Neurological Complications of Biological Treatment of Psoriasis
Abstract
1. Introduction
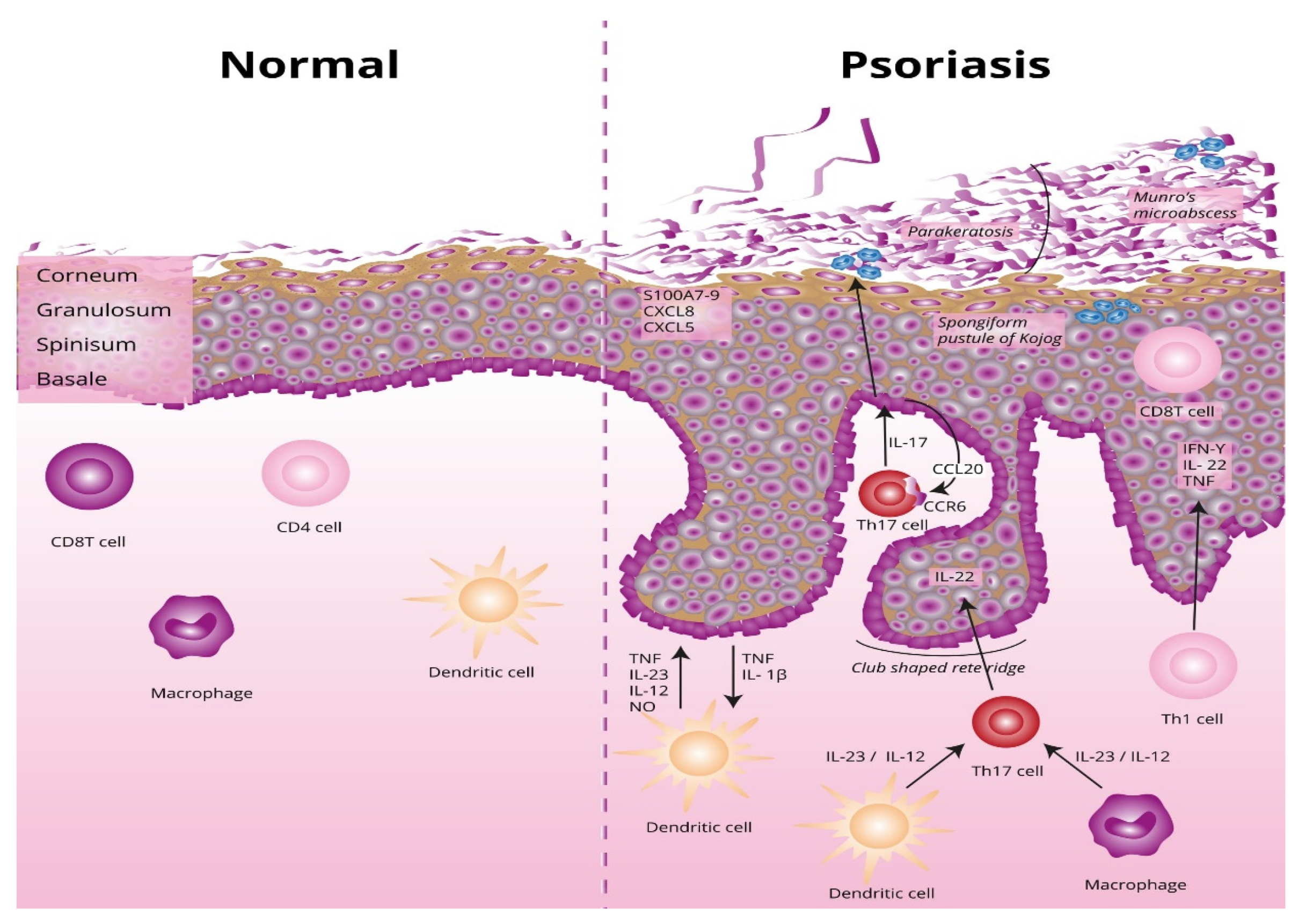
2. Etiopathogenesis of Psoriasis
2.1. Parakeratosis
2.2. Factors Precipitating the Development of Psoriasis and Stimulating the Development of Changes
2.2.1. Genetic Factors
2.2.2. Environmental Factors
2.2.3. Stress
2.2.4. Pharmacotherapy of Comorbidities
2.2.5. Infections
2.2.6. Nicotinism and Alcohol Consumption
3. Biological Drugs Used in the Treatment of Psoriasis
4. Connections between Psoriasis and the Nervous System
5. Neurological Complications and Adverse Reactions of the Biological Treatment of Psoriasis
5.1. TNF-Alpha Inhibitors
5.1.1. Demyelinating Diseases of the CNS and the Spinal Cord
5.1.2. Optic Neuritis
| Test | Results |
|---|---|
| Neurological test | Motor disorder as the neuropathy that develops is predominantly motor in nature |
| Electromyography | Demyelination |
| Cerebrospinal fluid testing | Often increased total protein concentration |
| Nerve biopsy | Demyelination |
| Peripheral nerve ultrasound | Nerve cross-sectional areas in nerves responsible for a given area of the body |
5.1.3. Peripheral Neuropathy
5.1.4. Facial Palsy
5.1.5. Myasthenia Gravis
5.2. Ustekinumab, an IL-12 and IL-23 Inhibitor
5.3. IL-23 Inhibitors
5.4. IL-17 Inhibitors
5.5. Abatacept, a T-Lymphocyte Inhibitor
6. Possible Explanations of the Mechanism Leading to Complications, Including the Connection between Psoriasis and the Nervous System
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Michalek, I.M.; Loring, B.; John, S. A Systematic Review of Worldwide Epidemiology of Psoriasis. J. Eur. Acad. Dermatol. Venereol. 2016, 31, 205–212. [Google Scholar] [CrossRef]
- Egeberg, A.; See, K.; Garrelts, A.; Burge, R. Epidemiology of Psoriasis in Hard-to-Treat Body Locations: Data from the Danish Skin Cohort. BMC Dermatol. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zuo, J.; Tang, W. Phosphodiesterase-4 Inhibitors for the Treatment of Inflammatory Diseases. Front. Pharmacol. 2018, 9, 1048. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Deng, X.; Xie, W.; Li, B.; Zhang, Z. Clinical Characteristics of Psoriatic Arthritis in Chinese Patients: A Cross-Sectional Study. Rheumatol. Ther. 2021, 8, 1845–1857. [Google Scholar] [CrossRef] [PubMed]
- Passante, M.; Dastoli, S.; Nisticò, S.P.; Bennardo, L.; Patruno, C. Effectiveness of Brodalumab in Acrodermatitis Continua of Hallopeau: A Case Report. Dermatol. Ther. 2019, 33, e13170. [Google Scholar] [CrossRef]
- Pittam, B.; Gupta, S.; Harrison, N.L.; Robertson, S.; Hughes, D.M.; Zhao, S.S. Prevalence of Extra-Articular Manifestations in Psoriatic Arthritis: A Systematic Review and Meta-Analysis. Rheumatology 2020, 59, 2199–2206. [Google Scholar] [CrossRef]
- Chandran, V.; Barrett, J.; Schentag, C.T.; Farewell, V.T.; Gladman, D.D. Axial Psoriatic Arthritis: Update on a Long-Term Prospective Study. J. Rheumatol. 2009, 36, 2744–2750. [Google Scholar] [CrossRef] [PubMed]
- Slobodin, G.; Rosner, I.; Rozenbaum, M.; Boulman, N.; Kessel, A.; Toubi, E. Psoriatic Arthropathy: Where Now? Isr. Med. Assoc. J. 2009, 1, 430–434. [Google Scholar]
- Swindell, W.R.; Xing, X.; Stuart, P.E.; Chen, C.S.; Aphale, A.; Nair, R.P.; Voorhees, J.J.; Elder, J.T.; Johnston, A.; Gudjonsson, J.E. Heterogeneity of Inflammatory and Cytokine Networks in Chronic Plaque Psoriasis. PLoS ONE 2012, 7, e34594. [Google Scholar] [CrossRef] [PubMed]
- Biswas, A. Cornoid Lamellation Revisited: Apropos of Porokeratosis with Emphasis on Unusual Clinicopathological Variants. Am. J. Dermatopathol. 2015, 37, 145–155. [Google Scholar] [CrossRef]
- Fischer, H.; Buchberger, M.; Napirei, M.; Tschachler, E.; Eckhart, L. Inactivation of DNase1L2 and DNase2 in Keratinocytes Suppresses DNA Degradation during Epidermal Cornification and Results in Constitutive Parakeratosis. Sci. Rep. 2017, 7, 6433. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, K.; Okada, Y. The Current Landscape of Psoriasis Genetics in 2020. J. Dermatol. Sci. 2020, 99, 2–8. [Google Scholar] [CrossRef]
- Membrive Jiménez, C.; Pérez Ramírez, C.; Sánchez Martín, A.; Vieira Maroun, S.; Arias Santiago, S.A.; Ramírez Tortosa, M.D.C.; Jiménez Morales, A. Influence of Genetic Polymorphisms on Response to Biologics in Moderate-to-Severe Psoriasis. J. Pers. Med. 2021, 11, 293. [Google Scholar] [CrossRef]
- Caputo, V.; Strafella, C.; Termine, A.; Dattola, A.; Mazzilli, S.; Lanna, C.; Cosio, T.; Campione, E.; Novelli, G.; Giardina, E.; et al. Overview of the Molecular Determinants Contributing to the Expression of Psoriasis and Psoriatic Arthritis Phenotypes. J. Cell Mol. Med. 2020, 24, 13554–13563. [Google Scholar] [CrossRef] [PubMed]
- Xie, W.; Huang, H.; Deng, X.; Gao, D.; Zhang, Z. Modifiable Lifestyle and Environmental Factors Associated with Onset of Psoriatic Arthritis in Patients with Psoriasis: A Systematic Review and Meta-Analysis of Observational Studies. J. Am. Acad. Dermatol. 2020, 84, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T. Similarity and Difference between Palmoplantar Pustulosis and Pustular Psoriasis. J. Dermatol. 2021, 48, 750–760. [Google Scholar] [CrossRef] [PubMed]
- Torales, J.; Echeverría, C.; Barrios, I.; García, O.; O′Higgins, M.; Castaldelli-Maia, J.M.; Jafferany, M. Psycho-Dermatological Mechanisms of Psoriasis. Dermatol. Ther. 2020, 33, e13827. [Google Scholar] [CrossRef]
- Lim, D.S.; Bewley, A.; Oon, H. Psychological Profile of Patients with Psoriasis. Ann. Acad. Med. Singap. 2018, 47, 516–522. [Google Scholar]
- Lakuta, P.; Marcinkiewicz, K.; Bergler-Czop, B.; Brzezińska-Wcisło, L.; Słomian, A. Associations between Site of Skin Lesions and Depression, Social Anxiety, Body-Related Emotions and Feelings of Stigmatization in Psoriasis Patients. Postepy Dermatol. Alergol. 2018, 35, 60–66. [Google Scholar] [CrossRef]
- Rousset, L.; Halioua, B. Stress and Psoriasis. Int. J. Dermatol. 2018, 57, 1165–1172. [Google Scholar] [CrossRef]
- Snast, I.; Reiter, O.; Atzmony, L.; Leshem, Y.; Hodak, E.; Mimouni, D.; Pavlovsky, L. Psychological Stress and Psoriasis: A Systematic Review and Meta-Analysis. Br. J. Dermatol. 2018, 178, 1044–1055. [Google Scholar] [CrossRef] [PubMed]
- Rao, T.S.S.; Basavaraj, K.H.; Das, K. Psychosomatic Paradigms in Psoriasis: Psoriasis, Stress and Mental Health. Indian J. Psychiatry 2013, 55, 313–315. [Google Scholar] [CrossRef]
- Balak, D.M.; Hajdarbegovic, E. Drug-Induced Psoriasis: Clinical Perspectives. Psoriasis Targets Ther. 2017, 7, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Kingsmore, K.M.; Grammer, A.C.; Lipsky, P.E. Drug Repurposing to Improve Treatment of Rheumatic Autoimmune Inflammatory Diseases. Nat. Rev. Rheumatol. 2019, 16, 32–52. [Google Scholar] [CrossRef]
- Kaushik, S.B.; Lebwohl, M.G. Psoriasis: Which Therapy for Which Patient: Focus on Special Populations and Chronic Infections. J. Am. Acad. Dermatol. 2019, 80, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-L.; Ku, Y.-H.; Yip, H.-T.; Wei, J.C.-C. Tonsillectomy and the Subsequent Risk of Psoriasis: A Nationwide Population-Based Cohort Study. J. Am. Acad. Dermatol. 2021, 85, 1493–1502. [Google Scholar] [CrossRef] [PubMed]
- Groot, J.; Blegvad, C.; Andersen, A.N.; Zachariae, C.; Jarløv, J.; Skov, L. Presence of Streptococci and Frequent Tonsillitis among Adolescents with Psoriasis. Br. J. Dermatol. 2020, 184, 758–759. [Google Scholar] [CrossRef]
- Constantin, M.-M.; Bucur, S.; Mutu, C.-C.; Poenaru, E.; Olteanu, R.; Ionescu, R.; Nicolescu, A.; Furtunescu, F.; Constantin, T. The Impact of Smoking on Psoriasis Patients with Biological Therapies in a Bucharest Hospital. J. Pers. Med. 2021, 11, 752. [Google Scholar] [CrossRef]
- Dey, M.; Hughes, D.M.; Zhao, S.S. Comment on: The Impact of Smoking on Prevalence of Psoriasis and Psoriatic Arthritis. Rheumatology 2021, 60, e26. [Google Scholar] [CrossRef]
- Salihbegovic, E.M.; Kurtalic, N.; Omerkic, E. Smoking Cigarettes and Consuming Alcohol in Patients with Psoriasis. Mater. Socio-Med. 2021, 33, 30. [Google Scholar] [CrossRef]
- Szentkereszty-Kovács, Z.; Gáspár, K.; Szegedi, A.; Kemény, L.; Kovács, D.; Törőcsik, D. Alcohol in Psoriasis—From Bench to Bedside. Int. J. Mol. Sci. 2021, 22, 4987. [Google Scholar] [CrossRef] [PubMed]
- Skandar, I.Y.; Lunt, M.; Thorneloe, R.J.; Cordingley, L.; Griffiths, C.E.; Ashcroft, D.M.; British Association of Dermatologists Biologics, Immunomodulators Register, Psoriasis Stratification to Optimise Relevant Therapy Study Groups. Alcohol Abuse Associated with Poor Response to Systemic Therapies for Psoriasis: Findings from a Prospective Multicentre Cohort Study. Br. J. Dermatol. 2021, 185, 952–960. [Google Scholar]
- Farkas, Á.; Kemény, L. Psoriasis and Alcohol: Is Cutaneous Ethanol One of the Missing Links? Br. J. Dermatol. 2010, 162, 711–716. [Google Scholar] [CrossRef]
- Reich, A.; Adamski, Z.; Chodorowska, G.; Kaszuba, A.; Krasowska, D.; Lesiak, A.; Maj, J.; Narbutt, J.; Osmola-Mańkowska, A.J.; Owczarczyk-Saczonek, A.; et al. Psoriasis. Diagnostic and Therapeutic Recommendations of the Polish Dermatological Society. Part 1. Prz. Dermatol. 2020, 107, 92–108. [Google Scholar] [CrossRef]
- Dattola, A.; Silvestri, M.; Bennardo, L.; Passante, M.; Rizzuto, F.; Dastoli, S.; Patruno, C.; Bianchi, L.; Nisticò, S.P. A Novel Vehicle for the Treatment of Psoriasis. Dermatol. Ther. 2020, 33, e13185. [Google Scholar] [CrossRef]
- Reich, A.; Adamski, Z.; Chodorowska, G.; Kaszuba, A.; Krasowska, D.; Lesiak, A.; Maj, J.; Narbutt, J.; Osmola-Mańkowska, A.J.; Owczarczyk-Saczonek, A.; et al. Psoriasis. Diagnostic and Therapeutic Recommendations of the Polish Dermatological Society. Part 2. Prz. Dermatol. 2020, 107, 110–137. [Google Scholar] [CrossRef]
- Rendon, A.; Schäkel, K. Psoriasis Pathogenesis and Treatment. Int. J. Mol. Sci. 2019, 20, 1475. [Google Scholar] [CrossRef]
- Danielsen, K.; Olsen, A.; Wilsgaard, T.; Furberg, A.-S. Is the Prevalence of Psoriasis Increasing? A 30-year Follow-up of a Population-Based Cohort. Br. J. Dermatol. 2013, 168, 1303–1310. [Google Scholar] [CrossRef]
- Bunte, K.; Beikler, T. Th17 Cells and the IL-23/IL-17 Axis in the Pathogenesis of Periodontitis and Immune-Mediated Inflammatory Diseases. Int. J. Mol. Sci. 2019, 20, 3394. [Google Scholar] [CrossRef]
- Jeon, C.; Sekhon, S.; Yan, D.; Afifi, L.; Nakamura, M.; Bhutani, T. Monoclonal Antibodies Inhibiting IL-12, -23, and -17 for the Treatment of Psoriasis. Hum. Vaccines Immunother. 2017, 13, 2247–2259. [Google Scholar] [CrossRef]
- Dattola, A.; Silvestri, M.; Tamburi, F.; Amoruso, G.F.; Bennardo, L.; Nisticò, S.P. Emerging Role of Anti-IL23 in the Treatment of Psoriasis: When Humanized Is very Promising. Dermatol. Ther. 2020, 33, e14504. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, L.; Chen, Y.; Ogg, G. Role of Regulatory T Cells in Psoriasis Pathogenesis and Treatment. Br. J. Dermatol. 2020, 184, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Noack, M.; Miossec, P. Importance of Lymphocyte-Stromal Cell Interactions in Autoimmune and Inflammatory Rheumatic Diseases. Nat. Rev. Rheumatol. 2021, 17, 550–564. [Google Scholar] [CrossRef] [PubMed]
- Raaby, L.; Ahlehoff, O.; de Thurah, A. Psoriasis and Cardiovascular Events: Updating the Evidence. Arch. Dermatol. Res. 2017, 309, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Guido, N.; Cices, A.; Ibler, E.; Huynh, T.; Majewski, S.; Sable, K.; Rangel, S.M.; West, D.P.; Laumann, A.E.; Nardone, B. Multiple Sclerosis Association with Psoriasis: A Large U.S. Population, Single Center, Retrospective Cross-Sectional Study. J. Eur. Acad. Dermatol. Venereol. 2017, 31, e397–e398. [Google Scholar] [CrossRef]
- Ong, M.-S.; Kohane, I.S.; Cai, T.; Gorman, M.P.; Mandl, K.D. Population-Level Evidence for an Autoimmune Etiology of Epilepsy. JAMA Neurol. 2014, 71, 569–574. [Google Scholar] [CrossRef]
- Galili, E.; Barzilai, A.; Shreberk-Hassidim, R.; Merdler, I.; Caspi, T.; Astman, N. Neuropsychiatric Comorbidity among Adolescents with Psoriasis. Br. J. Dermatol. 2018, 178, 910–916. [Google Scholar] [CrossRef]
- Lee, J.H.; Han, K.; Gee, H.Y. The Incidence Rates and Risk Factors of Parkinson Disease in Patients with Psoriasis: A Nationwide Population-Based Cohort Study. J. Am. Acad. Dermatol. 2020, 83, 1688–1695. [Google Scholar] [CrossRef]
- Huang, H.; Ran, H.; Liu, X.; Yu, L.; Qiu, L.; Lin, Z.; Ou, C.; Lu, Y.; Yang, W.; Liu, W. Leflunomide Ameliorates Experimental Autoimmune Myasthenia Gravis by Regulating Humoral and Cellular Immune Responses. Int. Immunopharmacol. 2021, 93, 107434. [Google Scholar] [CrossRef]
- Amanat, M.; Salehi, M.; Rezaei, N. Neurological and Psychiatric Disorders in Psoriasis. Rev. Neurosci. 2018, 29, 805–813. [Google Scholar] [CrossRef]
- Agah, E.; Nafissi, S.; Saleh, F.; Sarraf, P.; Tafakhori, A.; Mousavi, S.V.; Saghazadeh, A.; Sadr, M.; Sinaei, F.; Mohebbi, B.; et al. Investigating the Possible Association between NLRP3 Gene Polymorphisms and Myasthenia Gravis. Muscle Nerve 2021, 63, 730–736. [Google Scholar] [CrossRef]
- Bai, F.; Zheng, W.; Dong, Y.; Wang, J.; Garstka, M.A.; Li, R.; An, J.; Ma, H. Serum Levels of Adipokines and Cytokines in Psoriasis Patients: A Systematic Review and Meta-Analysis. Oncotarget 2018, 9, 1266–1278. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, K.; Friedman, B.A.; Larson, J.L.; Lauffer, B.E.; Goldstein, L.D.; Appling, L.L.; Hansen, D.V. Un-Tangling the Brain′s Neuroinflammatory and Neurodegenerative Transcriptional Responses. Nat. Commun. 2016, 7, 1–16. [Google Scholar]
- Neniskyte, U.; Vilalta, A.; Brown, G.C. Tumour Necrosis Factor Alpha-Induced Neuronal Loss Is Mediated by Microglial Phagocytosis. FEBS Lett. 2014, 588, 2952–2956. [Google Scholar] [CrossRef]
- Sheikh, M.H. Impact of Metabolic Disorders on the Structure, Function, and Immunological Integrity of the Blood-Brain Barrier. Ph.D. Thesis, Queen Mary University of London, London, UK, 2021. [Google Scholar]
- Zepp, J.; Wu, L.; Li, X. IL-17 Receptor Signaling and T helper 17-Mediated Autoimmune Demyelinating Disease. Trends Immunol. 2011, 32, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Nitsch, L.; Schneider, L.; Zimmermann, J.; Müller, M. Microglia-Derived Interleukin 23: A Crucial Cytokine in Alzheimer′s Disease? Front. Neurol. 2021, 12, 639353. [Google Scholar] [CrossRef]
- Charakterystyka Produktu Leczniczego: Certolizumab Pegol. Available online: https://www.ema.europa.eu/en/documents/product-information/cimzia-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Etanercept. Available online: https://www.ema.europa.eu/en/documents/product-information/enbrel-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Adalimumab. Available online: https://www.ema.europa.eu/en/documents/product-information/humira-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Infliximab. Available online: https://www.ema.europa.eu/en/documents/product-information/remicade-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Golimumab. Available online: https://www.ema.europa.eu/en/documents/product-information/simponi-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Ustekinumab. Available online: https://www.ema.europa.eu/en/documents/product-information/stelara-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Tildrakizumab. Available online: https://www.ema.europa.eu/en/documents/product-information/ilumetri-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Risankizumab. Available online: https://www.ema.europa.eu/en/documents/product-information/skyrizi-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Guselkumab. Available online: https://www.ema.europa.eu/en/documents/product-information/tremfya-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Secukinumab. Available online: https://www.ema.europa.eu/en/documents/product-information/cosentyx-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Brodalumab. Available online: https://www.ema.europa.eu/en/documents/product-information/kyntheum-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Ixekizumab. Available online: https://www.ema.europa.eu/en/documents/product-information/taltz-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Charakterystyka Produktu Leczniczego: Abatacept. Available online: https://www.ema.europa.eu/en/documents/product-information/orencia-epar-product-information_pl.pdf (accessed on 28 December 2021).
- Mocci, G.; Marzo, M.; Papa, A.; Armuzzi, A.; Guidi, L. Dermatological Adverse Reactions during Anti-TNF Treatments: Focus on Inflammatory Bowel Disease. J. Crohn′s Colitis 2013, 7, 769–779. [Google Scholar] [CrossRef]
- Broyles, A.D.; Banerji, A.; Barmettler, S.; Biggs, C.M.; Blumenthal, K.; Brennan, P.J.; Breslow, R.G.; Brockow, K.; Buchheit, K.M.; Cahill, K.N.; et al. Practical Guidance for the Evaluation and Management of Drug Hypersensitivity: Specific Drugs. J. Allergy Clin. Immunol. Pract. 2020, 8, S16–S116. [Google Scholar] [CrossRef]
- Gerriets, V.; Khaddour, K. Tumor Necrosis Factor (TNF) Inhibitors; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Jang, D.-I.; Lee, A.-H.; Shin, H.-Y.; Song, H.-R.; Park, J.-H.; Kang, T.-B.; Lee, S.-R.; Yang, S.-H. The Role of Tumor Necrosis Factor Alpha (TNF-α) in Autoimmune Disease and Current TNF-α Inhibitors in Therapeutics. Int. J. Mol. Sci. 2021, 22, 2719. [Google Scholar] [CrossRef]
- Deepak, P.; Stobaugh, D.J.; Sherid, M.; Sifuentes, H.; Ehrenpreis, E.D. Neurological Events with Tumour Necrosis Factor Alpha Inhibitors Reported to the Food and Drug Administration Adverse Event Reporting System. Aliment. Pharmacol. Ther. 2013, 38, 388–396. [Google Scholar] [CrossRef]
- Seror, R.; Richez, C.; Sordet, C.; Rist, S.; Gossec, L.; Direz, G.; Houvenagel, E.; Berthelot, J.-M.; Pagnoux, C.; Dernis, E.; et al. Pattern of Demyelination Occurring During Anti-TNF-α Therapy: A French National Survey. Rheumatology 2013, 52, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, G.; Ben-Zvi, I.; Furie, N.; Grossman, C. Clinical Significance of Positive Anti-Neutrophil Cytoplasmic Antibodies without Evidence of Anti-Neutrophil Cytoplasmic Antibodies-Associated Vasculitis. Int. J. Rheum. Dis. 2019, 22, 940–945. [Google Scholar] [CrossRef]
- Nurmohamed, M.; Bao, Y.; Signorovitch, J.; Trahey, A.; Mulani, P.; Furst, D.E. Longer Durations of Antitumour Necrosis Factor Treatment Are Associated with Reduced Risk of Cardiovascular Events in Patients with Rheumatoid Arthritis. RMD Open 2015, 1, e000080. [Google Scholar] [CrossRef]
- Kaushik, S.B.; Lebwohl, M.G. Psoriasis: Which Therapy for Which Patient: Psoriasis Comorbidities and Preferred Systemic Agents. J. Am. Acad. Dermatol. 2019, 80, 27–40. [Google Scholar] [CrossRef]
- Findeisen, K.E.; Sewell, J.; Ostor, A.J. Biological Therapies for Rheumatoid Arthritis: An Overview for the Clinician. Biol. Targets Ther. 2021, 15, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Kemanetzoglou, E.; Andreadou, E. CNS Demyelination with TNF-α Blockers. Curr. Neurol. Neurosci. Rep. 2017, 17, 36. [Google Scholar] [CrossRef]
- Silfvast-Kaiser, A.S.; Homan, K.B.; Mansouri, B. A Narrative Review of Psoriasis and Multiple Sclerosis: Links and Risks. Psoriasis Targets Ther. 2019, 9, 81–90. [Google Scholar] [CrossRef]
- Alexandre, B.; Vandermeeren, Y.; Dewit, O.; Moreels, T.; de Boer, N.; Dhar, A.; Ziady, C.; Shitrit, A.B.-G.; Steinwurz, F.; Jojić, N.; et al. Optic Neuritis Associated or Not with TNF Antagonists in Patients with Inflammatory Bowel Disease. J. Crohn’s Colitis 2016, 10, 541–548. [Google Scholar] [CrossRef]
- Tsouni, P.; Bill, O.; Truffert, A.; Liaudat, C.; Ochsner, F.; Steck, A.J.; Kuntzer, T. Anti-TNFalpha Medications and Neuropathy. J. Peripher. Nerv. Syst. 2015, 20, 397–402. [Google Scholar] [CrossRef]
- Lozeron, P.; Denier, C.; Lacroix, C.; Adams, D. Long-Term Course of Demyelinating Neuropathies Occurring During Tumor Necrosis Factor-α–Blocker Therapy. Arch. Neurol. 2009, 66, 490–497. [Google Scholar] [CrossRef]
- Gisondi, P.; Fostini, A.C.; Fossà, I.; Girolomoni, G.; Targher, G. Psoriasis and the Metabolic Syndrome. Clin. Dermatol. 2017, 36, 21–28. [Google Scholar] [CrossRef]
- Shavit, E.; Dreiher, J.; Freud, T.; Halevy, S.; Vinker, S.; Cohen, A. Psychiatric Comorbidities in 3207 Patients with Hidradenitis Suppurativa. J. Eur. Acad. Dermatol. Venereol. 2014, 29, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Pintos, L.M.R.; Villegas-Rivera, G.; Rodríguez-Carrizalez, A.D.; Miranda-Díaz, A.G.; Muñoz, E.G.C. Diabetic Polyneuropathy in Type 2 Diabetes Mellitus: Inflammation, Oxidative Stress, and Mitochondrial Function. J. Diabetes Res. 2016, 2016, 3425617. [Google Scholar] [CrossRef]
- Lehmann, H.C.; Wunderlich, G.; Fink, G.R.; Sommer, C. Diagnosis of Peripheral Neuropathy. Neurol. Res. Pract. 2020, 2, 1–7. [Google Scholar] [CrossRef]
- Yao, A.; Chan, H.; MacDonell, R.A.; Shuey, N.; Khong, J.J. Bilateral Facial Nerve Palsies Secondary to Chronic Inflammatory Demyelinating Polyneuropathy Following Adalimumab Treatment. Clin. Neurol. Neurosurg. 2018, 164, 64–66. [Google Scholar] [CrossRef] [PubMed]
- Farukhi, F.I.; Bollinger, K.; Ruggieri, P.; Lee, M.S. Infliximab-Associated Third Nerve Palsy. Arch. Ophthalmol. 2006, 124, 1055. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rowin, J. Etanercept Treatment in Myasthenia Gravis. Ann. N. Y. Acad. Sci. 2008, 1132, 300–304. [Google Scholar] [CrossRef]
- Li, X.L.; Li, H.; Zhang, M.; Xu, H.; Yue, L.T.; Zhang, X.X.; Duan, R.S. Exosomes Derived from Atorvas-Tatin-Modified Bone Marrow Dendritic Cells Ameliorate Experimental Autoimmune Myasthenia Gravis by up-Regulated Levels of IDO/Treg and Partly Dependent on FasL/Fas Pathway. J. Neuroinflamm. 2016, 13, 8. [Google Scholar] [CrossRef]
- Bruzzese, V.; Marrese, C.; Scolieri, P.; Hassan, C.; Lorenzetti, R.; Zullo, A. Myasthenia Gravis Onset during Rheumatic Disease: A New Paradoxical Effect of Anti-TNF Alpha Therapy? Int. J. Rheum. Dis. 2014, 18, 375–376. [Google Scholar] [CrossRef]
- Fee, D.B.; Kasarskis, E.J. Myasthenia Gravis Associated with Etanercept Therapy. Muscle Nerve 2009, 39, 866–870. [Google Scholar] [CrossRef]
- Sandborn, W.J.; Gasink, C.; Gao, L.-L.; Blank, M.A.; Johanns, J.; Guzzo, C.; Sands, B.E.; Hanauer, S.B.; Targan, S.; Rutgeerts, P.; et al. Ustekinumab Induction and Maintenance Therapy in Refractory Crohn′s Disease. N. Engl. J. Med. 2012, 367, 1519–1528. [Google Scholar] [CrossRef]
- Gratton, D.; Szapary, P.; Goyal, K.; Fakharzadeh, S.; Germain, V.; Saltiel, P. Reversible Posterior Leukoencephalopathy Syndrome in a Patient Treated with Ustekinumab: Case Report and Review of the Literature. Arch. Dermatol. 2011, 147, 1197–1202. [Google Scholar] [CrossRef]
- Mishra, A. Posterior Reversible Encephalopathy Syndrome and Tonic Clonic Seizures: Case Report. Reactions 2018, 1693, 492–517. [Google Scholar]
- Dickson, L.; Menter, A. Reversible Posterior Leukoencephalopathy Syndrome (RPLS) in a Psoriasis Patient Treated With Ustekinumab. J. Drugs Dermatol. 2017, 16, 177–179. [Google Scholar]
- Fischer, M.; Schmutzhard, E. Posterior Reversible Encephalopathy Syndrome. J. Neurol. 2017, 264, 1608–1616. [Google Scholar] [CrossRef]
- Granata, G.; Greco, A.; Iannella, G.; Granata, M.; Manno, A.; Savastano, E.; Magliulo, G. Posterior Reversible Encephalopathy Syndrome—Insight into Pathogenesis, Clinical Variants and Treatment Approaches. Autoimmun. Rev. 2015, 14, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Nicocia, G.; Bonanno, C.; Lupica, A.; Toscano, A.; Rodolico, C. Myasthenia Gravis after Etanercept and Ustekinumab Treatment for Psoriatic Arthritis: A Case Report. Neuromuscul. Disord. 2020, 30, 246–249. [Google Scholar] [CrossRef]
- Beck, K.M.; Sanchez, I.M.; Yang, E.J.; Liao, W. Profile of Tildrakizumab-Asmn in the Treatment of Moderate-to-Severe Plaque Psoriasis: Evidence to Date. Psoriasis Targets Ther. 2018, 8, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Megna, M.; Fabbrocini, G.; Ruggiero, A.; Cinelli, E. Efficacy and Safety of Risankizumab in Psoriasis Patients Who Failed Anti-IL-17, Anti-12/23 and/or Anti IL-23: Preliminary Data of a Real-Life 16-Week Retrospective Study. Dermatol. Ther. 2020, 33, e14144. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.; Yang, E.J.; Myers, B.; Liao, W. Clinical Evaluation of Risankizumab-Rzaa in the Treatment of Plaque Psoriasis. J. Inflamm. Res. 2020, 13, 53–60. [Google Scholar] [CrossRef]
- Reich, K.; Armstrong, A.W.; Langley, R.G.; Flavin, S.; Randazzo, B.; Li, S.; Hsu, M.-C.; Branigan, P.; Blauvelt, A. Guselkumab Versus Secukinumab for the Treatment of Moderate-to-Severe Psoriasis (ECLIPSE): Results from a Phase 3, Randomised Controlled Trial. Lancet 2019, 394, 831–839. [Google Scholar] [CrossRef]
- Hamadah, I.; Chisti, M.A. Axonal Sensorimotor Polyneuropathy after Starting Guselkumab. J. Dermatol. Treat. 2021, 1–7. [Google Scholar] [CrossRef]
- Schwensen, J.F.; Clemmensen, A.; Sand, C.; Gniadecki, R.; Skov, L.; Zachariae, C.; Iversen, L.; Rasmussen, M.; Thomsen, S.F. Effectiveness and Safety of Secukinumab in 69 Patients with Moderate to Severe Plaque Psoriasis: A Retrospective Multicenter Study. Dermatol. Ther. 2017, 30, e12550. [Google Scholar] [CrossRef] [PubMed]
- Golbari, N.M.; Basehore, B.M.; Zito, P.M. Brodalumab; StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK470324/ (accessed on 28 December 2021).
- Gordon, K.B.; Blauvelt, A.; Papp, K.A.; Langley, R.G.; Luger, T.; Ohtsuki, M.; Reich, K.; Amato, D.; Ball, S.G.; Braun, D.K.; et al. Phase 3 Trials of Ixekizumab in Moderate-to-Severe Plaque Psoriasis. N. Engl. J. Med. 2016, 375, 345–356. [Google Scholar] [CrossRef]
- Sumida, T.; Azuma, N.; Moriyama, M.; Takahashi, H.; Asashima, H.; Honda, F.; Tsuboi, H. Clinical Practice Guideline for Sjögren′s Syndrome. Mod. Rheumatol. 2017, 28, 383–408. [Google Scholar] [CrossRef]
- Noisette, A.; Hochberg, M.C. Abatacept for the Treatment of Adults with Psoriatic Arthritis: Patient Selection and Perspectives. Psoriasis Targets Ther. 2018, 8, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Sm, A.-M.; Alqurashi, H.A.; Al-Salmi, G.; Al-Muhaizea, M.A.; Al-Mayouf, S.M. Biologic Therapy-Related Demyelinating Peripheral Neuropathy in a Child with Juvenile Idiopathic Arthritis. Arch. Pharm. Pharm. Sci. 2017, 2, 020–022. [Google Scholar] [CrossRef]
- Probert, L. TNF and Its Receptors in the CNS: The Essential, the Desirable and the Deleterious Effects. Neuroscience 2015, 302, 2–22. [Google Scholar] [CrossRef]
- Kruglov, A.A.; Lampropoulou, V.; Fillatreau, S.; Nedospasov, S.A. Pathogenic and Protective Functions of TNF in Neuroinflammation Are Defined by Its Expression in T Lymphocytes and Myeloid Cells. J. Immunol. 2011, 187, 5660–5670. [Google Scholar] [CrossRef]
- Brambilla, R.; Ashbaugh, J.J.; Magliozzi, R.; Dellarole, A.; Karmally, S.; Szymkowski, D.; Bethea, J.R. Inhibition of Soluble Tumour Necrosis Factor Is Therapeutic in Experimental Autoimmune Encephalomyelitis and Promotes Axon Preservation and Remyelination. Brain 2011, 134, 2736–2754. [Google Scholar] [CrossRef]
- Chang, R.; Knox, J.; Chang, J.; DerBedrossian, A.; Vasilevko, V.; Cribbs, D.; Boado, R.J.; Pardridge, W.M.; Sumbria, R.K. Blood–Brain Barrier Penetrating Biologic TNF-α Inhibitor for Alzheimer′s Disease. Mol. Pharm. 2017, 14, 2340–2349. [Google Scholar] [CrossRef] [PubMed]
- Kaltsonoudis, E.; Voulgari, P.V.; Konitsiotis, S.; Drosos, A.A. Demyelination and Other Neurological Adverse Events after Anti-TNF Therapy. Autoimmun. Rev. 2013, 13, 54–58. [Google Scholar] [CrossRef] [PubMed]
| Group | Marketed Formulations | Biological Influence of the Drug |
|---|---|---|
| TNF-alpha inhibitors |
| Patients with psoriasis exhibit an excessive production of TNF-alpha in the skin as well as the joints. This is a proinflammatory cytokine that acts through by stimulating the release of numerous proinflammatory factors, which ultimately leads to inflammatory infiltration in the area of the skin. Through the inhibition of this cytokine, the inflammation in the skin area is reduced [39]. |
| IL-12 and IL-23 inhibitors |
| IL-12 and IL-23 are constructed from a common p40 subunit, which ustekinumab acts against. IL-12 stimulates NK (natural killer) cells and differentiation of CD4+ T cells towards the Th1 phenotype. Ustekinumab, if it is unable to attach to IL-12 or IL-23, which are attached to the IL-12Rβ1 receptors on the cell surface, does not affect complement activity and is not involved in antibody-mediated cytotoxicity of the receptor cells. Ustekinumab can exert its clinical effects in psoriasis and psoriatic arthritis by disrupting the Th1 and Th17 cytokine pathways that play a key role in the pathology of these diseases [40]. |
| IL-23 inhibitors |
| Recent studies indicated that IL-23 is the most important cytokine in the pathogenesis of psoriasis, as it induces the differentiation of naïve T lymphocytes towards the Th17 phenotype and thus to the formation of psoriatic plaque. The newest p19 inhibitor of IL-23 is risankizumab, which has a good safety profile, less frequent use, and suitable efficacy in severe psoriasis [41]. |
| IL-17 inhibitors |
| IL-17 is a cytokine that causes an increase in the expression of factors such as TNF-alpha, stimulating the development of inflammatory infiltration. Blocking IL-17 causes a significant reduction in infiltration [40]. |
| T-lymphocyte inhibitors |
| In the area of skin changes, there are numerous T-lymphocytes with impaired function. This causes the stimulation of an improper inflammatory reaction [42]. The cytotoxic activity of abatacept on T-lymphocytes causes a decrease in their population, resulting in a reduction of the inflammation in the area of psoriatic changes [43]. |
| Cytokine | Impact on Nerve Tissue |
|---|---|
| TNFα | TNF-alpha receptors are present on the surface of neurons as well as astrocytes and microglia. The stimulation of these receptors causes the activation of cascades leading to cell apoptosis and changes as far as the expression of genes responsible for the survival of a cell [53]. The exposure of nerve tissue to a high concentration of this cytokine results in the decomposition of microglia and a loss of neurons [54], which can lead to neurodegenerative diseases. |
| IL-12 | The exposure of the nervous system to a high concentration of IL-12 may induce the development of neurodegenerative diseases by inducing neuron apoptosis and stimulation of the proliferation of astrocytes [55]. |
| IL-17 | A high concentration of this cytokine may cause the activation of the glia and the infiltration of the CNS by proinflammatory cells [56]. |
| IL-23 | A high concentration of this cytokine may cause the activation of the glia and the infiltration of the CNS by proinflammatory cells [57]. |
| Group | Marketed Formulations | Specific Neurological Complications or Side Effects | |||
|---|---|---|---|---|---|
| Very Often | Often | Seldom | Rarely | ||
| TNF-alpha inhibitors | Certolizumab pegol [58] | - | Headache (including migraine), sensory disturbance | Mental disorders (anxiety and mood disorders, peripheral neuropathies, dizziness, tremors | Convulsions, inflammation of the cranial nerve, impaired coordination or balance, multiple sclerosis, Guillain–Barré syndrome |
| Etanercept [59] | Headache, demyelinating polyneuropathy, and multifocal motor neuropathy | - | Cases of CNS demyelinating syndromes (e.g., multiple sclerosis) or limited demyelinating syndromes (e.g., optic neuritis and transverse myelitis); cases of peripheral demyelinating polyneuropathy, including Guillain–Barré syndrome, chronic inflammatory demyelinating polyneuropathy | - | |
| Adalimumab [60] | Headache | Mood changes, including depression and anxiety; insomnia; paraesthesia (including hypoesthesia); migraine compression of the nerve root | Stroke, muscle tremors, neuropathy | Multiple sclerosis, demyelinating disorders (e.g., optic neuritis, Guillain–Barré syndrome) | |
| Infliximab [61] | Headache | Depression, insomnia, vertigo and post-hypoesthesia, hypoesthesia, paresthesia | Amnesia, agitation, confusion, seizure, neuropathy | Sleepiness, nervousness. apathy, transverse myelitis, central nervous system demyelinating diseases (multiple sclerosis-like diseases and optic neuritis), peripheral demyelinating diseases (such as Guillain–Barré syndrome, chronic inflammatory demyelinating polyneuropathy, and multifocal motor neuropathy), cerebrovascular accidents in close temporal association with the infusion | |
| Golimumab [62] | - | Dizziness, headache, paresthesia | Depression, insomnia, dizziness, headache, paresthesia | Balance disorders, demyelinating diseases (central and peripheral nervous system), taste disturbances | |
| IL-12/23 inhibitors | Ustekinumab [63] | - | Dizziness, headache | Depression, facial nerve palsy | - |
| IL-23 inhibitors | Tildrakizumab [64] | - | Headache | - | - |
| Risankizumab [65] | - | Headache | - | ||
| Guselkumab [66] | - | Headache | - | - | |
| IL-17 inhibitors | Secukinumab [67] | - | Headache | - | |
| Brodalumab [68] | - | Headache | - | ||
| Ixekizumab [69] | - | - | - | - | |
| T-lymphocyte inhibitors | Abatacept [70] | - | Headache, dizziness | Depression, anxiety, sleep disturbances (including insomnia), migraines, paresthesia | - |
| Diagnostic Tool | Finding |
|---|---|
| Laboratory data | Hypomagnesemia |
| Lactate dehydrogenase ↑ | |
| Liver function parameters ↑ | |
| Creatinine ↑ | |
| Albumin ↓ | |
| Cerebrospinal fluid | Albumin ↑ |
| Albuminocytologic dissociation | |
| EEG | Diffuse theta slowing |
| Delta slowing | |
| Rhythmic delta activity | |
| Sharp-slow wave activity | |
| Periodic lateralizing epileptiform discharges | |
| Diffuse or focal (symmetric) slowing of background activities | |
| CT and MRI | Vasogenic edema |
| Watershed distribution | |
| Parieto-occipital pattern | |
| Frontal and temporal lobe involvement | |
| Subcortical white matter lesions | |
| Bilateral, frequently symmetric distribution | |
| Hyperintense T2-weighted and FLAIR sequences | |
| Iso-, hypo-, or hyperintense lesions on DWI | |
| Facultative contrast enhancement | |
| Microbleeds, intracerebral hemorrhage possible | |
| Increased or decreased ADC values depending on or indicating the (ir) reversibility of lesions | |
| Angiography | Vasoconstriction, vasospasm (diffuse or focal) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ożóg, M.K.; Grabarek, B.O.; Wierzbik-Strońska, M.; Świder, M. Neurological Complications of Biological Treatment of Psoriasis. Life 2022, 12, 118. https://doi.org/10.3390/life12010118
Ożóg MK, Grabarek BO, Wierzbik-Strońska M, Świder M. Neurological Complications of Biological Treatment of Psoriasis. Life. 2022; 12(1):118. https://doi.org/10.3390/life12010118
Chicago/Turabian StyleOżóg, Mateusz Kamil, Beniamin Oskar Grabarek, Magdalena Wierzbik-Strońska, and Magdalena Świder. 2022. "Neurological Complications of Biological Treatment of Psoriasis" Life 12, no. 1: 118. https://doi.org/10.3390/life12010118
APA StyleOżóg, M. K., Grabarek, B. O., Wierzbik-Strońska, M., & Świder, M. (2022). Neurological Complications of Biological Treatment of Psoriasis. Life, 12(1), 118. https://doi.org/10.3390/life12010118






