Asymmetry in Muscle Strength, Dynamic Balance, and Range of Motion in Adult Symptomatic Hip Dysplasia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Participants
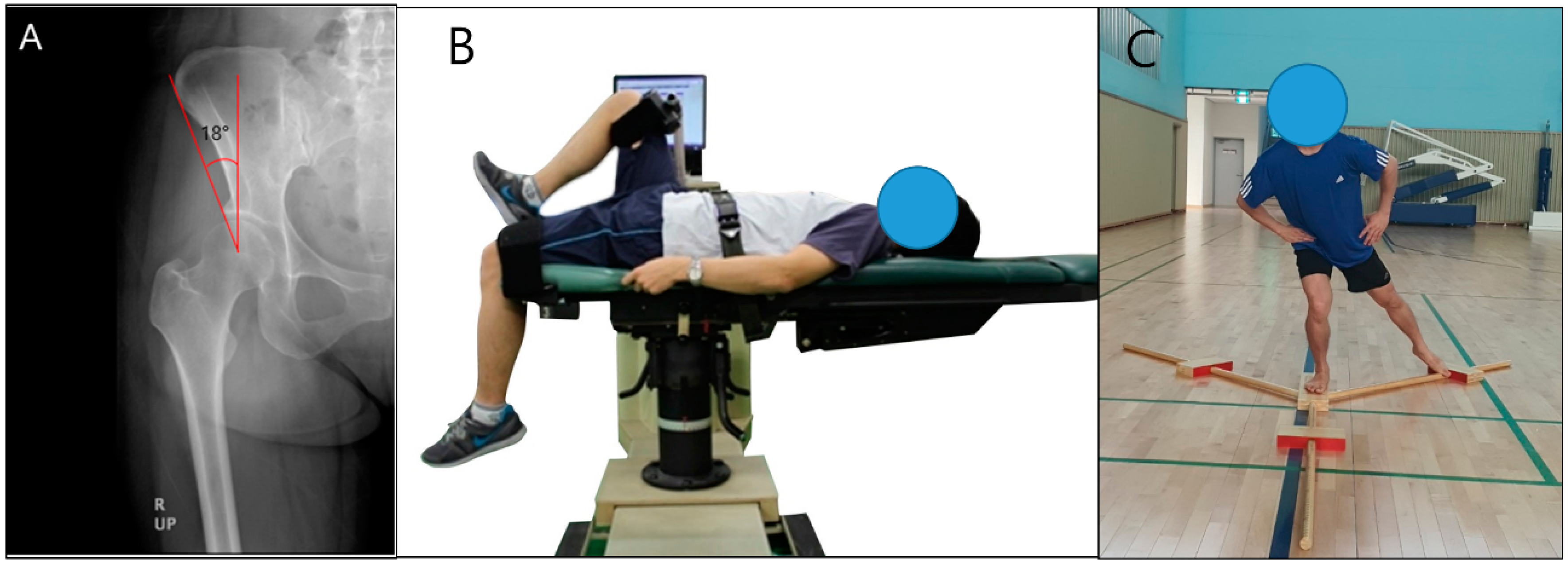
2.3. Isokinetic Strength Test
2.4. Dynamic Balance Test
2.5. Range of Motion Measurement
2.6. Subjective Hip Scoring Questionnaire
2.7. Data Analysis
3. Results
3.1. General Characteristics of Participants
3.2. Hip Morphology Angle, Pain, and Range of Motion
3.3. Y-Balance Test of Healthy Participants and Patients with Hip Dysplasia
3.4. Isokinetic Hip Strength of Healthy Participants and Patients with Hip Dysplasia
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schmitz, M.R.; Murtha, A.S.; Clohisy, J.C.; Group, A.S. Developmental dysplasia of the hip in adolescents and young adults. JAAOS J. Am. Acad. Orthop. Surg. 2020, 28, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Dezateux, C.; Rosendahl, K. Developmental dysplasia of the hip. Lancet 2007, 369, 1541–1552. [Google Scholar] [CrossRef] [Green Version]
- Storer, S.K.; Skaggs, D.L. Developmental dysplasia of the hip. Am. Fam. Physician 2006, 74, 1310–1316. [Google Scholar] [PubMed]
- Gala, L.; Clohisy, J.C.; Beaule, P.E. Hip Dysplasia in the Young Adult. J. Bone Jt. Surg. Am. Vol. 2016, 98, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Kolb, A.; Schweiger, N.; Mailath-Pokorny, M.; Kaider, A.; Hobusch, G.; Chiari, C.; Windhager, R. Low incidence of early developmental dysplasia of the hip in universal ultrasonographic screening of newborns: Analysis and evaluation of risk factors. Int. Orthop. 2016, 40, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.; McCaul, K.A.; Cundy, P.J.; Haan, E.A.; Byron-Scott, R. Perinatal risk factors for developmental dysplasia of the hip. Arch. Dis. Child. -Fetal Neonatal Ed. 1997, 76, F94–F100. [Google Scholar] [CrossRef] [PubMed]
- Cady, R.B. Developmental dysplasia of the hip: Definition, recognition, and prevention of late sequelae. Pediatric Ann. 2006, 35, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Bache, C.E.; Clegg, J.; Herron, M. Risk factors for developmental dysplasia of the hip: Ultrasonographic findings in the neonatal period. J. Pediatric Orthop. B 2002, 11, 212–218. [Google Scholar]
- Sanchez-Sotelo, J.; Berry, D.J.; Trousdale, R.T.; Cabanela, M.E. Surgical treatment of developmental dysplasia of the hip in adults: II. Arthroplasty options. JAAOS J. Am. Acad. Orthop. Surg. 2002, 10, 334–344. [Google Scholar] [CrossRef] [PubMed]
- Hunt, D.; Prather, H.; Harris Hayes, M.; Clohisy, J.C. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders. PM&R J. Inj. Funct. Rehabil. 2012, 4, 479–487. [Google Scholar] [CrossRef] [Green Version]
- Mortensen, L.; Schultz, J.; Elsner, A.; Jakobsen, S.S.; Søballe, K.; Jacobsen, J.S.; Kierkegaard, S.; Dalgas, U.; Mechlenburg, I. Progressive resistance training in patients with hip dysplasia: A feasibility study. J. Rehabil. Med. 2018, 50, 751–758. [Google Scholar] [CrossRef] [Green Version]
- Nunley, R.M.; Prather, H.; Hunt, D.; Schoenecker, P.L.; Clohisy, J.C. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. JBJS 2011, 93, 17–21. [Google Scholar] [CrossRef] [Green Version]
- Marangoz, S.; Atilla, B.; Gök, H.; Yavuzer, G.; Ergin, S.; Tokgözoğlu, A.M.; Alpaslan, M. Gait analysis in adults with severe hip dysplasia before and after total hip arthroplasty. Hip Int. 2010, 20, 466–472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hampton, S.; Nakonezny, P.; Richard, H.; Wells, J. Pain catastrophizing, anxiety, and depression in hip pathology. Bone Jt. J. 2019, 101, 800–807. [Google Scholar] [CrossRef]
- Matsuda, D.K.; Wolff, A.B.; Nho, S.J.; Salvo, J.P., Jr.; Christoforetti, J.J.; Kivlan, B.R.; Ellis, T.J.; Carreira, D.S.; Multicenter Arthroscopic Study of the Hip (MASH) Study Group. Hip dysplasia: Prevalence, associated findings, and procedures from large multicenter arthroscopy study group. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Scott, E.J.; Willey, M.C.; Mercado, A.; Davison, J.; Wilken, J.M. Assessment of disability related to hip dysplasia using objective measures of physical performance. Orthop. J. Sports Med. 2020, 8, 2325967120903290–2325967120903298. [Google Scholar] [CrossRef] [PubMed]
- Martin, H.D.; Kelly, B.T.; Leunig, M.; Philippon, M.J.; Clohisy, J.C.; Martin, R.L.; Sekiya, J.K.; Pietrobon, R.; Mohtadi, N.G.; Sampson, T.G. The pattern and technique in the clinical evaluation of the adult hip: The common physical examination tests of hip specialists. Arthrosc. J. Arthrosc. Relat. Surg. 2010, 26, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Sucato, D.J.; Tulchin, K.; Shrader, M.W.; DeLaRocha, A.; Gist, T.; Sheu, G. Gait, hip strength and functional outcomes after a Ganz periacetabular osteotomy for adolescent hip dysplasia. J. Pediatric Orthop. 2010, 30, 344–350. [Google Scholar] [CrossRef]
- Jacobsen, J.S.; Jakobsen, S.S.; Søballe, K.; Hölmich, P.; Thorborg, K. Isometric hip strength impairments in patients with hip dysplasia are improved but not normalized 1 year after periacetabular osteotomy: A cohort study of 82 patients. Acta Orthop. 2021, 92, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Zapparoli, F.Y.; Riberto, M. Isokinetic evaluation of the hip flexor and extensor muscles: A systematic review. J. Sport Rehabil. 2017, 26, 556–566. [Google Scholar] [CrossRef]
- Martin, H.D.; Palmer, I.J. History and physical examination of the hip: The basics. Curr. Rev. Musculoskelet. Med. 2013, 6, 219–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunt, D.; Clohisy, J.; Prather, H. Acetabular labral tears of the hip in women. Phys. Med. Rehabil. Clin. North Am. 2007, 18, 497–520. [Google Scholar] [CrossRef] [PubMed]
- LaPrade, M.D.; Melugin, H.P.; Hale, R.F.; Leland, D.P.; Bernard, C.D.; Sierra, R.J.; Trousdale, R.T.; Levy, B.A.; Krych, A.J. Incidence of hip dysplasia diagnosis in young patients with hip pain: A geographic population cohort analysis. Orthop. J. Sports Med. 2021, 9, 2325967121989087–2325967121989093. [Google Scholar] [CrossRef] [PubMed]
- Vaudreuil, N.J.; McClincy, M.P. Evaluation and treatment of borderline dysplasia: Moving beyond the lateral center edge angle. Curr. Rev. Musculoskelet. Med. 2020, 13, 28–37. [Google Scholar] [CrossRef] [PubMed]
- CSMi. Humac Norm Users Guide; Computer Sports Medicine, Inc.: Stoughton, MA, USA, 2019. [Google Scholar]
- Dvir, Z. Isokinetics: Muscle Testing, Interpretation, and Clinical Applications, 2nd ed.; Churchill Livingstone: London, UK, 2004. [Google Scholar]
- Powden, C.J.; Dodds, T.K.; Gabriel, E.H. The reliability of the star excursion balance test and lower quarter Y-balance test in healthy adults: A systematic review. Int. J. Sports Phys. Ther. 2019, 14, 683–694. [Google Scholar] [CrossRef]
- Thorborg, K.; Hölmich, P.; Christensen, R.; Petersen, J.; Roos, E.M. The Copenhagen Hip and Groin Outcome Score (HAGOS): Development and validation according to the COSMIN checklist. Br. J. Sports Med. 2011, 45, 478–491. [Google Scholar] [CrossRef] [Green Version]
- Thomeé, R.; Jónasson, P.; Thorborg, K.; Sansone, M.; Ahldén, M.; Thomeé, C.; Karlsson, J.; Baranto, A. Cross-cultural adaptation to Swedish and validation of the Copenhagen Hip and Groin Outcome Score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 835–842. [Google Scholar] [CrossRef] [Green Version]
- Jacobsen, J.S.; Hölmich, P.; Thorborg, K.; Bolvig, L.; Jakobsen, S.S.; Søballe, K.; Mechlenburg, I. Muscle-tendon-related pain in 100 patients with hip dysplasia: Prevalence and associations with self-reported hip disability and muscle strength. J. Hip Preserv. Surg. 2018, 5, 39–46. [Google Scholar] [CrossRef] [Green Version]
- Sørensen, H.; Nielsen, D.B.; Jacobsen, J.S.; Søballe, K.; Mechlenburg, I. Isokinetic dynamometry and gait analysis reveal different hip joint status in patients with hip dysplasia. Hip Int. 2019, 29, 215–221. [Google Scholar] [CrossRef]
- Casartelli, N.; Maffiuletti, N.; Item-Glatthorn, J.; Staehli, S.; Bizzini, M.; Impellizzeri, F.; Leunig, M. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthr. Cartil. 2011, 19, 816–821. [Google Scholar] [CrossRef] [Green Version]
- Arokoski, M.H.; Arokoski, J.P.; Haara, M.; Kankaanpää, M.; Vesterinen, M.; Niemitukia, L.H.; Helminen, H.J. Hip muscle strength and muscle cross sectional area in men with and without hip osteoarthritis. J. Rheumatol. 2002, 29, 2185–2195. [Google Scholar] [PubMed]
- Sucato, D.J.; Tulchin-Francis, K.; de La Rocha, A.; Kulkarni, V.; Podeszwa, D.A. Improved functional outcome with no decrease in hip strength 2 years following Ganz periacetabular osteotomies for adolescent hip dysplasia. J. Pediatric Orthop. B 2015, 24, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, D.; Maeyama, A.; Naito, M.; Moriyama, S.; Yoshimura, I.; Nakamura, Y.; Kiyama, T. Dynamic hip stability, strength and pain before and after hip abductor strengthening exercises for patients with dysplastic hips. Isokinet. Exerc. Sci. 2013, 21, 95–100. [Google Scholar] [CrossRef]
- Sipe, C.L.; Ramey, K.D.; Plisky, P.P.; Taylor, J.D. Y-balance test: A valid and reliable assessment in older adults. J. Aging Phys. Act. 2019, 27, 663–669. [Google Scholar] [CrossRef]
- Wilson, B.R.; Robertson, K.E.; Burnham, J.M.; Yonz, M.C.; Ireland, M.L.; Noehren, B. The relationship between hip strength and the Y balance test. J. Sport Rehabil. 2018, 27, 445–450. [Google Scholar] [CrossRef] [Green Version]
- Kumar, D.; Wyatt, C.R.; Lee, S.; Nardo, L.; Link, T.M.; Majumdar, S.; Souza, R.B. Association of cartilage defects, and other MRI findings with pain and function in individuals with mild–moderate radiographic hip osteoarthritis and controls. Osteoarthr. Cartil. 2013, 21, 1685–1692. [Google Scholar] [CrossRef] [Green Version]
- Jacobsen, S.; Rømer, L.; Søballe, K. The other hip in unilateral hip dysplasia. Clin. Orthop. Relat. Res. 2006, 446, 239–246. [Google Scholar] [CrossRef]
- Loder, R.T.; Skopelja, E.N. The epidemiology and demographics of hip dysplasia. Int. Sch. Res. Not. 2011, 2011, 1–46. [Google Scholar] [CrossRef] [Green Version]
| Healthy (n = 30) | HD (n = 46) | p-Value | Healthy (n = 40) | HD (n = 49) | p-Value | |
|---|---|---|---|---|---|---|
| Age, years | 35.4 ± 3.4 | 36.2 ± 13.6 | 0.234 | 34.9 ± 5.2 | 35.5 ± 10.8 | 0.376 |
| Height, cm | 172.7 ± 4.9 | 174.1 ± 7.3 | 0.429 | 162.9 ± 3.5 | 161.5 ± 4.7 | 0.088 |
| Weight, kg | 73.7 ± 11.1 | 74.2 ± 13.1 | 0.661 | 56.8 ± 7.1 | 57.2 ± 9.1 | 0.920 |
| BMI, kg/m2 | 24.7 ± 3.6 | 24.4 ± 3.5 | 0.343 | 21.0 ± 2.4 | 21.9 ± 3.2 | 0.584 |
| HD Bilateral, n (%) | – | 39 (84.8%) | – | – | 41 (83.7%) | – |
| HD Unilateral, n (%) | – | 7 (15.2%) | – | – | 8 (16.3%) | – |
| Pain duration, month | – | 7.2 ± 1.6 | – | – | 5.1 ± 2.1 | – |
| HAGOS total score | 97.5 ± 1.2 | 49.5 ± 22.3 | <0.001 | 97.1 ± 1.4 | 49.8 ± 21.5 | <0.001 |
| Symptoms | 97.4 ± 0.9 | 57.4 ± 19.4 | <0.001 | 98.1 ± 1.0 | 65.8 ± 18.6 | <0.001 |
| Pain | 97.0 ± 1.3 | 62.8 ± 15.4 | <0.001 | 96.3 ± 2.0 | 55.4 ± 22.5 | <0.001 |
| ADL | 98.1 ± 1.0 | 58.6 ± 21.6 | <0.001 | 96.4 ± 1.8 | 60.6 ± 17.1 | <0.001 |
| Sport and recreation | 98.3 ± 0.9 | 40.4 ± 25.0 | <0.001 | 97.0 ± 1.3 | 35.9 ± 21.0 | <0.001 |
| Physical activity | 97.5 ± 1.3 | 42.0 ± 24.1 | <0.001 | 98.8 ± 1.1 | 40.1 ± 23.8 | <0.001 |
| Quality of life | 98.0 ± 1.1 | 35.1 ± 28.3 | <0.001 | 95.9 ± 2.1 | 41.2 ± 26.5 | <0.001 |
| Variables | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Healthy | HDast | HDst | p-Value | Healthy | HDast | HDst | p-Value | |
| LCEA, degree | 37.0 ± 5.8 | 18.8 ± 2.7 a | 16.3 ± 2.5 b,c | <0.001 | 38.1 ± 5.9 | 17.9 ± 2.9 a | 16.7 ± 2.3 b,c | <0.001 |
| VAS | 1.3 ± ±0.4 | 2.2 ± 0.9 | 5.7 ± 1.5 b,c | <0.001 | 1.2 ± 0.7 | 2.7 ± 1.1 | 5.9 ± 1.7 b,c | <0.001 |
| ROM, degree | ||||||||
| Flexion | 134.2 ± 12.1 | 132.4 ± 12.6 | 118.4 ± 18.8 b,c | <0.001 | 142.1 ± 14.9 | 135.4 ± 18.9 | 131.1 ± 21.7 b,c | <0.001 |
| Extension | 17.2 ± 3.8 | 16.5 ± 3.5 | 15.1 ± 7.2 | 0.215 | 19.4 ± 5.4 | 17.2 ± 4.6 | 16.8 ± 6.9 | 0.254 |
| Adduction | 25.6 ± 3.9 | 24.4 ± 3.5 | 22.1 ± 6.4 | 0.353 | 27.6 ± 6.4 | 24.7 ± 6.1 | 23.4 ± 8.1 | 0.377 |
| Abduction | 42.1 ± 5.8 | 37.1 ± 10.1 a | 32.1 ± 14.8 b,c | <0.001 | 46.9 ± 9.4 | 43.1 ± 10.7 | 35.5 ± 12.1 b,c | <0.001 |
| IR | 40.2 ± 5.9 | 37.5 ± 7.4 | 32.4 ± 5.9 b,c | <0.001 | 45.1 ± 7.5 | 41.9 ± 8.8 | 35.4 ± 8.9 b,c | <0.001 |
| ER | 45.9 ± 5.6 | 39.1 ± 5.9 | 24.9 ± 6.4 b,c | <0.001 | 49.9 ± 8.4 | 44.2 ± 10.1 | 30.4 ± 9.1 b,c | <0.001 |
| Variables | Healthy | HDast | HDst | Healthy to HDast | Healthy to HDst | ||
|---|---|---|---|---|---|---|---|
| % df | p-Value | % df | p-Value | ||||
| Men | |||||||
| Anterior, cm | 62.3 ± 8.9 | 59.9 ± 13.8 | 46.0 ± 15.4 b,c | 3.9 | 0.347 | 26.2 | <0.001 |
| Posteromedial, cm | 90.5 ± 12.0 | 82.8 ± 14.8 | 68.1 ± 19.6 b,c | 8.5 | 0.296 | 24.8 | <0.001 |
| Posterolateral, cm | 93.8 ± 11.9 | 75.7 ± 17.3 a | 60.7 ± 17.7 b,c | 19.3 | <0.001 | 35.3 | <0.001 |
| Total score | 96.7 ± 11.8 | 85.2 ± 14.2 | 68.5 ± 18.3 b,c | 11.4 | 0.040 | 29.1 | <0.001 |
| Women | |||||||
| Anterior, cm | 55.5 ± 9.5 | 53.4 ± 14.0 | 40.5 ± 16.1 b,c | 3.8 | 0.402 | 27.0 | <0.001 |
| Posteromedial, cm | 79.4 ± 12.0 | 73.0 ± 16.3 | 52.1 ± 18.6 b,c | 8.1 | 0.314 | 34.4 | <0.001 |
| Posterolateral, cm | 82.8 ± 11.8 | 70.7 ± 15.1 a | 48.9 ± 18.8 b,c | 14.6 | <0.001 | 40.9 | <0.001 |
| Total score | 85.9 ± 12.3 | 77.9 ± 15.5 | 55.5 ± 18.1 b,c | 9.5 | 0.276 | 35.5 | <0.001 |
| Variables | Healthy | HDast | HDst | Healthy to HDast | Healthy to HDst | ||
|---|---|---|---|---|---|---|---|
| % df | p-Value | % df | p-Value | ||||
| Men | |||||||
| Flx, Nm/kg | 2.05 ± 0.23 | 1.83 ± 0.27 a | 1.32 ± 0.29 b,c | 10.7 | 0.004 | 35.6 | 0.015 |
| Ext, Nm/kg | 2.90 ± 0.26 | 2.79 ± 0.24 | 2.74 ± 0.27 | 3.8 | 0.289 | 5.5 | 0.541 |
| Add, Nm/kg | 1.76 ± 0.54 | 1.70 ± 0.69 | 1.60 ± 0.44 | 3.4 | 0.170 | 9.1 | 0.204 |
| Abd, Nm/kg | 1.66 ± 0.35 | 1.38 ± 0.44 a | 0.99 ± 0.48 b,c | 16.9 | 0.011 | 40.4 | <0.001 |
| Flx/Ext ratio | 0.71 ± 0.10 | 0.66 ± 0.09 | 0.48 ± 0.07 | 7.2 | 0.184 | 31.8 | 0.460 |
| Add/Abd ratio | 1.06 ± 0.12 | 1.23 ± 0.11 a | 1.62 ± 0.24 b,c | 13.9 | 0.019 | 34.3 | <0.001 |
| Women | |||||||
| Flx, Nm/kg | 1.67 ± 0.23 | 1.47 ± 0.38 a | 1.25 ± 0.32 b,c | 12.0 | 0.024 | 25.1 | <0.001 |
| Ext, Nm/kg | 2.56 ± 0.27 | 2.49 ± 0.39 | 2.42 ± 0.35 | 2.7 | 0.534 | 5.5 | 0.549 |
| Add, Nm/kg | 1.53 ± 0.25 | 1.43 ± 0.26 | 1.01 ± 0.33 b,c | 6.5 | 0.199 | 34.0 | <0.001 |
| Abd, Nm/kg | 1.52 ± 0.19 | 1.26 ± 0.23 a | 0.94 ± 0.28 b,c | 17.1 | <0.001 | 38.2 | <0.001 |
| Flx/Ext ratio | 0.65 ± 0.11 | 0.59 ± 0.10 | 0.39 ± 0.08 b,c | 9.5 | 0.357 | 20.8 | 0.015 |
| Add/Abd ratio | 1.01 ± 0.14 | 1.13 ± 0.35 | 1.07 ± 0.13 | 11.3 | 0.544 | 6.3 | 0.310 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Yu, H.; Kim, Y.; Chen, T. Asymmetry in Muscle Strength, Dynamic Balance, and Range of Motion in Adult Symptomatic Hip Dysplasia. Symmetry 2022, 14, 748. https://doi.org/10.3390/sym14040748
Wang H, Yu H, Kim Y, Chen T. Asymmetry in Muscle Strength, Dynamic Balance, and Range of Motion in Adult Symptomatic Hip Dysplasia. Symmetry. 2022; 14(4):748. https://doi.org/10.3390/sym14040748
Chicago/Turabian StyleWang, Haifang, Hailong Yu, Yonghwan Kim, and Tingting Chen. 2022. "Asymmetry in Muscle Strength, Dynamic Balance, and Range of Motion in Adult Symptomatic Hip Dysplasia" Symmetry 14, no. 4: 748. https://doi.org/10.3390/sym14040748
APA StyleWang, H., Yu, H., Kim, Y., & Chen, T. (2022). Asymmetry in Muscle Strength, Dynamic Balance, and Range of Motion in Adult Symptomatic Hip Dysplasia. Symmetry, 14(4), 748. https://doi.org/10.3390/sym14040748







