Abstract
Tropism, or asymmetry, of facet joints in the cervical spine has been found to be related to degenerative changes of the joints and discs. Clinicians often assume that differences in segmental mobility are related to tropism. The aims of this study were to determine the relationship between asymmetry of facet joints in the sub-axial cervical spine and (1) segmental mobility and (2) spinal levels perceived by therapists to have limited mobility. Eighteen participants with idiopathic neck pain had MRIs of their cervical spine in neutral and at the end of active rotation. Angular movement and translational movement of each motion segment was calculated from 3D segmentations of the vertebrae. A plane was fitted to the facet on each side. Tropism was considered to be the difference in the orientation of the facet planes and ranged from 1 to 30° with a median of 7.7°. No relationships were found between the extent of tropism and either segmental movement or locations deemed to be symptomatic. Tropism in the sub-axial cervical spine does not appear to be related to segmental mobility in rotation or to levels deemed to be symptomatic.
1. Introduction
Movement between individual spinal vertebrae involves three structures—the intervertebral disc anteriorly and a pair of facet (or zygapophyseal) joints posteriorly. The facet joints often exhibit asymmetry, which is referred to as tropism. Tropism is defined as “the turning of all or part of an organism in a particular direction in response to an external stimulus” [1] and is most frequently used to describe the growth of plants. The term was first used to describe asymmetry of the lumbar facets seen on anterior to posterior X-ray images in 1927 [2]. Even with three dimensional (3D) images, tropism was still usually considered to describe asymmetry of the facets in the sagittal plane as seen in axial images [3,4]. Currently, tropism is also used to indicate 3D asymmetry of the facets in any plane [5], which is how the term will be used in this manuscript.
There are conflicting views on the relevance of spinal tropism—in particular, whether tropism in the spine is related to degenerative changes of the facets or discs. A recent systematic review with meta-analysis [6] found that there is a relationship between tropism and degenerative changes for both the lumbar and cervical spines, and a further study in the cervical spine reinforced these findings [7]. Such changes are paradoxically thought to result from tropism either limiting movement [8] or increasing instability [9], but in either case, the result is thought to be increased stresses on the facets and discs [10]. Suggestions that tropism may be the result, rather than the cause, of degenerative changes have been proposed but, as with many aspects of tropism, the results are contradictory, with some authors expecting the incidence of tropism would increase with age [11] while others finding this not to be the case [12].
Although there are a number of in vitro studies and hypotheses on the potential effects of tropism on mobility, stability, and stresses, few in vivo investigations have considered the actual relationships between tropism and segmental movement, and most only considered movement in the sagittal plane (flexion and extension). In the lumbar spine, findings are mixed, with some studies finding no relationship between tropism and the magnitude of movement [13], while others found that increased tropism correlated with reduced segmental movement [14]. In the cervical spine, tropism in the axial and coronal planes was associated with decreased movement in flexion/extension, but not with any alterations in lateral bending [5]. In summary, although it appears that tropism in both the lumbar and cervical spines is related to increased degenerative changes and decreased mobility in the sagittal plane, it is unclear what effects tropism has on movements in other planes, particularly on rotational movements.
Data collected for a study on the effect of manual therapy on segmental movement in the cervical spine provided the opportunity for a secondary analysis that considered movement in cervical rotation in relation to facet tropism. The primary aim of the current study was to determine if there is a relationship between tropism and rotational movement in the sub-axial cervical spine. The fact that the original data also included an indication of which spinal level was symptomatic meant that a second aim could be considered—was tropism greater in symptomatic locations in the cervical spine than non-symptomatic locations?
2. Materials and Methods
The data in this paper are a re-analysis of data collected for another study about the effect of manual therapy treatment to the cervical spine (currently under review). Eighteen participants who had experienced neck pain for more than three months and had limitation of rotation by ≥15° were recruited from a university community. Participants rated their average and maximum pain on an 11-point Likert scale (0–10) over the preceding week as 2.3 (SD 1.9) and 3.2/10 (SD 2.7), respectively. Each participant had two magnetic resonance imaging (MRI) scans in supine: the first in a neutral position and the second with their head rotated until the onset of pain in the limited direction. The location that was deemed to be symptomatic and hypomobile was marked by a small vitamin E capsule to enable identification of the level on the scans.
Imaging and processing were performed according to our previous study, which includes the reliability of the motion measurements [15]. Mimics V17.9 and 3Matic V9 (Materialise NV) were used to process the images. Each vertebra from C2 to C7 was segmented with a semi-automatic procedure. The outline of each inferior facet (COF) was determined by manually drawing an outline of each facet and using an automated software function to calculate the centre of each facet (COF). Tropism was determined as shown in Figure 1. Repeatability of the orientation of facets was determined using images from a previous study, where two individuals independently segmented and drew facets from MRI scans for two individuals [15]. Fitting a plane to these facets was an automated process so could be applied to the previously processed images. The mean error between the angles of the facets was 3.2°.
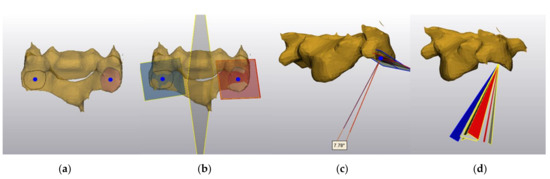
Figure 1.
Determination and representation of tropism. (a) A C4 vertebra with the facets outlined and the centre of the facets indicated by blue dots. (b) A plane fitted to each facet and a mirror plane that was placed perpendicular to, and through the midpoint of, a line through the centre of the facets. (c) The extent and orientation of tropism for one participant. A line drawn perpendicular to the plane of each facet passing through the centre of the left facet indicates the orientation of each facet. The angle between the line perpendicular to the left facet and the line perpendicular to the mirror image of the right facet was taken to be the tropism. (d) The angle and orientation of tropism for ten participants. Supplementary files that show angle and orientation of tropism for ten participants for each vertebra are included as Supplementary 3DPDF files (Figure S1).
An automated voxel-based registration using 3Matic was used to align contours and determine (1) the Euler angular movement calculated using the order Flex/Ext (X), Lateral Flexion (Y), Rotation (Z), and (2) the facet movements calculated as a single value for the translation of the COF of each side (contra and ipsilateral) movement.
The rotation in each axis of each whole vertebrae and the translations of the facets were normalised for each participant to enable consideration of the proportionate contribution of each motion segment. The total of the normalised contributions across all intervertebral levels for each participant was therefore equal to 1.00. Asymmetry of facet movement was calculated as the absolute value of the difference between the normalised translation on the two sides. Ethics approval was obtained from the university’s Human Research Ethics Committee (PES/34/11/HREC).
Statistical Analysis
ANOVAs were used to determine if there were any differences across levels for normalised angular movement, normalised facet translations, or tropism. The angular movements and facet translations were not normally distributed, as assessed by Shapiro–Wilk test and the assumption of sphericity was not met as indicated by Mauchly’s test. When neither assumption is met, it has been proposed that the means and confidence intervals are best calculated using a bootstrapping approach [16]. Bootstrapping the original data with 1000 resamples with replacements to determine the means and confidence intervals (CI) was therefore used in the subsequent analysis. Spearman’s correlation coefficients were calculated for relationships between tropism and (1) normalised angular movement in each axis, (2) normalised facet translation, and (3) asymmetry of facet translations. Normalisation was performed using Microsoft Excel (Microsoft 365 MSO (16.0.13127.21210). Other statistical analysis was performed in SPSS V26 (IBM Corp).
3. Results
No significant differences were found for tropism, normalised angular movements or facet translations by level which meant that further analysis could consider relationships between facets and movement across all levels. Tropism ranged from 1 to 30° with a median of 7.7°. Figure 2 and Figure 3 show plots of tropism vs. angular movement in each of the three axes of movement, facet translation, and asymmetry of facet movement. Correlation coefficients did not indicate significant relationships for any of these variables.
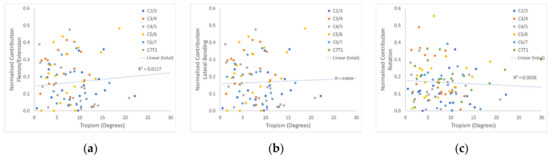
Figure 2.
Relationships between angular movement and tropism. Panels (a–c) show the relationships of tropism with normalised angular movement for each intervertebral level in flexion/extension, lateral bending, and rotation, respectively. The trendline and R2 value are for all levels combined.
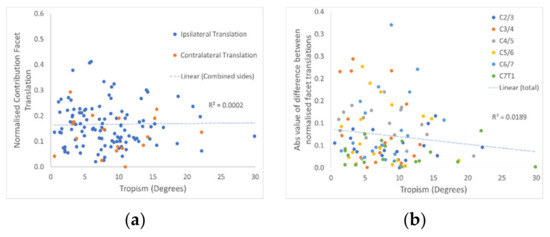
Figure 3.
Relationships between facet movement and tropism. (a) The relationship of tropism with normalised facet translation for the ipsilateral and contralateral facets. (b) The relationship with the asymmetry of normalised facet translation (ipsilateral minus contralateral sides). The trend line and R2 value are for both sides and all levels combined.
No difference was found between the angle of tropism for the symptomatic (mean: 8.3°, CI: 7.1 to 9.4°) and asymptomatic (mean: 7.9°, CI: 6.0 to 9.6°) locations.
The 3DPDFs in supplementary files (https://www.mdpi.com/article/10.3390/sym13050739/s1) allow the reader not only to see the magnitude of the tropism but also provide a visual representation of the orientation of the tropism.
4. Discussion
This study did not find that asymmetry of the orientation of facet joints (tropism) in the cervical spine was related to angular contributions or facet translations of that vertebra during active movement, the asymmetry of facet movement, or whether the location was symptomatic. The mean tropism was 7.7°, with 55 out of 108 vertebrae having tropism greater than the cutoff of 7° that had been proposed as defining tropism [4].
In relation to angular movement, these findings differ from some previous studies where tropism was found to be related to mobility, at least in flexion/extension in the lumbar [14] and cervical spines [5]. Methodological differences could account for the findings being different from other studies. First, we investigated rotation rather than flexion/extension, and a limitation in one axis of movement does not necessarily relate to limitation in another. A second important difference is in how tropism was measured. Previous studies determined the asymmetry in each cardinal plane and then analysed the relationships between movement and tropism in individual planes. Even in those studies that measured the asymmetry from 3D images, most measured tropism from single two-dimensional slices [8,13]. A difficulty with this method is that the angles of the facets can be different depending on which slice is measured [5,8]. To overcome this difficulty, Liu et al. [5] fit a single plane to each facet but still calculated asymmetry in each cardinal axis separately. It might seem that asymmetry in a given plane would likely be related to alteration of movement around an axis perpendicular to that plane, but this does not seem to be the case [5,6].
Since in previous studies, the plane that tropism was found did not seem to correspond with the orientation of movement limitation, the current study considered the relationship between the planes of the facets. Rotation within the plane of the facet was not considered to be an important indicator of asymmetry, so comparing the angles between the planes of the facets enabled a single measure of asymmetry to be calculated rather than separate indicators for each axis. Translation of the facets was not considered in other studies, but is another way of measuring intervertebral movement which introduces the possibility of indicating asymmetry of facet movement.
Tropism of the facets is common with the greater than 50% incidence found in the current study being consistent with findings from other studies [6]. The clinical implications of tropism are, however, less clear. Consistent relationships have been found between tropism and degenerative changes of both the facet joints and discs [6]. Tropism is thought to produce increased strain on and altered movement patterns of vertebrae and thus result in degenerative changes [6,14]. The presence of increased strain in the presence of in vivo tropism has not been investigated, so there is a possibility that degeneration could have caused the asymmetry. If degenerative changes caused the tropism, then both degenerative changes and tropism would be expected to increase with increasing age [11], but this is not the case [12]. Interestingly, although the angle of facets does not appear to alter in the presence of degenerative changes, the size of the facets does appear to increase [17].
The pattern of relationships between the orientation of tropism and the alterations in particular axes of movement found in previous studies is unclear. The difficulties in evaluating in vivo movement may, to some extent, account for this lack of clarity. Most studies have considered the relatively easy to measure movement in the sagittal plane and have done so at the limits of flexion/extension with plane X-rays or planar views of scans. Movement outside of the sagittal plane are much more complex due to coupled movements, and they are more difficult to measure due to the need to reconstruct 3D images of each vertebra. Two further difficulties are, first, that the relative contributions of individual motion segments vary through the range of movement [18] and, secondly, that spinal movement is complex with limitation of movement in one motion segment—as, for example, occurs with cervical fusion—resulting in compensatory movements at multiple levels and in multiple axes of movement [19]. The lack of relationship between tropism and alterations of movement found in the current study may therefore be, at least partially, the result of methodological difficulties rather than a true lack of relationship.
As stated above, tropism has previously been found to be separately related to degenerative changes and some limitations of segmental mobility, and relationships between degenerative changes and limited mobility have been found in other studies [20,21]. Similarly, limited spinal mobility has been found in symptomatic locations [22]. Links between tropism and symptomatic locations have not, however, been previously investigated.
Clinicians frequently discuss that tropism is thought to cause some of the altered segmental mobility found during physical assessment of patients with spinal pain and are related to their symptoms, but there appears to be little written on this idea in the literature. One clear finding of the current study was that tropism did not appear to be related to symptomatic locations.
A limitation of this study is that the images were only taken in one direction of rotation and, since the participants were symptomatic, they had a less than normal range of rotation. Considering the large variation in the orientation of the tropism found in the current study, any relationships could have been washed out in the analysis. It could be argued that asymmetry of facet orientation would be likely to result in an asymmetry of movement, which could manifest as more translation on one side than the other, but this was not found. Asymmetry of movement could also be caused by alterations in muscle function, which was not possible to evaluate with the current study design.
5. Conclusions
Although not conclusive, the findings of the current study suggest a lack of relationships between tropism of the facets and either angular movement or translation of the facets during active rotation of the cervical spine. There is a strong suggestion that there is no relationship between tropism and symptomatic locations. The mechanism whereby spinal tropism may be related to a greater incidence of degenerative changes remains unclear, but may be more related to movements in the sagittal rather than the axial plane.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/sym13050739/s1, Figures S1–S6: Tropism of ten representative participants for C2 to C7.
Author Contributions
Conceptualisation, N.T., K.E., C.S.d.S.R.; methodology, N.T., C.S.d.S.R.; formal analysis, N.T., C.S.d.S.R.; investigation, N.T., K.E., C.S.d.S.R.; writing N.T., K.E., C.S.d.S.R. All authors have read and agreed to the published version of the manuscript.
Funding
The original study was supported by funding from the International Maitland Teachers Association.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Griffith University (PES/03/12/HREC) Approval date March 2012.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available in Supplementary file S7.
Acknowledgments
The authors would like to thank a number of students who assisted with image processing in the original study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Stevenson, A. Oxford Dictionary of English; Oxford University Press: Oxford, MS, USA, 2010. [Google Scholar]
- Putti, V. New conceptions in the pathogenesis of sciatic pain. Lancet 1927, 2, 53–60. [Google Scholar] [CrossRef]
- Kim, H.J.; Chun, H.J.; Lee, H.M.; Kang, K.T.; Lee, C.K.; Chang, B.S.; Yeom, J.S. The biomechanical influence of the facet joint orientation and the facet tropism in the lumbar spine. Spine J. 2013, 13, 1301–1308. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Ye, L.; Liu, X.; Weng, R.; Tan, J.; Xie, P.; Yang, Y.; Liang, L.; Huang, W.; Jiang, X. The relationship between facet tropism and cervical disc herniation. J. Anat. 2020, 236, 916–922. [Google Scholar] [CrossRef]
- Liu, Z.; Rong, X.; Liu, H.; Ding, C.; Hong, Y.; Wang, B. Effect of facet tropism on postoperative cervical range of motion after single-level cervical disc arthroplasty. Glob. Spine J. 2021, 2192568220986144. [Google Scholar] [CrossRef]
- Garg, K.; Aggarwal, A. Facet tropism in lumbar spine and cervical spine: A systematic review and meta-analysis. World Neurosurg. 2021, 147, 47–65. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, G.; Lin, J.; Huang, W.; Wang, J.; Teng, H. The correlation between facet tropism and intervertebral disc herniation in the subaxial cervical spine. Spine 2021, 46, E310–E317. [Google Scholar] [CrossRef]
- Rong, X.; Liu, Z.; Wang, B.; Chen, H.; Liu, H. The facet orientation of the subaxial cervical spine and the implications for cervical movements and clinical conditions. Spine 2017, 42, E320–E325. [Google Scholar] [CrossRef]
- Cyron, B.; Hutton, W. Articular tropism and stability of the lumbar spine. Spine 1980, 5, 168–172. [Google Scholar] [CrossRef]
- Alonso, F.; Kirkpatrick, C.M.; Jeong, W.; Fisahn, C.; Usman, S.; Rustagi, T.; Loukas, M.; Chapman, J.R.; Oskouian, R.J.; Tubbs, R.S. Lumbar facet tropism: A comprehensive review. World Neurosurg. 2017, 102, 91–96. [Google Scholar] [CrossRef]
- Alonso, F.; Kirkpatrick, C.M.; Jeong, W.; Fisahn, C.; Usman, S.; Rustagi, T.; Loukas, M.; Chapman, J.R.; Oskouian, R.J.; Tubbs, R.S. Analysis of correlation between age and cervical facet joint degeneration and Modic changes in patients with cervical spondylotic myelopathy. Med. Sci. Monit. 2019, 25, 7882–7888. [Google Scholar]
- Samartzis, D.; Cheung, J.P.Y.; Rajasekaran, S.; Kawaguchi, Y.; Acharya, S.; Kawakami, M.; Satoh, S.; Chen, W.; Park, C.; Lee, C.; et al. Is lumbar facet joint tropism developmental or secondary to degeneration? An international, large-scale multicenter study by the AOSpine Asia Pacific Research Collaboration Consortium. Scoliosis Spinal Disord. 2016, 11, 1–8. [Google Scholar] [CrossRef]
- Kong, M.H.; He, W.; Tsai, Y.D.; Chen, N.F.; Keorochana, G.; Do, D.H.; Wang, J.C. Relationship of facet tropism with degeneration and stability of functional spinal unit. Yonsei Med. J. 2009, 50, 624–629. [Google Scholar] [CrossRef]
- Widmer, J.; Fornaciari, P.; Senteler, M.; Roth, T.; Snedeker, J.G.; Farshad, M. Kinematics of the spine under healthy and degenerative conditions: A systematic review. Ann. Biomed. Eng. 2019, 47, 1491–1522. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, N.; dos Santos Rocha, C.S.; Sheehan, B.; Kennedy, B.A.; Evans, K. Measurement of three-dimensional cervical segmental kinematics: Reliability of whole vertebrae and facet-based approaches. Musculoskelet Sci. Pract. 2019, 44, 102039. [Google Scholar] [CrossRef] [PubMed]
- Berkovits, I.; Hancock, G.R.; Nevitt, J. Bootstrap resampling approaches for repeated measure designs: Relative robustness to sphericity and normality violations. Educ. Psychol. Meas. 2000, 60, 877–892. [Google Scholar] [CrossRef]
- Van Vlasselaer, N.; van Roy, P.; Cattrysse, E. Morphological Asymmetry of the Superior Cervical Facets from C3 through C7 due to Degeneration. Biomed. Res. Int. 2017, 5216087. [Google Scholar] [CrossRef]
- Qu, N.; Lindstrøm, R.; Hirata, R.P.; Graven-Nielsen, T. Origin of neck pain and direction of movement influence dynamic cervical joint motion and pressure pain sensitivity. Clin. Biomech. 2019, 61, 120–128. [Google Scholar] [CrossRef]
- Anderst, W.J.; Lee, J.Y.; Donaldson, W.F., III; Kang, J.D. Six-degrees-of-freedom cervical spine range of motion during dynamic flexion-extension after single-level anterior arthrodesis: Comparison with asymptomatic control subjects. J. Bone Joint Surg. Am. 2013, 95, 497–506. [Google Scholar] [CrossRef]
- Morishita, Y.; Hida, S.; Miyazaki, M.; Hong, S.W.; Zou, J.; Wei, F.; Naito, M.; Wang, J.C. The effects of the degenerative changes in the functional spinal unit on the kinematics of the cervical spine. Spine 2008, 33, E178–E182. [Google Scholar] [CrossRef]
- Nagamoto, Y.; Ishii, T.; Sakaura, H.; Iwasaki, M.; Moritomo, H.; Kashii, M.; Hattori, T.; Yoshikawa, H.; Sugamoto, K. In vivo three-dimensional kinematics of the cervical spine during head rotation in patients with cervical spondylosis. Spine 2011, 36, 778–783. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, N.; Barrett, R.; Laakso, L. Relation between changes in posteroanterior stiffness and active range of movement of the cervical spine following manual therapy treatment. Spine 2008, 33, E673–E679. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).