NADomics: Measuring NAD+ and Related Metabolites Using Liquid Chromatography Mass Spectrometry
Abstract
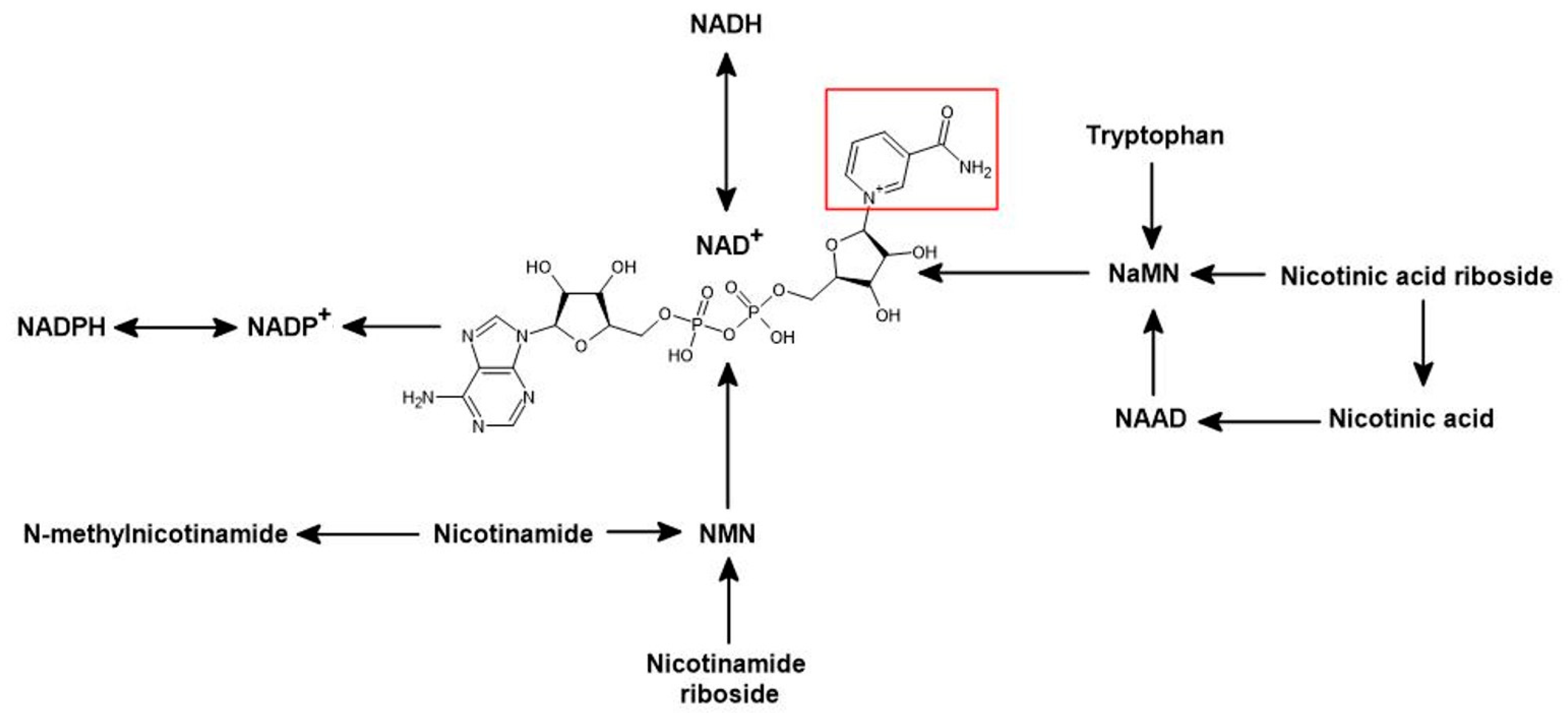
1. Introducing NADomics as a Tool for Quantification of the NADome in Biological Samples
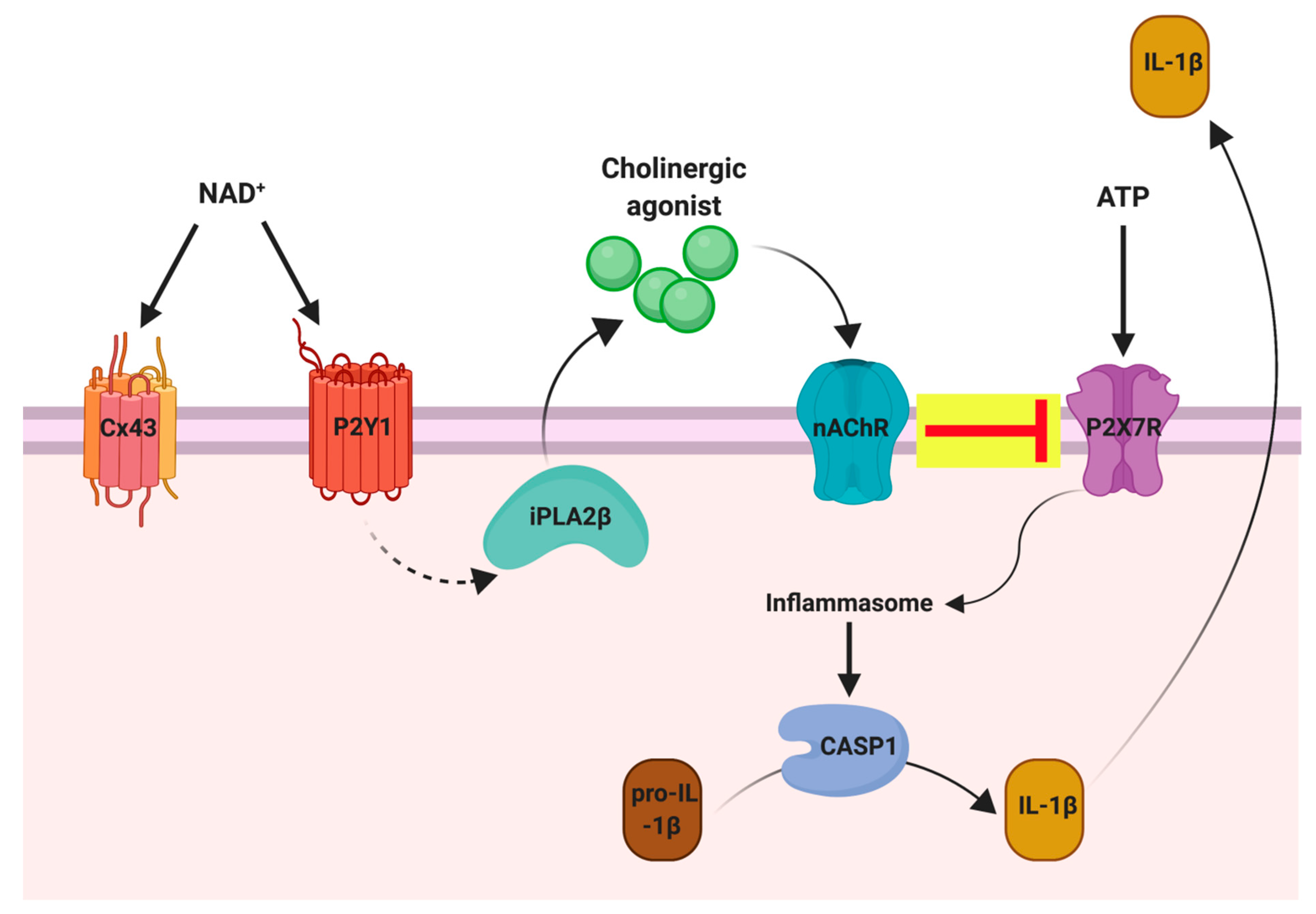
2. Clinical Relevance for Detection of the NADome in Biological Fluids
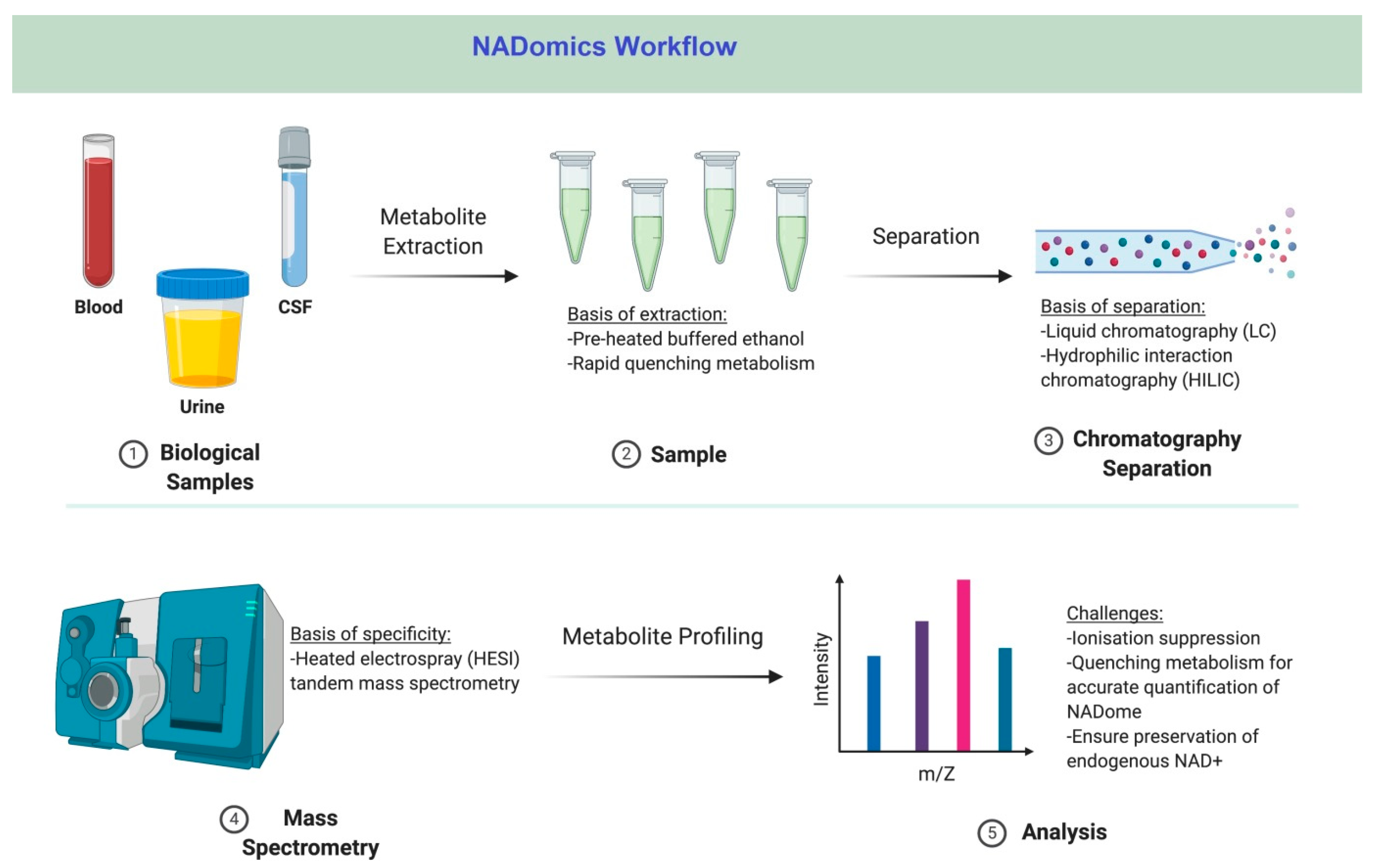
3. Analysis of the NADome Using Traditional Techniques
4. Quantification of the NADome Using Liquid Chromatography-Mass Spectrometry
5. Challenges of NADomics in Biological Specimens
5.1. Extraction
5.2. Internal Standards
5.3. Analyte Stability
5.4. Liquid Chromatography
6. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Massudi, H.; Grant, R.; Guillemin, G.J.; Braidy, N. NAD+ metabolism and oxidative stress: The golden nucleotide on a crown of thorns. Redox Rep. 2012, 17, 28–46. [Google Scholar] [CrossRef]
- Braidy, N.; Guillemin, G.J.; Mansour, H.; Chan-Ling, T.; Poljak, A.; Grant, R. Age Related Changes in NAD+ Metabolism Oxidative Stress and Sirt1 Activity in Wistar Rats. PLoS ONE 2011, 6, e19194. [Google Scholar] [CrossRef]
- Braidy, N.; Poljak, A.; Grant, R.; Jayasena, T.; Mansour, H.; Chan-Ling, T.; Guillemin, G.J.; Smythe, G.; Sachdev, P. Mapping NAD+ metabolism in the brain of ageing Wistar rats: Potential targets for influencing brain senescence. Biogerontology 2014, 15, 177–198. [Google Scholar] [CrossRef]
- Braidy, N.; Poljak, A.; Grant, R.; Jayasena, T.; Mansour, H.; Chan-Ling, T.; Smythe, G.; Sachdev, P.; Guillemin, G.J. Differential expression of sirtuins in the aging rat brain. Front. Cell. Neurosci. 2015, 9, 167. [Google Scholar] [CrossRef] [PubMed]
- Braidy, N.; Berg, J.; Clement, J.; Khorshidi, F.; Poljak, A.; Jayasena, T.; Grant, R.; Sachdev, P. NAD+ Precursors as Therapeutic Agents for Age-related Degenerative Diseases. Antioxid. Redox Signal. 2019, 30, 251–294. [Google Scholar] [CrossRef]
- Horenstein, A.L.; Sizzano, F.; Lusso, R.; Besso, F.G.; Ferrero, E.; Deaglio, S.; Corno, F.; Malavasi, F. CD38 and CD157 Ectoenzymes Mark Cell Subsets in the Human Corneal Limbus. Mol. Med. 2009, 15, 76–84. [Google Scholar] [CrossRef]
- Surjana, D.; Halliday, G.M.; Damian, D.L. Role of Nicotinamide in DNA Damage, Mutagenesis, and DNA Repair. J. Nucleic Acids 2010, 2010, 157591. [Google Scholar] [CrossRef]
- Vaquero, A.; Sternglanz, R.; Reinberg, D. NAD+ -dependent deacetylation of H4 lysine 16 by class III HDACs. Oncogene 2007, 26, 5505–5520. [Google Scholar] [CrossRef]
- Fan, J.; Krautkramer, K.A.; Feldman, J.L.; Denu, J.M. Metabolic Regulation of Histone Post-Translational Modifications. ACS Chem. Biol. 2015, 10, 95–108. [Google Scholar] [CrossRef]
- Braidy, N.; Guillemin, G.; Grant, R. Promotion of cellular NAD+ anabolism: Therapeutic potential for oxidative stress in ageing and Alzheimer’s disease. Neurotox. Res. 2008, 13, 173–184. [Google Scholar] [CrossRef]
- Fu, C.S.; Swendseid, M.E.; Jacob, R.A.; McKee, R.W. Biochemical Markers for Assessment of Niacin Status in Young Men: Levels of Erythrocyte Niacin Coenzymes and Plasma Tryptophan. J. Nutr. 1989, 119, 1949–1955. [Google Scholar] [CrossRef] [PubMed]
- Jacob, R.A.; Swendseid, M.E.; McKee, R.W.; Fu, C.S.; Clemens, R.A. Biochemical Markers for Assessment of Niacin Status in Young Men: Urinary and Blood Levels of Niacin Metabolites. J. Nutr. 1989, 119, 591–598. [Google Scholar] [CrossRef]
- Sartini, D.; Santarelli, A.; Rossi, V.; Goteri, G.; Rubini, C.; Ciavarella, D.; Muzio, L.L.; Emanuelli, M. Nicotinamide N-methyltransferase upregulation inversely correlates with lymph node metastasis in oral squamous cell carcinoma. Mol. Med. 2007, 13, 415–421. [Google Scholar] [CrossRef]
- Bogan, K.L.; Brenner, C. Nicotinic Acid, Nicotinamide, and Nicotinamide Riboside: A Molecular Evaluation of NAD+ Precursor Vitamins in Human Nutrition. Annu. Rev. Nutr. 2008, 28, 115–130. [Google Scholar] [CrossRef]
- Liu, Y.; Clement, J.; Grant, R.; Sachdev, P.; Braidy, N. Quantitation of NAD+: Why do we need to measure it? Biochim. Biophys. Acta Gen. Subj. 2018, 1862, 2527–2532. [Google Scholar] [CrossRef]
- Trammell, S.; Brenner, C. Targeted, LCMS-Based Metabolomics for Quantitative Measurement Of NAD+ Metabolites. Comput. Struct. Biotechnol. J. 2013, 4, e201301012. [Google Scholar] [CrossRef]
- Clement, J.; Wong, M.; Poljak, A.; Sachdev, P.; Braidy, N. The Plasma NAD+ Metabolome Is Dysregulated in “Normal” Aging. Rejuvenation Res. 2018, 22, 121–130. [Google Scholar] [CrossRef]
- Seyedsadjadi, N.; Berg, J.; Bilgin, A.A.; Braidy, N.; Salonikas, C.; Grant, R. High protein intake is associated with low plasma NAD+ levels in a healthy human cohort. PLoS ONE 2018, 13, e0201968. [Google Scholar] [CrossRef]
- Braidy, N.; Lim, C.K.; Grant, R.; Brew, B.J.; Guillemin, G.J. Serum nicotinamide adenine dinucleotide levels through disease course in multiple sclerosis. Brain Res. 2013, 1537, 267–272. [Google Scholar] [CrossRef]
- Long, A.N.; Owens, K.; Schlappal, A.E.; Kristian, T.; Fishman, P.S.; Schuh, R.A. Effect of nicotinamide mononucleotide on brain mitochondrial respiratory deficits in an Alzheimer’s disease-relevant murine model. BMC Neurol. 2015, 15, 19. [Google Scholar] [CrossRef]
- Trammell, S.; Schmidt, M.; Weidemann, B.J.; Redpath, P.; Jaksch, F.; Dellinger, R.W.; Philip, R.; Abel, E.D.; Migaud, M.E.; Brenner, C. Nicotinamide riboside is uniquely and orally bioavailable in mice and humans. Nat. Commun. 2016, 7, 12948. [Google Scholar] [CrossRef]
- Martens, C.R.; Denman, B.A.; Mazzo, M.R.; Armstrong, M.L.; Reisdorph, N.; McQueen, M.B.; Chonchol, M.; Seals, D.R. Chronic nicotinamide riboside supplementation is well-tolerated and elevates NAD+ in healthy middle-aged and older adults. Nat. Commun. 2018, 9, 1286. [Google Scholar] [CrossRef]
- Dollerup, O.L.; Christensen, B.; Svart, M.; Schmidt, M.; Sulek, K.; Ringgaard, S.; Stødkilde-Jørgensen, H.; Møller, N.; Brenner, C.; Treebak, J.T.; et al. A randomized placebo-controlled clinical trial of nicotinamide riboside in obese men: Safety, insulin-sensitivity, and lipid-mobilizing effects. Am. J. Clin. Nutr. 2018, 108, 343–353. [Google Scholar] [CrossRef]
- Demarest, T.G.; Truong, G.T.D.; Lovett, J.; Mohanty, J.G.; Mattison, J.A.; Mattson, M.P.; Ferrucci, L.; Bohr, V.A.; Moaddel, R. Assessment of NAD+ metabolism in human cell cultures, erythrocytes, cerebrospinal fluid and primate skeletal muscle. Anal. Biochem. 2019, 572, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Billington, R.A.; Travelli, C.; Ercolano, E.; Galli, U.; Roman, C.B.; Grolla, A.A.; Canonico, P.L.; Condorelli, F.; Genazzani, A.A. Characterization of NAD Uptake in Mammalian Cells. J. Biol. Chem. 2008, 283, 6367–6374. [Google Scholar] [CrossRef] [PubMed]
- Kulikova, V.; Shabalin, K.; Nerinovski, K.; Dölle, C.; Niere, M.; Yakimov, A.; Redpath, P.; Khodorkovskiy, M.; Migaud, M.E.; Ziegler, M.; et al. Generation, Release, and Uptake of the NAD Precursor Nicotinic Acid Riboside by Human Cells. J. Biol. Chem. 2015, 290, 27124–27137. [Google Scholar] [CrossRef]
- Airhart, S.E.; Shireman, L.M.; Risler, L.J.; Anderson, G.D.; Gowda, G.A.N.; Raftery, D.; Tian, R.; Shen, D.D.; O’Brien, K. An open-label, non-randomized study of the pharmacokinetics of the nutritional supplement nicotinamide riboside (NR) and its effects on blood NAD+ levels in healthy volunteers. PLoS ONE 2017, 12, e0186459. [Google Scholar] [CrossRef]
- Alefishat, E.; Alexander, S.P.H.; Ralevic, V. Effects of NAD at purine receptors in isolated blood vessels. Purinergic Signal. 2014, 11, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Adriouch, S.; Haag, F.; Boyer, O.; Seman, M.; Koch-Nolte, F. Extracellular NAD+: A danger signal hindering regulatory T cells. Microbes Infect. 2012, 14, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Boini, K.M.; Xia, M.; Xiong, J.; Li, C.; Payne, L.P.; Li, P.-L. Implication of CD38 gene in podocyte epithelial-to-mesenchymal transition and glomerular sclerosis. J. Cell. Mol. Med. 2012, 16, 1674–1685. [Google Scholar] [CrossRef]
- Sasaki, T.; Yamanaka, M.; Kagami, N. WITHDRAWN: Superoxide generation in different brain regions of rats during normoxia and hypoxia-reoxygenation. Neurosci. Res. 2012, 74, 261–268. [Google Scholar] [CrossRef]
- Liang, M.; Yin, X.-L.; Wang, L.-Y.; Yin, W.-H.; Song, N.-Y.; Shi, H.-B.; Li, C.-Y.; Yin, S.-K. NAD+ Attenuates Bilirubin-Induced Hyperexcitation in the Ventral Cochlear Nucleus by Inhibiting Excitatory Neurotransmission and Neuronal Excitability. Front. Cell. Neurosci. 2017, 11, 21. [Google Scholar] [CrossRef]
- Durnin, L.; Dai, Y.; Aiba, I.; Shuttleworth, C.W.; Yamboliev, I.A.; Mutafova-Yambolieva, V.N. Release, neuronal effects and removal of extracellular β-nicotinamide adenine dinucleotide (β-NAD+) in the rat brain. Eur. J. Neurosci. 2012, 35, 423–435. [Google Scholar] [CrossRef]
- Imai, S.-I. “Clocks” in the NAD World: NAD as a metabolic oscillator for the regulation of metabolism and aging. Biochim. Biophys. Acta Proteins Proteom. 2010, 1804, 1584–1590. [Google Scholar] [CrossRef] [PubMed]
- Sancesario, G.; Morello, M.; Massa, R.; Fusco, F.R.; D’Angelo, V.; Bernardi, G. NADPH-Diaphorase Neurons Contacting the Cerebrospinal Fluid in the Ventricles of Rat Brain. Br. J. Pharmacol. 1996, 16, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, K.; Matsubara, K.; Kondo, M.; Murakawa, Y.; Suno, M.; Yamashita, K.; Yamaguchi, S.; Kobayashi, S. Nicotinamide-N-methyltransferase is higher in the lumbar cerebrospinal fluid of patients with Parkinson’s disease. Neurosci. Lett. 2001, 298, 78–80. [Google Scholar] [CrossRef]
- Casabona, G.; Sturiale, L.; L’Episcopo, M.R.; Raciti, G.; Fazzio, A.; Sarpietro, M.G.; A Genazzani, A.; Cambria, A.; Nicoletti, F. HPLC analysis of cyclic adenosine diphosphate ribose and adenosine diphosphate ribose: Determination of NAD+ metabolites in hippocampal membranes. Ital. J. Biochem. 1995, 44, 258–268. [Google Scholar]
- Bernofsky, C.; Swan, M. An improved cycling assay for nicotinamide adenine dinucleotide. Anal. Biochem. 1973, 53, 452–458. [Google Scholar] [CrossRef]
- Helenius, M.; Jalkanen, S.; Yegutkin, G.G. Enzyme-coupled assays for simultaneous detection of nanomolar ATP, ADP, AMP, adenosine, inosine and pyrophosphate concentrations in extracellular fluids. Biochim. Biophys. Acta Bioenergy 2012, 1823, 1967–1975. [Google Scholar] [CrossRef]
- Romanova, N.; Ugarova, N.; Brovko, L. Bioluminescent Assay of Bacterial Intracellular AMP, ADP, and ATP with the Use of a Coimmobilized Three-Enzyme Reagent (Adenylate Kinase, Pyruvate Kinase, and Firefly Luciferase). Anal. Biochem. 1994, 220, 410–414. [Google Scholar] [CrossRef]
- Veech, R.L.; Eggleston, L.V.; Krebs, H.A. The redox state of free nicotinamide–adenine dinucleotide phosphate in the cytoplasm of rat liver. Biochem. J. 1969, 115, 609–619. [Google Scholar] [CrossRef]
- Lu, W.; Wang, L.; Chen, L.; Hui, S.; Rabinowitz, J.D. Extraction and Quantitation of Nicotinamide Adenine Dinucleotide Redox Cofactors. Antioxid. Redox Signal. 2018, 28, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Shabalin, K.; Nerinovski, K.; Yakimov, A.; Kulikova, V.; Svetlova, M.; Solovjeva, L.; Khodorkovskiy, M.; Gambaryan, S.; Cunningham, R.; Migaud, M.E.; et al. NAD Metabolome Analysis in Human Cells Using 1H NMR Spectroscopy. Int. J. Mol. Sci. 2018, 19, 3906. [Google Scholar] [CrossRef] [PubMed]
- Kiyokawa, E.; Hayama, T.; Yoshida, H.; Yamaguchi, M.; Nohta, H. Fluorous-assisted metal chelate affinity extraction for nucleotides followed by HILIC-MS/MS analysis. J. Chromatogr. B 2018, 1074–1075, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Dowell, D. HILIC-MS/MS Method for the Quantitation of Nucleotides in Infant Formula and Adult Nutritional Formula: First Action 2011.21. J. AOAC Int. 2012, 95, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Obara, R.; Hino, T.; Oka, H. Development and Application of an HILIC-MS/MS Method for the Quantitation of Nucleotides in Infant Formula. J. Agric. Food Chem. 2010, 58, 9918–9924. [Google Scholar] [CrossRef]
- Bustamante, S.; Jayasena, T.; Richani, D.; Gilchrist, R.; Wu, L.E.; Sinclair, D.A.; Sachdev, P.; Braidy, N. Quantifying the cellular NAD+ metabolome using a tandem liquid chromatography mass spectrometry approach. Metabolomics 2018, 14, 15. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Wang, T.-C.; Heyes, M.P.; Markey, S. LC/MS analysis of NAD biosynthesis using stable isotope pyridine precursors. Anal. Biochem. 2002, 306, 197–203. [Google Scholar] [CrossRef]
- Yamada, K.; Hara, N.; Shibata, T.; Osago, H.; Tsuchiya, M. The simultaneous measurement of nicotinamide adenine dinucleotide and related compounds by liquid chromatography/electrospray ionization tandem mass spectrometry. Anal. Biochem. 2006, 352, 282–285. [Google Scholar] [CrossRef]
- Evans, C.; Bogan, K.L.; Song, P.; Burant, C.F.; Kennedy, R.T.; Brenner, C. NAD+ metabolite levels as a function of vitamins and calorie restriction: Evidence for different mechanisms of longevity. BMC Chem. Biol. 2010, 10, 2. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Braidy, N.; Villalva, M.D.; Grant, R. NADomics: Measuring NAD+ and Related Metabolites Using Liquid Chromatography Mass Spectrometry. Life 2021, 11, 512. https://doi.org/10.3390/life11060512
Braidy N, Villalva MD, Grant R. NADomics: Measuring NAD+ and Related Metabolites Using Liquid Chromatography Mass Spectrometry. Life. 2021; 11(6):512. https://doi.org/10.3390/life11060512
Chicago/Turabian StyleBraidy, Nady, Maria D. Villalva, and Ross Grant. 2021. "NADomics: Measuring NAD+ and Related Metabolites Using Liquid Chromatography Mass Spectrometry" Life 11, no. 6: 512. https://doi.org/10.3390/life11060512
APA StyleBraidy, N., Villalva, M. D., & Grant, R. (2021). NADomics: Measuring NAD+ and Related Metabolites Using Liquid Chromatography Mass Spectrometry. Life, 11(6), 512. https://doi.org/10.3390/life11060512






