Immunotherapy and Metastatic Renal Cell Carcinoma: A Review of New Treatment Approaches
Abstract
:1. Introduction
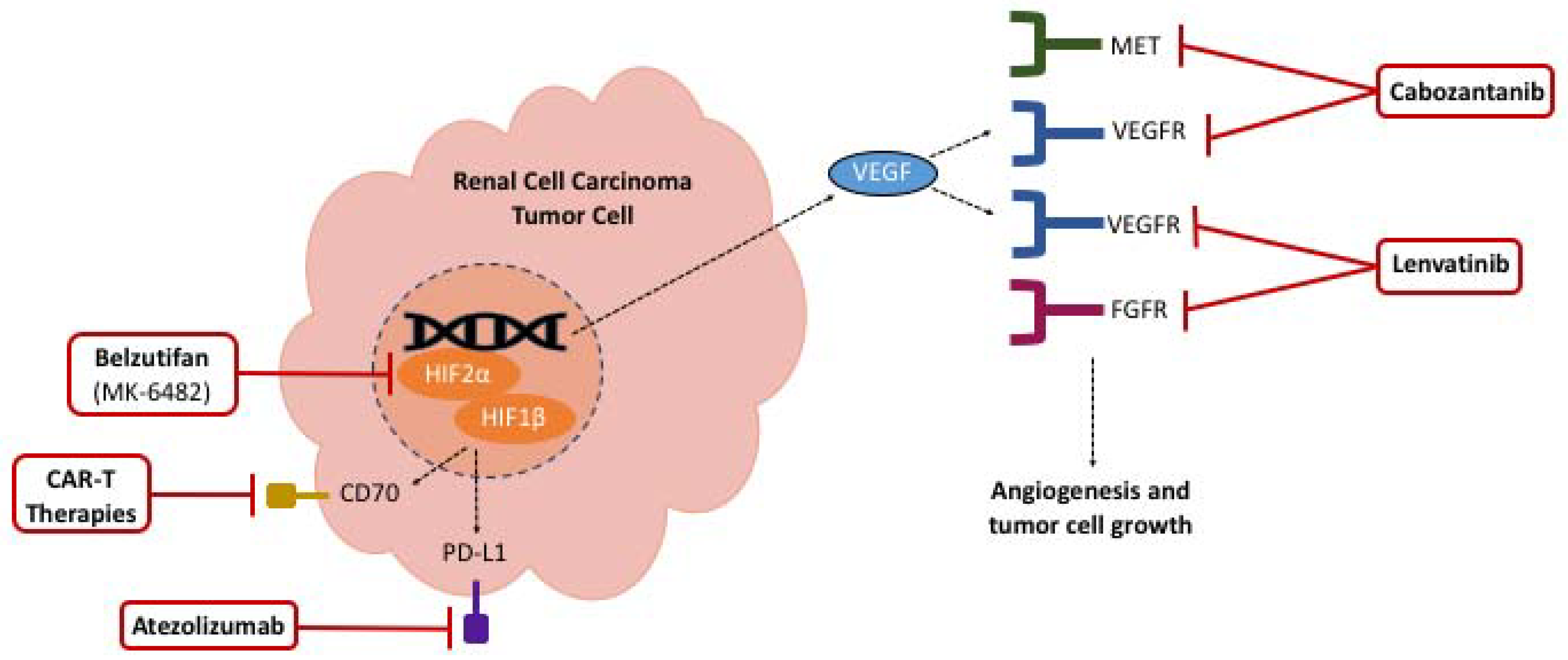
2. Current Therapies
2.1. Sunitinib
2.2. Ipilimumab & Nivolumab
2.3. Atezolizumab & Bevacizumab
2.4. Axitinib & Avelumab
2.5. Axitinib & Pembrolizumab
2.6. Cabozantinib & Nivolumab
2.7. Lenvatinib & Pembrolizumab
3. Future Therapies (Ongoing Clinical Trials)
3.1. HIF-2 Alpha Inhibitors
3.2. CD70A Targeted Antibody-Drug Conjugates
3.3. MK-6482-011
3.4. CONTACT-03
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cancer of the Kidney and Renal Pelvis—Cancer Stat Facts. SEER. Available online: https://seer.cancer.gov/statfacts/html/kidrp.html (accessed on 30 August 2021).
- Negrier, S.; Escudier, B.; Lasset, C.; Douillard, J.-Y.; Savary, J.; Chevreau, C.; Ravaud, A.; Mercatello, A.; Peny, J.; Mousseau, M.; et al. Recombinant Human Interleukin-2, Recombinant Human Interferon Alfa-2a, or Both in Metastatic Renal-Cell Carcinoma. N. Engl. J. Med. 1998, 338, 1272–1278. [Google Scholar] [CrossRef]
- Fyfe, G.; Fisher, R.I.; Rosenberg, S.A.; Sznol, M.; Parkinson, D.R.; Louie, A.C. Results of treatment of 255 patients with metastatic renal cell carcinoma who received high-dose recombinant interleukin-2 therapy. J. Clin. Oncol. 1995, 13, 688–696. [Google Scholar] [CrossRef] [PubMed]
- McDermott, D.F.; Regan, M.M.; Clark, J.I.; Flaherty, L.E.; Weiss, G.R.; Logan, T.F.; Kirkwood, J.M.; Gordon, M.S.; Sosman, J.A.; Ernstoff, M.S.; et al. Randomized Phase III Trial of High-Dose Interleukin-2 Versus Subcutaneous Interleukin-2 and Interferon in Patients with Metastatic Renal Cell Carcinoma. J. Clin. Oncol. 2005, 23, 133–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDermott, D.F.; Cheng, S.-C.; Signoretti, S.; Margolin, K.; Clark, J.I.; Sosman, J.A.; Dutcher, J.P.; Logan, T.F.; Curti, B.D.; Ernstoff, M.S.; et al. The High-Dose Aldesleukin “Select” Trial: A Trial to Prospectively Validate Predictive Models of Response to Treatment in Patients with Metastatic Renal Cell Carcinoma. Clin. Cancer Res. 2015, 21, 561–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patard, J.-J.; Leray, E.; Rioux-Leclercq, N.; Cindolo, L.; Ficarra, V.; Zisman, A.; De La Taille, A.; Tostain, J.; Artibani, W.; Abbou, C.C.; et al. Prognostic Value of Histologic Subtypes in Renal Cell Carcinoma: A Multicenter Experience. J. Clin. Oncol. 2005, 23, 2763–2771. [Google Scholar] [CrossRef]
- Lainakis, G.; Bamias, A. Targeting angiogenesis in renal cell carcinoma. Expert Opin. Pharmacother. 2013, 14, 2221–2236. [Google Scholar] [CrossRef]
- Posadas, E.M.; Limvorasak, S.; Figlin, R.A. Targeted therapies for renal cell carcinoma. Nat. Rev. Nephrol. 2017, 13, 496–511. [Google Scholar] [CrossRef]
- Motzer, R.J.; Hutson, T.E.; Tomczak, P.; Michaelson, M.D.; Bukowski, R.M.; Rixe, O.; Oudard, S.; Negrier, S.; Szczylik, C.; Kim, S.T.; et al. Sunitinib versus Interferon Alfa in Metastatic Renal-Cell Carcinoma. N. Engl. J. Med. 2007, 356, 115–124. [Google Scholar] [CrossRef]
- Chow, L.Q.; Eckhardt, S.G. Sunitinib: From Rational Design to Clinical Efficacy. J. Clin. Oncol. 2007, 25, 884–896. [Google Scholar] [CrossRef]
- Escudier, B.; Eisen, T.; Stadler, W.M.; Szczylik, C.; Oudard, S.; Siebels, M.; Negrier, S.; Chevreau, C.; Solska, E.; Desai, A.A.; et al. Sorafenib in Advanced Clear-Cell Renal-Cell Carcinoma. N. Engl. J. Med. 2007, 356, 125–134, (Published Online). [Google Scholar] [CrossRef]
- Sternberg, C.N.; Davis, I.D.; Mardiak, J.; Szczylik, C.; Lee, E.; Wagstaff, J.; Barrios, C.H.; Salman, P.; Gladkov, O.A.; Kavina, A.; et al. Pazopanib in Locally Advanced or Metastatic Renal Cell Carcinoma: Results of a Randomized Phase III Trial. J. Clin. Oncol. 2010, 28, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- Rini, B.I.; Powles, T.; Atkins, M.B.; Escudier, B.; McDermott, D.F.; Suarez, C.; Bracarda, S.; Stadler, W.M.; Donskov, F.; Lee, J.L.; et al. Atezolizumab plus bevacizumab versus sunitinib in patients with previously untreated metastatic renal cell carcinoma (IMmotion151): A multicentre, open-label, phase 3, randomised controlled trial. Lancet 2019, 393, 2404–2415. [Google Scholar] [CrossRef]
- Motzer, R.J.; Penkov, K.; Haanen, J.; Rini, B.; Albiges, L.; Campbell, M.T.; Venugopal, B.; Kollmannsberger, C.; Negrier, S.; Uemura, M.; et al. Avelumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2019, 380, 1103–1115. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Hutson, T.E.; Glen, H.; Michaelson, D.; Molina, A.; Eisen, T.; Jassem, J.; Zolnierek, J.; Maroto, J.P.; Mellado, B.; et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: A randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015, 16, 1473–1482. [Google Scholar] [CrossRef] [Green Version]
- Choueiri, T.K.; Powles, T.; Burotto, M.; Escudier, B.; Bourlon, M.T.; Zurawski, B.; Oyervides Juárez, V.M.; Hsieh, J.J.; Basso, U.; Shah, A.Y.; et al. Nivolumab plus Cabozantinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2021, 384, 829–841. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Escudier, B.; Powles, T.; Mainwaring, P.N.; Rini, B.I.; Donskov, F.; Hammers, H.; Hutson, T.E.; Lee, J.-L.; Peltola, K.; et al. Cabozantinib versus Everolimus in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2015, 373, 1814–1823. [Google Scholar] [CrossRef]
- Rini, B.I.; Halabi, S.; Rosenberg, J.E.; Stadler, W.M.; Vaena, D.A.; Ou, S.-S.; Archer, L.; Atkins, J.N.; Picus, J.; Czaykowski, P.; et al. Bevacizumab Plus Interferon Alfa Compared with Interferon Alfa Monotherapy in Patients with Metastatic Renal Cell Carcinoma: CALGB 90206. J. Clin. Oncol. 2008, 26, 5422–5428. [Google Scholar] [CrossRef]
- Hudes, G.; Carducci, M.; Tomczak, P.; Dutcher, J.; Figlin, R.; Kapoor, A.; Staroslawska, E.; Sosman, J.; McDermott, D.; Bodrogi, I.; et al. Temsirolimus, Interferon Alfa, or Both for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2007, 356, 2271–2281, (Published Online). [Google Scholar] [CrossRef] [Green Version]
- Motzer, R.J.; Escudier, B.; Oudard, S.; Do, T.E.H.; Porta, C.; Bracarda, S.; Grünwald, V.; Thompson, J.A.; Figlin, R.A.; Hollaender, N.; et al. Phase 3 trial of everolimus for metastatic renal cell carcinoma: Final results and analysis of prognostic factors. Cancer 2010, 116, 4256–4265. [Google Scholar] [CrossRef]
- Pardoll, D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer 2012, 12, 252–264. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Lopez, R.; Luchtel, R.A.; Hafizi, S.; Gartrell, B.; Shenoy, N. Immune evasion in renal cell carcinoma: Biology, clinical translation, future directions. Kidney Int. 2021, 99, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.H.; Dong, H.; Kwon, E.D. Implications of B7-H1 Expression in Clear Cell Carcinoma of the Kidney for Prognostication and Therapy. Clin. Cancer Res. 2007, 13, 709s–715s. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motzer, R.J.; Tannir, N.M.; McDermott, D.F.; Arén Frontera, O.; Melichar, B.; Choueiri, T.K.; Plimack, E.R.; Barthélémy, P.; Porta, C.; George, S.; et al. Nivolumab plus Ipilimumab versus Sunitinib in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2018, 378, 1277–1290. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Rini, B.I.; Bukowski, R.M.; Curti, B.D.; George, D.J.; Hudes, G.R.; Redman, B.G.; Margolin, K.; Merchan, J.R.; Wilding, G.; et al. Sunitinib in Patients with Metastatic Renal Cell Carcinoma. JAMA 2006, 295, 2516–2524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motzer, R.J.; Michaelson, M.D.; Redman, B.G.; Hudes, G.R.; Wilding, G.; Figlin, R.A.; Ginsberg, M.S.; Kim, S.T.; Baum, C.M.; DePrimo, S.E.; et al. Activity of SU11248, a Multitargeted Inhibitor of Vascular Endothelial Growth Factor Receptor and Platelet-Derived Growth Factor Receptor, in Patients with Metastatic Renal Cell Carcinoma. J. Clin. Oncol. 2006, 24, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Escudier, B.; Bukowski, R.; Rini, B.I.; Hutson, T.E.; Barrios, C.H.; Lin, X.; Fly, K.; Matczak, E.; Gore, M.E. Prognostic factors for survival in 1059 patients treated with sunitinib for metastatic renal cell carcinoma. Br. J. Cancer 2013, 108, 2470–2477. [Google Scholar] [CrossRef]
- Ravaud, A.; Motzer, R.J.; Pandha, H.S.; George, D.J.; Pantuck, A.J.; Patel, A.; Chang, Y.-H.; Escudier, B.; Donskov, F.; Magheli, A.; et al. Adjuvant Sunitinib in High-Risk Renal-Cell Carcinoma after Nephrectomy. N. Engl. J. Med. 2016, 375, 2246–2254. [Google Scholar] [CrossRef]
- Albiges, L.; Tannir, N.M.; Burotto, M.; McDermott, D.; Plimack, E.R.; Barthélémy, P.; Porta, C.; Powles, T.; Donskov, F.; George, S.; et al. Nivolumab plus ipilimumab versus sunitinib for first-line treatment of advanced renal cell carcinoma: Extended 4-year follow-up of the phase III CheckMate 214 trial. ESMO Open 2020, 5, e001079. [Google Scholar] [CrossRef] [PubMed]
- Rini, B.I.; Atkins, M.B.; Escudier, B.; Powles, T.; McDermott, D.F.; Alekseev, B.Y.; Lee, J.-L.; Stroyakovskiy, D.; Rodriguez, C.S.; De Giorgi, U.; et al. Abstract CT188: IMmotion 151: Updated overall survival (OS) and exploratory analysis of the association of gene expression and clinical outcomes with atezolizumab plus bevacizumab vs sunitinib in patients with locally advanced or metastatic renal cell carcinoma (mRCC). Clin. Trials 2021, 81, CT188. [Google Scholar] [CrossRef]
- Infinity Pharmaceuticals, Inc. A Phase 2, Multi-Arm, Multicenter, Open-Label Study to Evaluate the Efficacy and Safety of IPI-549 Administered in Combination with Front-Line Treatment Regimens in Patients with Locally Advanced and/or Metastatic Triple-Negative Breast Cancer or Renal Cell Carcinoma. 2020. Available online: https://clinicaltrials.gov/ct2/show/NCT03961698 (accessed on 9 September 2021).
- Choueiri, T.K.; Larkin, J.; Oya, M.; Thistlethwaite, F.; Martignoni, M.; Nathan, P.; Powles, T.; McDermott, D.; Robbins, P.B.; Chism, D.D.; et al. Preliminary results for avelumab plus axitinib as first-line therapy in patients with advanced clear-cell renal-cell carcinoma (JAVELIN Renal 100): An open-label, dose-finding and dose-expansion, phase 1b trial. Lancet Oncol. 2018, 19, 451–460. [Google Scholar] [CrossRef]
- Choueiri, T.; Motzer, R.; Rini, B.; Haanen, J.; Campbell, M.; Venugopal, B.; Kollmannsberger, C.; Gravis-Mescam, G.; Uemura, M.; Lee, J.; et al. Updated efficacy results from the JAVELIN Renal 101 trial: First-line avelumab plus axitinib versus sunitinib in patients with advanced renal cell carcinoma. Ann. Oncol. 2020, 31, 1030–1039. [Google Scholar] [CrossRef] [PubMed]
- Rini, B.I.; Plimack, E.R.; Stus, V.; Gafanov, R.; Hawkins, R.; Nosov, D.; Pouliot, F.; Alekseev, B.; Soulières, D.; Melichar, B.; et al. Pembrolizumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2019, 380, 1116–1127. [Google Scholar] [CrossRef] [PubMed]
- Powles, T.; Plimack, E.R.; Soulières, D.; Waddell, T.; Stus, V.; Gafanov, R.; Nosov, D.; Pouliot, F.; Melichar, B.; Vynnychenko, I.; et al. Pembrolizumab plus axitinib versus sunitinib monotherapy as first-line treatment of advanced renal cell carcinoma (KEYNOTE-426): Extended follow-up from a randomised, open-label, phase 3 trial. Lancet Oncol. 2020, 21, 1563–1573. [Google Scholar] [CrossRef]
- Rini, B.I.; Plimack, E.R.; Stus, V.; Waddell, T.; Gafanov, R.; Pouliot, F.; Nosov, D.; Melichar, B.; Soulieres, D.; Borchiellini, D.; et al. Pembrolizumab (pembro) plus axitinib (axi) versus sunitinib as first-line therapy for advanced clear cell renal cell carcinoma (ccRCC): Results from 42-month follow-up of KEYNOTE-426. J. Clin. Oncol. 2021, 39 (Suppl. 15), 4500. [Google Scholar] [CrossRef]
- Bedke, J.; Albiges, L.; Capitanio, U.; Giles, R.H.; Hora, M.; Lam, T.B.; Ljungberg, B.; Marconi, L.; Klatte, T.; Volpe, A.; et al. Updated European Association of Urology Guidelines on Renal Cell Carcinoma: Nivolumab plus Cabozantinib Joins Immune Checkpoint Inhibition Combination Therapies for Treatment-naïve Metastatic Clear-Cell Renal Cell Carcinoma. Eur. Urol. 2021, 79, 339–342. [Google Scholar] [CrossRef]
- FDA. Research C for DE and FDA Approves Nivolumab Plus Cabozantinib for Advanced Renal Cell Carcinoma. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-nivolumab-plus-cabozantinib-advanced-renal-cell-carcinoma (accessed on 12 June 2021).
- Motzer, R.; Alekseev, B.; Rha, S.-Y.; Porta, C.; Eto, M.; Powles, T.; Grünwald, V.; Hutson, T.E.; Kopyltsov, E.; Méndez-Vidal, M.J.; et al. Lenvatinib plus Pembrolizumab or Everolimus for Advanced Renal Cell Carcinoma. N. Engl. J. Med. 2021, 384, 1289–1300. [Google Scholar] [CrossRef]
- Eisai Inc. A Multicenter, Open-Label, Randomized, Phase 3 Trial to Compare the Efficacy and Safety of Lenvatinib in Combination with Everolimus or Pembrolizumab Versus Sunitinib Alone in First-Line Treatment of Subjects with Advanced Renal Cell Carcinoma (CLEAR). 2021. Available online: https://clinicaltrials.gov/ct2/show/NCT02811861 (accessed on 26 August 2021).
- Cuvillier, O. The therapeutic potential of HIF-2 antagonism in renal cell carcinoma. Transl. Androl. Urol. 2017, 6, 131–133. [Google Scholar] [CrossRef] [Green Version]
- Peloton Therapeutics, Inc. A Phase 1, Multiple-Dose, Dose-Escalation Trial of PT2385 Tablets, a HIF-2α Inhibitor, in Patients with Advanced Clear Cell Renal Cell Carcinoma. 2021. Available online: https://clinicaltrials.gov/ct2/show/NCT02293980 (accessed on 26 August 2021).
- FDA. Research C for DE and FDA Approves Belzutifan for Cancers Associated with von Hippel-Lindau Disease. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-belzutifan-cancers-associated-von-hippel-lindau-disease (accessed on 13 August 2021).
- Jonasch, E.; Donskov, F.; Iliopoulos, O.; Rathmell, W.K.; Narayan, V.; Maughan, B.L.; Oudard, S.; Else, T.; Maranchie, J.K.; Welsh, S.J.; et al. Phase II study of the oral HIF-2α inhibitor MK-6482 for Von Hippel-Lindau disease–associated renal cell carcinoma. J. Clin. Oncol. 2020, 38 (Suppl. 15), 5003. [Google Scholar] [CrossRef]
- Pal, S.K.; Forero-Torres, A.; Thompson, J.A.; Morris, J.C.; Chhabra, S.; Hoimes, C.; Vogelzang, N.J.; Boyd, T.; Bergerot, P.G.; Ba, J.J.A.; et al. A phase 1 trial of SGN-CD70A in patients with CD70-positive, metastatic renal cell carcinoma. Cancer 2019, 125, 1124–1132. [Google Scholar] [CrossRef]
- Allogene Therapeutics. A Phase 1 Multicenter Study Evaluating the Safety and Efficacy of ALLO-316 Following ALLO-647 Containing Conditioning Regimen in Subjects with Advanced or Metastatic Clear Cell Renal Cell Carcinoma. clinicaltri-als.gov. 2021. Available online: https://clinicaltrials.gov/ct2/show/NCT04696731 (accessed on 9 September 2021).
- Titov, A.; Zmievskaya, E.; Ganeeva, I.; Valiullina, A.; Petukhov, A.; Rakhmatullina, A.; Miftakhova, R.; Fainshtein, M.; Rizvanov, A.; Bulatov, E. Adoptive Immunotherapy beyond CAR T-Cells. Cancers 2021, 13, 743. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Plimack, E.R.; Bauer, T.M.; Merchan, J.R.; Papadopoulos, K.P.; McDermott, D.F.; Michaelson, M.D.; Appleman, L.J.; Thamake, S.; Zojwalla, N.J.; et al. Phase I/II study of the oral HIF-2 α inhibitor MK-6482 in patients with advanced clear cell renal cell carcinoma (RCC). J. Clin. Oncol. 2020, 38, 611. [Google Scholar] [CrossRef]
- Merck Sharp & Dohme Corp. An Open-Label, Randomized, Phase 3 Study of MK-6482 in Combination with Lenvatinib (MK-7902) vs. Cabozantinib for Second-Line or Third-Line Treatment in Participants with Advanced Renal Cell Carcinoma Who Have Progressed after Prior Anti-PD-1/L1 Therapy. Available online: https://clinicaltrials.gov/ct2/show/NCT04586231 (accessed on 23 August 2021).
- ClinicalTrials.gov. A Study of Atezolizumab in Combination with Cabozantinib Compared to Cabozantinib Alone in Participants with Advanced Renal Cell Carcinoma after Immune Checkpoint Inhibitor Treatment (CONTACT-03). Available online: https://www.clinicaltrials.gov/ct2/show/NCT04338269 (accessed on 18 August 2021).
- Agarwal, N.; Vaishampayan, U.; Green, M.; Di Nucci, F.; Chang, P.-Y.; Scheffold, C.; Pal, S. Phase IB study (COSMIC-021) of cabozantinib in combination with atezolizumab: Results of the dose escalation stage in patients (pts) with treatment-naïve advanced renal cell carcinoma (RCC). Ann. Oncol. 2018, 29, viii308. [Google Scholar] [CrossRef]
- Kwilas, A.R.; Ardiani, A.; Donahue, R.N.; Aftab, D.; Hodge, J.W. Effects of Cabozantinib, a small molecule tyrosine kinase inhibitor, on the immune permissiveness of the tumor microenvironment and immune-mediated killing of tumor cells. J. Immunother. Cancer 2014, 2 (Suppl. 3), P185. [Google Scholar] [CrossRef] [Green Version]
| Trial | Therapies Evaluated | Clinical Trial Phase |
|---|---|---|
| Motzer et al., 2007 [9] | sunitinib vs. interferon alfa | Phase 3 |
| Motzer et al., 2018 (CheckMate 214) [24] | ipilimumab + nivolumab vs. sunitinib | Phase 3 |
| Rini et al., 2019 (IMmotion 151) [13] | bevacizumab + atezolizumab vs. sunitinib | Phase 3 |
| Motzer et al., 2019 (JAVELIN Renal 101) [14] | axitinib + avelumab vs. sunitinib | Phase 3 |
| Rini et al., 2019 (KEYNOTE-426) [13] | axitinib + pembrolizumab vs. sunitinib | Phase 3 |
| Choueiri et al., 2021 (CheckMate 9ER) [16] | nivolumab + cabozantinib vs. sunitinib | Phase 3 |
| Motzer et al., 2021 (CLEAR) [15] | lenvatinib + pembrolizumab vs. lenvatinib + everolimus vs. sunitinib | Phase 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kathuria-Prakash, N.; Drolen, C.; Hannigan, C.A.; Drakaki, A. Immunotherapy and Metastatic Renal Cell Carcinoma: A Review of New Treatment Approaches. Life 2022, 12, 24. https://doi.org/10.3390/life12010024
Kathuria-Prakash N, Drolen C, Hannigan CA, Drakaki A. Immunotherapy and Metastatic Renal Cell Carcinoma: A Review of New Treatment Approaches. Life. 2022; 12(1):24. https://doi.org/10.3390/life12010024
Chicago/Turabian StyleKathuria-Prakash, Nikhita, Claire Drolen, Christopher A. Hannigan, and Alexandra Drakaki. 2022. "Immunotherapy and Metastatic Renal Cell Carcinoma: A Review of New Treatment Approaches" Life 12, no. 1: 24. https://doi.org/10.3390/life12010024
APA StyleKathuria-Prakash, N., Drolen, C., Hannigan, C. A., & Drakaki, A. (2022). Immunotherapy and Metastatic Renal Cell Carcinoma: A Review of New Treatment Approaches. Life, 12(1), 24. https://doi.org/10.3390/life12010024







