EBNA1 IgM-Based Discrimination Between Rheumatoid Arthritis Patients, Systemic Lupus Erythematosus Patients and Healthy Controls
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Patient Sera
2.3. Ethics
2.4. Enzyme-Linked Immunosorbent Assay
2.5. Statistics
3. Results
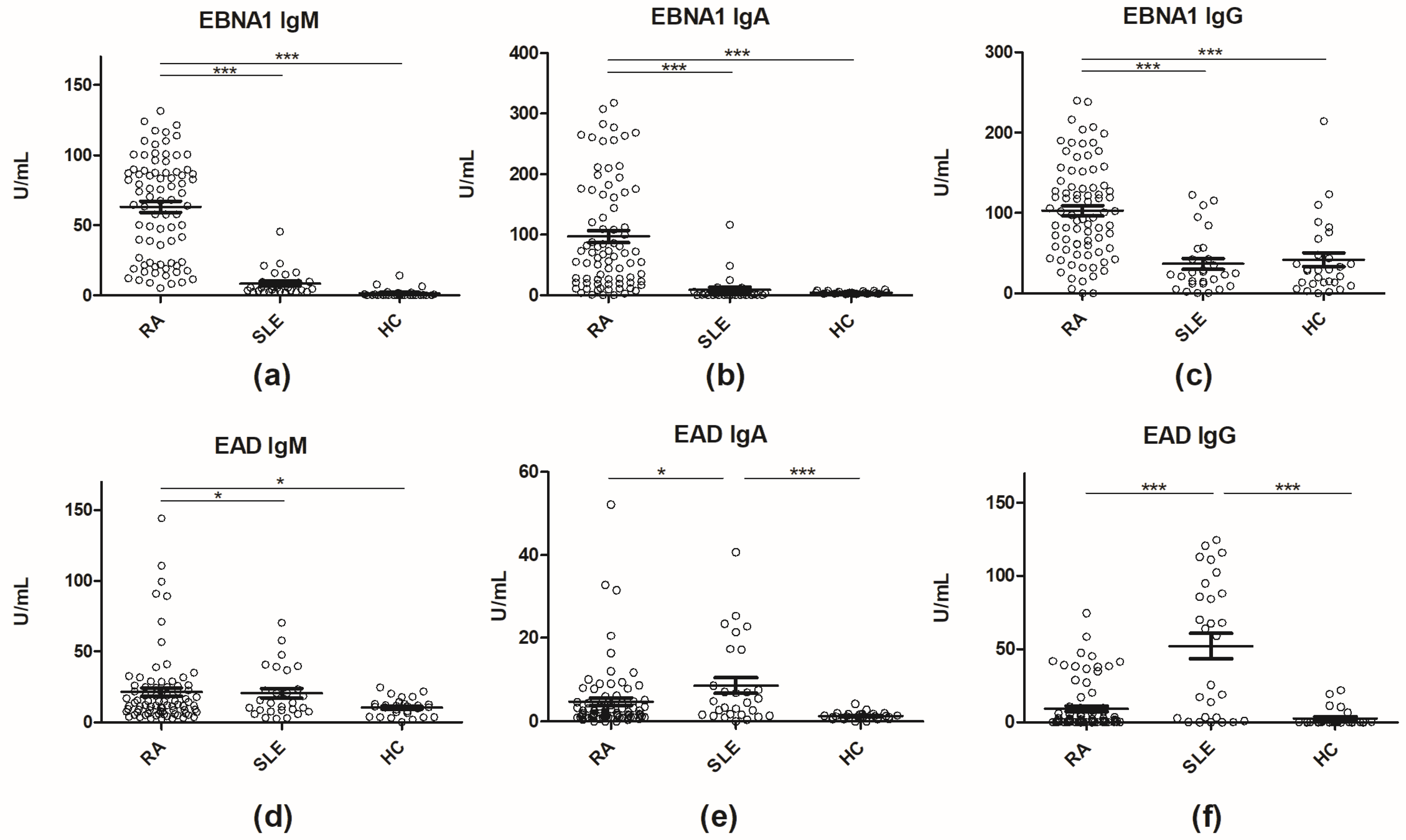
Determination of Antibody Titers to Early Antigen Diffuse and Epstein–Barr Virus Nuclear Antigen 1 by Enzyme-Linked Immunosorbent Assay
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Correa, R.M.; Fellner, M.D.; Alonio, L.V.; Durand, K.; Teyssie, A.R.; Picconi, M.A. Epstein-barr virus (ebv) in healthy carriers: Distribution of genotypes and 30 bp deletion in latent membrane protein-1 (lmp-1) oncogene. J. Med. Virol. 2004, 73, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Smatti, M.K.; Al-Sadeq, D.W.; Ali, N.H.; Pintus, G.; Abou-Saleh, H.; Nasrallah, G.K. Epstein-barr virus epidemiology, serology, and genetic variability of lmp-1 oncogene among healthy population: An update. Front. Oncol. 2018, 8, 211. [Google Scholar] [CrossRef] [PubMed]
- Young, L.S.; Rickinson, A.B. Epstein-barr virus: 40 years on. Nat. Rev. Cancer 2004, 4, 757–768. [Google Scholar] [CrossRef] [PubMed]
- Bravender, T. Epstein-barr virus, cytomegalovirus, and infectious mononucleosis. Adolesc. Med. State Art. Rev. 2010, 21, 251–264. [Google Scholar]
- McInnes, I.B.; Schett, G. The pathogenesis of rheumatoid arthritis. N. Engl. J. Med. 2011, 365, 2205–2219. [Google Scholar] [CrossRef]
- McInnes, I.B.; Schett, G. Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet 2017, 389, 2328–2337. [Google Scholar] [CrossRef]
- Sulaiman, F.N.; Wong, K.K.; Ahmad, W.A.W.; Ghazali, W.S.W. Anti-cyclic citrullinated peptide antibody is highly associated with rheumatoid factor and radiological defects in rheumatoid arthritis patients. Medicine 2019, 98, e14945. [Google Scholar] [CrossRef]
- Karami, J.; Aslani, S.; Jamshidi, A.; Garshasbi, M.; Mahmoudi, M. Genetic implications in the pathogenesis of rheumatoid arthritis; an updated review. Gene 2019, 702, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Deane, K.D.; Demoruelle, M.K.; Kelmenson, L.B.; Kuhn, K.A.; Norris, J.M.; Holers, V.M. Genetic and environmental risk factors for rheumatoid arthritis. Best Pract. Res. Clin. Rheumatol. 2017, 31, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Trier, N.; Izarzugaza, J.; Chailyan, A.; Marcatili, P.; Houen, G. Human mhc-ii with shared epitope motifs are optimal epstein-barr virus glycoprotein 42 ligands-relation to rheumatoid arthritis. Int. J. Mol. Sci. 2018, 19, 317. [Google Scholar] [CrossRef] [PubMed]
- Draborg, A.H.; Duus, K.; Houen, G. Epstein-barr virus and systemic lupus erythematosus. Clin. Dev. Immunol. 2012, 2012, 370516. [Google Scholar] [CrossRef] [PubMed]
- Fava, A.; Petri, M. Systemic lupus erythematosus: Diagnosis and clinical management. J. Autoimmun. 2019, 96, 1–13. [Google Scholar] [CrossRef]
- Kaul, A.; Gordon, C.; Crow, M.K.; Touma, Z.; Urowitz, M.B.; van Vollenhoven, R.; Ruiz-Irastorza, G.; Hughes, G. Systemic lupus erythematosus. Nat. Rev. Dis. Primers 2016, 2, 16039. [Google Scholar] [CrossRef] [PubMed]
- Marks, S.D.; Tullus, K. Autoantibodies in systemic lupus erythematosus. Pediatr. Nephrol. 2012, 27, 1855–1868. [Google Scholar] [CrossRef] [PubMed]
- Yaniv, G.; Twig, G.; Shor, D.B.; Furer, A.; Sherer, Y.; Mozes, O.; Komisar, O.; Slonimsky, E.; Klang, E.; Lotan, E.; et al. A volcanic explosion of autoantibodies in systemic lupus erythematosus: A diversity of 180 different antibodies found in sle patients. Autoimmun. Rev. 2015, 14, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Ghodke-Puranik, Y.; Niewold, T.B. Immunogenetics of systemic lupus erythematosus: A comprehensive review. J. Autoimmun. 2015, 64, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, P.; Avenell, A.; Aucott, L.; Vickers, M.A. Systematic review and meta-analysis of the sero-epidemiological association between epstein-barr virus and systemic lupus erythematosus. Arthritis Res. Ther. 2014, 16, R3. [Google Scholar] [CrossRef]
- Li, Z.X.; Zeng, S.; Wu, H.X.; Zhou, Y. The risk of systemic lupus erythematosus associated with epstein-barr virus infection: A systematic review and meta-analysis. Clin. Exp. Med. 2019, 19, 23–36. [Google Scholar] [CrossRef]
- Mak, A. The impact of vitamin d on the immunopathophysiology, disease activity, and extra-musculoskeletal manifestations of systemic lupus erythematosus. Int. J. Mol. Sci. 2018, 19, 2355. [Google Scholar] [CrossRef] [PubMed]
- Speyer, C.B.; Costenbader, K.H. Cigarette smoking and the pathogenesis of systemic lupus erythematosus. Expert Rev. Clin. Immunol. 2018, 14, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Cassaniti, I.; Cavagna, L.; Calarota, S.A.; Adzasehoun, K.M.G.; Comolli, G.; Montecucco, C.; Baldanti, F. Evaluation of ebv- and hcmv-specific t cell responses in systemic lupus erythematosus (sle) patients using a normalized enzyme-linked immunospot (elispot) assay. J. Immunol. Res. 2019, 2019, 4236503. [Google Scholar] [CrossRef] [PubMed]
- Draborg, A.H.; Jacobsen, S.; Westergaard, M.; Mortensen, S.; Larsen, J.L.; Houen, G.; Duus, K. Reduced response to epstein-barr virus antigens by t-cells in systemic lupus erythematosus patients. Lupus Sci. Med. 2014, 1, e000015. [Google Scholar] [CrossRef] [PubMed]
- Draborg, A.H.; Jorgensen, J.M.; Muller, H.; Nielsen, C.T.; Jacobsen, S.; Iversen, L.V.; Theander, E.; Nielsen, L.P.; Houen, G.; Duus, K. Epstein-barr virus early antigen diffuse (EBV-EA/D)-directed immunoglobulin a antibodies in systemic lupus erythematosus patients. Scand. J. Rheumatol. 2012, 41, 280–289. [Google Scholar] [CrossRef]
- Kang, I.; Quan, T.; Nolasco, H.; Park, S.H.; Hong, M.S.; Crouch, J.; Pamer, E.G.; Howe, J.G.; Craft, J. Defective control of latent epstein-barr virus infection in systemic lupus erythematosus. J. Immunol. 2004, 172, 1287–1294. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, N.S.; Draborg, A.H.; Nielsen, C.T.; Jacobsen, S.; Houen, G. Antibodies to early ebv, cmv, and hhv6 antigens in systemic lupus erythematosus patients. Scand. J. Rheumatol. 2015, 44, 143–149. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Guven, E.; Duus, K.; Lydolph, M.C.; Jorgensen, C.S.; Laursen, I.; Houen, G. Non-specific binding in solid phase immunoassays for autoantibodies correlates with inflammation markers. J. Immunol. Methods 2014, 403, 26–36. [Google Scholar] [CrossRef]
- Houen, G. Nonspecific binding in immunoassays for autoantibodies. Methods Mol. Biol. 2019, 1901, 13–17. [Google Scholar]
- Trier, N.H.; Holm, B.E.; Heiden, J.; Slot, O.; Locht, H.; Jensen, B.; Lindegaard, H.; Svendsen, A.; Nielsen, C.T.; Jacobsen, S.; et al. The use of synthetic peptides for detection of anti-citrullinated protein antibodies in rheumatoid arthritis. J. Immunol. Methods 2018, 454, 6–14. [Google Scholar] [CrossRef]
- Trier, N.H.; Holm, B.E.; Heiden, J.; Slot, O.; Locht, H.; Lindegaard, H.; Svendsen, A.; Nielsen, C.T.; Jacobsen, S.; Theander, E.; et al. Antibodies to a strain-specific citrullinated epstein-barr virus peptide diagnoses rheumatoid arthritis. Sci. Rep. 2018, 8, 3684. [Google Scholar] [CrossRef]
- Westergaard, M.W.; Draborg, A.H.; Troelsen, L.; Jacobsen, S.; Houen, G. Isotypes of epstein-barr virus antibodies in rheumatoid arthritis: Association with rheumatoid factors and citrulline-dependent antibodies. Biomed. Res. Int. 2015, 2015, 472174. [Google Scholar] [CrossRef]
- McDermott, M.; Molloy, M.; Buckley, J.; Greally, J. Antibodies to epstein-barr viral antigens in familial rheumatoid arthritis. Ir. J. Med. Sci. 1989, 158, 203–205. [Google Scholar] [CrossRef]
- Sternbaek, L.; Draborg, A.H.; Osterlund, M.T.; Iversen, L.V.; Troelsen, L.; Theander, E.; Nielsen, C.T.; Jacobsen, S.; Houen, G. Increased antibody levels to stage-specific epstein-barr virus antigens in systemic autoimmune diseases reveal a common pathology. Scand. J. Clin. Lab. Investig. 2019, 79, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Yazbek, M.A.; Barros-Mazon, S.; Rossi, C.L.; Londe, A.C.; Costallat, L.T.; Bertolo, M.B. Association analysis of anti-epstein-barr nuclear antigen-1 antibodies, anti-cyclic citrullinated peptide antibodies, the shared epitope and smoking status in brazilian patients with rheumatoid arthritis. Clinics 2011, 66, 1401–1406. [Google Scholar] [CrossRef] [PubMed]
- Origgi, L.; Perego, R.; Hu, C.; Bertetti, E.; D’Agostino, P.; Asero, R.; Riboldi, P. Anti-epstein-barr virus antibodies in systemic lupus erythematosus. Boll. Ist. Sieroter. Milan. 1988, 67, 116–122. [Google Scholar]
- Draborg, A.H.; Duus, K.; Houen, G. Epstein-barr virus in systemic autoimmune diseases. Clin. Dev. Immunol. 2013, 2013, 535738. [Google Scholar] [CrossRef] [PubMed]
- Dellavance, A.; Andrade, L.E.C. Detection of autoantibodies by indirect immunofluorescence cytochemistry on hep-2 cells. Methods Mol. Biol. 2019, 1901, 19–46. [Google Scholar] [PubMed]
- Houen, G. Autoantibodies as diagnostic tools. Methods Mol. Biol. 2019, 1901, 1–11. [Google Scholar]
- Jorgensen, K.T.; Wiik, A.; Pedersen, M.; Hedegaard, C.J.; Vestergaard, B.F.; Gislefoss, R.E.; Kvien, T.K.; Wohlfahrt, J.; Bendtzen, K.; Frisch, M. Cytokines, autoantibodies and viral antibodies in premorbid and postdiagnostic sera from patients with rheumatoid arthritis: Case-control study nested in a cohort of norwegian blood donors. Ann. Rheum. Dis. 2008, 67, 860–866. [Google Scholar] [CrossRef]
- Trier, N.H. Use of a citrullinated peptide panel for detection of anti-citrullinated protein antibodies by enzyme-linked immunosorbent assay. Methods Mol. Biol. 2019, 1901, 243–253. [Google Scholar]
- Erre, G.L.; Mameli, G.; Cossu, D.; Muzzeddu, B.; Piras, C.; Paccagnini, D.; Passiu, G.; Sechi, L.A. Increased epstein-barr virus DNA load and antibodies against ebna1 and ea in sardinian patients with rheumatoid arthritis. Viral Immunol. 2015, 28, 385–390. [Google Scholar] [CrossRef]
- Lunemann, J.D.; Frey, O.; Eidner, T.; Baier, M.; Roberts, S.; Sashihara, J.; Volkmer, R.; Cohen, J.I.; Hein, G.; Kamradt, T.; et al. Increased frequency of ebv-specific effector memory cd8+ t cells correlates with higher viral load in rheumatoid arthritis. J. Immunol. 2008, 181, 991–1000. [Google Scholar] [CrossRef] [PubMed]
- Petersen, J.; Rhodes, G.; Roudier, J.; Vaughan, J.H. Altered immune response to glycine-rich sequences of epstein-barr nuclear antigen-1 in patients with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Rheum. 1990, 33, 993–1000. [Google Scholar] [CrossRef] [PubMed]
- Us, T.; Cetin, E.; Kasifoglu, N.; Kasifoglu, T.; Akgun, Y. Investigation of epstein-barr virus and herpes simplex virus markers by serological and molecular methods in patients with rheumatoid arthritis and systemic lupus erythematosus. Mikrobiyol. Bul. 2011, 45, 677–683. [Google Scholar] [PubMed]
- Chen, C.J.; Lin, K.H.; Lin, S.C.; Tsai, W.C.; Yen, J.H.; Chang, S.J.; Lu, S.N.; Liu, H.W. High prevalence of immunoglobulin a antibody against epstein-barr virus capsid antigen in adult patients with lupus with disease flare: Case control studies. J. Rheumatol. 2005, 32, 44–47. [Google Scholar]
- Chougule, D.; Nadkar, M.; Rajadhyaksha, A.; Pandit-Shende, P.; Surve, P.; Dawkar, N.; Khadilkar, P.; Patwardhan, M.; Kaveri, S.; Ghosh, K.; et al. Association of clinical and serological parameters of systemic lupus erythematosus patients with epstein-barr virus antibody profile. J. Med. Virol. 2018, 90, 559–563. [Google Scholar] [CrossRef]
- Cui, J.; Yan, W.; Xu, S.; Wang, Q.; Zhang, W.; Liu, W.; Ni, A. Anti-epstein-barr virus antibodies in beijing during 2013-2017: What we have found in the different patients. PLoS ONE 2018, 13, e0193171. [Google Scholar] [CrossRef]
- Esen, B.A.; Yilmaz, G.; Uzun, S.; Ozdamar, M.; Aksozek, A.; Kamali, S.; Turkoglu, S.; Gul, A.; Ocal, L.; Aral, O.; et al. Serologic response to epstein-barr virus antigens in patients with systemic lupus erythematosus: A controlled study. Rheumatol. Int. 2012, 32, 79–83. [Google Scholar] [CrossRef]
- James, J.A.; Neas, B.R.; Moser, K.L.; Hall, T.; Bruner, G.R.; Sestak, A.L.; Harley, J.B. Systemic lupus erythematosus in adults is associated with previous epstein-barr virus exposure. Arthritis Rheum. 2001, 44, 1122–1126. [Google Scholar] [CrossRef]
- Zandman-Goddard, G.; Berkun, Y.; Barzilai, O.; Boaz, M.; Blank, M.; Ram, M.; Sherer, Y.; Anaya, J.M.; Shoenfeld, Y. Exposure to epstein-barr virus infection is associated with mild systemic lupus erythematosus disease. Ann. N. Y. Acad. Sci. 2009, 1173, 658–663. [Google Scholar] [CrossRef]
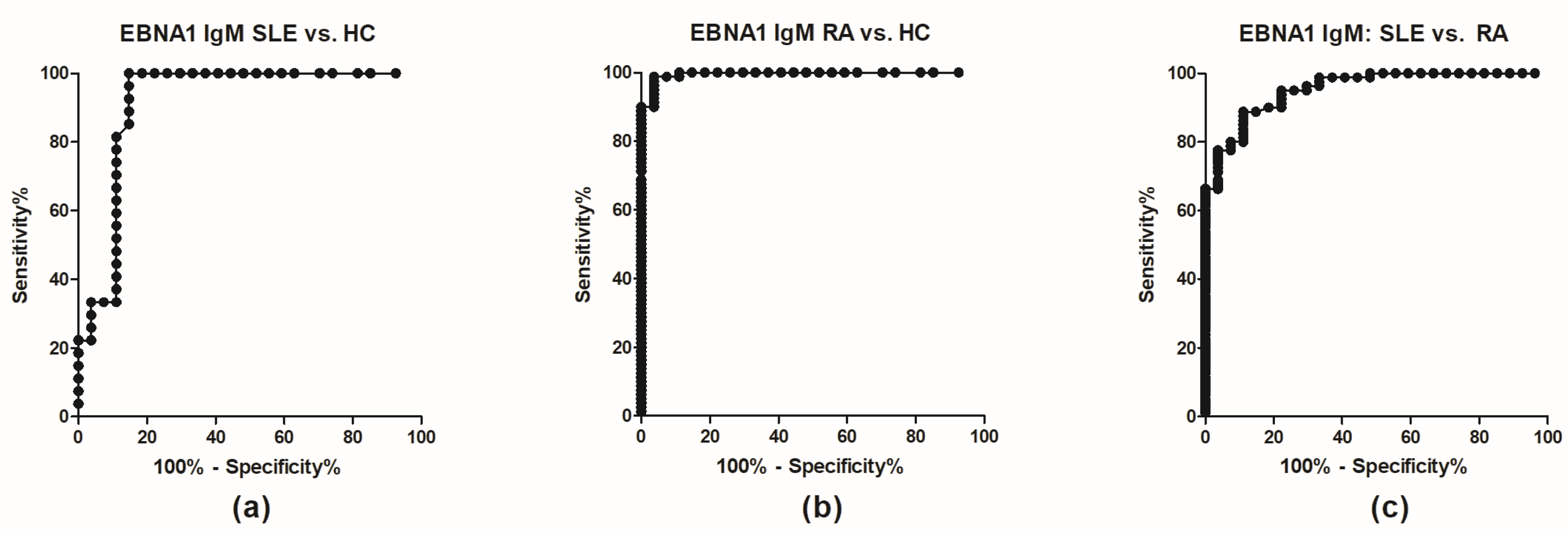
| AUC | Std. Error | 95% Confidence Interval | p Value | |
|---|---|---|---|---|
| EBNA1 IgG | ||||
| SLE vs HC | 0.5198 | 0.7885 | 0.3653–0.6744 | 0.8006 |
| RA vs HC | 0.8125 | 0.04936 | 0.7157–0.9093 | <0.0001 |
| SLE vs RA | 0.8356 | 0.04357 | 0.7503–0.921 | <0.0001 |
| EBNA1 IgA | ||||
| SLE vs HC | 0.7037 | 0.08256 | 0.5419–0.8655 | 0.0102 |
| RA vs HC | 0.9456 | 0.0237 | 0.8992–0.992 | <0.0001 |
| SLE vs RA | 0.9183 | 0.03222 | 0.8551–0.9814 | <0.0001 |
| EBNA1 IgM | ||||
| SLE vs HC | 0.9156 | 0.04432 | 0.8288–1.003 | <0.0001 |
| RA vs HC | 0.9954 | 0.04285 | 0.987–1.004 | <0.0001 |
| SLE vs RA | 0.953 | 0.01944 | 0.9149–0.9911 | <0.0001 |
| EAD IgG | ||||
| SLE vs HC | 0.8347 | 0.05862 | 0.7298–0.9496 | <0.0001 |
| RA vs HC | 0.7377 | 0.06006 | 0.62–0.8554 | 0.0002 |
| SLE vs RA | 0.7477 | 0.0694 | 0.6117–0.8837 | <0.0001 |
| EAD IgA | ||||
| SLE vs HC | 0.8272 | 0.06039 | 0.7088–0.9455 | <0.0001 |
| RA vs HC | 0.7169 | 0.04997 | 0.619–0.8248 | 0.0008 |
| SLE vs RA | 0.6544 | 0.06353 | 0.5299–0.7789 | 0.0410 |
| EAD IgM | ||||
| SLE vs HC | 0.6612 | 0.07527 | 0.5137–0.8087 | 0.0421 |
| RA vs HC | 0.6306 | 0.05724 | 0.5184–0.7427 | 0.0431 |
| SLE vs RA | 0.5417 | 0.06394 | 0.4163–0.667 | 0.8694 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trier, N.H.; Draborg, A.H.; Sternbæk, L.; Troelsen, L.; Larsen, J.L.; Jacobsen, S.; Houen, G. EBNA1 IgM-Based Discrimination Between Rheumatoid Arthritis Patients, Systemic Lupus Erythematosus Patients and Healthy Controls. Antibodies 2019, 8, 35. https://doi.org/10.3390/antib8020035
Trier NH, Draborg AH, Sternbæk L, Troelsen L, Larsen JL, Jacobsen S, Houen G. EBNA1 IgM-Based Discrimination Between Rheumatoid Arthritis Patients, Systemic Lupus Erythematosus Patients and Healthy Controls. Antibodies. 2019; 8(2):35. https://doi.org/10.3390/antib8020035
Chicago/Turabian StyleTrier, Nicole Hartwig, Anette Holck Draborg, Louise Sternbæk, Lone Troelsen, Janni Lisander Larsen, Søren Jacobsen, and Gunnar Houen. 2019. "EBNA1 IgM-Based Discrimination Between Rheumatoid Arthritis Patients, Systemic Lupus Erythematosus Patients and Healthy Controls" Antibodies 8, no. 2: 35. https://doi.org/10.3390/antib8020035
APA StyleTrier, N. H., Draborg, A. H., Sternbæk, L., Troelsen, L., Larsen, J. L., Jacobsen, S., & Houen, G. (2019). EBNA1 IgM-Based Discrimination Between Rheumatoid Arthritis Patients, Systemic Lupus Erythematosus Patients and Healthy Controls. Antibodies, 8(2), 35. https://doi.org/10.3390/antib8020035




