Loss of Concentration May Occur by Blink Inhibition in DED Simulation Models
Abstract
1. Introduction
2. Methods
2.1. Study Design, Ethical Approval, and Study Population
2.2. Study Participants and Screening Procedures
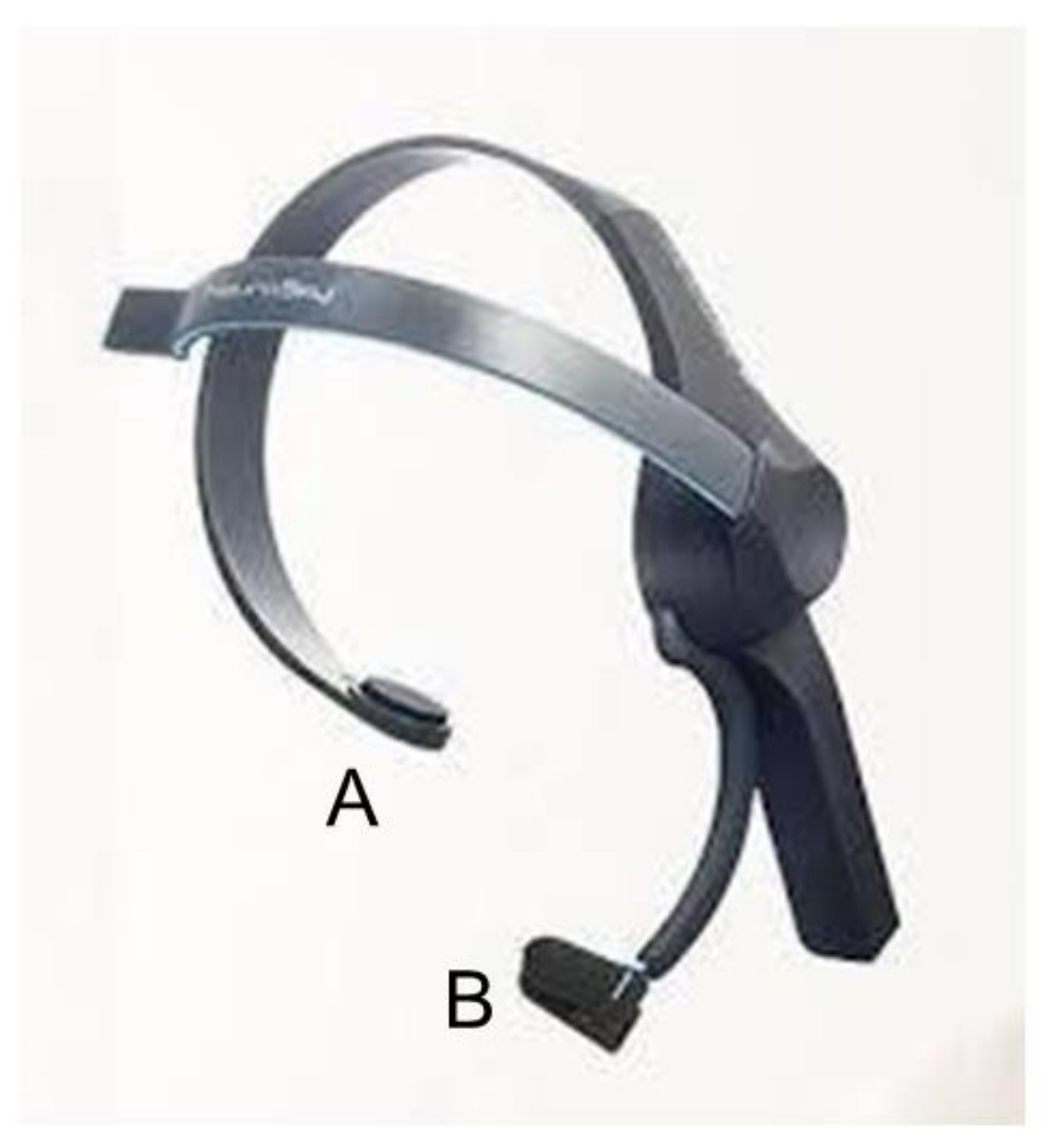
2.3. Electroencephalogram–KANSEI Analyzer
2.4. Questionnaires and Interblinking Time
2.5. Statistical Analysis
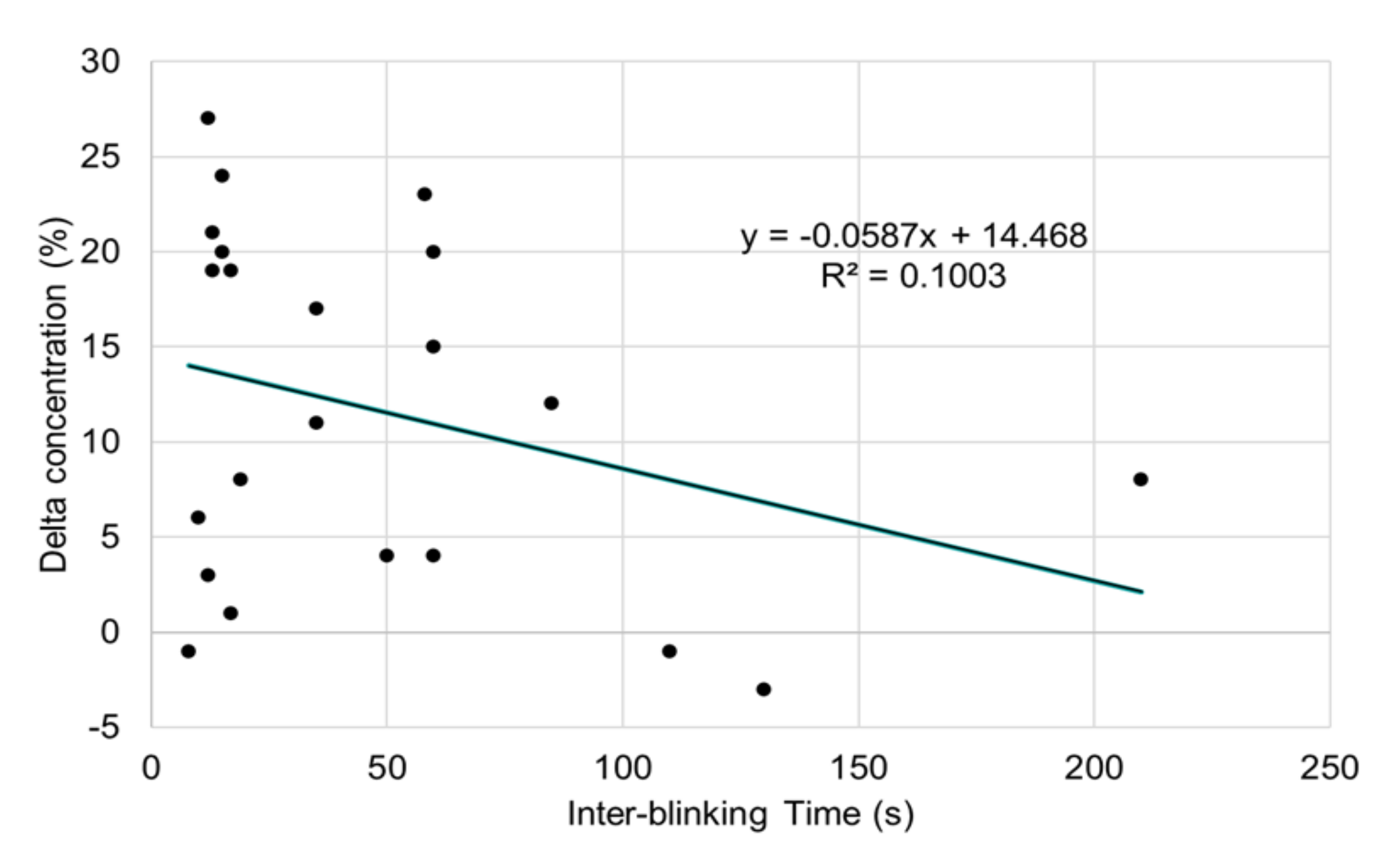
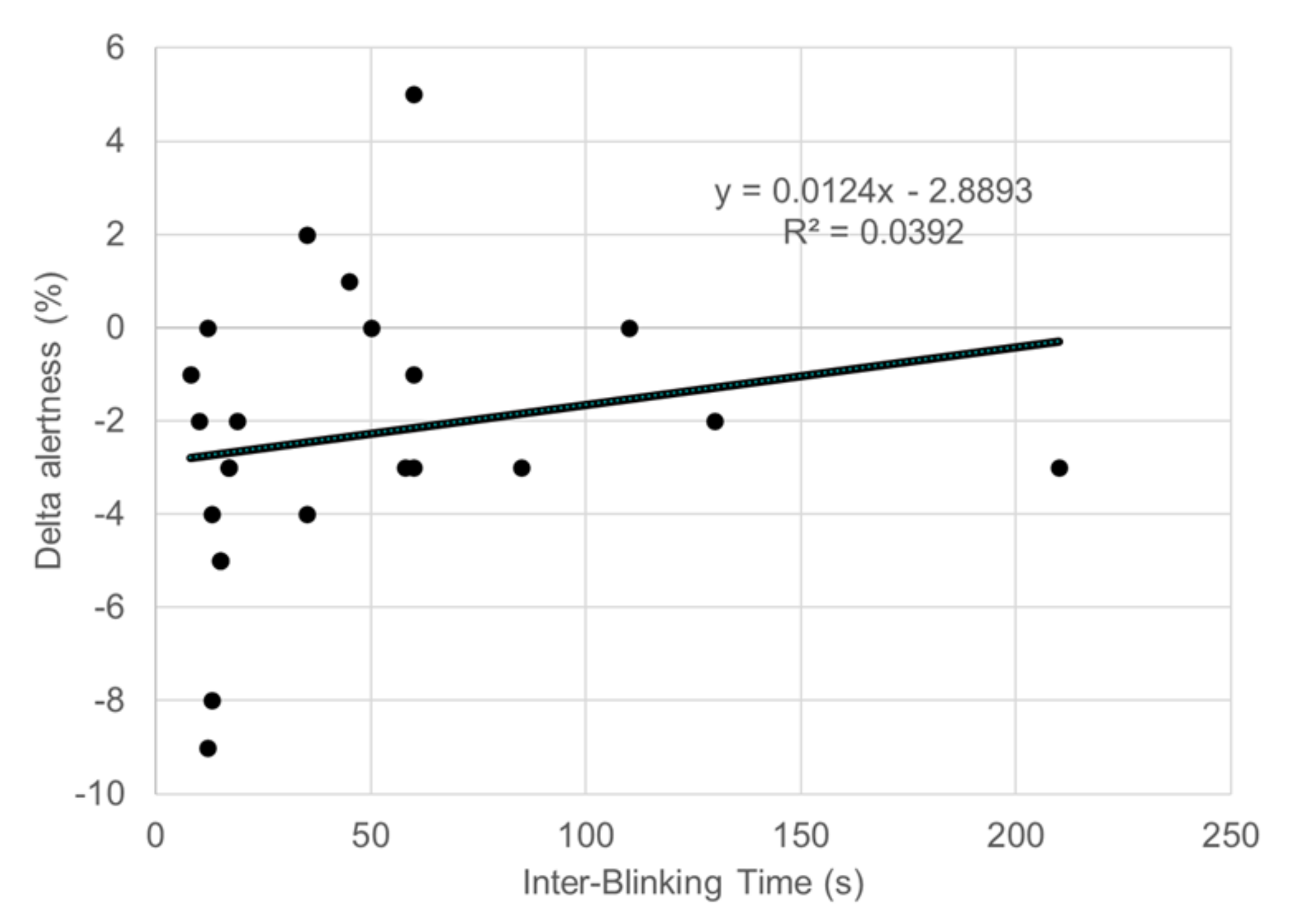
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Craig, J.P.; Nelson, J.D.; Azar, D.T.; Belmonte, C.; Bron, A.J.; Chauhan, S.K.; De Paiva, C.S.; Gomes, J.A.P.; Hammitt, K.; Jones, L.; et al. TFOS DEWS II Report Executive Summary. Ocul. Surf. 2017, 15, 802–812. [Google Scholar] [CrossRef]
- Uchino, M.; Nishiwaki, Y.; Michikawa, T.; Shirakawa, K.; Kuwahara, E.; Yamada, M.; Dogru, M.; Schaumberg, D.A.; Kawakita, T.; Takebayashi, T.; et al. Prevalence and Risk Factors of Dry Eye Disease in Japan: Koumi Study. Ophthalmology 2011, 118, 2361–2367. [Google Scholar] [CrossRef] [PubMed]
- Farrand, K.F.; Fridman, M.; Stillman, I. Özer; Schaumberg, D.A. Prevalence of Diagnosed Dry Eye Disease in the United States Among Adults Aged 18 Years and Older. Am. J. Ophthalmol. 2017, 182, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Kaido, M.; Kawashima, M.; Shigeno, Y.; Yamada, Y.; Tsubota, K. Relation of accommodative microfluctuation with dry eye symptoms in short tear break-up time dry eye. PLoS ONE 2017, 12, e0184296. [Google Scholar] [CrossRef]
- Koh, S. Irregular Astigmatism and Higher-Order Aberrations in Eyes With Dry Eye Disease. Investig. Opthalmology Vis. Sci. 2018, 59, DES36–DES40. [Google Scholar] [CrossRef]
- Miljanovic, B.; Dana, R.; Sullivan, D.A.; Schaumberg, D.A. Impact of Dry Eye Syndrome on Vision-Related Quality of Life. Am. J. Ophthalmol. 2007, 143, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Shigeyasu, C.; Yamada, M.; Kawashima, M.; Suwaki, K.; Hiratsuka, Y.; Yokoi, N.; Tsubota, K.; DECS-J study group. Quality of life measures and health utility values among dry eye subgroups. Heal. Qual. Life Outcomes 2018, 16, 170. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, M.; Uchino, M.; Yokoi, N.; Uchino, Y.; Dogru, M.; Komuro, A.; Sonomura, Y.; Kato, H.; Kinoshita, S.; Mimura, M.; et al. Associations between Subjective Happiness and Dry Eye Disease: A New Perspective from the Osaka Study. PLoS ONE 2015, 10, e0123299. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Wu, X.; Lin, X.; Lin, H. The Prevalence of Depression and Depressive Symptoms among Eye Disease Patients: A Systematic Review and Meta-analysis. Sci. Rep. 2017, 7, 46453. [Google Scholar] [CrossRef]
- Ayaki, M.; Tsubota, K.; Kawashima, M.; Kishimoto, T.; Mimura, M.; Negishi, K. Sleep Disorders are a Prevalent and Serious Comorbidity in Dry Eye. Investig. Opthalmology Vis. Sci. 2018, 59, DES143–DES150. [Google Scholar] [CrossRef]
- Uchino, M.; Uchino, Y.; Dogru, M.; Kawashima, M.; Yokoi, N.; Komuro, A.; Sonomura, Y.; Kato, H.; Kinoshita, S.; Schaumberg, D.A.; et al. Dry Eye Disease and Work Productivity Loss in Visual Display Users: The Osaka Study. Am. J. Ophthalmol. 2014, 157, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Mizuno, Y.; Shigeyasu, C. Impact of dry eye on work productivity. Clin. Outcomes Res. 2012, 4, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Bazeer, S.; Jansonius, N.; Snieder, H.; Hammond, C.; Vehof, J. The relationship between occupation and dry eye. Ocul. Surf. 2019, 17, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Van Tilborg, M.M.; Murphy, P.; Evans, K.S. Impact of Dry Eye Symptoms and Daily Activities in a Modern Office. Optom. Vis. Sci. 2017, 94, 688–693. [Google Scholar] [CrossRef] [PubMed]
- Nichols, K.K.; Bacharach, J.; Holland, E.; Kislan, T.; Shettle, L.; Lunacsek, O.; Lennert, B.; Burk, C.; Patel, V. Impact of Dry Eye Disease on Work Productivity, and Patients’ Satisfaction With Over-the-Counter Dry Eye Treatments. Investig. Ophthalmol. Vis. Sci. 2016, 57, 2975. [Google Scholar] [CrossRef]
- Patel, V.; Watanabe, J.; Strauss, J.; Dubey, A. Work productivity loss in patients with dry eye disease: An online survey. Curr. Med. Res. Opin. 2011, 27, 1041–1048. [Google Scholar] [CrossRef]
- Kaido, M.; Kawashima, M.; Ishida, R.; Tsubota, K. Relationship of Corneal Pain Sensitivity With Dry Eye Symptoms in Dry Eye With Short Tear Break-Up Time. Investig. Opthalmology Vis. Sci. 2016, 57, 914. [Google Scholar] [CrossRef]
- Tagawa, Y.; Noda, K.; Ohguchi, T.; Tagawa, Y.; Ishida, S.; Kitaichi, N. Corneal hyperalgesia in patients with short tear film break-up time dry eye. Ocul. Surf. 2019, 17, 55–59. [Google Scholar] [CrossRef]
- Pflugfelder, S.C.; De Paiva, C.S. The Pathophysiology of Dry Eye Disease. Ophthalmology 2017, 124, S4–S13. [Google Scholar] [CrossRef]
- Vehof, J.; Kozareva, D.; Hysi, P.; Harris, J.; Nessa, A.; Williams, F.M.; Bennett, D.L.; McMahon, S.B.; Fahy, S.; Direk, K.; et al. Relationship Between Dry Eye Symptoms and Pain Sensitivity. JAMA Ophthalmol. 2013, 131, 1304–1308. [Google Scholar] [CrossRef]
- Vehof, J.; Smitt-Kamminga, N.S.; Kozareva, D.; Nibourg, S.A.; Hammond, C.J.; Information, P.E.K.F.C. Clinical Characteristics of Dry Eye Patients with Chronic Pain Syndromes. Am. J. Ophthalmol. 2016, 162, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K.; Kwong, K.K.; Lee, T.-Y.; Nakamura, J.; Cheng, H.-M. Functional MRI of Brain Activation by Eye Blinking. Exp. Eye Res. 1999, 69, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Takano, Y.; Haida, M. Objective Ocular Discomfort: Noninvasive Evaluation by Functional Near-Infrared Ray Spectroscopy. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4683–4690. [Google Scholar] [CrossRef] [PubMed]
- Ratti, E.; Waninger, S.; Berka, C.; Ruffini, G.; Verma, A. Comparison of Medical and Consumer Wireless EEG Systems for Use in Clinical Trials. Front. Hum. Neurosci. 2017, 11, 398. [Google Scholar] [CrossRef]
- Mitsukura, Y.; Sumali, B.; Tazawa, Y.; Kishimoto, T.; Mimura, M. Simple Stress Quantitative Evalution for Healthcare Using Daily KANSEI Detection with EEG Device—Relation between Stress and Healthcare. Mod. Environ. Sci. Eng. 2019, 5, 345–350. [Google Scholar]
- Ogino, M.; Mitsukura, Y. Portable Drowsiness Detection through Use of a Prefrontal Single-Channel Electroencephalogram. Sensors 2018, 18, 4477. [Google Scholar] [CrossRef]
- Nakamura, S.; Shibuya, M.; Nakashima, H.; Imagawa, T.; Uehara, M.; Tsubota, K. D- -Hydroxybutyrate Protects against Corneal Epithelial Disorders in a Rat Dry Eye Model with Jogging Board. Investig. Ophthalmol. Vis. Sci. 2005, 46, 2379–2387. [Google Scholar] [CrossRef]
- Nakamura, S.; Kinoshita, S.; Yokoi, N.; Ogawa, Y.; Shibuya, M.; Nakashima, H.; Hisamura, R.; Imada, T.; Imagawa, T.; Uehara, M.; et al. Lacrimal Hypofunction as a New Mechanism of Dry Eye in Visual Display Terminal Users. PLoS ONE 2010, 5, e11119. [Google Scholar] [CrossRef]
- Sakane, Y.; Yamaguchi, M.; Yokoi, N.; Uchino, M.; Dogru, M.; Oishi, T.; Ohashi, Y.; Ohashi, Y. Development and Validation of the Dry Eye–Related Quality-of-Life Score Questionnaire. JAMA Ophthalmol. 2013, 131, 1331–1338. [Google Scholar] [CrossRef] [PubMed]
- Utsunomiya, T.; Kawahara, A.; Hanada, K.; Yoshida, A. Effects of Diquafosol Ophthalmic Solution on Quality of Life in Dry Eye Assessed Using the Dry Eye–Related Quality-of-Life Score Questionnaire. Cornea 2017, 36, 908–914. [Google Scholar] [CrossRef]
- Gulati, A.; Sullivan, R.; Buring, J.E.; Sullivan, D.A.; Dana, R.; Schaumberg, D.A. Validation and Repeatability of a Short Questionnaire for Dry Eye Syndrome. Am. J. Ophthalmol. 2006, 142, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K. Effects of Ocular Surface Area and Blink Rate on Tear Dynamics. Arch. Ophthalmol. 1995, 113, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Nakamori, K.; Odawara, M.; Nakajima, T.; Mizutani, T.; Tsubota, K. Blinking is controlled primarily by ocular surface conditions. Am. J. Ophthalmol. 1997, 124, 24–30. [Google Scholar] [CrossRef]
- Yokoi, N.; Bron, A.J.; Georgiev, G. The Precorneal Tear Film as a Fluid Shell: The Effect of Blinking and Saccades on Tear Film Distribution and Dynamics. Ocul. Surf. 2014, 12, 252–266. [Google Scholar] [CrossRef]
- Corrales, R.M. Desiccating Stress Stimulates Expression of Matrix Metalloproteinases by the Corneal Epithelium. Investig. Opthalmology Vis. Sci. 2006, 47, 3293–3302. [Google Scholar] [CrossRef]
- Marek, V.; Parsadaniantz, S.M.; Villette, T.; Montoya, F.; Baudouin, C.; Brignole-Baudouin, F.; DeNoyer, A. Blue light phototoxicity toward human corneal and conjunctival epithelial cells in basal and hyperosmolar conditions. Free Radic. Biol. Med. 2018, 126, 27–40. [Google Scholar] [CrossRef]
- Niwano, Y.; Iwasawa, A.; Tsubota, K.; Ayaki, M.; Negishi, K. Protective effects of blue light-blocking shades on phototoxicity in human ocular surface cells. BMJ Open Ophthalmol. 2019, 4, e000217. [Google Scholar] [CrossRef]
- Narimatsu, T.; Ozawa, Y.; Miyake, S.; Kubota, S.; Yuki, K.; Nagai, N.; Tsubota, K. Biological effects of blocking blue and other visible light on the mouse retina. Clin. Exp. Ophthalmol. 2013, 42, 555–563. [Google Scholar] [CrossRef]
- Lin, J.B.; Gerratt, B.W.; Bassi, C.J.; Apte, R.S. Short-Wavelength Light-Blocking Eyeglasses Attenuate Symptoms of Eye Fatigue. Investig. Ophthalmol. Vis. Sci. 2017, 58, 442. [Google Scholar] [CrossRef]
- Ayaki, M.; Kuze, M.; Kondo, M.; Tsubota, K.; Negishi, K. Association between Retinal Nerve Fiber Layer Thickness and Eye Fatigue. BioMed Res. Int. 2019, 2019, 3014567. [Google Scholar] [CrossRef]
- Matynia, A.; Nguyen, E.; Sun, X.; Blixt, F.W.; Parikh, S.; Kessler, J.; Müller, L.P.D.S.; Habib, S.; Kim, P.; Wang, Z.Z.; et al. Peripheral Sensory Neurons Expressing Melanopsin Respond to Light. Front. Neural Circuits 2016, 10, 3403. [Google Scholar] [CrossRef]
- Bristow, D.; Haynes, J.-D.; Sylvester, R.; Frith, U.; Rees, G. Blinking Suppresses the Neural Response to Unchanging Retinal Stimulation. Curr. Biol. 2005, 15, 1296–1300. [Google Scholar] [CrossRef]
- Cruz, A.A.; Garcia, D.; Pinto, C.T.; Cechetti, S.P. Spontaneous eyeblink activity. Ocul. Surf. 2011, 9, 29–41. [Google Scholar] [CrossRef]
- Berman, B.D.; Horovitz, S.G.; Morel, B.; Hallett, M. Neural correlates of blink suppression and the buildup of a natural bodily urge. NeuroImage 2011, 59, 1441–1450. [Google Scholar] [CrossRef] [PubMed]
- Crane, A.M.; Feuer, W.J.; Felix, E.R.; Levitt, R.; McClellan, A.; Sarantopoulos, K.D.; Galor, A. Evidence of central sensitisation in those with dry eye symptoms and neuropathic-like ocular pain complaints: Incomplete response to topical anaesthesia and generalised heightened sensitivity to evoked pain. Br. J. Ophthalmol. 2017, 101, 1238–1243. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K.; Yokoi, N.; Shimazaki, J.; Watanabe, H.; Dogru, M.; Yamada, M.; Kinoshita, S.; Kim, H.-M.; Tchah, H.-W.; Hyon, J.Y.; et al. New Perspectives on Dry Eye Definition and Diagnosis: A Consensus Report by the Asia Dry Eye Society. Ocul. Surf. 2017, 15, 65–76. [Google Scholar] [CrossRef] [PubMed]
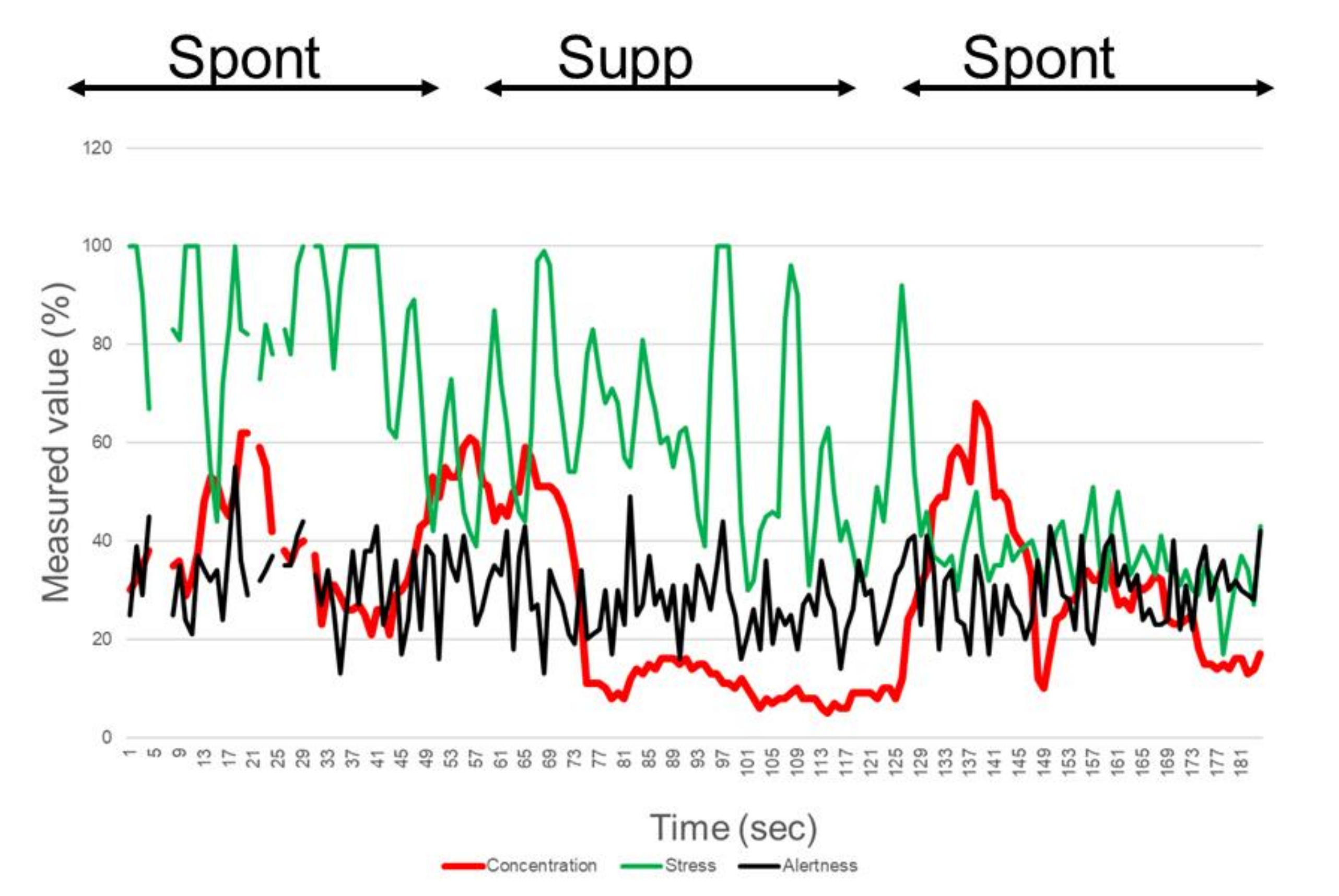
| Concentration | Stress | Alertness | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 Spont | 2 Supp | 3 Spont | 1 Spont | 2 Supp | 3 Spont | 1 Spont | 2 Supp | 3 Spont | |
| Mean (%) | 43.88 ± 10.20 | 34.32 ± 12.78 | 47.12 ± 9.09 | 34.64 ± 13.97 | 24.64 ± 9.53 | 29.20 ± 9.58 | 70.92 ± 6.05 | 72.72 ± 6.24 | 70.36 ± 6.04 |
| Paired t-test p values | <0.001 (vs. 2) | <0.001 (vs. 3) | 0.045 (vs. 1) | <0.001 (vs. 2) | 0.032 (vs. 3) | 0.069 (vs. 1) | 0.391 (vs. 2) | 0.732 (vs. 3) | 0.964 (vs. 1) |
| Delta Concentration | Delta Stress | Delta Alertness | ||||
|---|---|---|---|---|---|---|
| β | p value | β | p value | β | p value | |
| Non-adjusted | ||||||
| IBT | −0.381 | 0.066 | −0.130 | 0.552 | 0.378 | 0.062 |
| DEQS | 0.002 | 0.991 | −0.150 | 0.473 | −0.033 | 0.874 |
| Symptomatic dry eye | −0.297 | 0.157 | −0.086 | 0.687 | 0.033 | 0.874 |
| Adjusted for age and sex | ||||||
| IBT | −0.515 | 0.011* | −0.139 | 0.524 | 0.385 | 0.054 |
| DEQS | 0.022 | 0.923 | −0.222 | 0.331 | −0.086 | 0.696 |
| Symptomatic dry eye | −0.255 | 0.243 | −0.065 | 0.772 | 0.118 | 0.584 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitsukura, Y.; Negishi, K.; Ayaki, M.; Santo, M.; Kawashima, M.; Tsubota, K. Loss of Concentration May Occur by Blink Inhibition in DED Simulation Models. Life 2020, 10, 61. https://doi.org/10.3390/life10050061
Mitsukura Y, Negishi K, Ayaki M, Santo M, Kawashima M, Tsubota K. Loss of Concentration May Occur by Blink Inhibition in DED Simulation Models. Life. 2020; 10(5):61. https://doi.org/10.3390/life10050061
Chicago/Turabian StyleMitsukura, Yasue, Kazuno Negishi, Masahiko Ayaki, Mayuko Santo, Motoko Kawashima, and Kazuo Tsubota. 2020. "Loss of Concentration May Occur by Blink Inhibition in DED Simulation Models" Life 10, no. 5: 61. https://doi.org/10.3390/life10050061
APA StyleMitsukura, Y., Negishi, K., Ayaki, M., Santo, M., Kawashima, M., & Tsubota, K. (2020). Loss of Concentration May Occur by Blink Inhibition in DED Simulation Models. Life, 10(5), 61. https://doi.org/10.3390/life10050061






