Association of Contemporary Statin Pretreatment Intensity and LDL-C Levels on the Incidence of STEMI Presentation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Patients’ Inclusion/Exclusion/Withdrawal Criteria
2.3. Statistical Analyses
3. Results
3.1. Baseline Characteristics
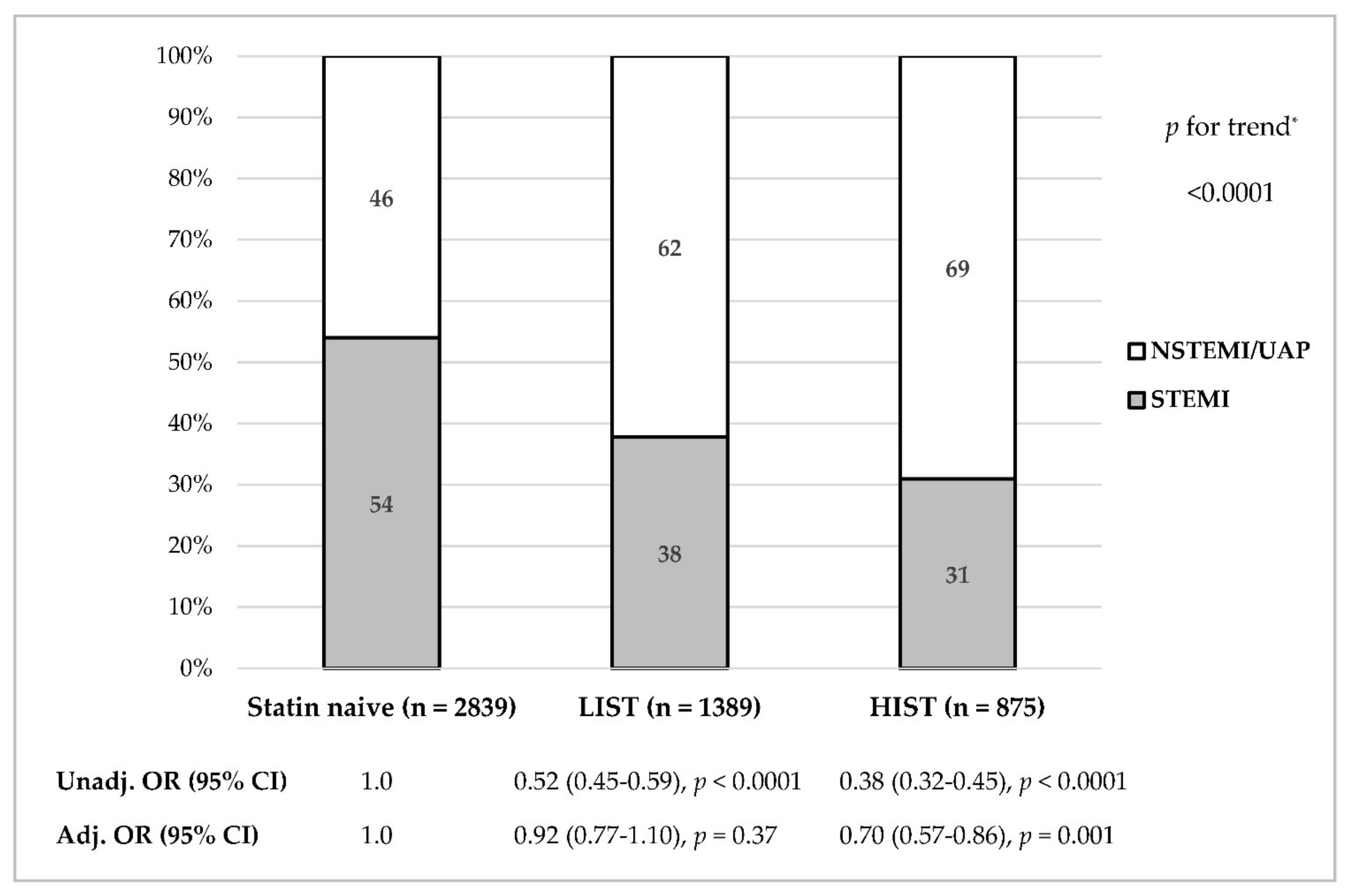
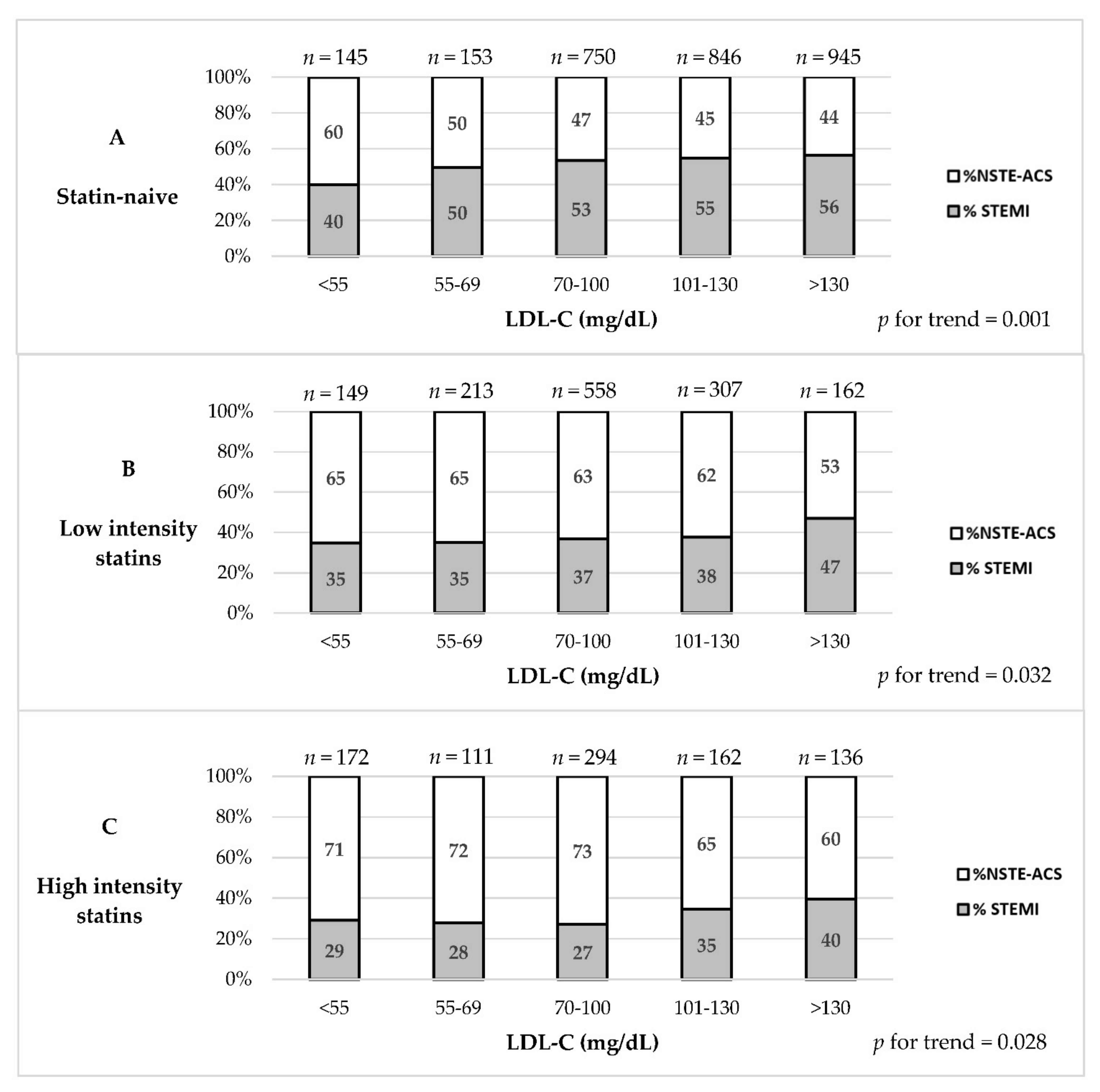
3.2. Association between Statin Therapy, LDL-C Levels and ACS Type
3.3. Association between Statin and Ezetimibe Therapy and ACS Type
3.4. Multivariate Analyses for STEMI Presentation
4. Discussion
4.1. Prior Studies
4.2. Statin Intensity and Plaque Characteristics
4.3. STEMI Presentation in Reduced LDL-C Levels Settings
4.4. HIST in Primary and Secondary Prevention
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mihaylova, B.; Emberson, J.; Blackwell, L.; Keech, A.; Simes, J.; Barnes, E.H.; Voysey, M.; Gray, A.; Collins, R.; Baigent, C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: Meta-analysis of individual data from 27 randomised trials. Lancet 2012, 380, 581–590. [Google Scholar]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; De Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, e285–e350. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Oesterle, A.; Laufs, U.; Liao, J.K. Pleiotropic effects of statins on the cardiovascular system. Circ. Res. 2017, 120, 229–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davignon, J. Beneficial cardiovascular pleiotropic effects of statins. Circulation 2004, 109 (Suppl. III), III-39–III-43. [Google Scholar] [CrossRef] [Green Version]
- Björck, L.; Wallentin, L.; Stenestrand, U.; Lappas, G.; Rosengren, A. Medication in relation to ST-segment elevation myocardial infarction in patients with a first myocardial infarction: Swedish Register of Information and Knowledge About Swedish Heart Intensive Care Admissions (RIKS-HIA). Arch. Intern. Med. 2010, 170, 1375–1381. [Google Scholar] [CrossRef] [Green Version]
- Spencer, F.A.; Allegrone, J.; Goldberg, R.J.; Gore, J.M.; Fox, K.A.; Granger, C.B.; Mehta, R.H.; Brieger, D. Association of statin therapy with outcomes of acute coronary syndromes: The GRACE study. Ann. Intern. Med. 2004, 140, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Cuculi, F.; Radovanovic, D.; Eberli, F.R.; Stauffer, J.C.; Bertel, O.; Erne, P. The impact of statin treatment on presentation mode and early outcomes in acute coronary syndromes. Cardiology 2008, 109, 156–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, M.; Huang, Y.; Du, X.; Li, S.; Ji, J.; Patel, A.; Gao, R.; Wu, Y. Impact of prior use of four preventive medications on outcomes in patients hospitalized for acute coronary syndrome–results from CPACS-2 Study. PLoS ONE 2016, 11, e0163068. [Google Scholar] [CrossRef]
- Ndrepepa, G.; Fusaro, M.; King, L.; Cassese, S.; Tada, T.; Schömig, A.; Kastrati, A. Statin pretreatment and presentation patterns in patients with coronary artery disease. Cardiol. J. 2013, 20, 52–58. [Google Scholar] [CrossRef] [Green Version]
- Segev, A.; Matetzky, S.; Danenberg, H.; Fefer, P.; Bubyr, L.; Zahger, D.; Roguin, A.; Gottlieb, S.; Kornowski, R. Contemporary use and outcome of percutaneous coronary interventions in patients with acute coronary syndromes: Insights from the 2010 ACSIS and ACSIS-PCI surveys. EuroIntervention 2012, 8, 465–469. [Google Scholar] [CrossRef]
- Expert Panel on Detection, E. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar]
- Weidmann, L.; Obeid, S.; Mach, F.; Shahin, M.; Yousif, N.; Denegri, A.; Muller, O.; Räber, L.; Matter, C.M.; Lüscher, T.F. Pre-existing treatment with aspirin or statins influences clinical presentation, infarct size and inflammation in patients with de novo acute coronary syndromes. Int. J. Cardiol. 2019, 275, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, S.; Kolker, S.; Shlomo, N.; Matetzky, S.; Leitersdorf, E.; Segev, A.; Goldenberg, I.; Tzivoni, D.; Weisz, G.; Moriel, M. Association between statin treatment and LDL-cholesterol levels on the rate of ST-elevation myocardial infarction among patients with acute coronary syndromes: ACS Israeli Survey (ACSIS) 2002–2010. Int. J. Cardiol. 2016, 210, 133–138. [Google Scholar] [CrossRef]
- Tarkin, J.M.; Dweck, M.R.; Rudd, J.H. Imaging as a surrogate marker of drug efficacy in cardiovascular disease. Heart 2019, 105, 567–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nissen, S.E.; Nicholls, S.J.; Sipahi, I.; Libby, P.; Raichlen, J.S.; Ballantyne, C.M.; Davignon, J.; Erbel, R.; Fruchart, J.C.; Tardif, J.C.; et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: The ASTEROID trial. JAMA 2006, 295, 1556–1565. [Google Scholar] [CrossRef]
- Nissen, S.E.; Tuzcu, E.M.; Schoenhagen, P.; Brown, B.G.; Ganz, P.; Vogel, R.A.; Crowe, T.; Howard, G.; Cooper, C.J.; Brodie, B.; et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: A randomized controlled trial. JAMA 2004, 291, 1071–1080. [Google Scholar] [CrossRef]
- Gili, S.; Iannaccone, M.; Colombo, F.; Montefusco, A.; Amabile, N.; Calcagno, S.; Capodanno, D.; Scalone, G.; Rognoni, A.; Omedè, P.; et al. Effects of statins on plaque rupture assessed by optical coherence tomography in patients presenting with acute coronary syndromes: Insights from the optical coherence tomography (OCT)-FORMIDABLE registry. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Ozaki, Y.; Garcia-Garcia, H.M.; Beyene, S.S.; Hideo-Kajita, A.; Kuku, K.O.; Kolm, P.; Waksman, R. Effect of Statin Therapy on Fibrous Cap Thickness in Coronary Plaque on Optical Coherence Tomography―Review and Meta-Analysis. Circ. J. 2019, 83, 1480–1488. [Google Scholar] [CrossRef] [Green Version]
- Hou, J.; Xing, L.; Jia, H.; Vergallo, R.; Soeda, T.; Minami, Y.; Hu, S.; Yang, S.; Zhang, S.; Lee, H.; et al. Comparison of intensive versus moderate lipid-lowering therapy on fibrous cap and atheroma volume of coronary lipid-rich plaque using serial optical coherence tomography and intravascular ultrasound imaging. Am. J. Cardiol. 2016, 117, 800–806. [Google Scholar] [CrossRef] [PubMed]
- Tawakol, A.; Fayad, Z.A.; Mogg, R.; Alon, A.; Klimas, M.T.; Dansky, H.; Subramanian, S.S.; Abdelbaky, A.; Rudd, J.H.; Farkouh, M.E.; et al. Intensification of statin therapy results in a rapid reduction in atherosclerotic inflammation: Results of a multicenter fluorodeoxyglucose-positron emission tomography/computed tomography feasibility study. J. Am. Coll. Cardiol. 2013, 62, 909–917. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hecht, H.S.; Blaha, M.J.; Kazerooni, E.A.; Cury, R.C.; Budoff, M.; Leipsic, J.; Shaw, L. CAC-DRS: Coronary Artery Calcium Data and Reporting System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT). J. Cadiovasc. Comput. Tomogr. 2018, 12, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Puri, R.; Nicholls, S.J.; Shao, M.; Kataoka, Y.; Uno, K.; Kapadia, S.R.; Tuzcu, E.M.; Nissen, S.E. Impact of statins on serial coronary calcification during atheroma progression and regression. J. Am. Coll. Cardiol. 2015, 65, 1273–1282. [Google Scholar] [CrossRef]
- Auscher, S.; Heinsen, L.; Nieman, K.; Vinther, K.H.; Løgstrup, B.; Møller, J.E.; Broersen, A.; Kitslaar, P.; Lambrechtsen, J.; Egstrup, K. Effects of intensive lipid-lowering therapy on coronary plaques composition in patients with acute myocardial infarction: Assessment with serial coronary CT angiography. Atherosclerosis 2015, 241, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Sabatine, M.S.; Giugliano, R.P.; Keech, A.C.; Honarpour, N.; Wiviott, S.D.; Murphy, S.A.; Kuder, J.F.; Wang, H.; Liu, T.; Wasserman, S.M.; et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N. Eng. J. Med. 2017, 376, 1713–1722. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Giugliano, R.P.; Morrow, D.A.; De Ferrari, G.M.; Lewis, B.S.; Huber, K.; Kuder, J.F.; Murphy, S.A.; Forni, D.M.; Kurtz, C.E.; et al. Effect of Evolocumab on Type and Size of Subsequent Myocardial Infarction: A Prespecified Analysis of the FOURIER Randomized Clinical Trial. JAMA Cardiol. 2020, 5, 787–793. [Google Scholar] [CrossRef]
- White, H.D.; Steg, P.G.; Szarek, M.; Bhatt, D.L.; Bittner, V.A.; Diaz, R.; Edelberg, J.M.; Erglis, A.; Goodman, S.G.; Hanotin, C.; et al. Effect of alirocumab on types of myocardial infarction: Insights from the ODYSSEY OUTCOMES trial. Eur. Heart J. 2019, 40, 2801–2809. [Google Scholar] [CrossRef]
- PCSK9 Inhibitors and Plaque: Increased FCT Demonstrated in the HUYGENS Study. Available online: https://www.clinicaltrialsarena.com/comment/pcsk9-inhibitors-plaque-huygens-study (accessed on 23 September 2021).
- Di Stefano, R.; Di Bello, V.; Barsotti, M.C.; Grigoratos, C.; Armani, C.; Dell’Omodarme, M.; Carpi, A.; Balbarini, A. Inflammatory markers and cardiac function in acute coronary syndrome: Difference in ST-segment elevation myocardial infarction (STEMI) and in non-STEMI models. Biomed Pharmacother. 2009, 63, 773–780. [Google Scholar] [CrossRef]
- Vaidya, K.; Arnott, C.; Martínez, G.J.; Ng, B.; McCormack, S.; Sullivan, D.R.; Celermajer, D.S.; Patel, S. Colchicine therapy and plaque stabilization in patients with acute coronary syndrome: A CT coronary angiography study. JACC Cardiovasc. Imaging 2018, 11, 305–316. [Google Scholar] [CrossRef]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N. Eng. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef] [PubMed]
| Variable | Statin-Naive n = 2839 | Statin-Treated n = 2264 | p-Value 1 | Low Intensity n = 1389 | High Intensity n = 875 | p-Value 2 |
|---|---|---|---|---|---|---|
| Patients’ characteristics | ||||||
| Age, years (mean ± SD) | 61.4 ± 13.15 | 66.1 ± 11.7 | <0.001 | 67.0 ± 11.9 | 64.8 ± 11.4 | <0.001 |
| Female sex, n (%) | 508 (17.9) | 546 (24.1) | <0.001 | 372 (26.8) | 174 (19.9) | <0.001 |
| Medical history | ||||||
| Diabetes mellitus, n (%) | 766 (27.0) | 1142 (50.4) | <0.001 | 655 (47.2) | 487 (55.7) | <0.001 |
| Hypertension, n (%) | 1412 (49.7) | 1761 (77.8) | <0.001 | 1052 (75.7) | 709 (81.0) | 0.004 |
| Current smoker, n (%) | 1334 (47.0) | 712 (31.4) | <0.001 | 397 (28.6) | 315 (36.0) | <0.001 |
| CAD family history, n (%) | 800 (28.2) | 590 (26.1) | 0.097 | 339 (24.4) | 251 (28.7) | 0.027 |
| Dyslipidemia, n (%) | 1522 (53.6) | 2139 (94.5) | <0.001 | 1322 (95.2) | 817 (93.4) | 0.082 |
| CKD, n (%) | 202 (7.1) | 373 (16.5) | <0.001 | 210 (15.1) | 163 (18.6) | <0.001 |
| Prior MI, n (%) | 486 (17.1) | 1185 (52.3) | <0.001 | 606 (43.6) | 579 (66.2) | <0.001 |
| Past PCI/CABG, n (%) | 464 (16.3) | 1302 (57.5) | <0.001 | 690 (49.7) | 612 (69.9) | <0.001 |
| Past CVA/TIA, n (%) | 160 (5.6) | 251 (11.1) | <0.001 | 144 (10.4) | 107 (12.2) | 0.192 |
| PVD, n (%) | 139 (4.9) | 246 (10.8) | <0.001 | 137 (9.9) | 109 (12.5) | 0.063 |
| Chronic medical treatment | ||||||
| ACE-I/ARB, n (%) | 617 (21.7) | 1380 (61.0) | <0.001 | 788 (56.7) | 592 (67.7) | <0.001 |
| Aspirin, n (%) | 598 (21.1) | 1687 (74.5) | <0.001 | 981 (70.6) | 706 (80.7) | <0.001 |
| Clopidogrel, n (%) | 85 (3.0) | 461 (20.4) | <0.001 | 213 (15.3) | 248 (28.3) | <0.001 |
| Anti-platelets, n (%) | 99 (3.5) | 528 (23.3) | <0.001 | 220 (15.8) | 308 (35.2) | <0.001 |
| Ezetimibe, n (%) | 20 (0.7) | 83 (3.7) | <0.001 | 27 (1.9) | 56 (6.4) | <0.001 |
| Beta blockers, n (%) | 454 (16.0) | 1300 (57.4) | <0.001 | 741 (53.3) | 559 (63.9) | <0.001 |
| Presenting characteristics | ||||||
| STEMI diagnosis, n (%) | 1533 (54.0) | 796 (35.2) | <0.001 | 525 (37.8) | 271 (31.0) | 0.001 |
| Killip class > I, n (%) | 267 (9.4) | 290 (12.8) | 0.001 | 180 (13.0) | 110 (12.6) | 0.838 |
| HR (bpm), median (IQR) | 78 (68, 90) | 78 (67, 90) | 0.602 | 77 (66, 90) | 79 (68, 91) | 0.057 |
| SBP (mmHg), median (IQR) | 140 (123, 159) | 140 (124, 160) | 0.044 | 140 (124, 160) | 141 (125, 160) | 0.365 |
| Lipid profile | ||||||
| TC (mg/dL), median (IQR) | 181 (153, 211) | 155 (131, 183) | <0.001 | 157 (134, 184) | 151 (126, 182) | 0.027 |
| LDL (mg/dL), median (IQR) | 113 (89, 139) | 86 (67, 110) | <0.001 | 88 (68, 109) | 84 (63, 112) | 0.400 |
| HDL (mg/dL), median (IQR) | 38 (32, 46) | 38 (32, 46) | 0.610 | 39 (32, 47) | 37 (30, 44) | 0.230 |
| TG (mg/dL), median (IQR) | 124 (89, 176) | 129 (91, 185) | 0.005 | 128 (89, 181) | 130 (95, 188) | 0.162 |
| LDL-C Subgroups (mg/dL) | <55 | 55–69 | 70–99 | 100–129 | >130 | All | p for Trend |
|---|---|---|---|---|---|---|---|
| A. All patients | |||||||
| n | 466 | 477 | 1602 | 1315 | 1243 | 5103 | |
| STEMI rates, n (%) | 160 (34.3) | 182 (38.2) | 687 (42.9) | 637 (48.4) | 663 (53.3) | 2329 (45.6) | <0.001 |
| B. Statin naive patients | |||||||
| n | 145 | 153 | 750 | 846 | 945 | 2839 | |
| STEMI rates, n (%) | 58 (40.0) | 76 (49.7) | 401 (53.5) | 465 (55.0) | 533 (56.4) | 1533 (54.0) | 0.001 |
| C. Statin treated patients | |||||||
| n | 321 | 324 | 852 | 469 | 298 | 2264 | |
| STEMI rates, n (%) | 102 (31.8) | 106 (32.7) | 286 (33.6) | 172 (36.7) | 130 (43.6) | 796 (35.2) | 0.001 |
| D. Low-intensity statin treated patients | |||||||
| n | 149 | 213 | 558 | 307 | 162 | 1389 | 0.032 |
| STEMI rates, n (%) | 52 (34.9) | 75 (35.2) | 206 (36.9) | 116 (37.8) | 76 (46.9) | 525 (37.8) | |
| E. High-intensity statin treated patients | |||||||
| n | 172 | 111 | 294 | 162 | 136 | 875 | |
| STEMI rates, n (%) | 50 (29.1) | 31 (27.9) | 80 (27.2) | 56 (34.6) | 54 (39.7) | 271 (31.0) | 0.028 |
| Variable | Multivariate Analysis | |||
|---|---|---|---|---|
| OR a | 95% CI | p Value | c-Statistics | |
| Model 1: Propensity score quintiles | 0.632 | |||
| 1 (reference) | 1.0 | |||
| 2 (vs. 1st quintile) | 0.88 | 0.74–1.06 | 0.65 | |
| 3 (vs. 1st quintile) | 0.65 | 0.54–0.78 | <0.001 | |
| 4 (vs. 1st quintile) | 0.42 | 0.35–0.51 | <0.001 | |
| 5 (vs. 1st quintile) | 0.26 | 0.21–0.31 | <0.001 | |
| Model 2: | 0.635 | |||
| Propensity score | 0.31 | 0.24–0.39 | <0.001 | |
| Low-intensity statins (vs. statin-naive) | 0.92 | 0.77–1.10 | 0.37 | |
| High-intensity statins (vs. statin-naive) | 0.70 | 0.57–0.86 | 0.001 | |
| LDL-C < 70 mg/dL (vs. ≥70) | 0.96 | 0.82–1.14 | 0.67 | |
| Model 3 b: | 0.648 | |||
| Propensity score | 0.66 | 0.45–0.96 | 0.03 | |
| Low-intensity statins (vs. statin-naive) | 0.88 | 0.74–1.05 | 0.17 | |
| High-intensity statins (vs. statin-naive) | 0.75 | 0.61–0.93 | 0.01 | |
| LDL-C < 70 mg/dL (vs. ≥70) | 0.94 | 0.80–1.11 | 0.49 | |
| Chronic aspirin (yes vs. no) | 0.92 | 0.76–1.10 | 0.36 | |
| Chronic clopidogrel (yes vs. no) | 0.58 | 0.46–0.73 | <0.001 | |
| Chronic ACE-I/ARB (yes vs. no) | 0.77 | 0.66–0.89 | <0.001 | |
| Chronic Beta-blocker (yes vs. no) | 0.71 | 0.63–0.83 | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dadon, Z.; Moriel, M.; Iakobishvili, Z.; Asher, E.; Samuel, T.Y.; Gavish, D.; Glikson, M.; Gottlieb, S. Association of Contemporary Statin Pretreatment Intensity and LDL-C Levels on the Incidence of STEMI Presentation. Life 2021, 11, 1268. https://doi.org/10.3390/life11111268
Dadon Z, Moriel M, Iakobishvili Z, Asher E, Samuel TY, Gavish D, Glikson M, Gottlieb S. Association of Contemporary Statin Pretreatment Intensity and LDL-C Levels on the Incidence of STEMI Presentation. Life. 2021; 11(11):1268. https://doi.org/10.3390/life11111268
Chicago/Turabian StyleDadon, Ziv, Mady Moriel, Zaza Iakobishvili, Elad Asher, Tal Y. Samuel, Dov Gavish, Michael Glikson, and Shmuel Gottlieb. 2021. "Association of Contemporary Statin Pretreatment Intensity and LDL-C Levels on the Incidence of STEMI Presentation" Life 11, no. 11: 1268. https://doi.org/10.3390/life11111268
APA StyleDadon, Z., Moriel, M., Iakobishvili, Z., Asher, E., Samuel, T. Y., Gavish, D., Glikson, M., & Gottlieb, S. (2021). Association of Contemporary Statin Pretreatment Intensity and LDL-C Levels on the Incidence of STEMI Presentation. Life, 11(11), 1268. https://doi.org/10.3390/life11111268







