Inadvertent Detachment of Stent Retrievers during Mechanical Thrombectomy—A Clinical and Biomechanical Perspective
Abstract
:1. Introduction
2. Methods
2.1. Patient Analysis
Mechanical Thrombectomy
2.2. Laboratory Traction Load Test
Study Design
2.3. Phantom Study
Study Design
2.4. pRESET
2.5. Tigertreiver
3. Results
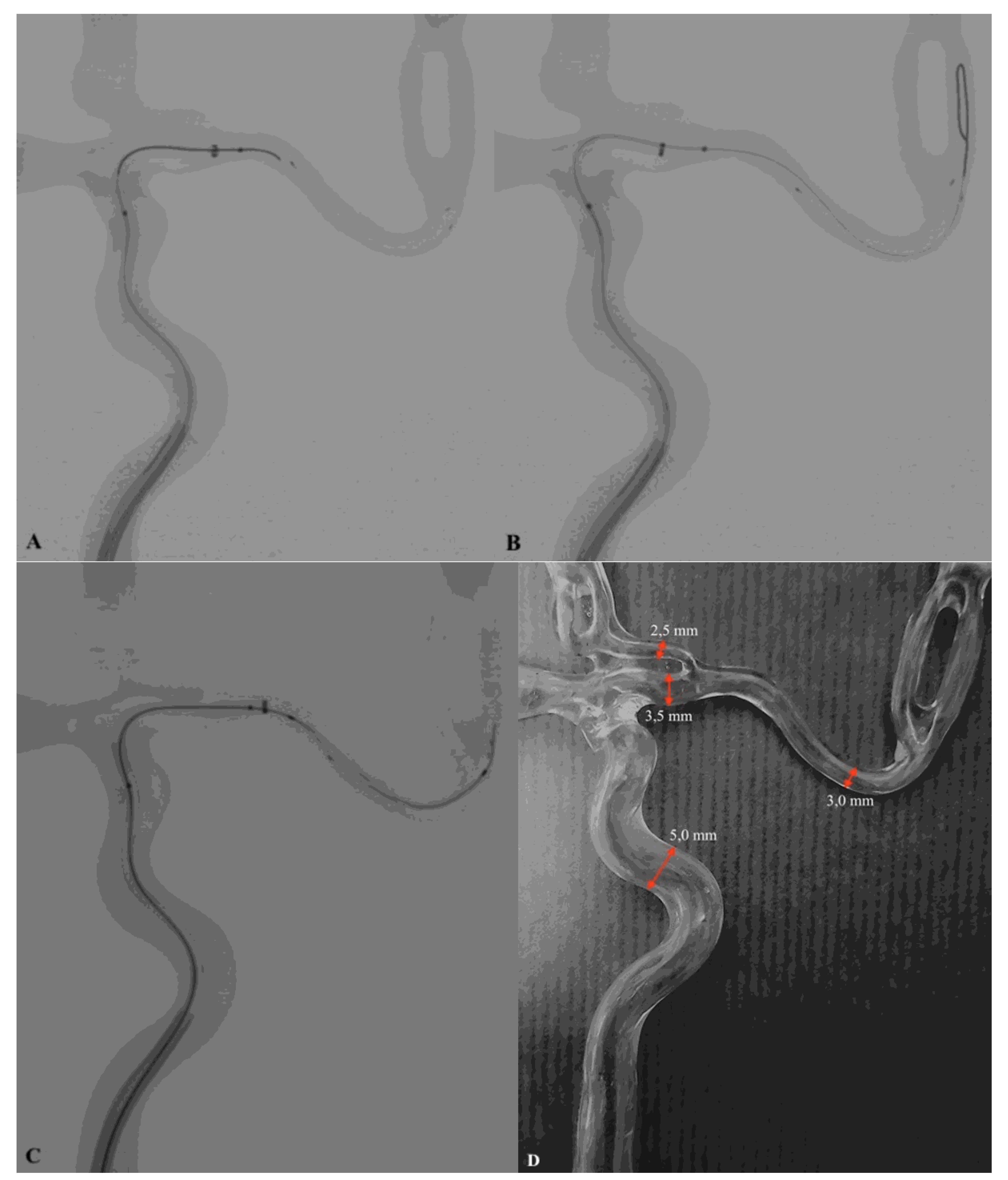
3.1. Case Study
3.1.1. Patient No. 1
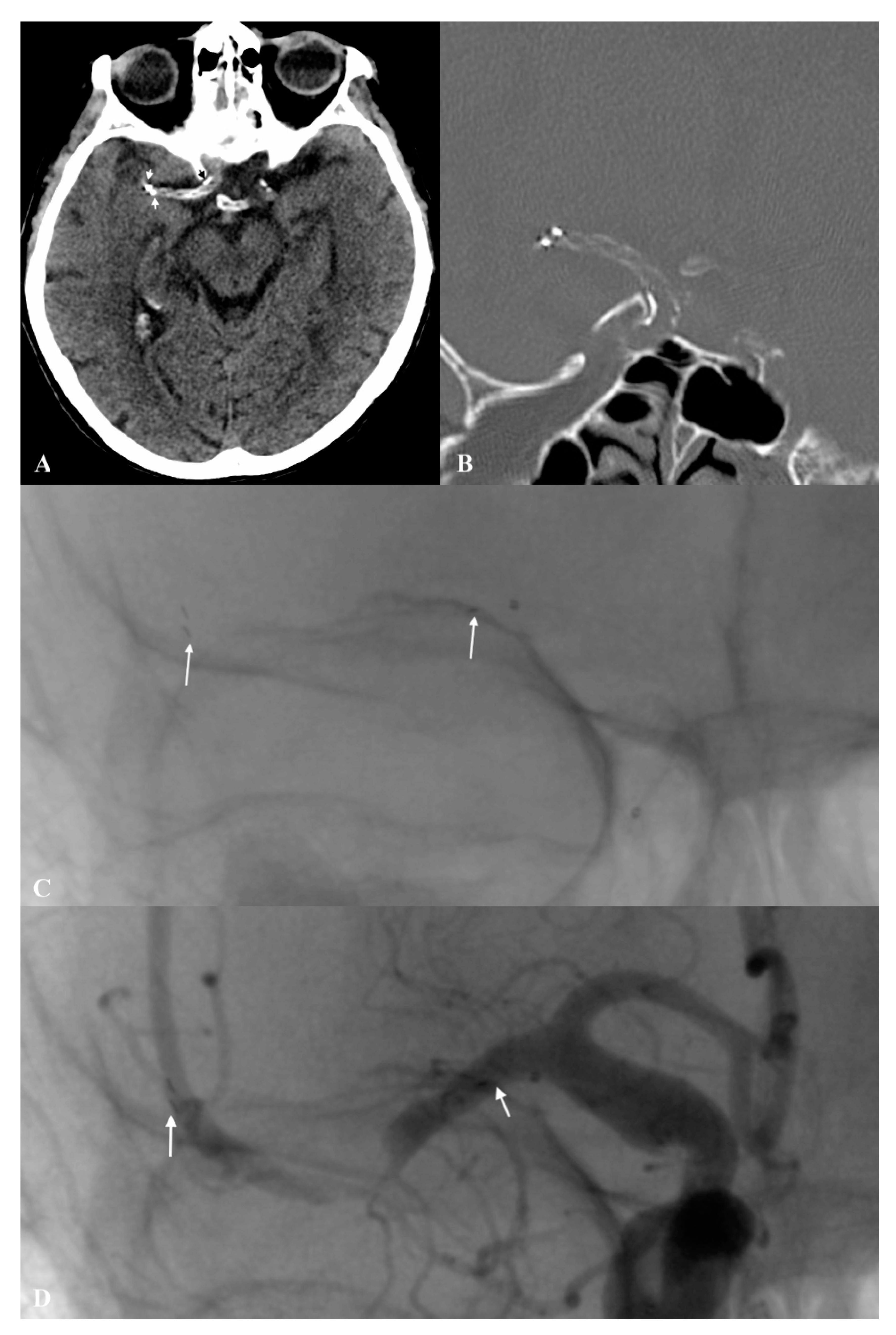
3.1.2. Patient No. 2
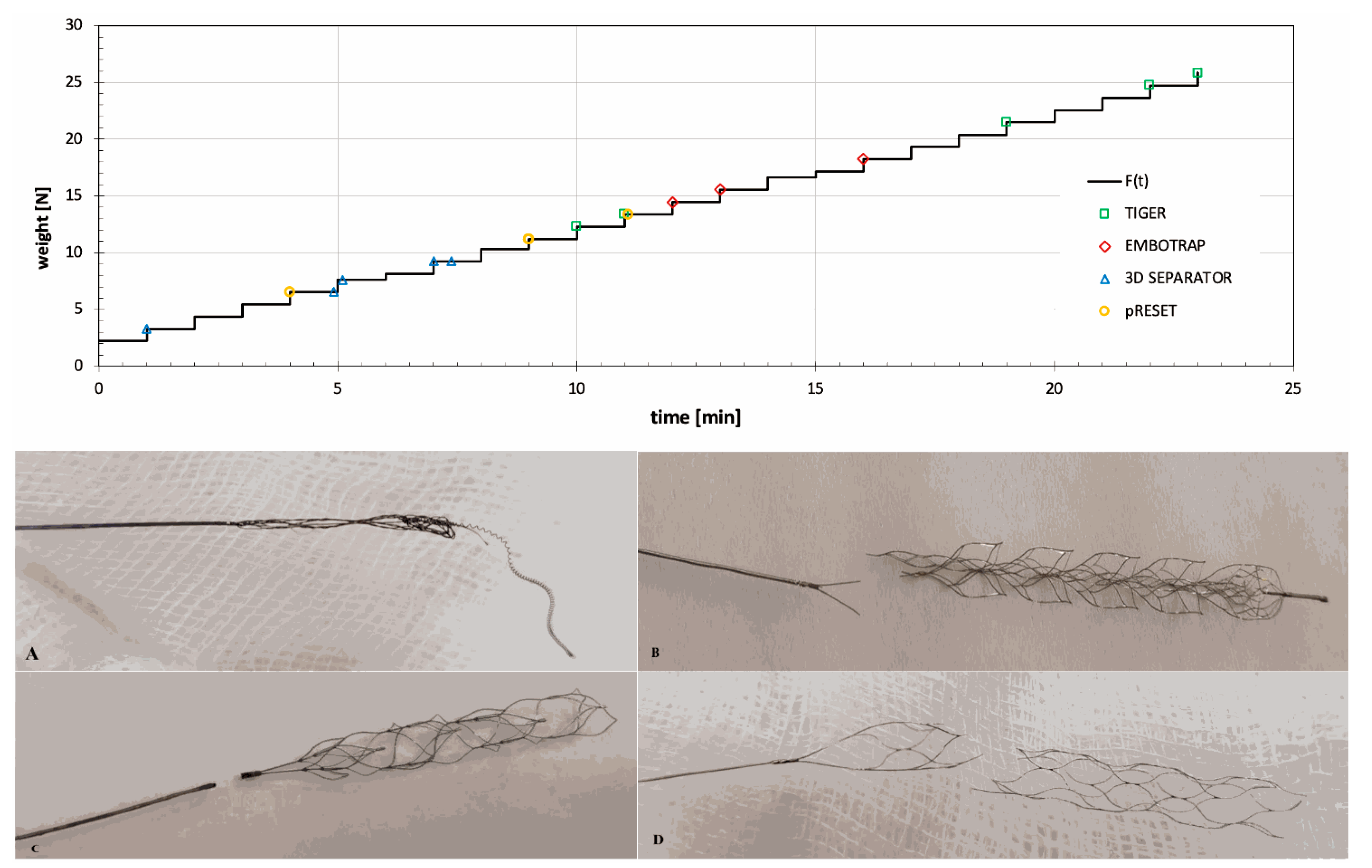
3.2. Laboratory Traction Load Test
3.3. Phantom Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goyal, M.; Demchuk, A.M.; Menon, B.K.; Eesa, M.; Rempel, J.L.; Thornton, J.; Roy, D.; Jovin, T.G.; Willinsky, R.A.; Sapkota, B.L.; et al. Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. N. Engl. J. Med. 2015, 372, 1019–1030. [Google Scholar] [CrossRef]
- Saver, J.L. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N. Engl. J. Med. 2015, 372, 2285–2295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bracard, S.; Ducrocq, X.; Mas, J.L.; Soudant, M.; Oppenheim, C.; Moulin, T.; Guillemin, F. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): A randomised controlled trial. Lancet Neurol. 2016, 15, 1138–1147. [Google Scholar] [CrossRef]
- Campbell, B.; Mitchell, P.J.; Kleinig, T.; Dewey, H.M.; Churilov, L.; Yassi, N.; Yan, B.; Dowling, R.J.; Parsons, M.W.; Oxley, T.; et al. Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection. N. Engl. J. Med. 2015, 372, 1009–1018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berkhemer, O.A. A randomized trial of intraarterial treatment for acute ischemic stroke. N. Engl. J. Med. 2015, 372, 11–20. [Google Scholar] [CrossRef] [Green Version]
- Kurre, W.; Aguilar-Pérez, M.; Schmid, E.; Sperber, W.; Bäzner, H.; Henkes, H. Clinical experience with the pREset stent retriever for the treatment of acute ischemic stroke—A review of 271 consecutive cases. Neuroradiology 2014, 56, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Prothmann, S.; Schwaiger, B.; Gersing, A.; Reith, W.; Niederstadt, T.; Felber, A.; Kurre, W. Acute Recanalization of Thrombo-Embolic Ischemic Stroke with pREset (ARTESp): The impact of occlusion time on clinical outcome of directly admitted and transferred patients. J. NeuroInterventional Surg. 2016, 9, 817–822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwaiger, B.J.; Kober, F.; Gersing, A.; Kleine, J.F.; Wunderlich, S.; Zimmer, C.; Poppert, H.; Prothmann, S. The pREset Stent Retriever for Endovascular Treatment of Stroke Caused by MCA Occlusion: Safety and Clinical Outcome. Clin. Neuroradiol. 2014, 26, 47–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pfaff, J.; Herweh, C.; Pham, M.; Schieber, S.; Ringleb, P.; Bendszus, M.; Möhlenbruch, M. Mechanical Thrombectomy of Distal Occlusions in the Anterior Cerebral Artery: Recanalization Rates, Periprocedural Complications, and Clinical Outcome. Am. J. Neuroradiol. 2015, 37, 673–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Behme, D.; Gondecki, L.; Fiethen, S.; Kowoll, A.; Mpotsaris, A.; Weber, W. Complications of mechanical thrombectomy for acute ischemic stroke—A retrospective single-center study of 176 consecutive cases. Neuroradiology 2014, 56, 467–476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masoud, H.; Nguyen, T.N.; Martin, C.O.; Holloway, W.E.; Ambekar, S.; Yavagal, D.R.; Haussen, D.C.; Nogueira, R.; Lozano, D.J.; Puri, A.; et al. Inadvertent Stent Retriever Detachment: A Multicenter Case Series and Review of Device Experience FDA Reports. Interv. Neurol. 2015, 4, 75–82. [Google Scholar] [CrossRef] [Green Version]
- Gascou, G.; Lobotesis, K.; Machi, P.; Maldonado, I.; Vendrell, J.-F.; Riquelme, C.; Eker, O.; Mercier, G.; Mourand, I.; Arquizan, C.; et al. Stent Retrievers in Acute Ischemic Stroke: Complications and Failures during the Perioperative Period. Am. J. Neuroradiol. 2013, 35, 734–740. [Google Scholar] [CrossRef] [Green Version]
- Simgen, A.; Kettner, M.; Webelsiep, F.J.; Tomori, T.; Mühl-Benninghaus, R.; Yilmaz, U.; Bhogal, P.; Laschke, M.W.; Menger, M.D.; Reith, W.; et al. Solitaire Stentectomy Using a Stent-Retriever Technique in a Porcine Model. Clin. Neuroradiol. 2021, 31, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Meyer, T.; Nikoubashman, O.; Kabelitz, L.; Müller, M.; Othman, A.; Afat, S.; Kramer, M.; Wiesmann, M.; Brockmann, M.A.; Brockmann, C. Endovascular stentectomy using the snare over stent-retriever (SOS) technique: An experimental feasibility study. PLoS ONE 2017, 12, e0178197. [Google Scholar] [CrossRef] [Green Version]
- Parthasarathy, R. Solitaire stentectomy: ‘deploy and engage’ and ‘loop and snare’ techniques. BMJ Case Rep. 2016, 10, e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e99. [Google Scholar] [CrossRef] [PubMed]
- Turc, G.; Bhogal, P.; Fischer, U.; Khatri, P.; Lobotesis, K.; Mazighi, M.; Schellinger, P.D.; Toni, D.; De Vries, J.; White, P.; et al. European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J. NeuroInterventional Surg. 2019, 11, 535–538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- von Elm, E. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- pRESET—Phenox. Available online: https://phenox.net/international/preset-thrombectomy-device/ (accessed on 11 November 2020).
- Kara, B.; Selcuk, H.H.; Salik, A.E.; Zalov, H.; Yildiz, O.; Gul, G.; Balkan, B. Single-center experience with the Tigertriever device for the recanalization of large vessel occlusions in acute ischemic stroke. J. NeuroInterventional Surg. 2018, 11, 455–459. [Google Scholar] [CrossRef]
- Higashida, R.T. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 2003, 34, e109–e137. [Google Scholar] [CrossRef] [Green Version]
- Park, H.; Baek, J.-H.; Kim, B.M. Endovascular Treatment of Acute Stroke Due to Intracranial Atherosclerotic Stenosis–Related Large Vessel Occlusion. Front. Neurol. 2019, 10, 308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balami, J.S.; White, P.M.; McMeekin, P.; A Ford, G.; Buchan, A.M. Complications of endovascular treatment for acute ischemic stroke: Prevention and management. Int. J. Stroke 2018, 13, 348–361. [Google Scholar] [CrossRef] [Green Version]
- Kamal, N.; Sheng, S.; Xian, Y.; Matsouaka, R.; Hill, M.D.; Bhatt, D.L.; Saver, J.L.; Reeves, M.J.; Fonarow, G.C.; Schwamm, L.H.; et al. Delays in Door-to-Needle Times and Their Impact on Treatment Time and Outcomes in Get With The Guidelines-Stroke. Stroke 2017, 48, 946–954. [Google Scholar] [CrossRef] [PubMed]
- García-Tornel, Á.; Requena, M.; Rubiera, M.; Muchada, M.; Pagola, J.; Rodriguez-Luna, D.; Deck, M.; Juega, J.; Rodríguez-Villatoro, N.; Boned, S.; et al. When to Stop. Stroke 2019, 50, 1781–1788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, D.-H.; Park, J.; Hwang, Y.-H.; Kim, Y.-S. Inadvertent Self-Detachment of Solitaire AB Stent during the Mechanical Thrombectomy for Recanalization of Acute Ischemic Stroke: Lessons Learned from the Removal of Stent via Surgical Embolectomy. J. Korean Neurosurg. Soc. 2013, 53, 360–363. [Google Scholar] [CrossRef] [PubMed]
- Heck, D.V.; Brown, M.D. Carotid stenting and intracranial thrombectomy for treatment of acute stroke due to tandem occlusions with aggressive antiplatelet therapy may be associated with a high incidence of intracranial hemorrhage. J. NeuroInterventional Surg. 2015, 7, 170–175. [Google Scholar] [CrossRef]
| Phantom Study | |||||||
|---|---|---|---|---|---|---|---|
| Interventional Radiologist (No.) | Successful Rescue Procedure Rate (No.) | Average Procedure Time (s) | Procedure Complications | ||||
| pRESET Migration (n) | Breaking of pRESET and/or Tigertriever Structure (n) | Stent Retriever’s Entrapment (n) | Inadvertent Detachment of Tigertriever (n) | ||||
| 1 | 5/5 | 165 | 0 | 0 | 0 | 0 | |
| 2 | 5/5 | 173 | 0 | 0 | 0 | 0 | |
| 3 | 5/5 | 183 | 0 | 0 | 0 | 0 | |
| LABORATORY TENSION LOADING TEST | |||||||
| Tested stent retriever | Tigertriever (RapidMedical) | pRESET (Phenox) | 3D Separator (Penumbra) | Embotrap (Johnson&Johnson) | |||
| Number of tested SR (n) | 5 | 5 | 5 | 3 | |||
| Average tension load causing SR damage (g) | 1992 | 1093 | 733 | 1639 | |||
| Average tension causing SR damage (N) | 19.5 | 10.7 | 7.2 | 16.1 | |||
| Duration of the breaking load (n): | |||||||
| when the load was applied | 5 | 4 | 3 | 3 | |||
| 5 s after the load was applied | 0 | 1 | 1 | 0 | |||
| 23 s after the load was applied | 0 | 0 | 0 | 0 | |||
| 55 s after the load was applied | 0 | 0 | 1 | 0 | |||
| Type of SR damage (n): | |||||||
| deformation of the SR structure, without rupture | 3 | 0 | 0 | 0 | |||
| SR rupture at 1/3 proximal length | 0 | 2 | 0 | 2 | |||
| SR rupture at the point of connection with pusher wire (near the proximal stent marker) | 0 | 3 | 5 | 0 | |||
| pusher wire rupture | 2 | 0 | 0 | 0 | |||
| SR rupture at the 1/3 distal length | 0 | 0 | 0 | 1 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piasecki, P.; Wierzbicki, M.; Tulik, P.; Potocka, K.; Stępień, A.; Staszewski, J.; Dębiec, A.; Narloch, J. Inadvertent Detachment of Stent Retrievers during Mechanical Thrombectomy—A Clinical and Biomechanical Perspective. Life 2021, 11, 658. https://doi.org/10.3390/life11070658
Piasecki P, Wierzbicki M, Tulik P, Potocka K, Stępień A, Staszewski J, Dębiec A, Narloch J. Inadvertent Detachment of Stent Retrievers during Mechanical Thrombectomy—A Clinical and Biomechanical Perspective. Life. 2021; 11(7):658. https://doi.org/10.3390/life11070658
Chicago/Turabian StylePiasecki, Piotr, Marek Wierzbicki, Piotr Tulik, Katarzyna Potocka, Adam Stępień, Jacek Staszewski, Aleksander Dębiec, and Jerzy Narloch. 2021. "Inadvertent Detachment of Stent Retrievers during Mechanical Thrombectomy—A Clinical and Biomechanical Perspective" Life 11, no. 7: 658. https://doi.org/10.3390/life11070658
APA StylePiasecki, P., Wierzbicki, M., Tulik, P., Potocka, K., Stępień, A., Staszewski, J., Dębiec, A., & Narloch, J. (2021). Inadvertent Detachment of Stent Retrievers during Mechanical Thrombectomy—A Clinical and Biomechanical Perspective. Life, 11(7), 658. https://doi.org/10.3390/life11070658






