Does Surgical Repair Benefit Pipkin Type I Femoral Head Fractures?: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Registration and Guidelines
2.2. Literature Search
2.3. Independent Review Process
2.4. Study Selection and Eligibility
2.5. Data Extraction
2.6. Assessment of Methodological Quality and Risk of Bias
2.7. Outcome Measures, Data Synthesis, and Statistical Analysis
3. Results
3.1. Study Selection, Quality Assessment, and Study Characteristics
3.2. Patient Demographics and Procedures
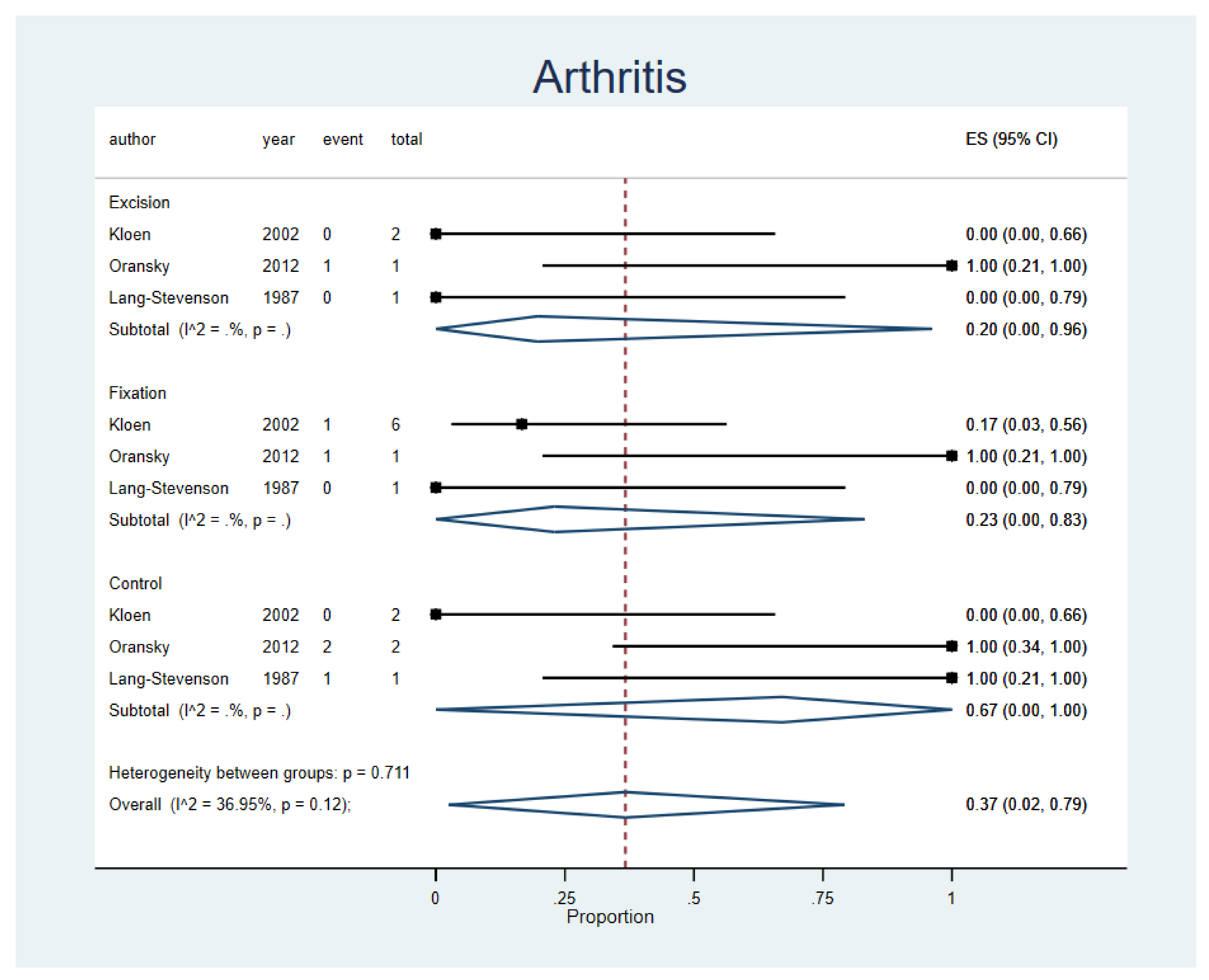
3.3. Post-Traumatic Arthritis
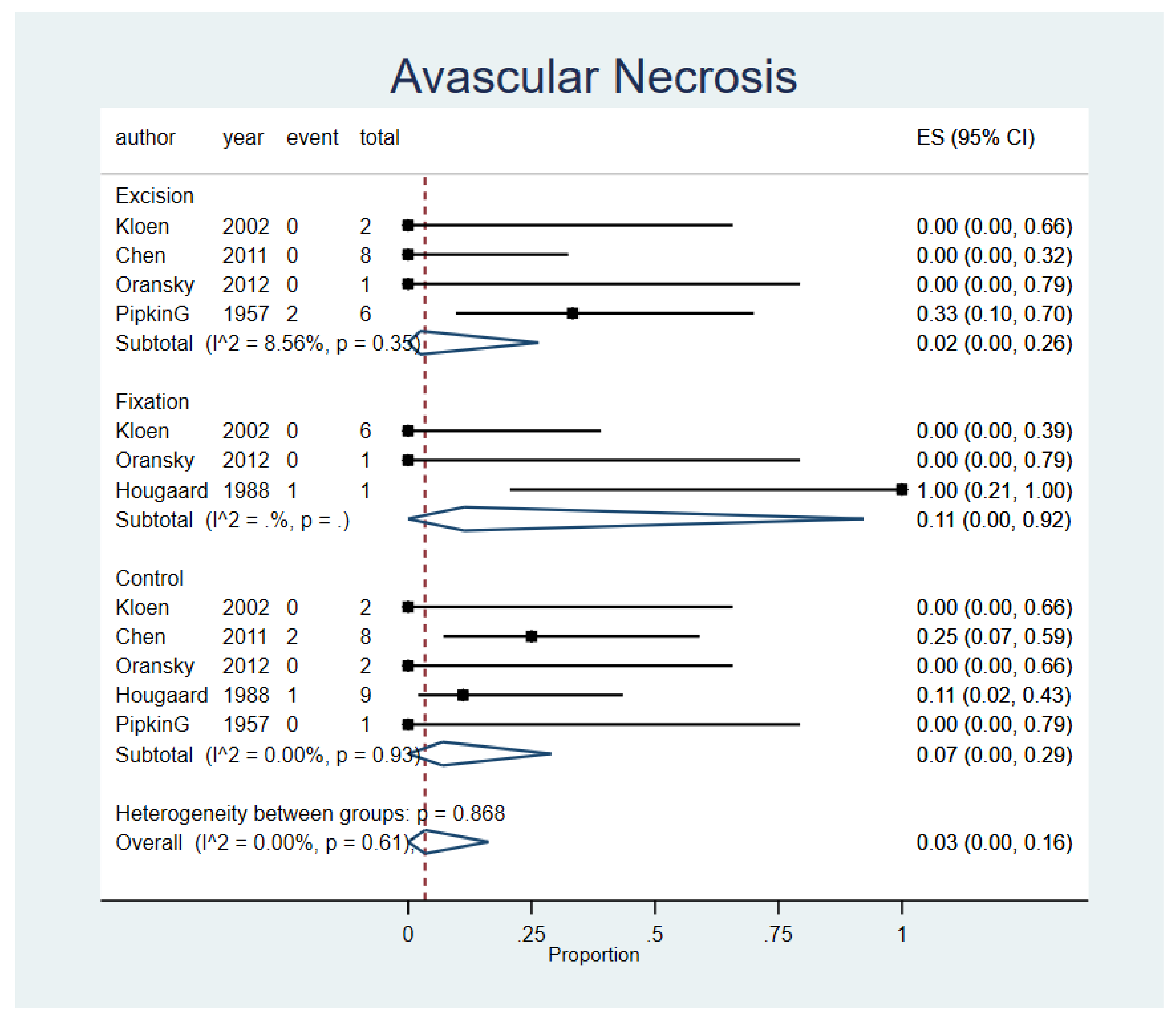
3.4. Avascular Necrosis
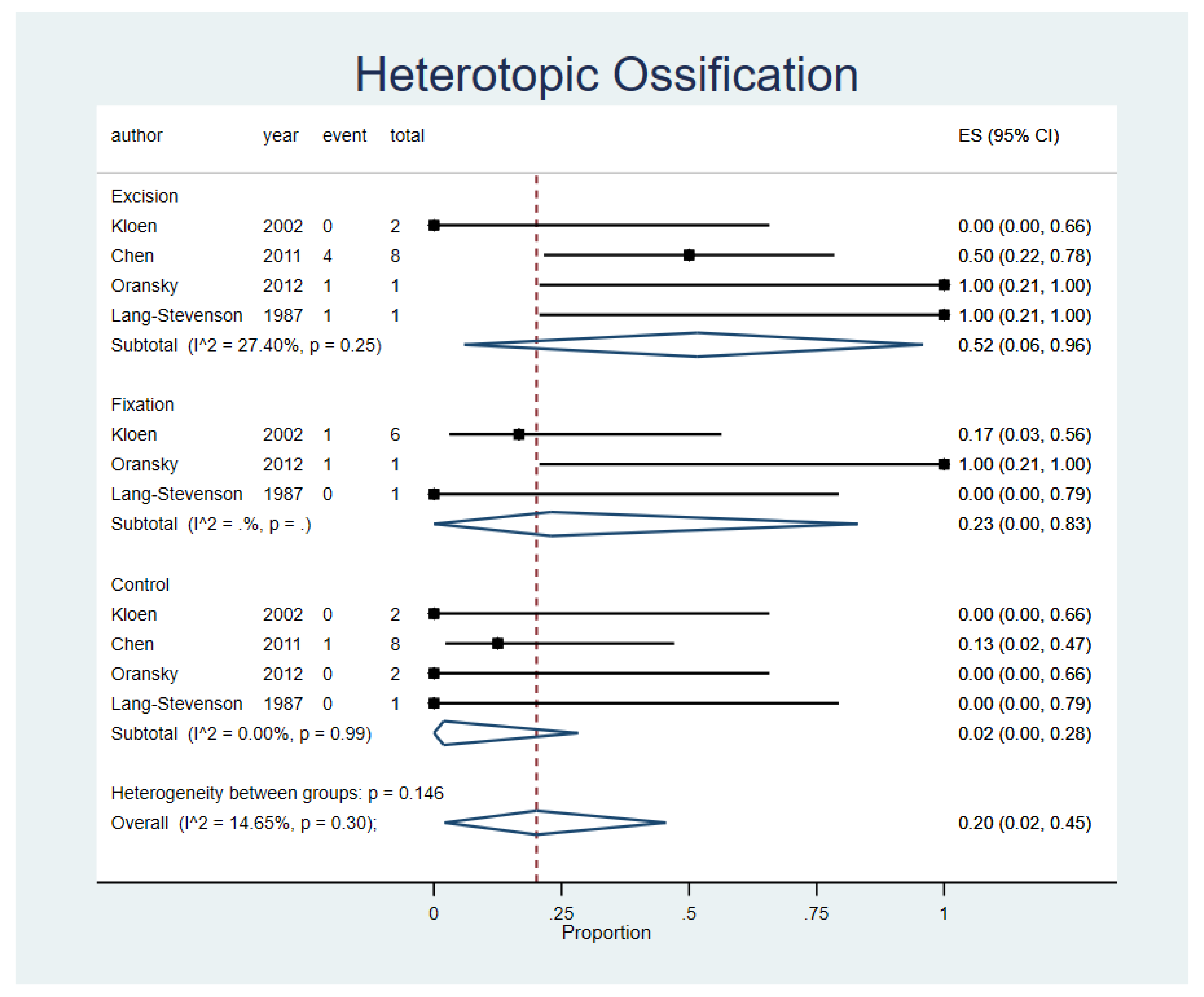
3.5. Heterotopic Ossification
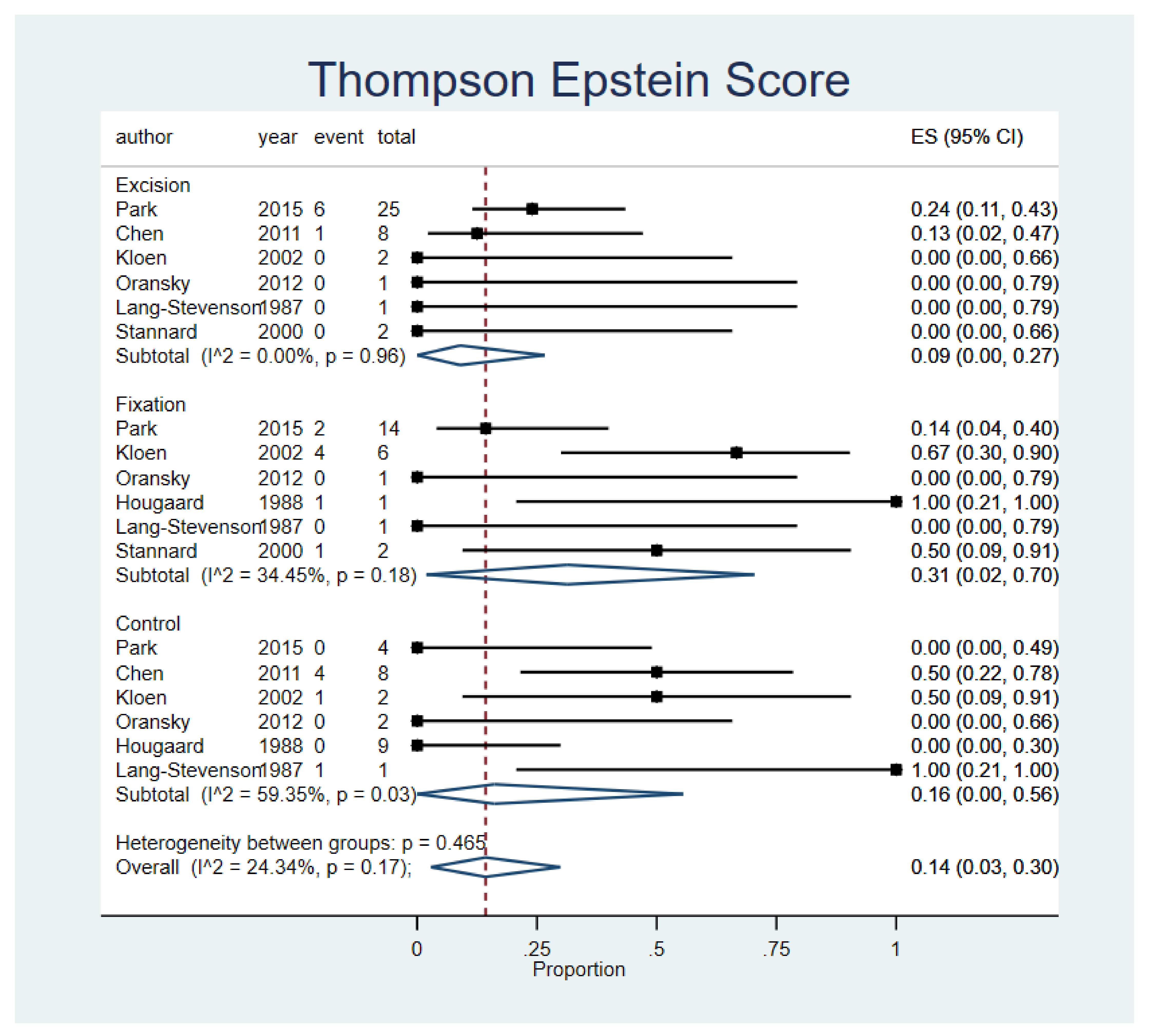
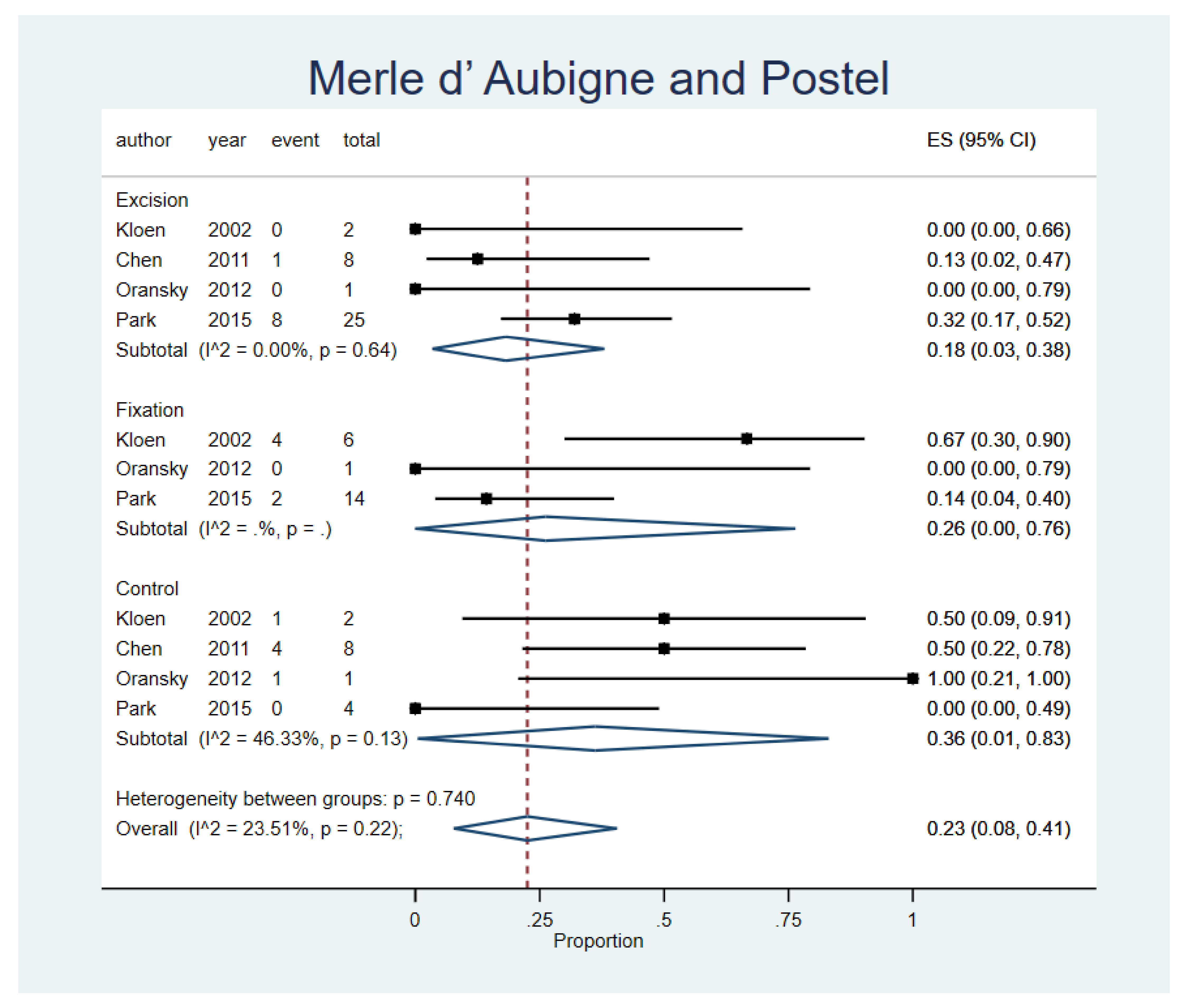
3.6. Thompson Epstein Score and Merle d’ Aubigne and Postel Score
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HO | Heterotopic Ossification |
| AVN | Avascular Necrosis |
| CI | Confidence Interval |
| ES | effect size |
| RCT | Randomized Controlled Trial |
| ORIFs | open reduction internal fixations |
| WA | weighted averages |
| SDs | standard deviations |
References
- Kelly, P.J.; Lipscomb, P.R. Primary Vitallium-Mold Arthroplasty for Posterior Dislocation of the Hip with Fracture of the Femoral Head. J. Bone Joint Surg. Am. Vol. 1958, 40, 675–680. [Google Scholar] [CrossRef]
- Henle, P.; Kloen, P.; Siebenrock, K.A. Femoral head injuries: Which treatment strategy can be recommended? Injury 2007, 38, 478–488. [Google Scholar] [CrossRef] [PubMed]
- Giannoudis, P.; Kontakis, G.; Christoforakis, Z.; Akula, M.; Tosounidis, T.; Koutras, C. Management, complications and clinical results of femoral head fractures. Injury 2009, 40, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Park, K.-S.; Lee, K.-B.; Na, B.-R.; Yoon, T.-R. Clinical and radiographic outcomes of femoral head fractures: Excision vs. fixation of fragment in Pipkin type I: What is the optimal choice for femoral head fracture? J. Orthop. Sci. 2015, 20, 702–707. [Google Scholar] [CrossRef]
- Scolaro, J.A.; Marecek, G.; Firoozabadi, R.; Krieg, J.C.; Routt, M.L. “Chip” Management and radiographic outcomes of femoral head fractures. J. Orthop. Traumatol. 2017, 18, 235–241. [Google Scholar] [CrossRef] [Green Version]
- Asghar, F.A.; Karunakar, M.A. Femoral head fractures: Diagnosis, management, and complications. Orthop. Clin. North Am. 2004, 35, 463–472. [Google Scholar] [CrossRef] [PubMed]
- Brumback, R.J. Fractures of the femoral head. Hip 1987, 181–206. [Google Scholar]
- Epstein, H.C. Posterior Fracture-Dislocations of the Hip. J. Bone Joint Surg. Am. Vol. 1974, 56, 1103–1127. [Google Scholar] [CrossRef]
- Hougaard, K.; Thomsen, P.B. Traumatic posterior fracture-dislocation of the hip with fracture of the femoral head or neck, or both. J. Bone Joint Surg. Am. Vol. 1988, 70, 233–239. [Google Scholar] [CrossRef]
- Stannard, J.P.; Harris, H.W.; Volgas, D.A.; Alonso, J.E. Functional Outcome of Patients with Femoral Head Fractures Associated with Hip Dislocations. Clin. Orthop. Relat. Res. 2000, 377, 44–56. [Google Scholar] [CrossRef]
- Pipkin, G. Treatment of Grade IV Fracture-Dislocation of the Hip. J. Bone Joint Surg. Am. Vol. 1957, 5, 1027–1042. [Google Scholar] [CrossRef]
- Romeo, N.M.; Firoozabadi, R. Classifications in Brief: The Pipkin Classification of Femoral Head Fractures. Clin. Orthop. Relat. Res. 2018, 476, 1114–1119. [Google Scholar] [CrossRef]
- Behery, O.A.; Dai, A.Z.; McLaurin, T.M. Posttraumatic Heterotopic Ossification of the Hip. J. Orthop. Trauma 2018, 32, S18–S19. [Google Scholar] [CrossRef]
- Bossche, L.V.; Vanderstraeten, G. Heterotopic ossification: A review. J. Rehabil. Med. 2005, 37, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Chiron, P.; Lafontan, V.; Reina, N. Fracture-dislocations of the femoral head. Orthop. Traumatol. Surg. Res. 2013, 99, S53–S66. [Google Scholar] [CrossRef] [Green Version]
- Guo, J.J.; Tang, N.; Yang, H.L.; Qin, L.; Leung, K.S. Impact of surgical approach on postoperative heterotopic ossification and avascular necrosis in femoral head fractures: A systematic review. Int. Orthop. 2009, 34, 319–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoskinson, S.; Morison, Z.; Shahrokhi, S.; Schemitsch, E.H. Managing AVN following internal fixation: Treatment options and clinical results. Injury 2015, 46, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Masse’, A.; Aprato, A.; Alluto, C.; Favuto, M.; Ganz, R. Surgical Hip Dislocation Is a Reliable Approach for Treatment of Femoral Head Fractures. Clin. Orthop. Relat. Res. 2015, 473, 3744–3751. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Tian, Q.; Liu, Y.; Shao, Z.; Yang, S. Mid- and long-term clinical effects of trochanteric flip osteotomy for treatment of Pipkin I and II femoral head fractures. J. South. Med Univ. 2013, 33, 1260–1264. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Ugino, F.K.; Righetti, C.M.; Alves, D.P.L.; Guimarães, R.P.; Honda, E.K.; Ono, N.K. Evaluation of the reliability of the modified Merle d’Aubigné and Postel Method. Acta Ortop. Bras. 2012, 20, 213–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [Green Version]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Lang-Stevenson, A.; Getty, C. The Pipkin fracture-dislocation of the hip. Injury 1987, 18, 264–269. [Google Scholar] [CrossRef]
- Kloen, P.; Siebenrock, K.A.; Raaymakers, E.L.F.B.; Marti, R.K.; Ganz, R. Femoral Head Fractures Revisited. Eur. J. Trauma Emerg. Surg. 2002, 28, 221–233. [Google Scholar] [CrossRef]
- Chen, Z.-W.; Lin, B.; Zhai, W.-L.; Guo, Z.-M.; Liang, Z.; Zheng, J.-P.; Lian, K.-J.; Ding, Z.-Q. Conservative versus surgical management of Pipkin type I fractures associated with posterior dislocation of the hip: A randomised controlled trial. Int. Orthop. 2010, 35, 1077–1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oransky, M.; Martinelli, N.; Sanzarello, I.; Papapietro, N. Fractures of the femoral head: A long-term follow-up study. Musculoskelet. Surg. 2012, 96, 95–99. [Google Scholar] [CrossRef]
- Wilson, E.B. Probable Inference, the Law of Succession, and Statistical Inference. J. Am. Stat. Assoc. 1927, 22, 209–212. [Google Scholar] [CrossRef]
- Freeman, M.F.; Tukey, J.W. Transformations Related to the Angular and the Square Root. Ann. Math. Stat. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.; Egger, M. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. J. Clin. Epidemiol. 2001, 54, 1046–1055. [Google Scholar] [CrossRef]
- Rosenthal, R.E.; Coker, W.L. Posterior Fracture-dislocation of the Hip. J. Trauma Inj. Infect. Crit. Care 1979, 19, 572–581. [Google Scholar] [CrossRef]
- Yoon, T.R.; Rowe, S.M.; Chung, J.Y.; Song, E.K.; Jung, S.T.; Anwar, I.B. Clinical and radiographic outcome of femoral head fractures: 30 patients followed for 3-10 years. Acta Orthop. Scand. 2001, 72, 348–353. [Google Scholar] [CrossRef] [PubMed]
- McMurtry, I.; Quaile, A. Closed reduction of the traumatically dislocated hip: A new technique. Injury 2001, 32, 162–164. [Google Scholar] [CrossRef]
- Mostafa, M.F.; El-Adl, W.; El-Sayed, M.A.-E. Operative treatment of displaced Pipkin type I and II femoral head fractures. Arch. Orthop. Trauma Surg. 2014, 134, 637–644. [Google Scholar] [CrossRef]
- Ross, J.R.; Gardner, M.J. Femoral head fractures. Curr. Rev. Musculoskelet. Med. 2012, 5, 199–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chakraborti, S.; Miller, I. Dislocation of the hip associated with fracture of the femoral head. Injury 1975, 7, 134–142. [Google Scholar] [CrossRef]
- Epstein, H.C.; A Wiss, D.; Cozen, L. Posterior fracture dislocation of the hip with fractures of the femoral head. Clin. Orthop. Relat. Res. 1985, 201, 9–17. [Google Scholar] [CrossRef]
- Holmes, W.J.; Solberg, B.; Bay, B.K.; Laubach, J.E.; Olson, S.A. Biomechanical consequences of excision of displaced Pipkin femoral head fractures. J. Orthop. Trauma 2000, 14, 149–150. [Google Scholar] [CrossRef]

| Study | Selection | Comparability | Exposure/Outcome | Total |
|---|---|---|---|---|
| Pipkin et al. (1957) [11] | 2 | NA | 3 | 5 |
| Lang-Stevenson et al. (1987) [24] | 2 | NA | 3 | 5 |
| Hougaard et al. (1988) [9] | 2 | NA | 3 | 5 |
| Stannard et al. (2000) [10] | 2 | NA | 3 | 5 |
| Kloen et al. (2002) [25] | 2 | NA | 3 | 5 |
| Chen et al. (2010) [26] | 4 | 2 | 3 | 9 |
| Oransky et al. (2012) [27] | 1 | NA | 3 | 4 |
| Park et al. (2015) [4] | 2 | NA | 3 | 5 |
| Study | Study Design | Total Patient Number, n (%) | Pipkin 1 Cases, n (%) |
|---|---|---|---|
| Pipkin et al. (1957) [11] | Retrospective | 24 (12) | 7 (7.2) |
| Lang-Stevenson et al. (1987) [24] | Retrospective | 7 (3.5) | 3 (3.1) |
| Hougaard et al. (1988) [9] | Retrospective | 19 (9.5) | 10 (10.3) |
| Stannard et al. (2000) [10] | Retrospective | 22 (11) | 4 (4.1) |
| Kloen et al. (2002) [25] | Retrospective | 32 (16) | 10 (10.3) |
| Chen et al. (2010) [26] | Prospective | 16 (8) | 16 (16.5) |
| Oransky et al. (2012) [27] | Retrospective | 21 (10.5) | 4 (4.1) |
| Park et al. (2015) [4] | Retrospective | 59 (29.5) | 43 (44.3) |
| Total | 200 | 97 |
| Treatment Choice | Pipkin 1 Cases (n = 97) |
|---|---|
| Excision fragment, n (%) | 45(46.4) |
| Large fragment | 11 |
| Small fragment + | 23 |
| Not classified | 11 |
| Open reduction internal fixation, n (%) | 25(25.8) |
| Close reduction, n (%) | 27(27.8) |
| Characteristics | Pipkin 1 Cases (n = 97) |
|---|---|
| Age (yrs) * | 39.3 |
| Gender, n (%) | |
| Male | 70 (72.2) |
| Female | 27 (27.8) |
| Follow-up, months | 79.7 |
| Mechanism of injury, n (%) | |
| Motor-vehicle accident | 87 (89.7) |
| Fall Injury | 5 (5.2) |
| Hit by a falling wall | 1 (1.0) |
| Not recorded | 4 (4.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, S.H.L.; Tai, W.-C.; Fu, T.-S.; Tischler, E.H.; Rahman, R.; Lim, Y.-K.; Yu, Y.-H.; Su, C.-Y. Does Surgical Repair Benefit Pipkin Type I Femoral Head Fractures?: A Systematic Review and Meta-Analysis. Life 2022, 12, 71. https://doi.org/10.3390/life12010071
Tsai SHL, Tai W-C, Fu T-S, Tischler EH, Rahman R, Lim Y-K, Yu Y-H, Su C-Y. Does Surgical Repair Benefit Pipkin Type I Femoral Head Fractures?: A Systematic Review and Meta-Analysis. Life. 2022; 12(1):71. https://doi.org/10.3390/life12010071
Chicago/Turabian StyleTsai, Sung Huang Laurent, Wei-Che Tai, Tsai-Sheng Fu, Eric H. Tischler, Rafa Rahman, Yong-Kuan Lim, Yi-Hsun Yu, and Chun-Yi Su. 2022. "Does Surgical Repair Benefit Pipkin Type I Femoral Head Fractures?: A Systematic Review and Meta-Analysis" Life 12, no. 1: 71. https://doi.org/10.3390/life12010071
APA StyleTsai, S. H. L., Tai, W.-C., Fu, T.-S., Tischler, E. H., Rahman, R., Lim, Y.-K., Yu, Y.-H., & Su, C.-Y. (2022). Does Surgical Repair Benefit Pipkin Type I Femoral Head Fractures?: A Systematic Review and Meta-Analysis. Life, 12(1), 71. https://doi.org/10.3390/life12010071





