrossRef] [Green Version]
- Hammer, M.R.; Kanaan, Y. Imaging of the Pediatric Temporomandibular Joint. Oral. Maxillofac. Surg. Clin. North Am. 2018, 30, 25–34. [Google Scholar] [CrossRef]
- Gumussoy, I.; Duman, S.B. Alternative cone-beam CT method for the analysis of mandibular condylar bone in patients with degenerative joint disease. Oral. Radiol. 2020, 36, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Yap, A.U.; Liu, M.Q.; Fu, K.Y. Condylar repair and regeneration in adolescents/young adults with early-stage degenerative temporomandibular joint disease: A randomised controlled study. J. Oral. Rehabil. 2019, 46, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Sethna Muthlakshmi, K.S.; Krithika, C.L.; Asokan, K. Evaluation and Correlation of Condylar Cortication by Cone-Beam Computed Tomography: A Retrospective Study. Contemp. Clin. Dent. 2022, 13, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Liu, M.Q.; Yap, A.U.; Fu, K.Y. Condylar subchondral formation of cortical bone in adolescents and young adults. Br. J. Oral. Maxillofac. Surg. 2013, 51, 63–68. [Google Scholar] [CrossRef]
- Kim, K.Y. Statistical methods for accessing agreement between repeated measurements in dental research. J. Korean Dent. Assoc. 2016, 54, 880–896. [Google Scholar]
- Roberts, W.E.; Goodacre, C.J. The Temporomandibular Joint: A Critical Review of Life-Support Functions, Development, Articular Surfaces, Biomechanics and Degeneration. J. Prosthodont. 2020, 29, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.M.; Chai, J.W.; Wu, F.Y.; Chen, M.H.; Kao, C.T. Differences between the temporal and mandibular components of the temporomandibular joint in topographic distribution of osseous degenerative features on cone-beam computerized tomography. J. Dent. Sci. 2021, 16, 1010–1017. [Google Scholar] [CrossRef]
- Liu, Y.Y.; Wang, H.; Yang, Z.Y.; Ba, K.; Li, M.X.; Liu, L. The correlation between temporomandibular joint maturity and second molar root development in adolescents. Int. J. Stomatol. 2010, 37, 154–156. [Google Scholar]
- Morimoto, Y.; Konoo, T.; Tominaga, K.; Tanaka, T.; Yamaguchi, K.; Fukuda, J.; Ohba, T. Relationship between cortical bone formation on mandibular condyles and alternation of the magnetic resonance signals characteristic of growth. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 473–480. [Google Scholar] [CrossRef]
- Yalcin, E.D.; Bozan, C. Relationship between mandibular condyle and articular eminence cortication with mandibular cortical index on cone-beam CT. Surg. Radiol. Anat. 2020, 42, 515–522. [Google Scholar] [CrossRef]
- Larheim, T.A.; Abrahamsson, A.K.; Kristensen, M.; Arvidsson, L.Z. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac. Radiol. 2015, 44, 20140235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayrak, S.; Göller, B.D. Relationship between condyle cortication, sphenooccipital synchondrosis, and chronological age. Oral. Radiol. 2020, 36, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Yang, I.H.; Hyun, H.K.; Lee, J.Y. Dental and skeletal maturation in female adolescents with temporomandibular joint osteoarthritis. J. Oral. Rehabil. 2017, 44, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Smartt, J.M., Jr.; Low, D.W.; Bartlett, S.P. The pediatric mandible: I. A primer on growth and development. Plast. Reconstr. Surg. 2005, 116, 14e–23e. [Google Scholar] [CrossRef]
- Bayrak, S.; Halıcıoglu, S.; Kose, G.; Halıcıoglu, K. Evaluation of the relationship between mandibular condyle cortication and chronologic age with cone beam computed tomography. J. Forensic. Leg. Med. 2018, 55, 39–44. [Google Scholar] [CrossRef]
| Men | Women | Chi-Square Test | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age (n) | CMC 0 | CMC 1 | CMC 2 | Age (n) | CMC 0 | CMC 1 | CMC 2 | p-Value | χ2, df |
| 13 (56) | 45 (80.4) | 11 (19.6) | 0 (0) | 13 (66) | 38 (65.5) | 20 (34.5) | 0 (0) | 0.075 | 3.17, 1 |
| 14 (66) | 51 (77.3) | 15 (22.7) | 0 (0) | 14 (66) | 41 (62.1) | 23 (34.8) | 2 (3.0) | 0.761 | 0.09, 1 |
| 15 (64) | 48 (75.0) | 16 (25.0) | 0 (0) | 15 (64) | 35 (54.7) | 27 (42.2) | 2 (3.1) | 0.033 * | 6.85, 2 |
| 16 (62) | 36 (58.1) | 26 (41.9) | 0 (0) | 16 (64) | 24 (37.5) | 36 (56.3) | 4 (6.3) | 0.018 * | 7.98, 2 |
| 17 (66) | 34 (51.5) | 30 (45.5) | 2 (3.0) | 17 (64) | 18 (28.1) | 37 (57.8) | 9 (14.1) | 0.006 * | 10.08, 2 |
| 18 (66) | 32 (48.5) | 31 (47.0) | 3 (4.5) | 18 (64) | 6 (9.4) | 46 (71.9) | 12 (18.8) | 0.000 * | 26.09, 2 |
| 19 (66) | 7 (10.6) | 50 (75.8) | 9 (13.6) | 19 (64) | 1 (1.6) | 43 (67.2) | 20 (31.3) | 0.010 * | 9.17, 2 |
| 20 (62) | 2 (3.2) | 47 (75.8) | 13 (21.0) | 20 (62) | 0 (0) | 42 (67.7) | 20 (32.3) | 0.152 | 3.77, 2 |
| 21 (64) | 0 (0) | 41 (64.1) | 23 (35.9) | 21 (64) | 0 (0) | 31 (48.4) | 33 (51.6) | 0.075 | 3.18, 1 |
| 22 (66) | 0 (0) | 35 (53.0) | 31 (47.0) | 22 (63) | 0 (0) | 17 (27.0) | 46 (73.0) | 0.003 * | 9.09, 1 |
| 23 (66) | 0 (0) | 23 (34.8) | 43 (65.2) | 23 (63) | 0 (0) | 15 (23.8) | 48 (76.2) | 0.169 | 1.89, 1 |
| 24 (66) | 0 (0) | 15 (24.2) | 48 (75.8) | 24 (64) | 0 (0) | 16 (25.0) | 48 (75.0) | 0.916 | 0.01, 1 |
| 25 (60) | 0 (0) | 13 (21.7) | 47 (78.3) | 25 (66) | 0 (0) | 16 (24.2) | 50 (75.8) | 0.732 | 0.12, 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, Y.-S.; Park, H.-J.; Yu, S.-K.; Jeong, S.-R.; Ryu, J.-W. Evaluation of Cortical Bone Formation on Mandibular Condyle in Asymptomatic Adolescents and Young Adults Using Cone-Beam Computed Tomography. Life 2022, 12, 2032. https://doi.org/10.3390/life12122032
Seo Y-S, Park H-J, Yu S-K, Jeong S-R, Ryu J-W. Evaluation of Cortical Bone Formation on Mandibular Condyle in Asymptomatic Adolescents and Young Adults Using Cone-Beam Computed Tomography. Life. 2022; 12(12):2032. https://doi.org/10.3390/life12122032
Chicago/Turabian StyleSeo, Yo-Seob, Hyun-Jeong Park, Sun-Kyoung Yu, Seo-Rin Jeong, and Ji-Won Ryu. 2022. "Evaluation of Cortical Bone Formation on Mandibular Condyle in Asymptomatic Adolescents and Young Adults Using Cone-Beam Computed Tomography" Life 12, no. 12: 2032. https://doi.org/10.3390/life12122032
APA StyleSeo, Y.-S., Park, H.-J., Yu, S.-K., Jeong, S.-R., & Ryu, J.-W. (2022). Evaluation of Cortical Bone Formation on Mandibular Condyle in Asymptomatic Adolescents and Young Adults Using Cone-Beam Computed Tomography. Life, 12(12), 2032. https://doi.org/10.3390/life12122032





