Neutralizing and Total/IgG Spike Antibody Responses Following Homologous CoronaVac vs. BNT162b2 Vaccination Up to 90 Days Post-Booster
Abstract
:1. Introduction
2. Methods
2.1. Study Participants
2.2. Methods and Materials
2.3. Statistical Analysis
3. Results
4. Discussion
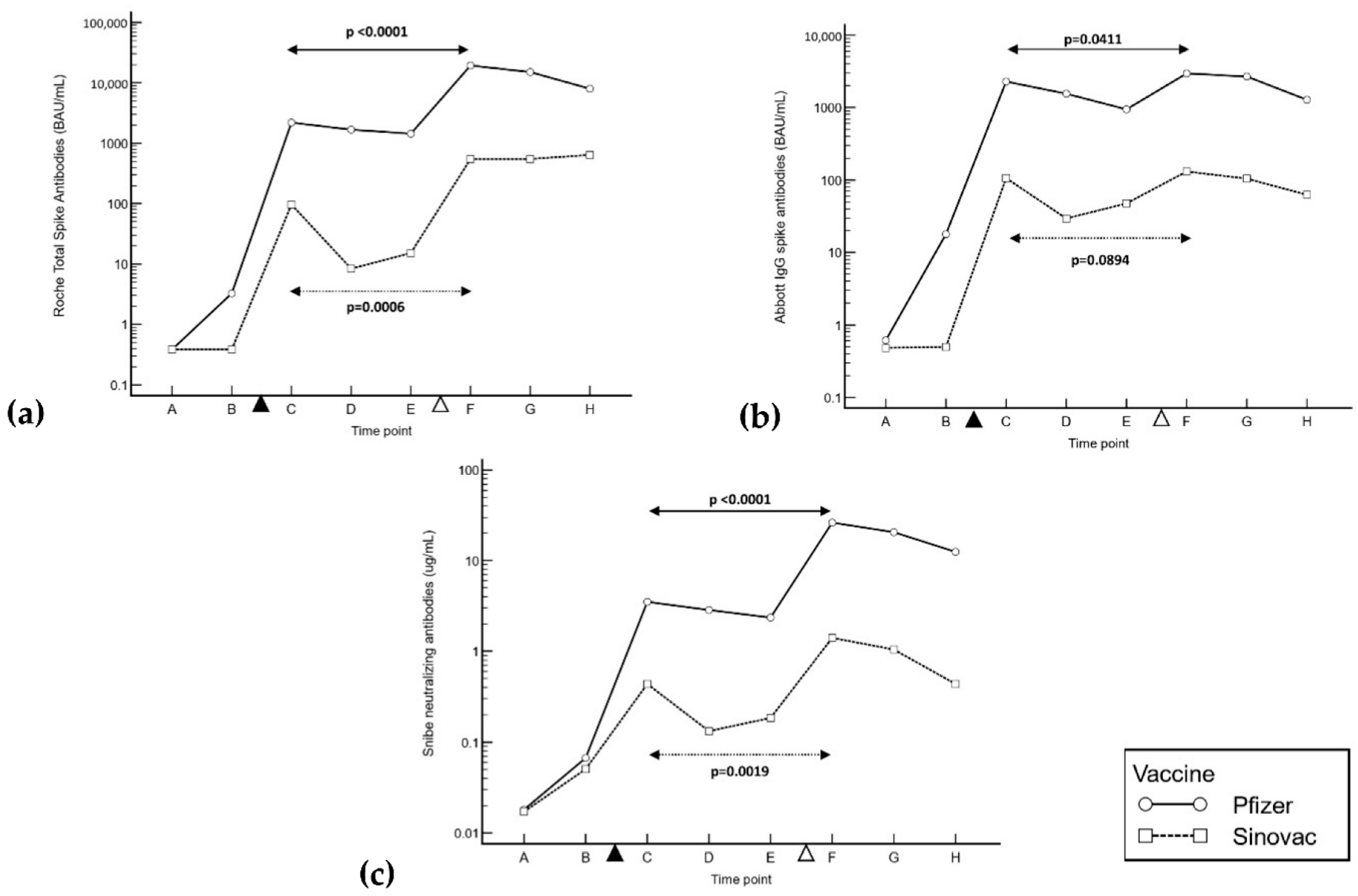
- After the second and third inoculations, inactivated virus vaccines produced a much lower post-vaccination antibody response than mRNA vaccines considering all antibodies (total S-Ab, IgG and N-Ab), even 90 days post-booster.
- Aside from IgG in inactivated virus vaccinees, the peak antibody titers increased after booster vaccination in both vaccination groups.
- In all vaccinees, total S-Ab, IgG and N-Ab antibody levels declined up to 90 days post-booster.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Watson, O.J.; Barnsley, G.; Toor, J.; Hogan, A.B.; Winskill, P.; Ghani, A.C. Global impact of the first year of COVID-19 vaccination: A mathematical modelling study. Lancet Infect. Dis. 2022, 22, 1293–1302. [Google Scholar] [CrossRef]
- Premikha, M.; Chiew, C.J.; Wei, W.E.; Leo, Y.S.; Ong, B.; Lye, D.C.; Lee, V.J.; Tan, K.B. Comparative Effectiveness of mRNA and Inactivated Whole Virus Vaccines against COVID-19 Infection and Severe Disease in Singapore. Clin. Infect. Dis. 2022, 75, 1442–1445. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Shao, W.; Chen, X.; Zhang, B.; Wang, G.; Zhang, W. Real-world effectiveness of COVID-19 vaccines: A literature review and meta-analysis. Int. J. Infect. Dis. 2022, 114, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Zuo, F.; Abolhassani, H.; Du, L.; Piralla, A.; Bertoglio, F.; de Campos-Mata, L.; Wan, H.; Schubert, M.; Cassaniti, I.; Wang, Y.; et al. Heterologous immunization with inactivated vaccine followed by mRNA-booster elicits strong immunity against SARS-CoV-2 Omicron variant. Nat. Commun. 2022, 13, 2670. [Google Scholar] [CrossRef] [PubMed]
- Klingler, J.; Weiss, S.; Itri, V.; Liu, X.; Oguntuyo, K.Y.; Stevens, C.; Ikegame, S.; Hung, C.T.; Enyindah-Asonye, G.; Amanat, F.; et al. Role of Immunoglobulin M and A Antibodies in the Neutralization of Severe Acute Respiratory Syndrome Coronavirus 2. J. Infect. Dis. 2021, 223, 957–970. [Google Scholar] [CrossRef]
- Pang, N.Y.L.; Pang, A.S.R.; Chow, V.T.; Wang, D.Y. Understanding neutralizing antibodies against SARS-CoV-2 and their implications in clinical practice. Mil. Med. Res. 2021, 8, 47. [Google Scholar] [CrossRef]
- Lau, C.S.; Oh, M.L.H.; Phua, S.K.; Liang, Y.L.; Li, Y.; Huo, J.; Huang, Y.; Zhang, B.; Xu, S.; Aw, T.C. Kinetics of the Neutralizing and Spike SARS-CoV-2 Antibodies following the Sinovac Inactivated Virus Vaccine Compared to the Pfizer mRNA Vaccine in Singapore. Antibodies 2022, 11, 38. [Google Scholar] [CrossRef]
- Ng, O.T.; Marimuthu, K.; Lim, N.; Lim, Z.Q.; Thevasagayam, N.M.; Koh, V.; Chiew, C.J.; Ma, S.; Koh, M.; Low, P.Y.; et al. Analysis of COVID-19 Incidence and Severity Among Adults Vaccinated With 2-Dose mRNA COVID-19 or Inactivated SARS-CoV-2 Vaccines with and Without Boosters in Singapore. JAMA. Netw. Open. 2022, 5, e2228900. [Google Scholar] [CrossRef]
- Qaqish, A.; Abbas, M.M.; Al-Tamimi, M.; Abbas, M.A.; Al-Omari, M.; Alqassieh, R. SARS-CoV-2 Antinucleocapsid Antibody Response of mRNA and Inactivated Virus Vaccines Compared to Unvaccinated Individuals. Vaccines 2022, 10, 643. [Google Scholar] [CrossRef]
- Lau, C.S.; Phua, S.K.; Liang, Y.L.; Oh, H.M.L.; Aw, T.C. Robust SARS-CoV-2 Antibody Responses in Asian COVID-Naïve Subjects 180 Days after Two Doses of BNT162b2 mRNA COVID-19 Vaccine. Vaccines 2021, 9, 1241. [Google Scholar] [CrossRef]
- Padoan, A.; Cosma, C.; Bonfante, F.; Rocca, F.D.; Barbaro, F.; Santarossa, C.; Dall’Olmo, L.; Pagliari, M.; Bortolami, A.; Cattelan, A.; et al. Neutralizing antibody titers six months after Comirnaty vaccination: Kinetics and comparison with SARS-CoV-2 immunoassays. Clin. Chem. Lab. Med. 2021, 60, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Bednarski, E.; Estrada, P.M.D.R.; DaSilva, J.; Boudkadida, C.; Zhang, F.; Luna-Villalobos, Y.A.; Rodriguez-Rangel, X.; Piten-Isidro, E.; Luna-Garcia, E.; Rivera, D.D.; et al. Antibody and Memory B-Cell Immunity in a Heterogeneously SARS-CoV-2-Infected and -Vaccinated Population. mBio 2022, 13, e0084022. [Google Scholar] [CrossRef] [PubMed]
- Ozakbas, S.; Baba, C.; Dogan, Y.; Cevik, S.; Ozcelik, S.; Kaya, E. Comparison of SARS-CoV-2 antibody response after two doses of mRNA and inactivated vaccines in multiple sclerosis patients treated with disease-modifying therapies. Mult. Scler. Relat. Disord. 2022, 58, 103486. [Google Scholar] [CrossRef] [PubMed]
- Barin, B.; Kasap, U.; Selcuk, F.; Volkan, E.; Uluckan, O. Comparison of SARS-CoV-2 anti-spike receptor binding domain IgG antibody responses after CoronaVac, BNT162b2, ChAdOx1 COVID-19 vaccines, and a single booster dose: A prospective, longitudinal population-based study. Lancet Microbe. 2022, 3, e274–e283. [Google Scholar] [CrossRef]
- Clemens, S.A.C.; Weckx, L.; Clemens, R.; Mendes, A.V.A.; Souza, A.R.; Silveira, M.B.V.; da Guarda, S.N.F.; de Nobrega, M.M.; Pinto, M.I.M.; Gonzalez, I.G.S.; et al. Heterologous versus homologous COVID-19 booster vaccination in previous recipients of two doses of CoronaVac COVID-19 vaccine in Brazil (RHH-001): A phase 4, non-inferiority, single blind, randomised study. Lancet 2022, 399, 521–529. [Google Scholar] [CrossRef]
- Smith, A.W.; Mulholland, K. Effectiveness of an Inactivated SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 385, 946–948. [Google Scholar] [CrossRef]
- Matusali, G.; Sberna, G.; Meschi, S.; Gramigna, G.; Colavita, F.; Lapa, D.; Francalancia, M.; Bettini, A.; Capobianchi, M.R.; Puro, V.; et al. Differential Dynamics of SARS-CoV-2 Binding and Functional Antibodies upon BNT162b2 Vaccine: A 6-Month Follow-Up. Viruses 2022, 14, 312. [Google Scholar] [CrossRef]
- Collie, S.; Nayager, J.; Bamford, L.; Bekker, L.G.; Zylstra, M.; Gray, G. Effectiveness and Durability of the BNT162b2 Vaccine against Omicron Sublineages in South Africa. N. Engl. J. Med. 2022, 387, 1332–1333. [Google Scholar] [CrossRef]
- Hitchings, M.D.T.; Ranzani, O.; Lind, M.L.; Dorion, M.; D’Agostini, T.L.; de Paula, R.C.; de Paula, O.F.P.; Villela, E.F.M.; Torres, M.S.S.; de Oliveira, S.B.; et al. Change in COVID-19 risk over time following vaccination with CoronaVac: Test negative case-control study. BMJ 2022, 377, e070102. [Google Scholar] [CrossRef]
- Ranzani, O.T.; Hitchings, M.D.T.; de Melo, R.L.; de Franca, G.V.A.; Fernandes, C.F.R.; Lind, M.L.; Torres, M.S.S.; Tsuha, D.H.; David, L.C.S.; Said, R.F.C.; et al. Effectiveness of an Inactivated COVID-19 Vaccine with Homologous and Heterologous Boosters against Omicron in Brazil. Nat. Commun. 2022, 13, 5536. [Google Scholar] [CrossRef]
- Zhang, B.; Huo, J.; Huang, Y.; Teo, S.Y.; Duan, K.; Li, Y.; Toh, L.K.; Lam, K.P.; Xu, S. mRNA Booster Vaccination Enhances Antibody Responses against SARS-CoV2 Omicron Variant in Individuals Primed with mRNA or Inactivated Virus Vaccines. Vaccines 2022, 10, 1057. [Google Scholar] [CrossRef] [PubMed]
- Vargas, L.; Valdivieso, N.; Tempio, F.; Simon, V.; Sauma, D.; Valenzuela, L.; Beltran, C.; Castillo-Delgado, L.; Contreras-Benavides, X.; Acevedo, M.L.; et al. Serological study of CoronaVac vaccine and booster doses in Chile: Immunogenicity and persistence of anti-SARS-CoV-2 spike antibodies. BMC. Med. 2022, 20, 216. [Google Scholar] [CrossRef] [PubMed]
- Khoury, D.S.; Cromer, D.; Reynaldi, A.; Schlub, T.E.; Wheatley, A.K.; Juno, J.A.; Subbarao, K.; Kent, S.J.; Triccas, J.A.; Davenport, M.P. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 2021, 27, 1205–1211. [Google Scholar] [CrossRef]
- Xin, Q.; Wu, Q.; Chen, X.; Han, B.; Chu, K.; Song, Y.; Jin, H.; Chen, P.; Lu, W.; Yang, T.; et al. Six-month follow-up of a booster dose of CoronaVac in two single-centre phase 2 clinical trials. Nat. Commun. 2022, 13, 3100. [Google Scholar] [CrossRef]
- Earle, K.A.; Ambrosino, D.M.; Fiore-Gartland, A.; Goldblatt, D.; Gilber, P.B.; Siber, G.R.; Dull, P.; Plotkin, S.A. Evidence for antibody as a protective correlate for COVID-19 vaccines. Vaccine 2021, 39, 4423–4428. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.M.S.; Mok, C.K.P.; Leung, Y.W.Y.; Ng, S.S.; Chan, K.C.K.; Ko, F.W.; Chen, C.; You, K.; Lam, B.H.S.; Lau, E.H.Y.; et al. Neutralizing antibodies against the SARS-CoV-2 Omicron variant BA.1 following homologous and heterologous CoronaVac or BNT162b2 vaccination. Nat. Med. 2022, 28, 486–489. [Google Scholar] [CrossRef] [PubMed]
- Leung, N.H.L.; Cheng, S.M.S.; Cohen, C.A.; Martin-Sanchez, M.; Au, N.Y.M.; Luk, L.L.H.; Tsang, L.C.H.; Kwan, K.K.H.; Chaothai, S.; Fung, L.W.C.; et al. Homologous and heterologous boosting with CoronaVac and BNT162b2: A randomized trial (the Cobovax study). medRxiv 2022. [Google Scholar] [CrossRef]
| Population Characteristic | BNT162b2 Vaccinees | CoronaVac Vaccinees |
|---|---|---|
| Mean Age (range, SD) | 43.8 (22–90, 13.5) | 46.1 (22–68, 13.6) |
| Percentage ≥ 60 years old | 16.18% (22/136) | 18.75% (6/32) |
| Gender | 39 male, 97 female | 6 male, 11 female, 15 unknown |
| Median days (IQR) | ||
| Interval between dose 1 and 2 | 21.0 (21.0 to 21.0) | 21.0 (21.0 to 21.8) |
| Interval between dose 2 and 3 | 239.5 (231.0 to 254.0) | 93.0 (93.0 to 100.5) |
| Dose 1 to time point B (10 days post-dose 1) | 10.0 (10.0 to 12.0) | 11.0 (10.5 to 13.0) |
| Dose 2 to time point C (20 days post-dose 2) | 21.0 (20.0 to 22.0) | 20.5 (19.5 to 21.5) |
| Dose 2 to time point D (40 days post-dose 2) | 40.0 (40.0 to 43.0) | 40.5 (40.0 to 41.0) |
| Dose 2 to time point E (60 days post-dose 2) | 61.0 (60.0 to 62.0) | 60.0 (60.0 to 60.0) |
| Dose 3 to time point F (20–30 days post-dose 3) | 26.5 (19.0 to 31.0) | 20.0 (20.0 to 22.0) |
| Dose 3 to time point G (50–70 days post-dose 3) | 59.5 (57.0 to 61.0) | 70.0 (54.3 to 70.0) |
| Dose 3 to time point H (90 days post-dose 3) | 89.5 (88.0 to 92.0) | 90.0 (90.0 to 90.5) |
| Time Point | Roche Total Antibodies | Abbott IgG | Snibe Neutralizing Antibodies | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pfizer (BAU/mL) | Sinovac (BAU/mL) | Difference (BAU/mL) (p Value) | Pfizer (BAU/mL) | Sinovac (BAU/mL) | Difference (BAU/mL) (p Value) | Pfizer Median N-Ab (μg/mL) | Sinovac Median N-Ab (μg/mL) | Mann–Whitney U Difference (μg/mL) (95% CI) | |
| 10 days post-dose 1 | 3.29 | 0.39 | 2.29 (p < 0.0001) | 17.8 | 0.50 | 17.2 (p < 0.0001) | 1.71 | 0.22 | 0.019 (p = 0.1191) |
| 20 days post-dose 2 | 2219 | 97.0 | 2079 (p < 0.0001) | 2271 | 106 | 2177 (p < 0.0001) | 3.52 | 0.44 | 2.87 (p < 0.0001) |
| 40 days post-dose 2 | 1695 | 13.0 | 1682 (p = 0.0173) | 1547 | 29.5 | 1509 (p = 0.0174) | 2.84 | 0.14 | 2.68 (p = 0.0173) |
| 60 days post-dose 2 | 1454 | 94.9 | 1373 (p = 0.0173) | 941 | 48.0 | 898 (p = 0.0173) | 2.35 | 0.21 | 2.17 (p = 0.0173) |
| 20–30 days post-dose 3 | 19,562 | 555 | 18,285 (p < 0.0001) | 2932 | 131 | 2685 (p < 0.0001) | 26.4 | 1.41 | 24.4 (p < 0.0001) |
| 50–70 days post-dose 3 | 14,992 | 590 | 14,403 (p = 0.0055) | 2659 | 105 | 2554 (p = 0.0055) | 20.6 | 1.05 | 19.6 (p = 0.0055) |
| 90 days post-dose 3 | 7532 | 646 | 7101 (p = 0.0001) | 1276 | 62.4 | 1174 (p = 0.0001) | 12.5 | 0.44 | 11.6 (p = 0.0037) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lau, C.S.; Thundyil, J.; Oh, M.L.H.; Phua, S.K.; Liang, Y.L.; Li, Y.; Huo, J.; Huang, Y.; Zhang, B.; Xu, S.; et al. Neutralizing and Total/IgG Spike Antibody Responses Following Homologous CoronaVac vs. BNT162b2 Vaccination Up to 90 Days Post-Booster. Antibodies 2022, 11, 70. https://doi.org/10.3390/antib11040070
Lau CS, Thundyil J, Oh MLH, Phua SK, Liang YL, Li Y, Huo J, Huang Y, Zhang B, Xu S, et al. Neutralizing and Total/IgG Spike Antibody Responses Following Homologous CoronaVac vs. BNT162b2 Vaccination Up to 90 Days Post-Booster. Antibodies. 2022; 11(4):70. https://doi.org/10.3390/antib11040070
Chicago/Turabian StyleLau, Chin Shern, John Thundyil, May Lin Helen Oh, Soon Kieng Phua, Ya Li Liang, Yanfeng Li, Jianxin Huo, Yuhan Huang, Biyan Zhang, Shengli Xu, and et al. 2022. "Neutralizing and Total/IgG Spike Antibody Responses Following Homologous CoronaVac vs. BNT162b2 Vaccination Up to 90 Days Post-Booster" Antibodies 11, no. 4: 70. https://doi.org/10.3390/antib11040070
APA StyleLau, C. S., Thundyil, J., Oh, M. L. H., Phua, S. K., Liang, Y. L., Li, Y., Huo, J., Huang, Y., Zhang, B., Xu, S., & Aw, T. C. (2022). Neutralizing and Total/IgG Spike Antibody Responses Following Homologous CoronaVac vs. BNT162b2 Vaccination Up to 90 Days Post-Booster. Antibodies, 11(4), 70. https://doi.org/10.3390/antib11040070






