Individuals with Unilateral Mild-to-Moderate Hip Osteoarthritis Exhibit Lower Limb Kinematic Asymmetry during Walking But Not Sit-to-Stand
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Protocol
2.3. Data Collection and Analysis Procedures
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Spatiotemporal Asymmetry during Walking
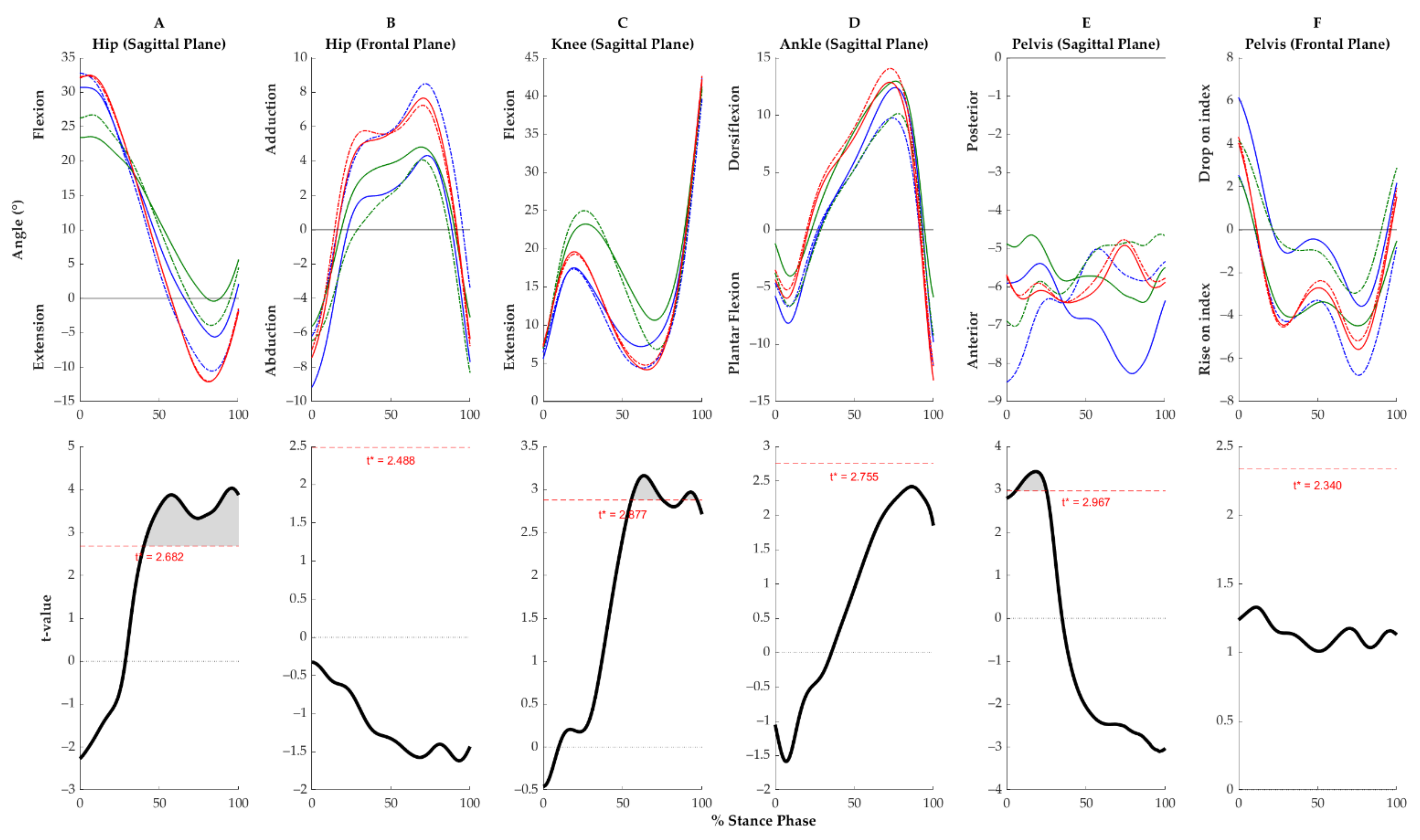
3.3. Within-Group Kinematic Symmetry during Walking
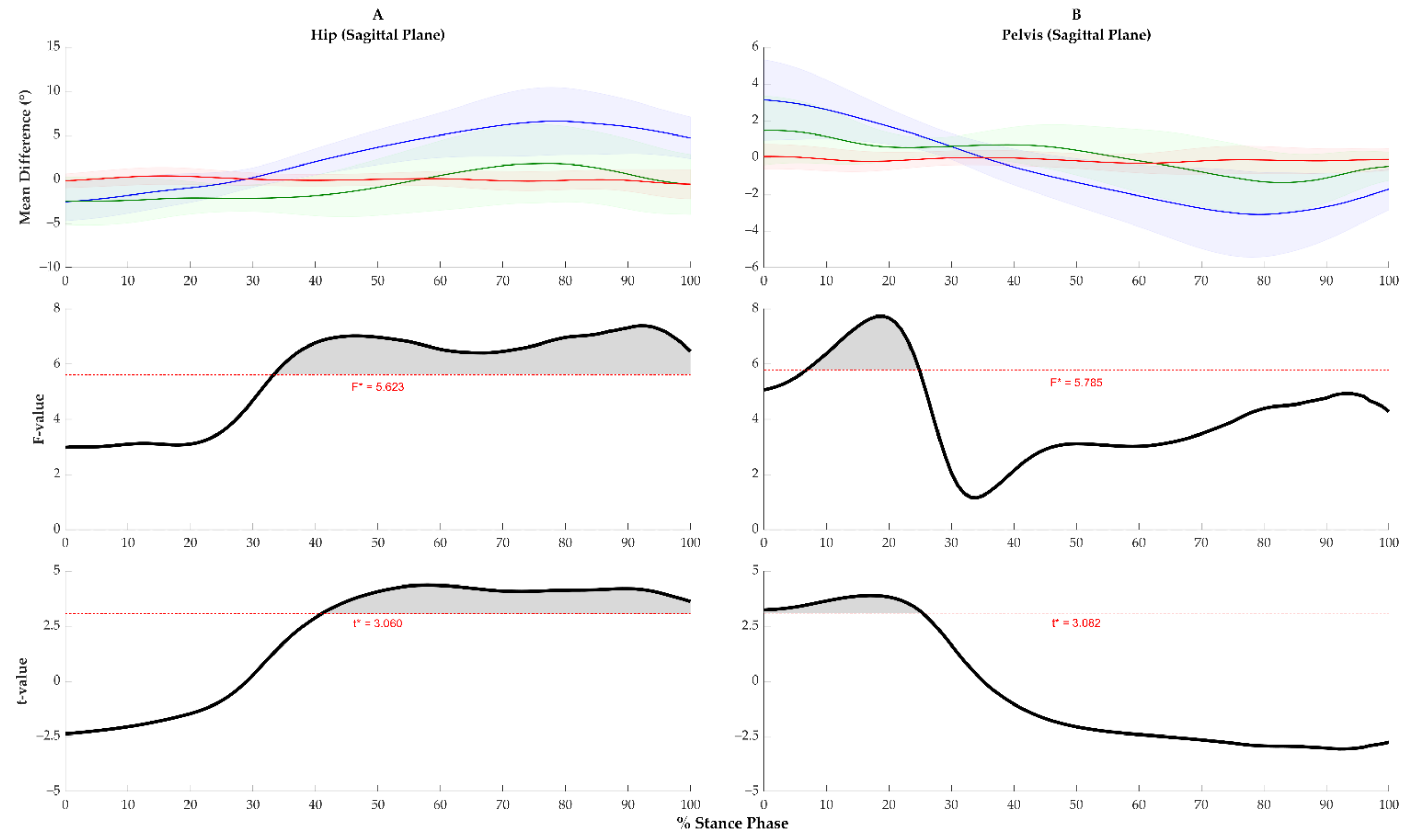
3.4. Between-Group Kinematic Asymmetry during Walking
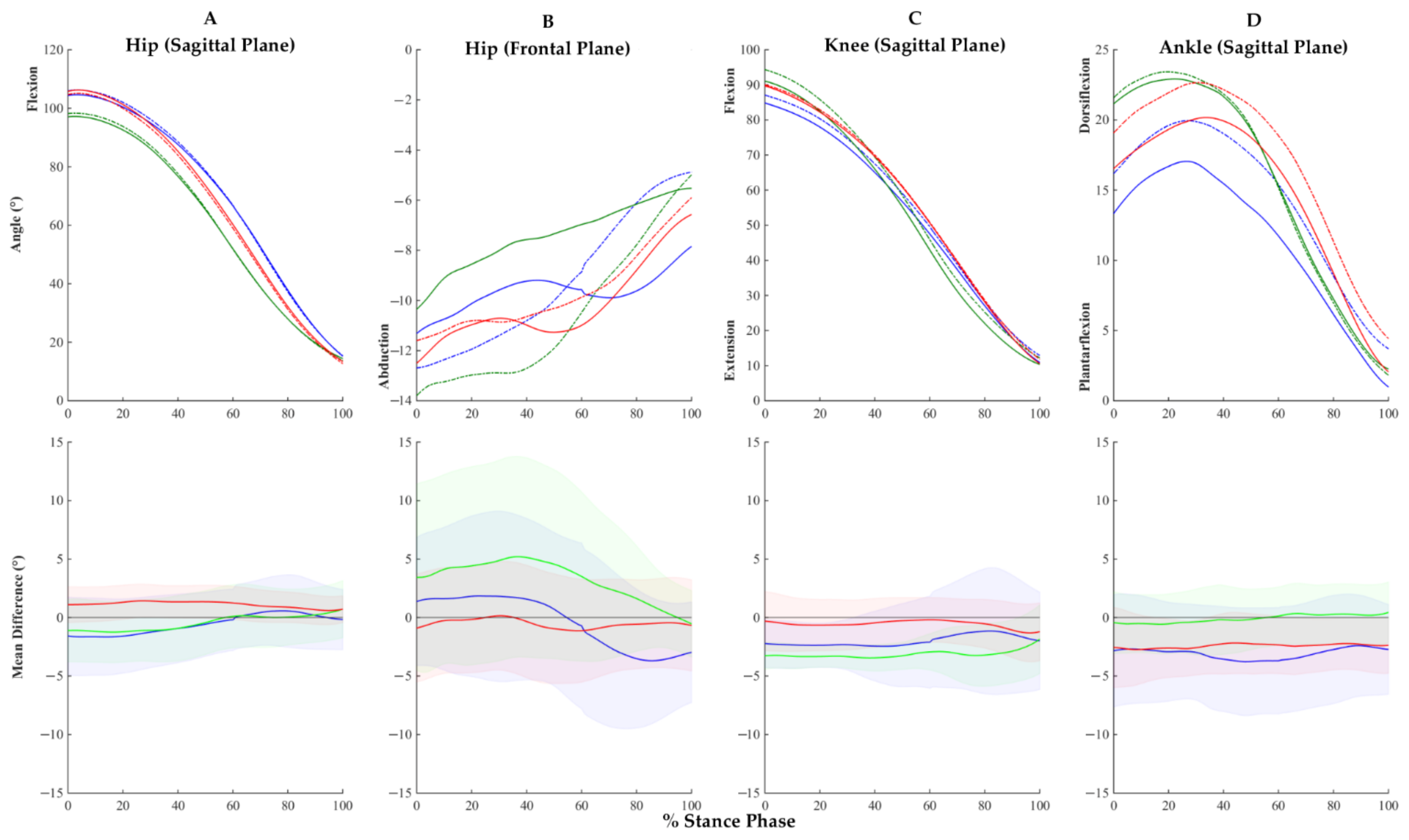
3.5. Kinematic Asymmetry during Sit-to-Stand
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Access Economics Arthritis Australia. Painful Realities: The Economic Impact of Arthritis in Australia in 2007. Available online: http://www.arthritisaustralia.com.au/ (accessed on 13 April 2020).
- Sun, H.B. Mechanical loading, cartilage degradation, and arthritis. Ann. N. Y. Acad. Sci. 2010, 1211, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Hoaglund, F.T.; Steinbach, L.S. Primary osteoarthritis of the hip: Etiology and epidemiology. J. Am. Acad. Orthop. Surg. 2001, 9, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, H.; Allard, P.; Prince, F.; Labelle, H. Symmetry and limb dominance in able-bodied gait: A review. Gait Posture 2000, 12, 34–45. [Google Scholar] [CrossRef]
- Shakoor, N.; Block, J.A.; Shott, S.; Case, J.P. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum. 2002, 46, 3185–3189. [Google Scholar] [CrossRef] [PubMed]
- Foucher, K.C.; Wimmer, M.A. Contralateral hip and knee gait biomechanics are unchanged by total hip replacement for unilateral hip osteoarthritis. Gait Posture 2012, 35, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Creaby, M.W.; Bennell, K.L.; Hunt, M.A. Gait differs between unilateral and bilateral knee osteoarthritis. Arch. Phys. Med. Rehabil. 2012, 93, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, A.N.; Pena, G.M.; Guilherme, E.M.; Rocha, N. Asymmetry in children with unilateral cerebral palsy during sit-to-stand movement: Cross-sectional, repeated-measures and comparative study. Clin. Biomech. 2020, 71, 152–159. [Google Scholar] [CrossRef] [PubMed]
- King, E.; Richter, C.; Franklyn-Miller, A.; Daniels, K.; Wadey, R.; Jackson, M.; Moran, R.; Strike, S. Biomechanical but not timed performance asymmetries persist between limbs 9months after acl reconstruction during planned and unplanned change of direction. J. Biomech. 2018, 81, 93–103. [Google Scholar] [CrossRef]
- Little, V.L.; Perry, L.A.; Mercado, M.W.V.; Kautz, S.A.; Patten, C. Gait asymmetry pattern following stroke determines acute response to locomotor task. Gait Posture 2020, 77, 300–307. [Google Scholar] [CrossRef]
- Shakoor, N.; Hurwitz, D.E.; Block, J.A.; Shott, S.; Case, J.P. Asymmetric knee loading in advanced unilateral hip osteoarthritis. Arthritis Rheum. 2003, 48, 1556–1561. [Google Scholar] [CrossRef]
- Saxby, D.J.; Lloyd, D.G. Osteoarthritis year in review 2016: Mechanics. Osteoarthr. Cartil. 2017, 25, 190–198. [Google Scholar] [CrossRef]
- Zeni, J., Jr.; Pozzi, F.; Abujaber, S.; Miller, L. Relationship between physical impairments and movement patterns during gait in patients with end-stage hip osteoarthritis. J. Orthop. Res. 2015, 33, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Miki, H.; Sugano, N.; Hagio, K.; Nishii, T.; Kawakami, H.; Kakimoto, A.; Nakamura, N.; Yoshikawa, H. Recovery of walking speed and symmetrical movement of the pelvis and lower extremity joints after unilateral tha. J. Biomech. 2004, 37, 443–455. [Google Scholar] [CrossRef]
- Oken, O.F.; Yildirim, A.O.; Yavuzer, G.; Gulcek, M.; Unal, V.S.; Ucaner, A.; Oken, O. Gait symmetry in patients with unilateral partial hip arthroplasty. Eklem Hastalik. Cerrahisi 2010, 21, 86–90. [Google Scholar] [PubMed]
- Queen, R.M.; Watters, T.S.; Abbey, A.N.; Sabesan, V.J.; Vail, T.P.; Bolognesi, M.P. Gait symmetry: A comparison of hip resurfacing and jumbo head total hip arthroplasty patients. J. Arthroplast. 2011, 26, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Talis, V.L.; Grishin, A.A.; Solopova, I.A.; Oskanyan, T.L.; Belenky, V.E.; Ivanenko, Y.P. Asymmetric leg loading during sit-to-stand, walking and quiet standing in patients after unilateral total hip replacement surgery. Clin. Biomech. 2008, 23, 424–433. [Google Scholar] [CrossRef] [PubMed]
- Hodt-Billington, C.; Helbostad, J.L.; Vervaat, W.; Rognsvag, T.; Moe-Nilssen, R. Changes in gait symmetry, gait velocity and self-reported function following total hip replacement. J. Rehabil. Med. 2011, 43, 787–793. [Google Scholar] [CrossRef]
- Constantinou, M.; Barrett, R.; Brown, M.; Mills, P. Spatial-temporal gait characteristics in individuals with hip osteoarthritis: A systematic literature review and meta-analysis. J. Orthop. Sports Phys. Ther. 2014, 44, 291-B7. [Google Scholar] [CrossRef]
- Cichy, B.; Wilk, M.; Sliwinski, Z. Changes in gait parameters in total hip arthroplasty patients before and after surgery. Med. Sci. Monit. 2008, 14, Cr159–Cr169. [Google Scholar]
- Kyriazis, V.; Rigas, C. Temporal gait analysis of hip osteoarthritic patients operated with cementless hip replacement. Clin. Biomech. 2002, 17, 318–321. [Google Scholar] [CrossRef]
- Lugade, V.; Wu, A.; Jewett, B.; Collis, D.; Chou, L.S. Gait asymmetry following an anterior and anterolateral approach to total hip arthroplasty. Clin. Biomech. 2010, 25, 675–680. [Google Scholar] [CrossRef]
- Isobe, Y.; Okuno, M.; Otsuki, T.; Yamamoto, K. Clinical study on arthroplasties for osteoarthritic hip by quantitative gait analysis. Comparison between total hip arthroplasty and bipolar endoprosthetic arthroplasty. Biomed. Mater. Eng. 1998, 8, 167–175. [Google Scholar] [PubMed]
- Vogt, L.; Banzer, W.; Bayer, I.; Schmidtbleicher, D.; Kerschbaumer, F. Overground and walkway ambulation with unilateral hip osteoarthritis: Comparison of step length asymmetries and reproducibility of treadmill mounted force plate readings. Physiother. Theory Pract. 2006, 22, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Shakoor, N.; Foucher, K.C.; Wimmer, M.A.; Mikolains, R.A.; Khandelwal, S.; Block, J.A. Gait alterations and their association with radiographic severity and pain in unilateral hip osteoarthritis. Osteoarthr. Cartil. 2010, 18, S67–S68. [Google Scholar] [CrossRef][Green Version]
- Eitzen, I.; Fernandes, L.; Nordsletten, L.; Snyder-Mackler, L.; Risberg, M.A. Weight-bearing asymmetries during sit-to-stand in patients with mild-to-moderate hip osteoarthritis. Gait Posture 2014, 39, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Lamontagne, M.; Beaulieu, M.L.; Varin, D.; Beaule, P.E. Lower-limb joint mechanics after total hip arthroplasty during sitting and standing tasks. J. Orthop. Res. 2012, 30, 1611–1617. [Google Scholar] [CrossRef] [PubMed]
- Abujaber, S.B.; Marmon, A.R.; Pozzi, F.; Rubano, J.J.; Zeni, J.A. Sit-to-stand biomechanics before and after total hip arthroplasty. J. Arthroplast. 2015, 30, 2027–2033. [Google Scholar] [CrossRef] [PubMed]
- Loureiro, A.; Constantinou, M.; Beck, B.; Barrett, R.S.; Diamond, L.E. A 12-month prospective exploratory study of muscle and fat characteristics in individuals with mild-to-moderate hip osteoarthritis. BMC Musculoskelet. Disord. 2019, 20, 283. [Google Scholar] [CrossRef]
- Loureiro, A.; Constantinou, M.; Diamond, L.E.; Beck, B.; Barrett, R. Individuals with mild-to-moderate hip osteoarthritis have lower limb muscle strength and volume deficits. BMC Musculoskelet. Disord. 2018, 19, 303. [Google Scholar] [CrossRef]
- Constantinou, M.; Loureiro, A.; Carty, C.; Mills, P.; Barrett, R. Hip joint mechanics during walking in individuals with mild-to-moderate hip osteoarthritis. Gait Posture 2017, 53, 162–167. [Google Scholar] [CrossRef]
- Higgs, J.P.; Saxby, D.J.; Constantinou, M.; Loureiro, A.; Hoang, H.; Diamond, L.E.; Barrett, R.S. Individuals with mild-to-moderate hip osteoarthritis exhibit altered pelvis and hip kinematics during sit-to-stand. Gait Posture 2019, 71, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Boniatis, I.; Costaridou, L.; Cavouras, D.; Kalatzis, I.; Panagiotopoulos, E.; Panayiotakis, G. A morphological index for assessing hip osteoarthritis severity from radiographic images. Brit. J. Radiol. 2008, 81, 129–136. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Mahomed, N.N.; Arndt, D.C.; McGrory, B.J.; Harris, W.H. The Harris hip score: Comparison of patient self-report with surgeon assessment. J. Arthroplast. 2001, 16, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef] [PubMed]
- Besier, T.F.; Sturnieks, D.L.; Alderson, J.A.; Lloyd, D.G. Repeatability of gait data using a functional hip joint centre and a mean helical knee axis. J. Biomech. 2003, 36, 1159–1168. [Google Scholar] [CrossRef]
- Mantoan, A.; Pizzolato, C.; Sartori, M.; Sawacha, Z.; Cobelli, C.; Reggiani, M. MOtoNMS: A MATLAB toolbox to process motion data for neuromusculoskeletal modeling and simulation. Source Code Biol. Med. 2015, 10, 12. [Google Scholar] [CrossRef] [PubMed]
- Delp, S.L.; Anderson, F.C.; Arnold, A.S.; Loan, P.; Habib, A.; John, C.T.; Guendelman, E.; Thelen, D.G. OpenSim: Open-source software to create and analyze dynamic simulations of movement. IEEE Trans. Biomed. Eng. 2007, 54, 1940–1950. [Google Scholar] [CrossRef] [PubMed]
- Pataky, T.C. Generalized n-dimensional biomechanical field analysis using statistical parametric mapping. J. Biomech. 2010, 43, 1976–1982. [Google Scholar] [CrossRef]
- Steultjens, M.P.; Dekker, J.; van Baar, M.E.; Oostendorp, R.A.; Bijlsma, J.W. Range of joint motion and disability in patients with osteoarthritis of the knee or hip. Rheumatology 2000, 39, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Loizeau, J.; Allard, P.; Duhaime, M.; Landjerit, B. Bilateral gait patterns in subjects fitted with a total hip prosthesis. Arch. Phys. Med. Rehabil. 1995, 76, 552–557. [Google Scholar] [CrossRef]
- Loureiro, A.; Mills, P.M.; Barrett, R.S. Muscle weakness in hip osteoarthritis: A systematic review. Arthritis. Care Res. 2013, 65, 340–352. [Google Scholar] [CrossRef]
- Heuts, P.H.; Vlaeyen, J.W.; Roelofs, J.; de Bie, R.A.; Aretz, K.; van Weel, C.; van Schayck, O.C. Pain-related fear and daily functioning in patients with osteoarthritis. Pain 2004, 110, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Sims, K.J.; Richardson, C.A.; Brauer, S.G. Investigation of hip abductor activation in subjects with clinical unilateral hip osteoarthritis. Ann. Rheum. Dis. 2002, 61, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, N.E.; Bruce-Brand, R.; Bennett, D.; O’Brien, S.; Beverland, D.E. No difference in gait kinematics or kinetics between limbs in bilateral total hip replacement patients at long-term follow-up. Clin. Biomech. 2019, 67, 166–170. [Google Scholar] [CrossRef]
- Viteckova, S.; Kutilek, P.; Svoboda, Z.; Krupicka, R.; Kauler, J.; Szabo, Z. Gait symmetry measures: A review of current and prospective methods. Biomed. Signal Process. Control. 2018, 42, 89–100. [Google Scholar] [CrossRef]
- Yoshioka, S.; Nagano, A.; Himeno, R.; Fukashiro, S. Computation of the kinematics and the minimum peak joint moments of sit-to-stand movements. Biomed. Eng. Online 2007, 6, 26. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Adams, J.; Leddy, H.A.; McNulty, A.L.; O’Conor, C.J.; Guilak, F. The mechanobiology of articular cartilage: Bearing the burden of osteoarthritis. Curr. Rheumatol. Rep. 2014, 16. [Google Scholar] [CrossRef] [PubMed]
- Arden, N.; Nevitt, M.C. Osteoarthritis: Epidemiology. Best Pract. Res. Clin. Rheumatol. 2006, 20, 3–25. [Google Scholar] [CrossRef]
| Hip OA | Control | |||||
|---|---|---|---|---|---|---|
| Unilateral | Bilateral | |||||
| n = 42 | 12 (4 M, 8 F) | 9 (4 M, 5 F) | 21 (5 M, 16 F) | |||
| Age (years) | 62.5 (SD 10.0) | 63.2 (SD 6.0) | 58.7 (SD 8.2) | |||
| Age (range) | 58–78 | 56–71 | 49–75 | |||
| Height (m) | 1.67 (SD 0.05) | 1.69 (SD 0.12) | 1.67 (SD 0.07) | |||
| Mass (kg) | 78.5 (SD 13.4) * | 81.6 (SD 16.9) * | 69.5 (SD 9.2) | |||
| BMI (kg/m2) | 27.2 (SD 3.2) * | 27.6 (SD 4.6) * | 25.3 (SD 3.4) | |||
| HHS | 73.04 (SD 12.06) | 65.12 (11.9) | 99.88 (SD 1.04) | |||
| Index | Non-index | Index | Non-index | Index | Non-index | |
| JSW (mm) | 2.5 (SD 0.9) * | 3.5 (SD 0.7) | 2.7 (SD 0.7) * | 3.1 (SD 0.7) * | 4.1 (SD 0.6) | 3.9 (SD 0.5) |
| JSW difference | 1 (SD 0.8) *, + | −0.37 (SD 0.3) | −0.21 (SD 0.4) | |||
| KL 0 | 5 | 14 | 12 | |||
| KL 1 | 7 | 7 | 9 | |||
| KL 2 | 5 | 5 | 6 | |||
| KL 3 | 7 | 4 | 3 | |||
| KL difference | 1.8 (SD 1.1) *, + | 0.1 (SD 0.3) | −0.1 (SD 0.6) | |||
| Hip OA | Control | ||
|---|---|---|---|
| Unilateral | Bilateral | ||
| Gait Velocity (m/s) | |||
| Index | 1.19 (SD 0.21) | 1.11 (SD 0.11) | 1.31 (SD 0.11) |
| Non-index | 1.20 (SD 0.21) | 1.11 (SD 0.11) | 1.30 (SD 0.11) |
| Difference | −0.01 (SD 0.03) | 0.001 (SD 0.03) | 0.008 (SD 0.03) |
| Step Length (m) | |||
| Index | 0.70 (SD 0.11) | 0.70 (SD 0.09) | 0.77 (SD 0.10) |
| Non-index | 0.70 (SD 0.11) | 0.69 (SD 0.05) | 0.74 (SD 0.05) |
| Difference | 0.00 (SD 0.12) | 0.01 (SD 0.13) | 0.03 (SD 0.13) |
| Stance Duration (ms) | |||
| Index | 662 (SD 60) | 700 (SD 59) | 613 (SD 39) |
| Non-index | 660 (SD 62) | 714 (SD 58) | 612 (SD 40) |
| Difference | 0.6 (SD 9) + | −14 (SD 8) * | 0.9 (SD 9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Higgs, J.P.; Diamond, L.E.; Saxby, D.J.; Constantinou, M.; Barrett, R.S. Individuals with Unilateral Mild-to-Moderate Hip Osteoarthritis Exhibit Lower Limb Kinematic Asymmetry during Walking But Not Sit-to-Stand. Symmetry 2021, 13, 768. https://doi.org/10.3390/sym13050768
Higgs JP, Diamond LE, Saxby DJ, Constantinou M, Barrett RS. Individuals with Unilateral Mild-to-Moderate Hip Osteoarthritis Exhibit Lower Limb Kinematic Asymmetry during Walking But Not Sit-to-Stand. Symmetry. 2021; 13(5):768. https://doi.org/10.3390/sym13050768
Chicago/Turabian StyleHiggs, Jeremy P., Laura E. Diamond, David J. Saxby, Maria Constantinou, and Rod S. Barrett. 2021. "Individuals with Unilateral Mild-to-Moderate Hip Osteoarthritis Exhibit Lower Limb Kinematic Asymmetry during Walking But Not Sit-to-Stand" Symmetry 13, no. 5: 768. https://doi.org/10.3390/sym13050768
APA StyleHiggs, J. P., Diamond, L. E., Saxby, D. J., Constantinou, M., & Barrett, R. S. (2021). Individuals with Unilateral Mild-to-Moderate Hip Osteoarthritis Exhibit Lower Limb Kinematic Asymmetry during Walking But Not Sit-to-Stand. Symmetry, 13(5), 768. https://doi.org/10.3390/sym13050768






