Characteristics of Foot Pressure Distribution During Standing and Walking with Anatomical Leg Length Discrepancy—A Comparative Analysis of Patients with and Without Low Back Pain
Abstract
1. Introduction
2. Description of This Study
2.1. Aim
2.2. Material and Methods
- Group 1—30 participants (NP = 30; 50%) with LLD and low back pain (LBP), including 9 women and 21 men (nf = 9 women, nf%= 30%; nm = 21 men, nm%= 70%);
- Group 2—30 participants (NwP = 30; 50%) with LLD without LBP, including 14 women and 16 men (nf = 14 women, nf%= 46.66%; nm = 16 men, nm% = 53.33%).
2.3. Inclusion Criteria
- -
- Individuals with radiographically confirmed LLD, with and without low back pain (LBP);
- -
- Individuals aged over 18 and under 60 years.
2.4. Exclusion Criteria
- -
- Individuals with a history of spinal or limb surgery;
- -
- Individuals with a history of mechanical musculoskeletal and other injuries likely to affect the distribution of foot pressure, unrelated to LLD;
- -
- Individuals with a history of injuries to the limbs and axial skeleton with a significant effect on musculoskeletal biomechanics;
- -
- Those with diabetes and other endocrinopathies;
- -
- Those with rheumatic diseases;
- -
- Those with other diseases that affect fitness and locomotion;
- -
- Those who were pregnant.
2.5. Research Methodology
- Limb length was measured by radiography (X-ray) in a standing position with equal weight on both legs (i.e., central alignment of the long axis of the patella). The study included both an absolute leg length measurement, which involved measuring the actual length of the bones from the femoral head to the lateral malleolus, as well as a relative measurement, which took into account the alignment of the pelvis and spine, measuring the length from the anterior superior iliac spine to the malleolus.
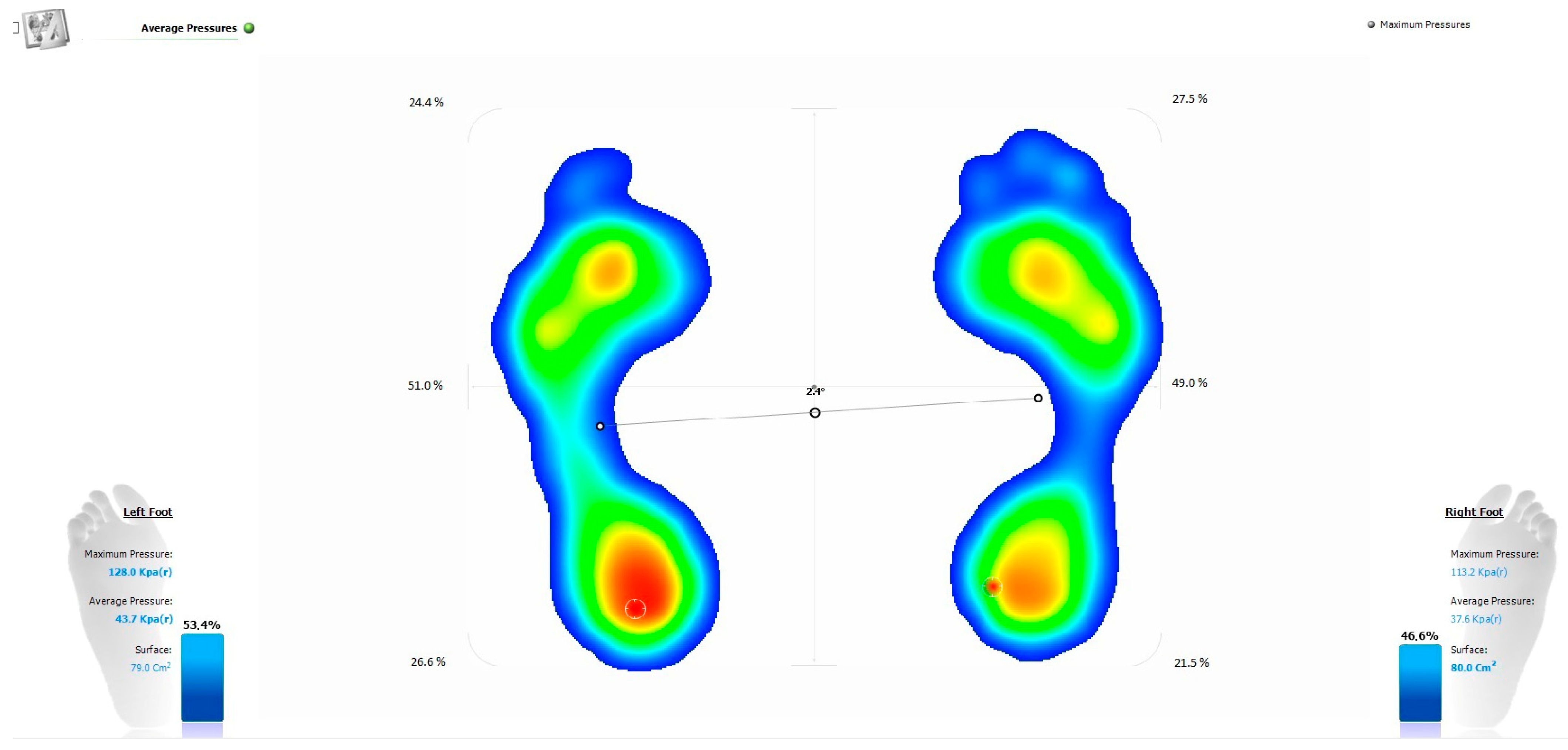
- Pedobarography was conducted using the EPS R2 pedobarograph (LETSENSE GROUP LORAN ENGINEERING, Castel Maggione Bologna, Italy), paired with Biomech Studio software version 1.6.4.28272. The test was performed barefoot in casual clothing to eliminate potential confounding factors. Participants did not engage in any physical activity on the day of testing. Standing pedobarography was performed for 20 s with a sampling interval of one millisecond. In this way, the procedure eliminated the need for repeated measurements, as the recording of front–back and left–right oscillations at such a high frequency ensured the high sensitivity and reliability of the results obtained. In the dynamic test, the gait path was designed to allow free walking, without having to aim at the instrument. As a result, the footprints where the patient missed the mat could be erased, thus ensuring the greater accuracy of the results. Twenty footprints for each foot were included in the analysis, allowing a reliable assessment of gait parameters. The following parameters were assessed by pedobarography:
2.6. Data Analysis
3. Results
3.1. Results Obtained During Standing Test
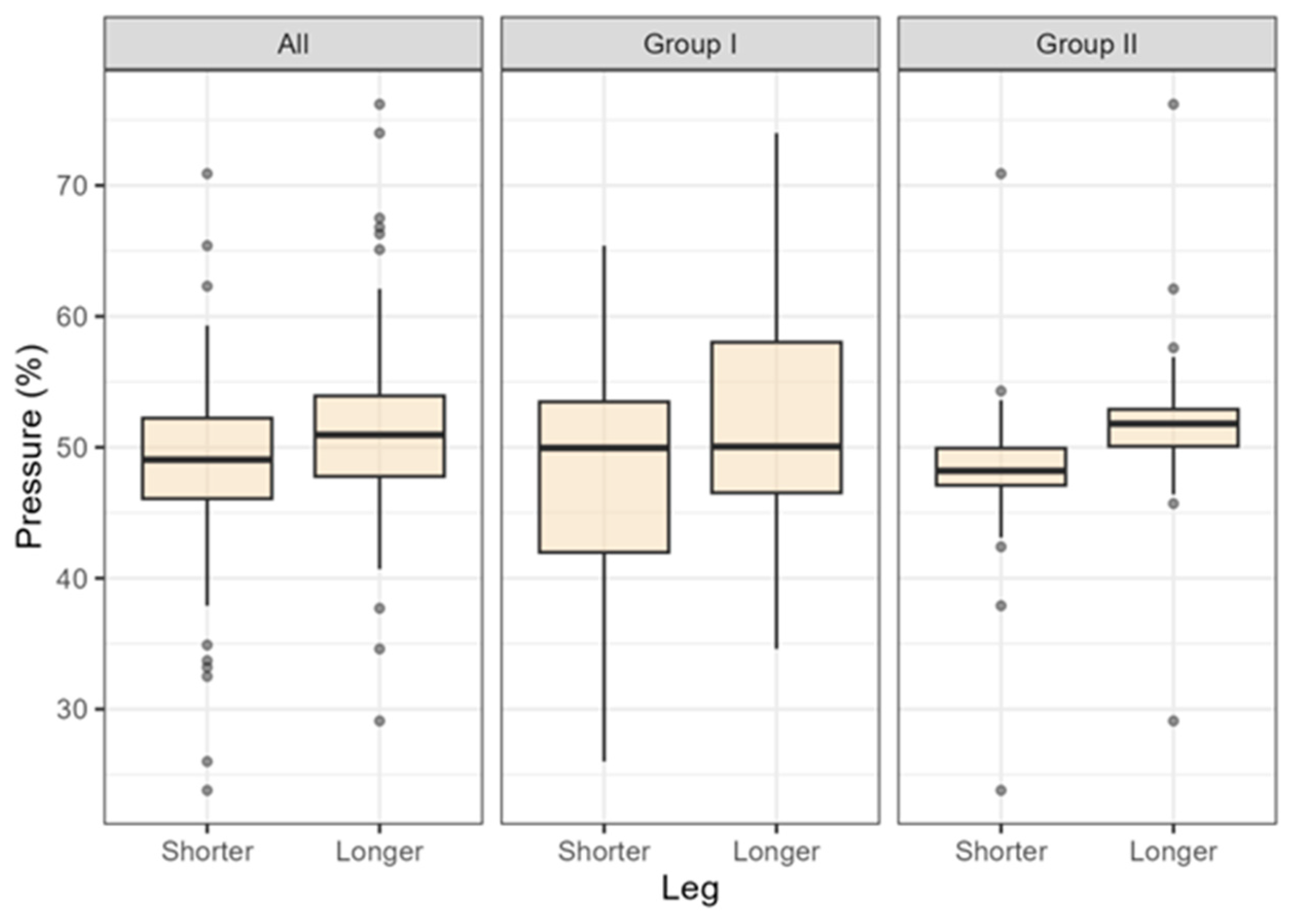
3.1.1. Left–Right Distribution of Foot Pressure During Standing (i.e., Pressure in the Shorter Limb vs. Pressure in the Longer Limb; The Range of 48–52% Was Adopted as the Normal Range of Left–Right Pressure Distribution for Both Limbs)
3.1.2. Foot Abduction Angle During Standing
3.2. Results Obtained During Walking Test (Spatial–Temporal Parameters)
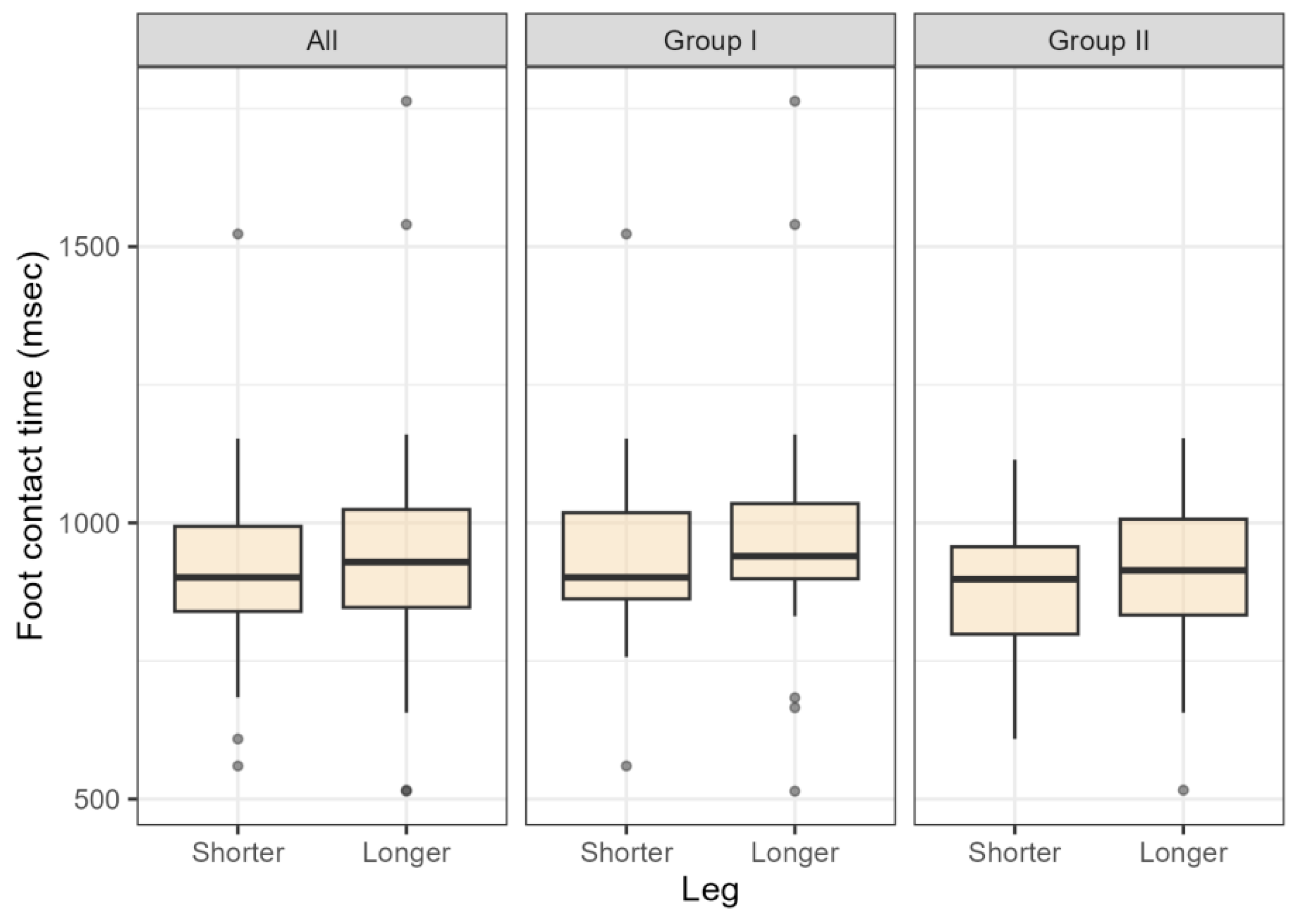
3.2.1. Foot Contact Time
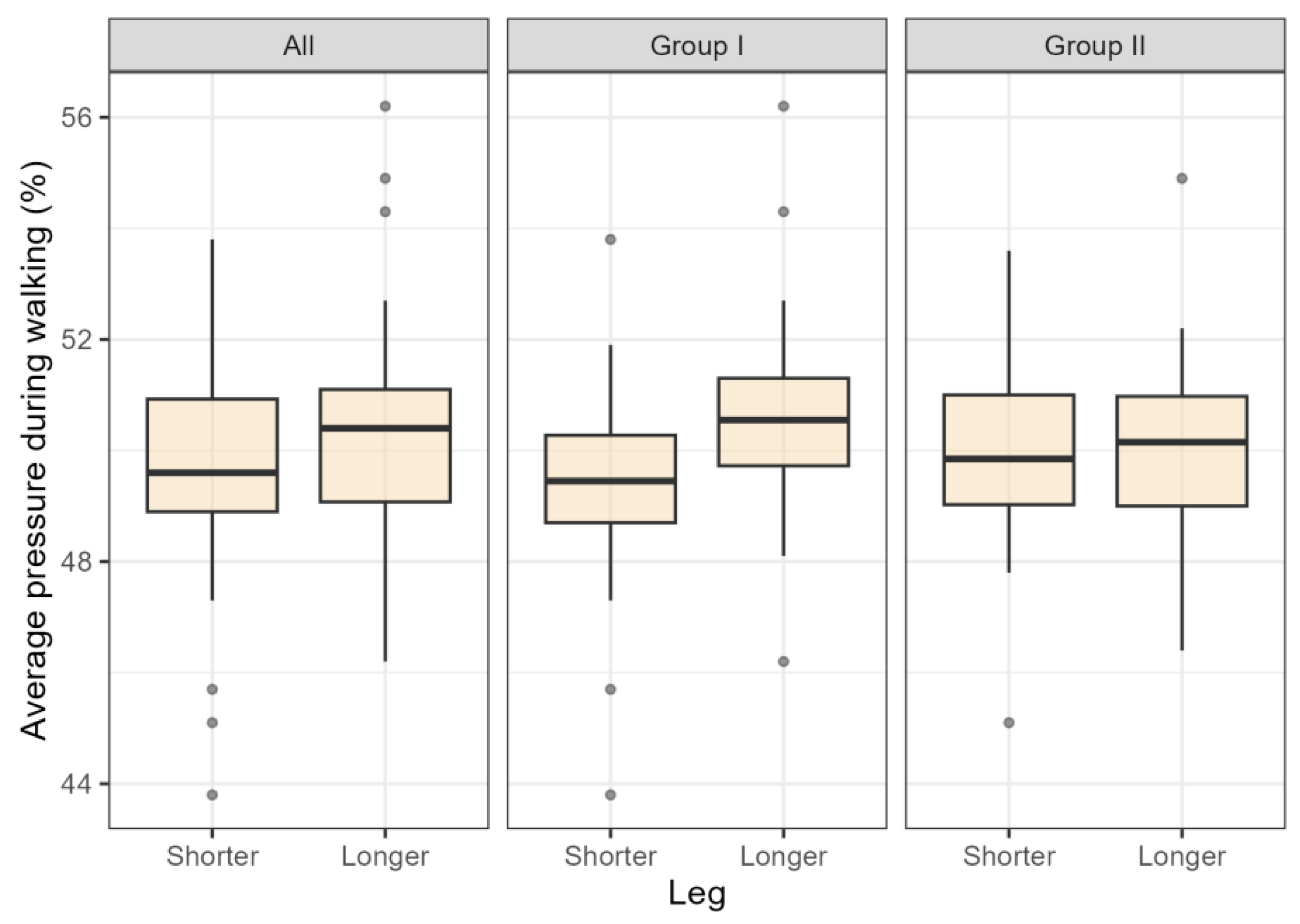
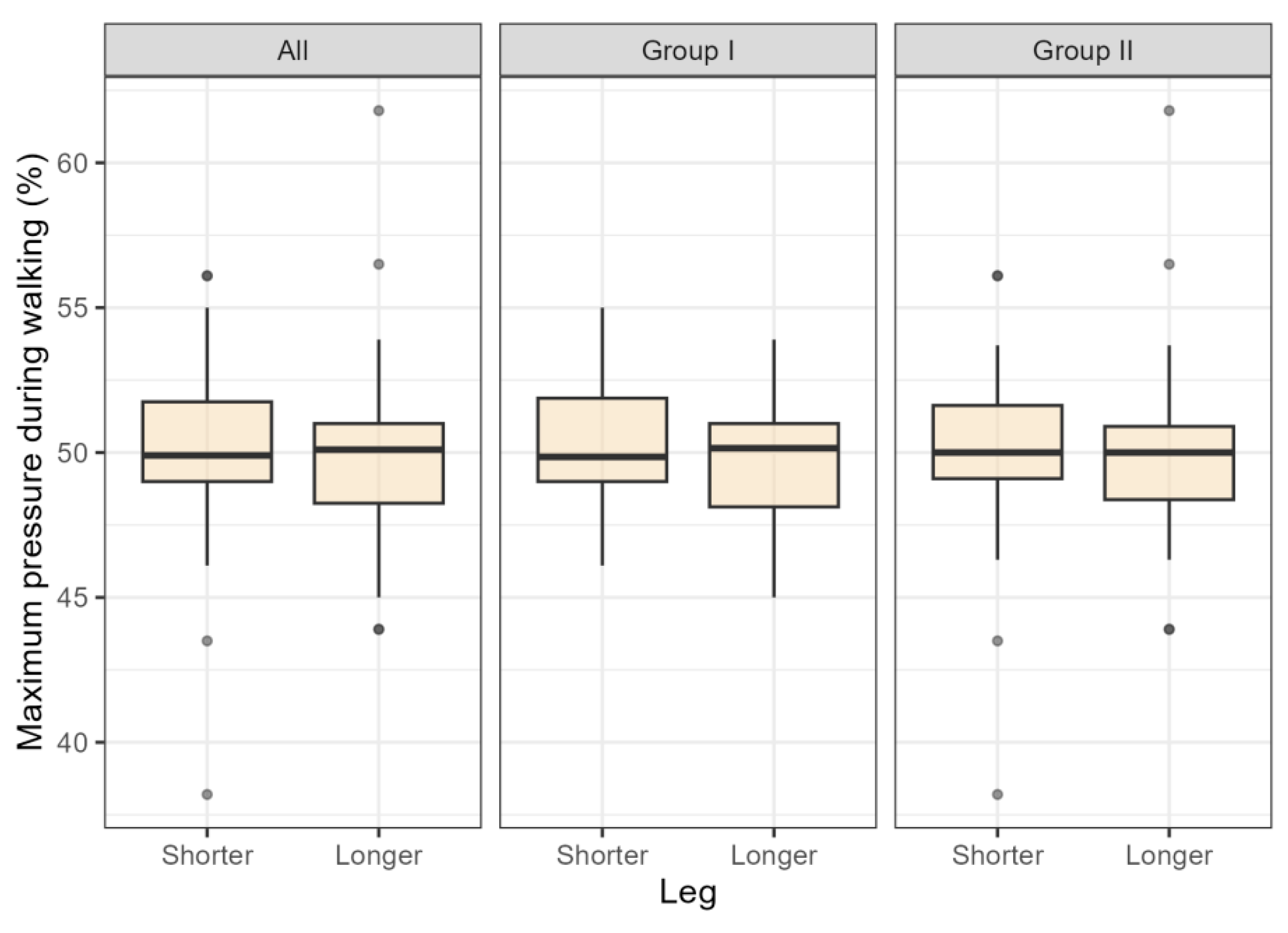
3.2.2. Foot Pressure Distribution (Mean Pressure and Peak Pressure)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| LLD | leg length discrepancy |
| LBP | low back pain |
| COM | centre of mass |
| COP | centre of pressure |
References
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzat, M. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef] [PubMed]
- Patrick, N.; Emanski, E.; Knaub, M.A. Acute and chronic low back pain. Med. Clin. N. Am. 2014, 98, 777–778. [Google Scholar] [CrossRef] [PubMed]
- Golob, A.L.; Wipf, J.E. Low back pain. Med. Clin. N. Am. 2014, 98, 405–428. [Google Scholar] [CrossRef]
- Meucci, R.D.; Fassa, A.G.; Xavier Faria, N.M. Prevalence of chronic low back pain: Systematic review. Rev. Saude Publica 2015, 49, 1. [Google Scholar] [CrossRef]
- Pellisé, F.; Balagué, F.; Rajmil, L.; Cedraschi, C.; Aguirre, M.; Fontecha, C.G.; Pasarín, M.; Ferrer, M. Prevalence of low back pain and its effect on health-related quality of life in adolescents. Arch. Pediatr. Adolesc. Med. 2009, 163, 65–71. [Google Scholar] [CrossRef]
- Jeffries, L.J.; Milanese, S.F.; Grimmer-Somers, K.A. Epidemiology of adolescent spinal pain: A systematic overview of the research literature. Spine 2007, 32, 2630–2637. [Google Scholar] [CrossRef]
- Deyo, R.A.; Rainville, J.; Kent, D.L. What can the history and physical examination tell us about low back pain? JAMA 1992, 268, 760–765. [Google Scholar] [CrossRef]
- Dionne, C.E.; Dunn, K.M.; Croft, P.R. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing 2006, 35, 229–234. [Google Scholar] [CrossRef]
- Queiros, A.F.; Costa, F.G. Leg length discrepancy: A brief review. Port. J. Orthop. Traumatol. 2018, 26, 14–19. [Google Scholar]
- Swaminathan, V.; Cartwright-Terry, M.; Moorehead, J.D.; Bowey, A.; Scott, S.J. The effect of leg length discrepancy upon Pressure distribution in the static phase (standing). Gait Posture 2014, 40, 561–563. [Google Scholar] [CrossRef]
- Bonnet, C.T.; Cherraf, S.; Szaffarczyk, S.; Rougier, P.R. The contribution of body weight distribution and center of pressure location in the control of mediolateral stance. J. Biomech. 2014, 47, 1603–1608. [Google Scholar] [CrossRef] [PubMed]
- Azizan, N.A.; Basaruddin, K.S.; Salleh, A.F.; Sulaiman, A.R.; Safar, M.J.; Rusli, W.M. Leg length discrepancy: Dynamic balance response during gait. J. Health Eng. 2018, 2018, 7815451. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Carmeli, E. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait Posture 2017, 57, 115–123. [Google Scholar] [CrossRef]
- Walsh, M.; Connolly, P.; Jenkinson, A.; O’Brien, T. Leg length discrepancy: An experimental study of compensatory changes in three dimensions using gait analysis. Gait Posture 2000, 12, 156–161. [Google Scholar] [CrossRef]
- D’Amico, M.; Kinel, E.; D’Amico, G.; Roncoletta, P. A 3D Spine and Full Skeleton Model for Opto-Electronic Stereo- Photogrammetric Multi-Sensor Biomechanical Analysis in Posture and Gait. In Innovations in Spinal Deformities and Postural Disorders; INTECH: Rijeka, Croatia, 2017. [Google Scholar]
- D’Amico, M.; Kinel, E.; Roncoletta, P. Normative 3D Opto-Electronic Stereo-Photogrammetric Posture and Spine Morphology Data in Young Healthy Adult Population. PLoS ONE 2017, 12, e0179619. [Google Scholar] [CrossRef]
- Yu, Q.; Huang, H.; Zhang, Z.; Hu, X.; Li, W.; Li, L.; Chen, M.; Liang, Z.; Leung Ambrose Lo, W.; Wang, C. The association between pelvic asymmetry and non-specific chronic low back pain as assessed by the global postural system. BMC Musculoskelet. Disord. 2020, 21, 596. [Google Scholar] [CrossRef]
- White, S.C.; Gilchrist, L.A.; Wilk, B.E. Asymmetric limb Pressureing with true or simulated leg-length differences. Clin. Orthop. Relat. Res. 2004, 421, 287–292. [Google Scholar] [CrossRef]
- Al-Eisa, E.; Egan, D.A.; Wassersug, R. Fluctuating asymmetry and low back pain. Evol. Hum. Behav. 2004, 25, 31–37. [Google Scholar] [CrossRef]
- Grundy, P.F.; Roberts, C.J. Does unequal leg length cause back pain? Lancet 1984, 2, 256–258. [Google Scholar] [CrossRef]
- Knutson, G.A. Incidence of foot rotation, pelvic crest unleveling, and supine leg length alignment asymmetry and their relationship to self-reported back pain. J. Manip. Physiol. Ther. 2002, 25, 110E. [Google Scholar] [CrossRef]
- Levangie, P.K. The association between static pelvic asymmetry and low back pain. Spine 1999, 24, 1234–1242. [Google Scholar] [CrossRef] [PubMed]
- Fann, A.V. The prevalence of postural asymmetry in people with and without chronic low back pain. Arch. Phys. Med. Rehabil. 2002, 83, 1736–1738. [Google Scholar] [CrossRef]
- Al-Eisa, E.; Egan, D.A.; Fenety, A. The association between lateral pelvic tilt and asymmetry in sitting pressure distribution. J. Man. Manip. Ther. 2004, 12, 133–142. [Google Scholar] [CrossRef]
- Lund, T.; Nydegger, T.; Schlenzka, D.; Oxland, T.R. Three-dimensional motion patterns during active bending in patients with chronic low back pain. Spine 2002, 27, 1865–1874. [Google Scholar] [CrossRef] [PubMed]
- Al-Eisa, E.; Egan, D.A.; Deluzio, K.; Wassersug, R. Effects of Pelvic Asymmetry and Low Back Pain on Trunk Kinematics During Sitting: A Comparison with Standing. Spine 2006, 31, E135–E143. [Google Scholar] [CrossRef] [PubMed]
- Friberg, O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine 1983, 8, 643–651. [Google Scholar] [CrossRef]
- Kendall, J.C.; Birdb, A.R.; Azari, M.F. Foot posture, leg length discrepancy and low back pain—Their relationship and clinical management using foot orthoses—An overview. Foot 2014, 24, 75–80. [Google Scholar] [CrossRef]
- Defrin, R.; Ben Benyamin, S.; Aldubi, R.D.; Pick, C.G. Conservative correction of LegLength discrepancies of 10mm or less for the relief of chronic low back Pain. Arch. Phys. Med. Rehabil. 2005, 86, 2075–2080. [Google Scholar] [CrossRef]
- Applebaum, A.; Nessim, A.; Cho, W. Overwiew and Spinal Implications of Leg Lenght Discrepancy: Narrative Review. Clin. Orthop. Surg. 2021, 13, 127–134. [Google Scholar] [CrossRef]
- King, A.C.; Wang, Z.; Newell, K.M. Asymmetry of recurrent dynamics as a function of postural stance. Exp. Brain Res. 2012, 220, 239–250. [Google Scholar] [CrossRef]
- Pereiro-Buceta, H.; Calvo-Lobo, C.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Romero-Morales, C.; López-López, D.; Martínez-Jiménez, E.-M. Intra and intersession repeatability and reliability of dynamic parameters in pressure platform assessments on subjects with simulated leg length discrepancy. A cross-sectional research. Sao Paulo Med. J. 2021, 139, 424–434. [Google Scholar] [CrossRef] [PubMed]
- Pereiro-Buceta, H.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; López-López, D.; Navarro-Flores, E.; Martínez-Jiménez, E.M.; Martiniano, J.; Calvo-Lobo, C. The Effect of Simulated Leg-Length Discrepancy on the Dynamic Parameters of the Feet during Gait—Cross-Sectional Research. Healthcare 2021, 9, 932. [Google Scholar] [CrossRef] [PubMed]
- Betsch, M.; Wild, M.; Große, B.; Rapp, W.; Horstmann, T. The effect of simulating leg length inequality on spinal posture and pelvic position: A dynamic rasterstereographic analysis. Eur. Spine J. 2012, 21, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Vella, S.P.; Swain, M.; Downie, A.; Howarth, S.J.; Funabashi, M.; Engel, R.M. Induced leg length inequality affects pelvis orientation during upright standing immediately following a sit-to-stand transfer: A pre-post measurement study. BMC Musculoskelet. Disord. 2023, 24, 203. [Google Scholar] [CrossRef]
- De Bengoa Vallejo, R.B.; Iglesias, M.E.L.; Zeni, J.; Thomas, S. Reliability and Repeatability of the Portable EPS-Platform Digital Pressure-Plate System. J. Am. Podiatr. Med. Assoc. 2004, 103, 197–203. [Google Scholar]
- Lorkowski, J.; Gawronska, K. Pedobarography in Physiotherapy: A Narrative Review on Current Knowledge. Adv. Exp. Med. Biol. 2022, 1375, 13–22. [Google Scholar]
- Klöpfer-Krämer, I.; Brand, A.; Wackerle, H.; Müßig, J.; Kröger, I.; Augat, P. Gait analysis—Available platforms for outcome assessment. Injury 2020, 51 (Suppl. 2), S90–S96. [Google Scholar] [CrossRef]
- D’Amico, M.; Roncoletta, P.; Di Felice, F.; Porto, D.; Bellomo, R.; Saggini, R. LBP and lower limb discrepancy: 3D evaluation of postural rebalancing via underfoot wedge correction. Stud. Health Technol. Inform. 2012, 176, 108–112. [Google Scholar]
- Steele, J. Handedness in past human populations: Skeletal markers. Laterality 2000, 5, 193–220. [Google Scholar] [CrossRef]
- Lazenby, R.A. Skeletal biology, functional asymmetry and the origins of handedness. J. Theor. Biol. 2002, 218, 129–138. [Google Scholar] [CrossRef]
- Plochocki, J.H. Bilateral variation in limb articular surface dimensions. Am. J. Hum. Biol. 2004, 16, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Sládek, V.; Berner, M.; Sosna, D.; Sailer, R. Human manipulative behavior in the Central European Late Eneolithic and Early Bronze Age: Humeral bilateral asymmetry. Am. J. Phys. Anthropol. 2007, 133, 669–681. [Google Scholar] [CrossRef]
- Giles, L.; Singer, K. Clinical Anatomy and Management of Low Back Pain; Butterworth Heinemann: Oxford, UK, 1997; Volume 1, 411p, ISBN 0 7506 2305 0. [Google Scholar]
- Knutson, G.A. Anatomic and functional leg-length inequality: A review and recommendation for clinical decision-making. Part, I.; anatomic leg-length inequality: Prevalence, magnitude, effects and clinical significance. Chiropr. Osteopat. 2005, 13, 11. [Google Scholar] [CrossRef]
- Hamada, T.; Matsubara, H.; Kato, S.; Hikichi, T.; Shimokawa, K.; Demura, S.; Tsuchiya, H. Correlation Analysis between Leg-length Discrepancy and Lumbar Scoliosis Using Full-length Standing Radiographs. Strateg. Trauma Limb Reconstr. 2022, 17, 144–147. [Google Scholar]
- Golightly, Y.M.; Tate, J.J.; Burns, C.B.; Gross, M.T. Changes in pain and disability secondary to shoe lift intervention in subjects with limb length inequality and chronic low back pain: A preliminary report. J. Orthop. Sports Phys. Ther. 2007, 37, 380–388. [Google Scholar] [CrossRef]
- Gofton, J.P. Persistent low back pain and leg length disparity. J. Rheumatol. 1985, 12, 747–750. [Google Scholar]
- Helliwell, M. Leg length inequality and low back pain. Pract. Tioner. 1985, 229, 483–485. [Google Scholar]
- Menez, C.; L’Hermette, M.; Coquart, J. Orthotic Insoles Improve Gait Symmetry and Reduce Immediate Pain in Subjects with Mild Leg Length Discrepancy. Front. Sports Act. Living 2020, 2, 579152. [Google Scholar] [CrossRef] [PubMed]
- Menez, C.; Coquart, J.; Dodelin, D.; Tourny, C.; L’Hermette, M. Effects of Orthotic Insoles on Gait Kinematics and Low-Back Pain in Patients with Mild Leg Length Discrepancy. J. Am. Podiatr. Med. Assoc. 2021, 111, 1–10. [Google Scholar] [CrossRef]
- Mannello, D.M. Leg Length Inequality. J. Manip. Physiol. Ther. 1992, 15, 576–590. [Google Scholar]
- Perttunen, J.R.; Anttila, E.; Södergård, J.; Merikanto, J.; Komi, P.V. Gait asymmetry in patients with limb length discrepancy. Scand. J. Med. Sci. Sports 2004, 14, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Rannisto, S.; Okuloff, A.; Uitti, J.; Paananen, M.; Rannisto, P.-H.; Malmivaara, A.; Karppinen, J. Leg-length Discrepancy Is Associated with Low Back Pain Among Those Who Must Stand while Working. BMC Musculoskelet. Disord. 2015, 16, 110. [Google Scholar] [CrossRef] [PubMed]



| Test | Measurement | Leg/Side | NA | Min | Q1 | Median | Q3 | Max | Mean | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| Standing | Pressure | Shorter | 60 | 23.8 | 46.1 | 49.1 | 52.2 | 70.9 | 48.15 | 8.27 |
| Longer | 60 | 29.1 | 47.8 | 51.0 | 53.9 | 76.2 | 51.85 | 8.27 | ||
| Angle of foot abduction | Shorter | 60 | 0.7 | 8.7 | 11.5 | 16.6 | 36.7 | 12.83 | 7.23 | |
| Longer | 60 | 0.0 | 6.1 | 8.9 | 14.3 | 30.1 | 11.04 | 7.47 | ||
| Walking | Foot contact time | Shorter | 60 | 559.9 | 839.8 | 901.3 | 993.5 | 1523.0 | 914.99 | 149.58 |
| Longer | 60 | 514.3 | 847.0 | 929.0 | 1024.2 | 1763.3 | 938.32 | 194.18 | ||
| Mean pressure | Shorter | 60 | 34.4 | 87.0 | 108.0 | 128.9 | 175.6 | 105.40 | 34.64 | |
| Longer | 60 | 37.6 | 87.8 | 110.2 | 131.7 | 163.6 | 106.13 | 33.39 | ||
| Peak pressure | Shorter | 60 | 65.4 | 204.9 | 287.4 | 343.5 | 613.5 | 279.50 | 118.73 | |
| Longer | 60 | 69.2 | 201.5 | 273.9 | 341.3 | 764.8 | 278.57 | 123.66 |
| Test | Measurement | Leg/Side | NP | Min | Q1 | Median | Q3 | Max | Mean | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| Standing | Pressure | Shorter | 30 | 26 | 41.975 | 49.95 | 53.475 | 65.4 | 48.22 | 9.43 |
| Longer | 30 | 34.6 | 46.525 | 50.05 | 58.025 | 74 | 51.78 | 9.43 | ||
| Angle of foot abduction | Shorter | 30 | 0.9 | 10.3 | 13.35 | 17.6 | 31.2 | 14.40 | 6.52 | |
| Longer | 30 | 0 | 7.65 | 9.2 | 14.15 | 30 | 11.12 | 6.29 | ||
| Walking | Foot contact time | Shorter | 30 | 559.9 | 862.35 | 901.25 | 1018.3 | 1523 | 947.95 | 169.05 |
| Longer | 30 | 514.3 | 898.63 | 939.75 | 1034.8 | 1763.3 | 978.17 | 229.07 | ||
| Average pressure | Shorter | 30 | 40.4 | 102.93 | 116.2 | 130.23 | 175.6 | 115.85 | 26.57 | |
| Longer | 30 | 41.6 | 103.03 | 118.6 | 131.95 | 163.3 | 118.07 | 25.73 | ||
| Maximum pressure | Shorter | 30 | 65.4 | 272.45 | 300.65 | 356.98 | 547.7 | 307.45 | 95.41 | |
| Longer | 30 | 69.2 | 269.93 | 302.55 | 345.53 | 491 | 303.07 | 87.39 |
| Test | Measurement | Leg/Side | NwP | Min | Q1 | Median | Q3 | Max | Mean | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| Standing | Pressure | Shorter | 30 | 23.8 | 47.1 | 48.2 | 49.925 | 70.9 | 48.08 | 7.09 |
| Longer | 30 | 29.1 | 50.075 | 51.8 | 52.9 | 76.2 | 51.92 | 7.09 | ||
| Angle of foot abduction | Shorter | 30 | 0.7 | 7.5 | 10.05 | 13.15 | 36.7 | 11.26 | 7.67 | |
| Longer | 30 | 1.1 | 4.175 | 7.85 | 14.525 | 30.1 | 10.95 | 8.61 | ||
| Walking | Foot contact time | Shorter | 30 | 608.8 | 798.45 | 898 | 956.75 | 1114.5 | 882.03 | 121.22 |
| Longer | 30 | 516.2 | 833.15 | 913.95 | 1006.8 | 1153.3 | 898.47 | 144.74 | ||
| Mean pressure | Shorter | 30 | 34.4 | 75.925 | 90.9 | 126.05 | 171.8 | 94.95 | 38.84 | |
| Longer | 30 | 37.6 | 74.85 | 89.8 | 129 | 163.6 | 94.19 | 36.22 | ||
| Maximum pressure | Shorter | 30 | 71.9 | 165.35 | 221.1 | 324.48 | 613.5 | 251.55 | 134.02 | |
| Longer | 30 | 73.7 | 164.43 | 217.2 | 304.45 | 764.8 | 254.07 | 149.10 |
| Loading, Shorter Leg | Loading, Longer Leg | p | |||
|---|---|---|---|---|---|
| Mean [%] | SD [%] | Mean [%] | SD [%] | ||
| All participants NA = 60; 100% | 48.15 | 8.274 | 51.85 | 8.274 | 0.022 |
| Group 1 (with LBP, NP = 30; 50%) | 48.22 | 9.434 | 51.78 | 9.434 | 0.359 |
| Group 2 (without LBP, NwP = 30; 50%) | 48.08 | 7.089 | 51.92 | 7.089 | 0.002 |
| Group 1 (with LBP, NP = 30) | Group 2 (without LBP, NwP = 30) | p | |||
| Mean [%] | SD [%] | Mean [%] | SD [%] | ||
| Loading, shorter leg | 48.22 | 9.434 | 48.08 | 7.089 | 0.231 |
| Loading, longer leg | 51.78 | 9.434 | 51.92 | 7.089 | 0.231 |
| Abduction Shorter Leg | Abduction Longer Leg | p | |||
|---|---|---|---|---|---|
| Mean [°] | SD [°] | Mean [°] | SD [°] | ||
| All participants NA = 60; 100% | 12.83 | 7.229 | 11.04 | 7.474 | 0.065 |
| Group 1 (with LBP, NP = 30; 50%) | 14.4 | 6.515 | 11.12 | 6.291 | 0.054 |
| Group 2 (without LBP, NwP = 30; 50%) | 11.26 | 7.667 | 10.95 | 8.606 | 0.451 |
| Group 1 (with LBP, NP = 30) | Group 2 (without LBP, NwP = 30) | p | |||
| Mean [°] | SD [°] | Mean [°] | SD [°] | ||
| Abduction, shorter leg | 14.4 | 6.515 | 11.26 | 7.667 | 0.022 |
| Abduction, longer leg | 11.12 | 6.291 | 10.95 | 8.606 | 0.340 |
| Contact Time, Shorter Leg | Contact Time, Longer Leg | p | |||
|---|---|---|---|---|---|
| Mean [ms] | SD [ms] | Mean [ms] | SD [ms] | ||
| All participants NA = 60; 100% | 915 | 149.6 | 938.3 | 194.2 | 0.305 |
| Group 1 (with LBP, NP = 30; 50%) | 947.9 | 169.1 | 978.2 | 229.1 | 0.390 |
| Group 2 (without LBP, NwP = 30; 50%) | 882 | 121.2 | 898.5 | 144.7 | 0.562 |
| Group 1 (with LBP, NP = 30) | Group 2 (without LBP, NwP = 30) | p | |||
| Mean [ms] | SD [ms] | Mean [ms] | SD [ms] | ||
| Contact time, shorter leg | 947.9 | 169.1 | 882 | 121.2 | 0.150 |
| Contact time, longer leg | 978.2 | 229.1 | 898.5 | 144.7 | 0.208 |
| Mean Pressure, Shorter Leg | Mean Pressure, Longer Leg | p | |||
|---|---|---|---|---|---|
| Mean [%] | SD [%] | Mean [%] | SD [%] | ||
| All participants NA = 60; 100% | 49.7 | 1.747 | 50.3 | 1.747 | 0.101 |
| Group 1 (with LBP, NP = 30; 50%) | 49.46 | 1.890 | 50.54 | 1.890 | 0.031 |
| Group 2 (without LBP, NwP = 30; 50%) | 49.93 | 1.589 | 50.07 | 1.589 | 0.976 |
| Group 1 (with LBP, NP = 30) | Group 2 (without LBP, NwP = 30) | p | |||
| Mean [%] | SD [%] | Mean [%] | SD [%] | ||
| Mean pressure, shorter leg | 49.46 | 1.890 | 49.93 | 1.589 | 0.284 |
| Mean pressure, longer leg | 50.54 | 1.890 | 50.07 | 1.589 | 0.284 |
| Peak Pressure, Shorter Leg | Peak Pressure, Longer Leg | p | |||
|---|---|---|---|---|---|
| Mean [%] | SD [%] | Mean [%] | SD [%] | ||
| All participants NA = 60; 100% | 50.09 | 2.797 | 49.91 | 2.797 | 0.530 |
| Group 1 (with LBP, NP = 30; 50%) | 50.19 | 2.045 | 49.81 | 2.045 | 0.888 |
| Group 2 (without LBP, NwP = 30; 50%) | 49.99 | 3.422 | 50.01 | 3.422 | 0.530 |
| Group 1 (with LBP, NP = 30) | Group 2 (without LBP, NwP = 30) | p | |||
| Mean [%] | SD [%] | Mean [%] | SD [%] | ||
| Peak pressure, shorter leg | 50.19 | 2.045 | 49.99 | 3.422 | 0.734 |
| Peak pressure, longer leg | 49.81 | 2.045 | 50.01 | 3.422 | 0.734 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konior, K.; Bitenc-Jasiejko, A.; Lubkowska, A.; Stachowska, E.; Walińska, A.; Gonta, K.; Skomro, P.; Lietz-Kijak, D. Characteristics of Foot Pressure Distribution During Standing and Walking with Anatomical Leg Length Discrepancy—A Comparative Analysis of Patients with and Without Low Back Pain. Symmetry 2025, 17, 1059. https://doi.org/10.3390/sym17071059
Konior K, Bitenc-Jasiejko A, Lubkowska A, Stachowska E, Walińska A, Gonta K, Skomro P, Lietz-Kijak D. Characteristics of Foot Pressure Distribution During Standing and Walking with Anatomical Leg Length Discrepancy—A Comparative Analysis of Patients with and Without Low Back Pain. Symmetry. 2025; 17(7):1059. https://doi.org/10.3390/sym17071059
Chicago/Turabian StyleKonior, Krzysztof, Aleksandra Bitenc-Jasiejko, Anna Lubkowska, Ewa Stachowska, Anna Walińska, Kinga Gonta, Piotr Skomro, and Danuta Lietz-Kijak. 2025. "Characteristics of Foot Pressure Distribution During Standing and Walking with Anatomical Leg Length Discrepancy—A Comparative Analysis of Patients with and Without Low Back Pain" Symmetry 17, no. 7: 1059. https://doi.org/10.3390/sym17071059
APA StyleKonior, K., Bitenc-Jasiejko, A., Lubkowska, A., Stachowska, E., Walińska, A., Gonta, K., Skomro, P., & Lietz-Kijak, D. (2025). Characteristics of Foot Pressure Distribution During Standing and Walking with Anatomical Leg Length Discrepancy—A Comparative Analysis of Patients with and Without Low Back Pain. Symmetry, 17(7), 1059. https://doi.org/10.3390/sym17071059









